Abstract
Spontaneous medialstinal emphysema (pneumomediastinum) and pneumopericardium may be defined as the presence of free air or gas in the mediastinal structures and in the pericardial sac without an apparent precipitating cause. It most frequently occurs in young healthy adults without serious underlying pulmonary disease.
Although pneumomediastinum and pneumopericardium is often asymptomatic, it may cause pain in the neck and chest, dysphonia and shortness of breath. Treatment is supportive unless the patient has a history of trauma from foreign body aspiration. The course of spontaneous pneumomediastinum and pneumopericardium is usually benign and self-limited.
A case of spontaneous pneumomediastinum, pneumopericardium and subcutaneous emphysema in a 20-year-old male is reported in this paper.
Keywords: Mediastinal emphysema (pneumomediastinum), Pneumopericardium
INTRODUCTION
Spontaneous pneumomediastinum and pneumopericardium may be defined as the presence of free air or gas in the mediastinal structures and in the pericardial sac without an apparent precipitating cause. Its occurrence approximates one case per 12,000 hospital admissions1). It most frequently occurs in young healthy adults without serious underlying pulmonary disease2).
Free air can enter mediastinal tissues by rupture of alveoli, laceration of the tracheobronchial tree or gastrointestinal tract, or passage of extraluminal gas into the thorax from the neck, retroperitoneum or chest wall3). Posteroanterior chest radiographs typically reveal a radiolucency between the left heart border and the mediastinal pleura.
Although pneumomediastinum is often asymptomatic, it may cause pain in the neck and chest, dysphonia and shortness of breath. Although severe complications develop in some patients, the course of spontaneous pneumomediastinum is usually benign and self-limited.
We report here a rare case of spontaneous pneumomediastinum, pneumopericardium and subcutaneous emphysema in a young adult, with a review of the literature.
CASE
A 20-year-old male was admitted to the hospital with acute respiratory distress due to severe pain in the neck and chest during inspiration after having a spontaneous cough when he had been drinking a cup of coffee. He was in his usual state of good health prior to this event. He had no current history of trauma, aspiration of foreign body or drug abuse. He had no prior history of medical and surgical disease.
He was afebrile. On physical examination, the blood pressure was 150/100 mmHg, the pulse was 80 beats/min and respirations were 22/min. He appeared acutely ill. The crepitus by palpitation was remarkable along the left side of neck and anterior chest wall. The chest evaluation demonstrated symmetric, clear breath sounds and regular heart beats without murmur or Hamman’s sign.
An arterial blood gas analysis in room-air was followed; pH 7.432, PaO2 79.7 mmHg, PaCO2 45.9 mmHg, and SaO2 96.4%. The hemoglobin was 12.5 g/dL, the hematocrit was 38%, the white cell count was 13,200/mm3 and the Platelet was 231,000/mm3. The blood chemistry and urinalysis were normal. The electrocardiogram was nonspecific.
The chest and neck radiographs showed pneumomediastinum, pneumopericardium and subcutaneous emphysema in the neck and prevertebral space, but there was no evidence of pneumothorax (Figure 1).
Figure 1.
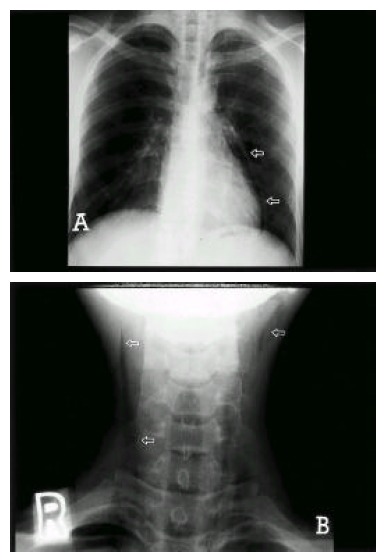
The radiograph of the chest (Panel A) showed pneumomediastinum and pneumopericardium (arrow) but it was clear on the lung fields. The radiograph of the neck (Panel B) showed subcutaneous emphysema (arrow).
