Introduction
Theories about health and aging have evolved beyond medical models of illness and disease to emphasize a more holistic process of health and wellbeing at older ages. For example, Lindau, Laumann, Levinson, & Waite (2003) conceptualize health broadly with the Interactive Biopsychosocial Model (IBM). This framework embraces (1) an orientation toward health rather than illness; (2) analytic capacity for outcomes of health or illness; (3) biophysical, psychocognitive, and social capital as equally important factors in an individual’s health endowment; (4) consideration of causality and feedback between various types of capital and health; (5) an understanding of individual health or illness that is embedded in the intimate dyad, the family, or other social networks; (6) interdependency of social and life course dynamics; and (7) the potential of capital inputs to act as assets or liabilities.
Consistent with the IBM’s proposals, current research shows that social connections affect and are affected by physical health, functionality, emotional health, and cognitive health, and have strong effects on longevity. The relationship between social ties and health unfolds over the entire life course, with unique implications in older adulthood (Charles & Mavandadi, 2003; Umberson, Crosnoe, & Reczek, 2010). Scholars propose that older adults’ social relationships moderate individual health outcomes by influencing behaviors, physiological function, cognitive function, and emotional regulation; providing access to health inputs; and even changing gene expression. While older adults’ social networks often include relatives, friends, and co-workers, they typically spend the most time with spouses and long-term partners so the characteristics of the dyad have a particularly important impact on health.
This paper highlights the various pathways through which social relationships affect the production of health at older ages. We focus in particular on the ways that changes in an individual’s social networks and partner relationships affect health and wellbeing during the last third of life. We address these aims by reviewing recent research from the National Social Life, Health, and Aging Project (NSHAP), a nationally representative, longitudinal study of aging in America. The detailed information about older adults’ network members, partners, and spouses, and innovative measures of physical, mental, functional, and cognitive health makes NSHAP especially well-suited to illuminating the production of health in social contexts.
NSHAP Methods and Data
Data for Wave 1 was collected in 2005 and 2006 from 3,005 individuals aged 57–85 (Waite, Laumann, Levinson, Lindau, & O’Muircheartaigh, 2014). Respondents participated in face-to-face interviews, biomeasure collection, and self-administered paper and pencil questionnaires in which they provided information on their demographic characteristics, social networks, physical health, sexual and intimate partnership histories, fertility and menopause, children and grandchildren, mental health, employment and finances, and religion.
Data collection for Wave 2 took place five years later in 2010 and 2011, and nearly 3,400 surviving respondents and their coresidential spouses and partners participated in this wave (Waite et al., 2014). To allow for longitudinal analysis of stability and change, most of the Wave 2 in-person questionnaire and biomeasure data collection remained unchanged from Wave 1. However, new items for Wave 2 include measures of pain and personality, new biomeasures such as cortisol, cholesterol, and hip circumference, a new actigraphy sub-study to measure sleep and activity cycles, new measures of sexuality, and measures of social network and partnership change. The release of Wave 2 data enables a study of how changes in social contexts can affect health.
Social Networks Shape Health
Scholars point to the importance of social networks to many aspects of older adulthood. To assess older adults’ social networks, NSHAP respondents were asked to name up to five confidants with whom they most often discussed important things. They were asked to identify each confidant and rate how close they felt to each of them. Respondents were further asked how often they interact with each confidant, as well as how frequently each confidant interacts with each of their other confidants. Wave 2 includes additional questions, such as the reason a respondent fell out of touch with a previously named network member, to measure changes in social networks (Cornwell et al., 2014).
The unique information on social networks in Wave 1 and the information on network change in Wave 2 allow researchers to investigate the mechanisms through which the social world affects health. Such research speaks directly to the Biopsychosocial Model of the embeddedness of the production of health, in the dyad, the social network, and the social context.
Recent findings from NSHAP show that social network characteristics, apart from simply its size, have profound effects on health outcomes. Shiovitz-Ezra and Litwin (2012) examine the relationship between network type and health behaviors. They identified five types of networks among the elderly: “Diverse” networks characterized by high sociability with family, friends, and organized groups; “Friends” networks characterized by a large number of friends; “Congregant” networks distinguished by frequent attendance at religious services; “Family” networks characterized by a large number of children; and “Restricted” networks distinguished by low sociability with few family or extra-familial ties. They show that older people embedded in Family and Restricted networks, the types with the fewest resources, were more likely than others to report alcohol abuse, physical inactivity, and less use of complementary and alternative medicine. The results are presented in Table 1. Shiovitz-Ezra and Litwin propose that people exposed to the control of a variety of social agents are more apt to experience positive pressure to adopt health-promoting behaviors, and more often receive informal sanctions that discourage health-damaging habits.
Table 1.
Associations Between Social Network Type and Health Related Behaviors from Shiovitz-Ezra & Litwin (2012).
| Alcohol Abuse1 OR (SE) [95% CI] |
Physical Activity1 OR (SE) [95% CI] |
Alternative Meds1 OR (SE) [95% CI] |
|
|---|---|---|---|
| Network types | |||
| Friends2 | |||
| Diverse | 1.40 (.38) [.82–2.39] | .91 (.19) [.61–1.39] | 1.43 (.28)+ [.98–2.10] |
| Congregant | 1.06 (.29) [.61–1.85] | .80 (.17) [.52–1.23] | .70 (.15)+ [.46–1.06] |
| Family | 1.71 (.44)* [1.02–2.86] | .64(.14)* [.42–.98] | .55 (.12)** [.36–.85] |
| Restricted | 1.76 (.44)* [1.07–2.87] | .77 (.15) [.52–1.13] | .78 (.15) [.54–1.13] |
| Lonely to some degree | |||
| No2 | |||
| Yes | 1.27 (.24) [.88–1.83] | .80 (.11) [.60–1.07] | 1.21 (.18) [.91–1.61] |
p<0.1,
p<0.05,
p<0.01,
p<0.001
Regressions are adjusted for age, gender, education, income, ethnicity, self-rated health, and difficulties with activities of daily living
Reference categories
Others have also found that network size is not the only factor that matters for health. In a study of hypertension management, York Cornwell and Waite (2012) find that having a large network is beneficial only if the individual is likely to discuss health with network members. The authors take advantage of self-reports of hypertension diagnosis and objective blood pressure readings in NSHAP to identify individuals with uncontrolled hypertension: those who have been diagnosed with hypertension and who also have high blood pressure (readings greater than 140/90 mm Hg). Table 2 shows the different hypertension categories identified in the study.
Table 2.
Hypertension Categories Derived from Self-Report and Blood Pressure from Cornwell, E. Y. and L. J. Waite (2012).
| Normal blood pressure (≤ 140/90 mmHg) | High blood pressure (> 140/90 mmHg)a | ||
|---|---|---|---|
| Self-report: Do you have hypertension? | No |
Non-hypertensive n = 687 (25.85%) |
Undiagnosed Hypertensive n = 445 (16.74%) |
| Yes |
Controlled Hypertensive n = 614 (23.10%) |
Uncontrolled Hypertensive n = 912 (34.31%) |
Individuals who had been diagnosed with diabetes were considered to have high blood pressure if their measurements exceeded 130/80 mm Hg.
Using multinomial logistic regression analyses, the authors find that larger networks are associated with lower chances of having uncontrolled hypertension—provided that network discusses health. The less likely the network is to have health discussions, the greater the risk that a large network is actually associated with worse health. Figure 1 displays the predicted probabilities of having uncontrolled hypertension by social network size and likelihood of health discussion. The probability of having uncontrolled hypertension decreases as network size increases for those who are very likely to discuss health with their network members (solid gray line). Conversely, the probability of having uncontrolled hypertension increases as network size increases among those not likely to discuss health with their networks (solid black line). These findings contradict the general hypothesis that having more social relationships is always beneficial. The authors suggest that when lines of communication about health are closed, relationships may present more costs than benefits. A lack of communication about health may also indicate tense, conflicted, or demanding network ties that bring additional stress for those suffering from chronic conditions. Thus, having a large social network that does not support positive health behaviors may be worse for an individual’s health than having a smaller but more resourceful or supportive network.
Figure 1.
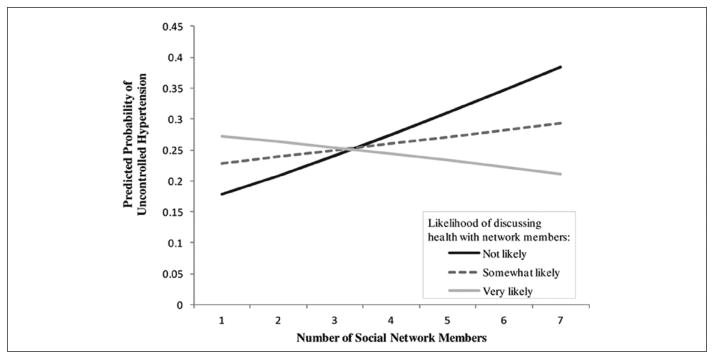
Predicted Probability of Uncontolled Hypertension According to Network Size and Health Discussion from Cornwell, E. Y. and L. J. Waite (2012).
Finally, some authors show that network position influences other outcomes in aging. Cornwell and Laumann (2011) find that about 25% of men in NSHAP experience “partner betweenness,” a situation in which a heterosexual man’s female partner has more frequent contact with his confidants than he does. Compared to men who do not experience partner betweenness, these men are 92% more likely to report erectile dysfunction. They suggest that network positions that afford independence and control over social resources are more consistent with traditional masculine roles and deviations from this situation undermine these roles and may therefore affect men’s sexual performance.
Clearly, these studies show that different characteristics of individuals’ social networks shape various components of health and well-being. However, networks are not static, especially among older adults, who are likely to lose family members, friends, and spouses as they age. The introduction of Wave 2 data enabled Cornwell and Laumann (2013) to assess how older adults’ social networks changed between 2005/2006 and 2010/2011. Respondents “lost” a network member if they named a person in Wave 1 but not in Wave 2. The most common reason respondents gave for why they did not name confidants again at Wave 2 had to do with geographic distance (either the respondent or the confidant moved, or it was determined that the confidant lived “too far away” from the respondent; 23.4% of all losses). Another common response was that the confidant died during the study period (17.1%). Otherwise, respondents sometimes reported that they were “still in touch” with the confidant but presumably not on the same level they had been at Wave 1 (15.3%), or that they just “drifted apart” (14.8%).
Table 3 shows the number of NSHAP respondents who lost and added network members between Waves 1 and 2. More respondents (37.9%) reported a net expansion of their networks than a net decrease (26.6%). The large numbers along the diagonal in Table 3 suggest “network turnover:” when respondents lost network members, they tended to add the same number of new ones. Of the 770 respondents who reported no net change in network size between waves, 621 (80.6%) reported some change in the people in their networks. Regardless of whether network size changed between waves, 81.8% of respondents named a confidant at Wave 2 who they had not named at Wave 1. And only 7% of respondents reported complete stability in their networks - no changes in network size or network members.
Table 3.