The radiograph with Gastrografin swallowing did not reveal any definite evidence of leakage from the esophagus and structural abnormalities (Figure 2). The chest CT scan showed pneumomediastinum with extensive emphysema in the lower neck region with extension to the prevertebral soft tissue space and pneumopericardium. But there was neither a definite lung lesion nor any structural abnormalities in the bronchi and esophagus (Figure 3).
Figure 2.

The radiograph with Gastrografin swallowing did not reveal any definite evidence of leakage from the esophagus and structural abnormalities.
Figure 3.
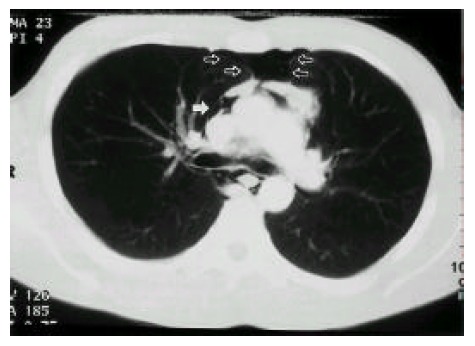
The chest CT scan showed pneumomediastinum (blank arrow) and pneumopericardium (white arrow) but there was neither a definite lung lesion nor any structural abnormalities in bronchi and esophagus.
He was put on absolute bed rest. We tried an oxygen supply with close observation. The next day, his clinical symptoms were alleviated to a great extent. On the 7th hospital day, he had neither any symptoms of respiratory distress nor pain in the neck and chest. The follow-up radiographs and CT scan of the chest showed a complete resolution of pneumomediastinum, pneumopericardium and subcutaneous emphysema (Figure 4).
Figure 4.
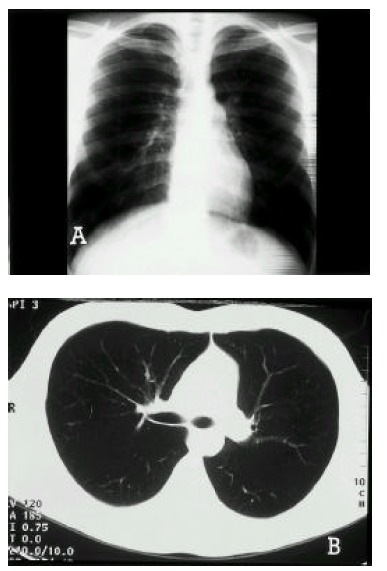
The follow-up radiograph (panel A) and CT scan (Panel B) of chest showed a complete resolution of prior pneumomediastinum and pneumopericardium.
DISCUSSION
Spontaneous pneumomediastinum is a rare and usually self-limited disease most commonly seen in young men and parturient women. The incidence is difficult to evaluate because the disease is frequently unrecognized.
The pathophysiology was demonstrated by Macklin in animal studies4). An increased pressure gradient between the intra-alveolar and interstitial spaces enhances air leakage from small alveolar openings and ruptured alveoli into the perivascular adventitia yielding interstitial emphysema. The pressure gradient favors air dissection along the vascular sheaths toward the hilum. Pneumothorax may occur if the mediastinal pressure rises abruptly. However, because the visceral layers of the deep cervical fascia are contiguous with the mediastinum, air usually decompresses into the neck, preventing physiologically tamponade and pneumothorax. Elevated pressure in the deep cervical fascia then favors dissection along blood vessels to other planes in the neck. Dissection of the free air into the pericardial space is a common complication of barotrauma in neonates, but is very rare in adults where the apposition of pericardial layers is very tight.5)
The most common cause of pneumomediastinum is alveolar rupture6). Alveolar rupture occurs in the presence of elevated intra-alveolar pressure or damage to alveolar walls. Causes of elevated alveolar pressure include airway obstruction (e.g., by mucous plugging in an asthmatic person or by a foreign body), mechanical ventilation (particularly with a large ventilatory volume or high end-expiration pressure), blunt, trauma, coughing, emesis or Valsalva maneuver (e.g., during parturition)7, 8). Causes of damage to alveolar walls include pneumonitis, emphysema, lung fibrosis and acute respiratory distress syndrome. Causes of pneumomediastinum would be associated with the use of heroin marijuana, cocaine or nitrous oxide9–11). Other causes of pneumomediastinum include trauma, gas producing infections in the head, neck and abdomen, and surgery in the upper digestive tract as well as dental surgery3).