Matrix of the Number of Respondents Who Lost and Added Confidants between Waves 1 and 2 from Cornwell & Laumann (2013).
| Number of New Confidants at W2 | |||||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | ||
|
|
|||||||
| Number of W1 Confidants Lost | 0 | 149 | 109 | 117 | 61 | 34 | 0 |
| 1 | 104 | 187 | 122 | 87 | 54 | 12 | |
| 2 | 76 | 105 | 223 | 71 | 47 | 17 | |
| 3 | 38 | 54 | 71 | 128 | 39 | 13 | |
| 4 | 22 | 18 | 34 | 25 | 63 | 12 | |
| 5 | 0 | 6 | 8 | 7 | 7 | 20 | |
|
|
|||||||
Further, Cornwell and Laumann find that older adults who cultivate new ties appear to enjoy health benefits: as the number of confidants added at Wave 2 increases, the risk of functional impairment declines; the odds of reporting better health increase; and the probabilities of reporting depressive symptomology decrease. The authors hypothesize that cultivating new network members may increase levels of physical and cognitive activity to an extent that benefits immune function and cardiovascular health. Or, the addition of new network members may boost self-esteem and reduce depression, which can have a variety of downstream health benefits.
Marriage Shapes Health
While connections with social networks members are important for successful aging, the Biopsychosocial Model suggests that relationships with partners and spouses will have the most impact on well-being (Lindau, Laumann, Levinson, & Waite, 2003). NSHAP collects highly detailed information about older adults’ marital, cohabitational, and sexual partnerships. Respondents are asked about their partners’ mental and physical health, relationship quality, the level of support and demands they receive from their partners, and the dyad’s sexual activity. Wave 2 includes new questions about changes in marital and partnership status in order to understand widowhood and relationship formation at older ages.
Research using NSHAP data shows that marriage matters for one’s health, with damaging effects from marital loss. In a study of C-reactive protein (CRP), an indicator of chronic or acute inflammation, Sbarra (2009) showed that CRP levels were elevated in divorced and widowed men but not in married men, documenting a possible physiological pathway through which being married and marital loss alter health and risk of illness. Mean levels of CRP for each sex-marital status group and the results from statistical contrasts are presented in Table 4. Sbarra’s findings indicate that, for men, marital status may have a direct effect on CRP levels that remains significant after accounting for a variety of measures of health behavior and psychological stress. He proposes that gendered family roles provide married men a unique context in which they are protected against the ups and downs of daily life relative to their unmarried counterparts or to women in general. Whereas men receive substantial benefits from being married, women shoulder more emotional and caregiving burdens, typically, than men do, tempering the benefits they receive. So, for women, marital loss is not associated with higher levels of inflammation compared to marriage, as it is for men.
Table 4.
Mean CRP Levels and Contrasts by Sex and Marital Status from Sbarra (2009)
| Group (Sample Size) | Mean CRP Level, mg/L (SD) | Contrast 1 (C1) | Contrast 2 (C2) | Contrast 3 (C3) |
|---|---|---|---|---|
| Married men (662) | 2.16(2.04) | 1/4 | −2/3 | 0 |
| Unmarried men (423) | 2.72 (2.49) | −3/4 | 0 | 0 |
| Married women (176) | 2.61 (2.28) | 1/4 | 1/3 | −1/2 |
| Unmarried women (454) | 2.79 (2.34) | 1/4 | 1/3 | 1/2 |
Comparisons computed using log-transformed CRP. C1 compares unmarried men with all other participants. C2 Compares married men with women. C3 compares married and unmarried women.
Other studies also show a link between marriage and biological processes. McFarland, Hayward, and Brown (2013) find that marital biography - transitions into and out of marriage, age at first marriage, and marital exposure - is associated with cardiovascular, metabolic, and chronic inflammation risk. They defined five mutually exclusive marital status categories: continuously married, remarried 1 dissolution, remarried 2+ dissolutions, previously married 1 dissolution, and previously married 2+ dissolutions; measured the cumulative length of time a respondent was married since his or her first marriage; and determined a person’s age at first marriage. The authors found evidence to suggest that the relationship between marital biography and biological risk differs for men and women, and depends on the dimension of marital biography and biological risk factor being examined. For example, women who had been married for a longer cumulative length of time had lower cardiovascular risk than women who had been married for shorter periods of time. Further, women who experienced multiple marital dissolutions were at higher metabolic risk than continuously married women. Among men, those who married at younger ages were more likely to experience chronic inflammation than those who married at later ages.
Their findings suggest that marital biography gets under the skin through different mechanisms and into different bodily systems over different time scales. They suggest that marital exposure may be especially important for cardiovascular risk because cardiovascular health develops slowly over time. In contrast, marital transitions influence the metabolic system over relatively short periods of time since marital transitions may prompt fairly rapid changes in diet and physical activity.
Though being married is associated with many health benefits, many scholars show that the quality of the marital relationship often matters more for well-being than being married in itself. For example, Bookwala (2011) shows that older adults with poor vision were less likely to be depressed and suffer from restrictions in their daily lives if they were happily married and could count on their spouse to help. In another study, Warner and Adams (2012) find that functional impairment is associated with feelings of loneliness in older adults, and that nonmarital and marital relations have independent effects on loneliness. However, only the marital relationship moderated the effect of disablement on loneliness, and supportive non-spousal relationships did not counteract the negative effects of a weak marital relationship for functionally impaired older adults: while physically-disabled older adults in higher-quality marriages were buffered from loneliness, supportive non-martial relationships did not offset elevated loneliness among those in low-quality marriages. The Biopsychosocial Model points to the dyad as a site of health production; these results suggest that an elaboration of this model should account for the quality of the dyadic relationship.
While it is evident that the quality of a marriage matters for health, information about the marital relationship from the perspective of both members of the couple is rarely available from a nationally representative sample. The addition of partner interviews in Wave 2 of NSHAP offers a unique opportunity to examine shared activities and relationship quality for older adults in married or partnered relationships from the independent perspective of each of the partners.
Kim and Waite (2014) use the new detailed information about partnered men and women and their relationships in Wave 2 to construct scales of positive relationship quality, negative relationship quality, and shared activity, with the goal of enabling researchers to look at changes in relationships over a five-year period that could be used to predict various health outcomes. In constructing these scales they find that husbands and male cohabitors score higher on both positive and negative relationship quality than do wives and cohabiting women, suggesting that a greater share of older men than of older women experience ambivalent feelings toward their spouse or partner. Women reported significantly lower scores than men, on average, on both positive and negative relationship quality, which suggests that at least on the dimensions of the relationship measured in NSHAP, more women than men have relationships of indifferent quality, with relatively low costs and relatively low benefits. Across age categories, the authors find that women’s positive relationship quality scores decline and negative relationship quality scores increase with age while men’s positive and negative relationship quality scores fluctuate with age: older women have worse relationships than younger women, and older men have better relationships than younger men. Surprisingly, Kim and Waite find that women have significantly lower scores than men on the shared activity scale even though the shared activity scale is a measure of joint activities that cannot be achieved without both partners. Further analyses show that this gender difference stems from differences in sexual activity: partnered sexual activity declines with age, and men tend to have younger spouses while women tend to have older spouses. When analyzing general activities without sexual activities, they found no significant differences in general activities between men and women or among age groups. The distribution of relationship quality and shared activity scale sores are shown in Table 5.
Table 5.
Mean and Standard Deviation for Relationship Quality and Shared Activity Scale from Kim & Waite (2014).
| All Partnered
|
All Dyads
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Husband
|
Wife
|
Husband
|
Wife
|
|||||
| Ma | SD | Ma | SD | Ma | SD | Ma | SD | |
| Relationship Quality | ||||||||
| Positive dimension | ||||||||
| Overall | 0.06 | 0.67 | −0.07 c | 0.81 | 0.07 | 0.64 | −0.05 c | 0.77 |
| Age groupb | ||||||||
| 62–69 | 0.07 | 0.59 | −0.03 | 0.74 | 0.09 | 0.55 | −0.01 | 0.72 |
| 70–79 | 0.04 | 0.74 | −0.08 c | 0.83 | 0.06 | 0.66 | −0.09 c | 0.78 |
| 80–90 | 0.05 | 0.77 | −0.22 c | 1.06 | 0.09 | 0.72 | −0.14 c | 0.85 |
| Negative dimension | ||||||||
| Overall | 0.05 | 0.78 | −0.12 c | 0.86 | 0.07 | 0.80 | −0.06 c | 0.88 |
| Age groupb | ||||||||
| 62–69 | 0.04 | 0.69 | −0.17 c | 0.79 | 0.03 | 0.69 | −0.10 c | 0.82 |
| 70–79 | 0.07 | 0.85 | −0.05 | 0.93 | 0.12 | 0.86 | −0.02 | 0.93 |
| 80–90 | 0.01 | 0.91 | −0.05 | 0.97 | 0.05 | 0.99 | 0.03 | 0.94 |
| Shared Activity | ||||||||
| Overall | 0.08 | 0.64 | −0.02 c | 0.67 | 0.08 | 0.66 | −0.01 c | 0.68 |
| Age groupb | ||||||||
| 62–69 | 0.16 | 0.56 | 0.06 | 0.60 | 0.17 | 0.56 | 0.09 | 0.63 |
| 70–79 | 0.06 | 0.69 | −0.10 c, d | 0.74 | 0.04 d | 0.71 | −0.12 c, d | 0.73 |
| 80–90 | −0.10 d | 0.75 | −0.20 c, d | 0.72 | −0.09 d | 0.78 | −0.10 d | 0.73 |
126 women and 11 men are age 61 and under, and 4 men are age 91 and older. These cases were excluded in age group comparisons.
Significant difference between men and women (at p = 0.05)
Significantly different from age 62–69 group (at p = 0.05)
Health Shapes Social Networks and Marriage
At the same time that the social world gets under the skin to affect health and well-being, an individual’s health endowment (Lindau, Laumann, Levinson, & Waite, 2003) - one’s genetic makeup and physiology, intelligence and emotional well-being, as well as other factors - affects the social relationships one has. For example, Cornwell’s (2009) analyses of older adults’ egocentric social networks suggest that people who have poorer cognitive health may be less likely to span structural holes, the gap between two networks that inhibits the flow of information. It is possible that maintaining bridging positions - positions that close structural holes - may be more difficult for those who have cognitive impairments, or that cognitively impaired individuals may have more difficulty recognizing (and thus strategically using) bridges in their networks.
In addition to influencing social network position, health colors a marriage. Utilizing data on both partners in 955 marital and cohabitational dyads, Iveniuk et al. (2014) find a negative association between poor health and negative personality traits, and marital quality. A person’s own health and personality affect his or her view of the marriage, but the health and personality of one’s spouse also affect how a person views the marriage. The authors also show noteworthy gender differences between men and women in the associations between individual characteristics and levels of marital conflict. Wives with husbands in fair or poor physical health were more likely to report high levels of marital conflict but the reverse was not true. Further, wives reported more conflict when their husbands scored high on the personality traits Neuroticism and Extraversion, and low on Positivity, but wives’ personality had no effect on husbands’ assessments of marital quality. The authors conclude that both health and personality traits operate on separate, gendered pathways in the production of good marital quality.
Galinsky and Waite (2013) identify other pathways between health and marital quality in their analysis of marital dyads in NSHAP. They propose that poor physical health affects the psychological well-being of an individual and his or her spouse at the same time that it affects the sexual behavior of the couple. These subsequently affect marital quality directly and moderate the effect of physical health on marital quality. This conceptual model is presented in Figure 2. Their findings support this model: one’s own fair or poor physical health is linked to lower positive and higher negative marital quality; and spouses’ health is linked to positive marital quality. Further, both partners’ mental health and more frequent sex mediate the relationship between own and partner’s health and marital quality. Their findings point to the importance of maintaining sexual and emotional health in order to protect marital quality in later life.