Pneumopericardium is typically the result of blunt or penetrating trauma or recent heart surgery. However, in a patient on a ventilator, it may occur by the same mechanism as that which causes most cases of pneumomediastinum, that is, by gas dissecting medially from interstitial emphysema of the lung3). Higher pressure is required to cause pneumopericardium12). Gas probably enters the pericardium along the venous sheaths, in which the collagenous support of the pericardial reflections is weak12).
Most commonly, patients present with chest pain exacerbated by deep breath and cough13). They may experience dyspnea, dysphagia, neck and throat pain or dysphonia. Physical examination may show respiratory distress, neck crepitus, decreased cardiac dullness, Hamman’s sign (a mediastinal crunching sound that is synchronized with systole) or, rarely, signs of pericardial tamponade14, 15). Low grade fever is present in about one-third and mild leukocytosis in about one-half of cases16).
Posteroanterior chest radiographs typically reveal a radiolucency between the left heart border and the mediastinal pleura. Other findings may include “highlighting” of the aortic knob and the “continuous diaphragm sign”3). These structures are outlined by the radiolucent gas. However, almost 50% of cases will be missed by posteroanterior chest view17). Lateral chest examinations are more sensitive for identifying pneumomediastinum. Air is visualized most commonly in the retrosternal space18). It also looks like a lucent streak outlining the aorta or other mediastinal structures. Pneumopericardium is usually manifested as a single band of gas that may outline both left ventricle and right atrium. If there is enough air, pneumopericardium can completely surround the heart and create the halo sign3). A CT scan is more sensitive in detecting air than plain radiographs. Esophagogram should also be performed to detect the possible esophageal tear if emesis or retching was the precipitating event.
There are no pathognomic electrocardiographic changes in pneumomediastinum, although low voltage and axis shifts have been described19). Electrocardiographic changes are due to the presence of air interfering with electrical conduction.
Initial therapy should be directed at underlying disease processes. Analgesics, bed rest and treatment for coughing are appropriate. Breathing 100% oxygen will enhance reabsorption of the free air by increasing the gradient of nitrogen between the alveoli and the tissues. Pain typically resolves within 1 to 2 days, and follow-up chest radiograph within 12 to 24 hours is necessary to detect any progression or complications such as pneumothorax17, 20). The chest radiograph usually returns to normal within a week. If progression occurs, the patient may require a needle aspiration or chest tube placement20), but they are dangerous and provide only questionable benefit. In an adult with pneumopericardium, pericardial drainage should be performed only if there is hemodynamic embarrassment.21)
In conclusion, spontaneous pneumomediastinum and pneumopericardum is a rare disease that occurs in a young healthy adult without underlying cause. Absolute bed rest and a high concentration of oxygen supply were found to be a definite benefit.