Figure 2.
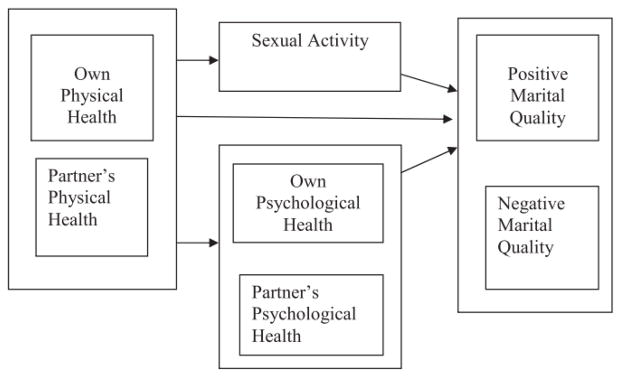
Conceptual Model of the Associations Among Physical Health, Sexual Activity, Psychological Health, and Marital Quality from Galinsky & Waite (2013)
Since sexuality is an important factor in determining marital quality, and marital quality affects health and well-being, it is crucial that researchers study sexuality to understand successful aging. Wave 2 of NSHAP includes new measures of sexual interest and behavior, new measures of the context of sexual experience, and measures of the frequency and appeal of physical contact. Galinsky, McClintock, & Waite (2014) describe the new measures and compare the distributions of each across gender and age groups (Table 6). They find that sexual activity declines with age, but that very few partnered older adults say they rarely or never agree to sex when their partner wants to have sex. An analysis of novel measures of physical contact shows that most men and most women report that light touching, hugging, and cuddling appeal to them. They argue that non-sexual and other caring behaviors are important for making later sexual interactions pleasurable. In fact, they report that among those who had sex in the past year, over 20% of women and nearly a quarter of men say that the amount of foreplay was less than they would have liked. These new sexuality items in Wave 2 of NSHAP offer the opportunity to more precisely and richly characterize sexual motivation in older adulthood and to examine how the context of sexual experience and the non-sexual aspects of physical intimacy are connected to sexual behavior, enjoyment and problems.
Table 6.
Distributions of NSHAP Sexuality Questions, New in Wave 2 from Galinsky, McClintock & Waite (2014)
| WAVE 2 Age Eligible Participants | Mode | Men | Women | Total 62–90 % | ||||
|---|---|---|---|---|---|---|---|---|
| 62–69 % | 70–79 % | 80–90 % | 62–69 % | 70–79 % | 80–90 % | |||
| (1) When you had sex with [current/recent partner] in the last 12 months, how often did your partner touch your genitals with (his/her) hands? | CAPI | |||||||
| Always | 42.2 | 37.3 | 35.1 | 50.0 | 41.0 | 43.2 | 42.6 | |
| Usually | 28.4 | 27.4 | 22.0 | 27.0 | 23.0 | 24.4 | 26.6 | |
| Sometimes | 22.6 | 23.0 | 25.4 | 17.0 | 24.7 | 16.3 | 21.6 | |
| Rarely | 4.9 | 7.5 | 8.6 | 3.7 | 6.9 | 10.6 | 5.8 | |
| Never | 1.2 | 5.0 | 9.4 | 2.0 | 4.6 | 5.4 | 3.4 | |
| Mean | 4.0 | 3.8 | 3.6 | 4.2 | 3.9 | 3.9 | 4.0 | |
| Number of observations | 383 | 309 | 104 | 313 | 197 | 59 | 1365 | |
| (2) How often do you find someone you don’t know such as people in movies, television, books, or strangers on the street physically attractive? | CAPI* | |||||||
| Every day | 24.2 | 18.8 | 15.3 | 7.7 | 8.2 | 6.1 | 13.8 | |
| Several times a week | 23.9 | 22.6 | 10.8 | 12.7 | 8.5 | 7.1 | 15.3 | |
| Once a week | 19.6 | 17.1 | 17.7 | 13.6 | 14.0 | 9.2 | 15.5 | |
| Less than once a week | 22.4 | 26.0 | 23.8 | 42.7 | 36.2 | 27.3 | 30.9 | |
| Never | 9.9 | 15.4 | 32.5 | 23.3 | 33.2 | 50.5 | 24.6 | |
| Mean | 3.3 | 3.0 | 2.5 | 2.4 | 2.2 | 1.9 | 2.6 | |
| Number of observations | 550 | 584 | 324 | 634 | 619 | 379 | 3090 | |
| (3) In the past month, how much effort have you made to make yourself look attractive for your partner? | CAPI | |||||||
| A great deal of effort | 5.6 | 4.1 | 3.3 | 15.1 | 11.6 | 9.0 | 8.4 | |
| A lot of effort | 19.0 | 18.0 | 16.8 | 32.7 | 26.5 | 24.7 | 23.3 | |
| A moderate amount of effort | 48.6 | 53.3 | 52.1 | 40.8 | 48.3 | 48.4 | 47.9 | |
| Some effort | 19.7 | 17.9 | 23.1 | 8.5 | 9.6 | 13.3 | 15.2 | |
| No effort | 7.2 | 6.8 | 4.8 | 2.9 | 4.1 | 4.6 | 5.3 | |
| Mean | 3.0 | 2.9 | 2.9 | 3.5 | 3.3 | 3.2 | 3.1 | |
| Number of observations | 415 | 423 | 194 | 416 | 325 | 113 | 1886 | |
| (4) In the past month, how much effort have you made to make yourself look attractive for someone you find attractive? | LBQ** | |||||||
| A great deal of effort | 4.3 | 9.3 | 4.8 | 5.3 | 5.5 | 2.9 | 5.2 | |
| A lot of effort | 32.9 | 12.1 | 8.7 | 6.1 | 11.0 | 8.2 | 11.5 | |
| A moderate amount of effort | 28.9 | 30.4 | 34.0 | 31.0 | 27.9 | 23.0 | 28.6 | |
| Some effort | 22.7 | 30.1 | 15.5 | 19.3 | 17.8 | 17.6 | 19.9 | |
| No effort | 11.3 | 18.2 | 37.1 | 38.2 | 37.8 | 48.3 | 34.7 | |
| Mean | 3.0 | 2.6 | 2.3 | 2.2 | 2.3 | 2.0 | 2.3 | |
| Number of observations | 64 | 99 | 87 | 150 | 219 | 196 | 815 | |
| (5) When your partner wants to have sex with you, how often do you agree? | CAPI | |||||||
| Always | 61.3 | 53.4 | 42.0 | 34.2 | 29.9 | 26.8 | 45.4 | |
| Usually | 19.6 | 15.4 | 11.8 | 32.1 | 22.2 | 21.0 | 21.6 | |
| Sometimes | 6.4 | 4.5 | 6.7 | 15.5 | 14.8 | 5.8 | 9.4 | |
| Rarely | 2.8 | 2.4 | 1.6 | 2.9 | 3.2 | 2.4 | 2.7 | |
| Never | 3.9 | 8.4 | 13.4 | 5.0 | 9.0 | 17.0 | 7.2 | |
| If volunteered: My partner has not wanted to have sex with me in the past 12 months | 5.9 | 15.6 | 24.5 | 10.4 | 21.0 | 27.2 | 13.8 | |
| Mean | 4.4 | 4.2 | 3.9 | 4.0 | 3.8 | 3.5 | 4.1 | |
| Number of observations | 457 | 398 | 165 | 418 | 270 | 93 | 2139 | |
| (6) During the past 12 months, when you had sex, was the amount of time you and your partner spent kissing, hugging, and touching before having vaginal intercourse: | LBQ | |||||||
| Much more often than you would like | 1.1 | 1.0 | 0.4 | 0.6 | 0.7 | 0.0 | 0.8 | |
| Somewhat more often than you would like | 1.4 | 1.1 | 0.4 | 2.9 | 0.0 | 0.0 | 1.4 | |
| About as often as you would like | 53.8 | 45.9 | 35.6 | 48.2 | 44.4 | 25.8 | 46.9 | |
| Somewhat less often than you would like | 10.6 | 5.3 | 5.7 | 11.6 | 4.8 | 1.2 | 8.2 | |
| Much less often than you would like | 10.0 | 7.7 | 5.0 | 4.5 | 4.0 | 0.0 | 6.5 | |
| I have not had vaginal intercourse in the past 12 months | 23.1 | 39.1 | 53.0 | 32.2 | 46.1 | 73.0 | 36.3 | |
| Mean | 2.6 | 2.7 | 2.7 | 2.8 | 2.8 | 3.0 | 2.7 | |
| Number of observations | 389 | 377 | 155 | 380 | 262 | 88 | 1651 | |
| (7) For some people, their sexual enjoyment is affected by non-sexual things that their partner does before having sex, such as helping out, compliments or sharing activities. For others it is not important at all. Given how important such things are for your enjoyment of sex, how often did they happen during the past 12 months? | LBQ | |||||||
| Much more often than you would like | 1.0 | 1.9 | 4.5 | 1.5 | 0.4 | 0.0 | 1.5 | |
| Somewhat more often than you would like | 3.8 | 1.6 | 3.8 | 2.6 | 1.7 | 0.0 | 2.6 | |
| About as often as you would like | 59.3 | 54.1 | 43.1 | 56.4 | 57.8 | 51.8 | 55.8 | |
| Somewhat less often than you would like | 16.4 | 15.1 | 19.8 | 18.6 | 14.5 | 7.0 | 16.4 | |
| Much less often than you would like | 19.6 | 27.3 | 28.8 | 20.9 | 25.7 | 41.3 | 23.7 | |
| Mean | 2.5 | 2.4 | 2.4 | 2.5 | 2.4 | 2.1 | 2.4 | |
| Number of observations | 387 | 371 | 143 | 368 | 237 | 63 | 1569 | |
| (8) To what extent do you feel your sex life is lacking in quality? | LBQ | |||||||
| Extremely lacking in quality | 20.2 | 28.7 | 25.4 | 21.6 | 24.0 | 26.8 | 23.7 | |
| Moderately lacking in quality | 18.4 | 14.0 | 15.8 | 15.6 | 9.9 | 7.5 | 14.6 | |
| Slightly lacking in quality | 26.3 | 21.6 | 22.0 | 20.9 | 17.2 | 9.0 | 21.2 | |
| Not at all lacking in quality | 35.1 | 35.6 | 36.9 | 42.0 | 49.2 | 56.7 | 40.5 | |
| Mean | 2.2 | 2.4 | 2.3 | 2.2 | 2.1 | 2.0 | 2.2 | |
| Number of observations | 449 | 454 | 205 | 464 | 372 | 154 | 2098 | |
| (9) How appealing or pleasant do you find the following ways of being touched? Being touched lightly, such as someone putting a hand on your arm. | LBQ | |||||||
| Very appealing | 35.6 | 39.1 | 26.9 | 46.7 | 39.7 | 32.7 | 38.5 | |
| Somewhat appealing | 51.3 | 48.2 | 55.7 | 42.5 | 48.3 | 50.0 | 48.4 | |
| Not appealing | 11.2 | 10.6 | 12.2 | 6.8 | 9.3 | 13.6 | 10.0 | |
| Not at all appealing | 1.9 | 2.2 | 5.2 | 4.1 | 2.7 | 3.7 | 3.1 | |
| Mean | 3.2 | 3.2 | 3.0 | 3.3 | 3.3 | 3.1 | 3.2 | |
| Number of observations | 482 | 521 | 282 | 571 | 553 | 319 | 2728 | |
| (10) How appealing or pleasant do you find the following ways of being touched? Hugging. | LBQ | |||||||
| Very appealing | 43.7 | 46.9 | 39.8 | 61.6 | 49.1 | 38.2 | 48.6 | |
| Somewhat appealing | 48.9 | 45.0 | 49.4 | 33.3 | 44.0 | 48.7 | 43.7 | |
| Not appealing | 6.0 | 6.6 | 7.1 | 4.5 | 4.8 | 9.5 | 6.0 | |
| Not at all appealing | 1.4 | 1.4 | 3.8 | 0.7 | 2.2 | 3.5 | 1.8 | |
| Mean | 3.3 | 3.4 | 3.3 | 3.6 | 3.4 | 3.2 | 3.4 | |
| Number of observations | 483 | 523 | 282 | 573 | 553 | 321 | 2735 | |