REFERENCES
- 1.Yellin A, Gapany-Gapanavivius M, Lieberman Y. Spontaneous pneumomediastinum; Is it a cause of chest pain? Thorax. 1983;38:383–385. doi: 10.1136/thx.38.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Munsell WP. Pneumomediastinum: A report of 28 cases and a review of the literature. J Am Med Assoc. 1967;202:689–693. doi: 10.1001/jama.202.8.689. [DOI] [PubMed] [Google Scholar]
- 3.Bejvan SM, Godwin JD. Pneumomediastinum: Old signs and new signs. Am J Roentgenol. 1996;166:1041–1048. doi: 10.2214/ajr.166.5.8615238. [DOI] [PubMed] [Google Scholar]
- 4.Macklin CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum : clinical implications. Arch Intern Med. 1939;64:913–926. [Google Scholar]
- 5.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema: pathophysiology, diagnosis and management. Arch Intern Med. 1984;144:1447–1453. [PubMed] [Google Scholar]
- 6.Bratton SL, O’Rourke PP. Spontaneous pneumomediastinum. J Emerg Med. 1993;11:525–529. doi: 10.1016/0736-4679(93)90305-q. [DOI] [PubMed] [Google Scholar]
- 7.Rose WD, Veach JS, Tehranzdeh J. Spontaneous pneumomediasinum as a cause of neck pain, dysphagia and chest pain. Arch Intern Med. 1984;144:392–393. [PubMed] [Google Scholar]
- 8.Manco JC, Adler RH, Taheri SA. Pneumomediastinum, pneumothorax and subcutaneous emphysema following the measurement of maximal expiratory pressure in a normal subject. Chest. 1990;98:1530–1532. doi: 10.1378/chest.98.6.1530. [DOI] [PubMed] [Google Scholar]
- 9.Frekel MA, Lyons LL. Spontaneous pnemomediastinum : an unusual cause of sore throat. Postgrad Med. 1991;89:257–259. doi: 10.1080/00325481.1991.11700803. [DOI] [PubMed] [Google Scholar]
- 10.Mattox KL. Pneumomediastinum in heroin and marijuana users. JACEP. 1976;5:26–28. doi: 10.1016/s0361-1124(76)80162-1. [DOI] [PubMed] [Google Scholar]
- 11.Lipuma JP, Wellman J, Stern HP. Nitrous oxide : a new cause of pneumomediastinum. Radiology. 1982;145:602. doi: 10.1148/radiology.145.3.7146387. [DOI] [PubMed] [Google Scholar]
- 12.Mansfield PB, Granam CB, Beckwith JB, Hall DG, Sauvage LR. Pneumopericardium and pneumomediastinum in infants and children. J Pediatr Surg. 1973;8:691–699. doi: 10.1016/0022-3468(73)90408-9. [DOI] [PubMed] [Google Scholar]
- 13.Lee SK, Im JS, Cho NS. Clinical Evaluation of pneumomediastinum in Adult. Korean J Throac Cardiovasc Surg. 1995;28:1150–1154. [Google Scholar]
- 14.Gossage AR, Robertson PW. Spontaneous pneumomediastinum. Thorax. 1976;31:460–465. doi: 10.1136/thx.31.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh-Kelly C, Kelly KJ. Dysphonia: an unusual presentation of spontaneous pneumomediastinum. Pediatric Emerg Care. 1986;2:26–27. [PubMed] [Google Scholar]
- 16.Ralph-Edwards C, Pearson FG. A typical presentation of spontaneous pneumomediastinum. Ann Thorac Surg. 1994;58:1758–1760. doi: 10.1016/0003-4975(94)91683-7. [DOI] [PubMed] [Google Scholar]
- 17.Millard CE. Pneumomediastinum. Dis Chest. 1969;56:297–300. doi: 10.1378/chest.56.4.297. [DOI] [PubMed] [Google Scholar]
- 18.Kim SH, Im JG, Seo JB, Park JH, Yeon KM, Han MC. Spontaneous pneumomediastinum on CT : related condition and its clinical signification. J Korean Radiol Soc. 1998;38:459–462. [Google Scholar]
- 19.Littman D. Elecrocardiographic phenomena associated with spontaneous pneumomediastinum and mediastinal emphysema. Am J Med SCi. 1946;212:682–690. doi: 10.1097/00000441-194612000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Holmes KD, McGuirt WF. Spontaneous pneoumomediastinum : evaluation and treatment. J Fam Pract. 1990;31:422–429. [PubMed] [Google Scholar]
- 21.Cummings RG, Wesley RLR, Adam DH, Lowe JE. Pneumopericardium resulting in cardiac tamponade. Ann Thorac Surg. 1984;37:511–517. doi: 10.1016/s0003-4975(10)61146-0. [DOI] [PubMed] [Google Scholar]