| (11) How appealing or pleasant do you find the following ways of being touched? Cuddling. | LBQ | |||||||
| Very appealing | 41.7 | 41.1 | 21.3 | 46.7 | 29.3 | 14.4 | 35.9 | |
| Somewhat appealing | 39.7 | 38.5 | 44.7 | 35.1 | 40.3 | 29.5 | 37.9 | |
| Not appealing | 16.8 | 17.4 | 26.0 | 14.4 | 22.3 | 40.2 | 20.6 | |
| Not at all appealing | 1.8 | 3.1 | 8.1 | 3.8 | 8.1 | 15.9 | 5.7 | |
| Mean | 3.2 | 3.2 | 2.8 | 3.2 | 2.9 | 2.4 | 3.0 | |
| Number of observations | 478 | 518 | 275 | 569 | 547 | 315 | 2702 | |
| (12) How appealing or pleasant do you find the following ways of being touched? Sexual Touching. | LBQ | |||||||
| Very appealing | 52.8 | 44.2 | 23.4 | 29.0 | 17.5 | 7.2 | 31.9 | |
| Somewhat appealing | 33.7 | 28.1 | 34.8 | 37.7 | 26.2 | 14.5 | 30.4 | |
| Not appealing | 6.9 | 18.5 | 23.4 | 17.7 | 25.6 | 19.1 | 17.7 | |
| Not at all appealing | 6.6 | 9.3 | 18.5 | 15.6 | 30.7 | 59.2 | 20.0 | |
| Mean | 3.3 | 3.1 | 2.6 | 2.8 | 2.3 | 1.7 | 2.7 | |
| Number of observations | 468 | 508 | 269 | 548 | 530 | 302 | 2625 | |
| (13) How often have you and your partner shared caring touch, such as a hug, sitting or lying cuddled up, a neck rub or holding hands? | LBQ | |||||||
| Many times a day | 13.9 | 12.8 | 10.7 | 17.6 | 13.6 | 13.0 | 14.2 | |
| A few times a day | 23.4 | 24.6 | 26.5 | 23.3 | 26.1 | 27.2 | 24.9 | |
| About once a day | 13.6 | 18.3 | 22.1 | 16.2 | 18.3 | 13.8 | 16.7 | |
| Several times a week | 22.0 | 20.8 | 17.5 | 17.5 | 10.9 | 17.2 | 18.4 | |
| About once a week | 11.6 | 9.5 | 13.1 | 7.7 | 12.3 | 9.4 | 10.4 | |
| About once a month or less | 12.8 | 10.7 | 7.1 | 9.4 | 10.4 | 11.1 | 10.6 | |
| Never | 2.8 | 3.4 | 3.0 | 6.3 | 8.5 | 8.2 | 4.9 | |
| Mean | 4.6 | 4.6 | 4.7 | 4.7 | 4.5 | 4.5 | 4.6 | |
| Number of observations | 414 | 419 | 193 | 414 | 321 | 105 | 1866 | |
| (14) Other than your partner, how often have you and a person, such as a friend, grandchild or another adult, shared a caring touch, such as a greeting hug, a touch on the arm, or a neck rub? | LBQ | |||||||
| Many times a day | 3.2 | 4.2 | 2.2 | 11.1 | 8.0 | 3.0 | 6.0 | |
| A few times a day | 6.2 | 8.5 | 5.8 | 8.7 | 9.5 | 4.3 | 7.6 | |
| About once a day | 8.6 | 7.9 | 5.5 | 10.4 | 9.3 | 9.0 | 8.8 | |
| Several times a week | 21.6 | 25.5 | 21.8 | 33.3 | 27.5 | 26.7 | 26.7 | |
| About once a week | 27.0 | 18.4 | 28.8 | 22.3 | 27.9 | 30.0 | 25.0 | |
| About once a month or less | 29.3 | 25.7 | 28.3 | 12.3 | 15.6 | 20.1 | 21.1 | |
| Never | 4.1 | 9.7 | 7.5 | 2.0 | 2.3 | 6.9 | 4.8 | |
| Mean | 3.3 | 3.4 | 3.2 | 4.1 | 3.9 | 3.4 | 3.6 | |
| Number of observations | 478 | 520 | 285 | 572 | 559 | 311 | 2725 | |
| (15) How often have you pet, stroked, touched, or slept next to a cat, dog, or other pet? | LBQ | |||||||
| Many times a day | 16.7 | 15.8 | 9.6 | 28.3 | 28.6 | 13.1 | 20.5 | |
| A few times a day | 18.1 | 9.5 | 7.5 | 11.3 | 8.1 | 10.0 | 11.4 | |
| About once a day | 11.8 | 5.6 | 9.0 | 6.0 | 5.0 | 7.0 | 7.4 | |
| Several times a week | 5.2 | 6.2 | 6.5 | 4.8 | 3.9 | 4.5 | 5.1 | |
| About once a week | 5.6 | 3.7 | 3.1 | 4.3 | 5.1 | 4.6 | 4.6 | |
| About once a month or less | 8.5 | 13.8 | 7.9 | 11.2 | 8.1 | 10.7 | 10.1 | |
| Never | 34.1 | 45.5 | 56.5 | 34.2 | 41.2 | 50.1 | 41.0 | |
| Mean | 3.7 | 3.0 | 2.6 | 3.8 | 3.6 | 2.9 | 3.4 | |
| Number of observations | 481 | 524 | 282 | 565 | 555 | 315 | 2722 | |
Computer Assisted Personal Interview (CAPI)
Leave Behind Questionnaire (LBQ)
Conclusion
Research using NSHAP data both confirms and elaborates the Interactive Biopsychosocial Model, showing that older adults’ social networks and marriages matter for their health and how they do so. More resource-rich networks promote good health and protect against risky health behaviors (Cornwell & Waite, 2012; Shiovitz-Ezra & Litwin, 2012), and changes in networks can change health outcomes (Cornwell & Laumann, 2013). The marital relationship exerts a unique influence on health, offering protection from adverse physiological health states (Sbarra, 2009; McFarland, Hayward, and Brown, 2013), and buffering the negative emotional consequences of disablement and functional decline, especially if the marriage is good (Bookwala, 2011; Warner & Adams, 2012).
At the same time, health affects social relationships. Those with better cognitive function may be better able to manage their networks (Cornwell, 2009). Physical and psychological health, as well as personality traits and the dyad’s sexual behavior, affect marital quality (Iveniuk, et al, 2014; Galinsky & Waite, 2013). Aging is a dynamic process, and the detailed measures on social contexts and health at older ages in NSHAP Wave 2 allow us to capture the nuances of this process over time.
References
- Bookwala J. Marital quality as a moderator of the effects of poor vision on quality of life among older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2011;66(5):605–616. doi: 10.1093/geronb/gbr091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, Mavandadi S. Relationships and health across the life span. In: Lang F, Fingerman K, editors. Growing together: Personal relationships across the life span. New York: Cambridge University Press; 2003. pp. 240–267. [Google Scholar]
- Cornwell B. Good health and the bridging of structural holes. Social Networks. 2009;31(1):92–103. doi: 10.1016/j.socnet.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, Laumann EO. Network position and sexual dysfunction: Implications of partner betweenness for men. American Journal of Sociology. 2011;117(1):172–208. doi: 10.1086/661079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, Laumann EO. The health benefits of network growth: New evidence from a national survey of older adults. Social Science & Medicine. 2013 doi: 10.1016/j.socscimed.2013.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, et al. Assessment of social network change in a national longitudinal survey. The Journals of Gerontology: Social Sciences. 2014 doi: 10.1093/geronb/gbu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galinsky A, McClintock MK, Waite LJ. Sexuality and physical contact in NSHAP wave 2. Journals of Gerontology: Social Sciences. 2014 doi: 10.1093/geronb/gbu072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galinsky AM, Waite LJ. Sexual activity and psychological health as mediators of the relationship between physical health and marital quality. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2013 doi: 10.1093/geronb/gbt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iveniuk J, Waite LJ, Laumann E, McClintock MK, Tiedt AD. Marital conflict in older couples: Positivity, personality, and health. Journal of Marriage and Family. 2014;76(1):130–144. doi: 10.1111/jomf.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Waite L. Relationship quality and shared activity in marital and cohabiting dyads in the National Social Life, Health and Aging Project, wave 2. Journals of Gerontology: Social Sciences. 2014 doi: 10.1093/geronb/gbu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindau ST, Laumann EO, Levinson W, Waite LJ. Synthesis of scientific disciplines in pursuit of health: The Interactive Biopsychosocial Model. Perspectives in Biology and Medicine. 2003;46:S74–S86. doi: 10.1353/pbm.2003.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland MJ, Hayward MD, Brown D. I’ve got you under my skin: Marital biography and biological risk. Journal of Marriage and Family. 2013;75:363–380. doi: 10.1111/jomf.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sbarra DA. Marriage protects men from clinically meaningful elevations in C-reactive protein: Results from the National Social Life, Health, and Aging Project (NSHAP) Psychosomatic Medicine. 2009;71(8):828–835. doi: 10.1097/PSY.0b013e3181b4c4f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiovitz-Ezra S, Litwin H. Social network type and health-related behaviors: Evidence from an American national survey. Social Science & Medicine. 2012;75(5):901–904. doi: 10.1016/j.socscimed.2012.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite LJ, Laumann EO, Levinson W, Lindau ST, O’Muircheartaigh CA. National Social Life, Health, and Aging Project (NSHAP): Wave 1. ICPSR20541-v6. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2014. Apr 30, [DOI] [Google Scholar]
- Waite LJ, Cagney K, Dale W, Huang E, Laumann EO, McClintock M, Cornwell B. National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection. ICPSR34921-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2014. Apr 29, [DOI] [Google Scholar]
- Warner DF, Adams SA. Widening the social context of disablement among married older adults: Considering the role of nonmarital relationships for loneliness. Social Science Research. 2012;41(6):1529–1545. doi: 10.1016/j.ssresearch.2012.05.018. [DOI] [PubMed] [Google Scholar]
- York Cornwell E, Waite LJ. Social network resources and management of hypertension. Journal of Health and Social Behavior. 2012;53(2):215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]


