Abstract
Objectives
Mutation of p53 may play a role in manifestation of rheumatoid arthritis synovium, but several studies on p53 expression in synovial tissues of rheumatoid arthritis showed conflicting results. We investigated the amount and pattern of p53 positive cells in rheumatoid arthritis synovium, in comparison with osteoarthritis synovium, by using immunohistochemistry with two other monoclonal antibodies for p53.
Methods
Synovial tissues from 9 patients with rheumatoid arthritis and 5 patients with osteoarthritis were examined for p53 expression by immunohistochemistry with 2 monoclonal antibodies for p53, DO-1 and DO-7. Histologic features of inflammation were also scored and compared with p53 expression.
Results
There was no significant difference between inflammatory scores in both groups. In the synovial tissues of rheumatoid arthritis patients, p53 positive cells were detected in 3 out of 9 samples(33%) and p53 expressions were restricted to inflammatory mononuclear cells, but synovial lining cells, subsynovial fibroblast-like cells and vascular endothelial cells were p53 negative. p53 expressions in osteoarthritis synovial tissues as control were observed in 2 out of 5 samples(40%) and the amount and pattern of p53 positive cells were comparable to those seen in rheumatoid arthritis synovial tissues. There was no demonstrable correlation between the synovial tissues of both groups with respect to inflammation scores and expression of p53 protein.
Conclusion
Our findings suggest that altered p53 expression may not play a significant role in the manifestation of rheumatoid arthritis synovium. However these data need to be strengthened by increasing the number of samples and molecular biology approaches.
Keywords: Rheumatoid arthritis, Synovium, p53
INTRODUCTION
Rheumatoid arthritis is characterized by hyperplasia of synovial lining cells, excessive infiltration of mononuclear cells and extensive destruction of the articular cartilage1), and this abnormal proliferation of synovial cells is an important event in the pathophysiology of rheumatoid arthritis. Rheumatoid arthritis synovium shows aggressive invasiveness of rheumatoid pannus2), occurrence of newly formed blood vessels3) and pleomorphic fibroblast-like cells with large nuclei and prominent nucleoli4). These features resemble those of preneoplastic conditions and suggest that dysregulation of the apoptosis may play a role in the pathogenesis of rheumatoid arthritis.
The wild type of p53 gene is tumor suppressor oncogene that behaves as a negative growth regulator and regulator of cell survival, proliferation and apoptosis, but the mutant type of p53 gene behaves in an oncogenic maneuver5,6). Mutations of the p53 gene are the most frequently found of all the known tumor suppressor genes and oncogenes7), and such mutations prolong the half-life of the p53 protein that is normally short(<20 min) and permit its detection using immunohistochemistry8).
Mutation of p53 may play a role in manifestation of rheumatoid arthritis synovium, but several studies on p53 expression in synovial tissues of rheumatoid arthritis showed conflicting and various results9–13). For that reason, we investigated the amount and pattern of p53 positive cells in rheumatoid arthritis synovium, in comparison with osteoarthritis synovium, by using immunohistochemistry with two other monoclonal antibodies for p53 to examine p53 expression in synovial tissues of rheumatoid arthritis.
MATERIALS AND METHODS
1. Patients
Synovial tissue specimens were obtained from nine patients with rheumatoid arthritis undergoing either synovectomy or joint replacement surgery. All patients included in this study satisfied the diagnostic criteria of the American College of Rheumatology14). They were receiving therapy with nonsteroidal anti-inflammatory drugs and four patients were treated with disease modifying anti-rheumatic drugs and four patients were receiving low dose prednisone. As a control, synovial tissue samples were also obtained from patients with osteoarthritis undergoing joint replacement surgery. The diagnosis of osteoarthritis was based on typical clinical and radiological features. All patients were receiving therapy with nonsteroidal anti-inflammatory drugs. Clinical characteristics of the patients were presented in Table 1. Tissue samples were fixed in 10% formalin at room temperature, immediately after removal.
Table 1.
Clinical features of patients with RA and OA
| Patient Age/Sex | Duration of disease(yrs) | RF(IU/ml) | Medication | Surgical procedure | |
|---|---|---|---|---|---|
| RA | |||||
| 1 | 46/M | 10 | 648 | NSAID, HCQ 200mg | THRA |
| 2 | 56/F | 16 | 52 | NSAID, pred 10mg | Knee synovectomy |
| 3 | 50/F | 12 | 129 | NSAID, pred 5mg, Triple* | TKRA |
| 4 | 47/F | 5 | 92 | NSAID, pred 10mg, HCQ 200mg | Wrist synovectomy |
| 5 | 63/F | 5 | 34 | NSAID | Wrist synovectomy |
| 6 | 49/F | 7 | 354 | NSAID | TKRA |
| 7 | 42/F | 13 | 143 | NSAID | TKRA |
| 8 | 40/F | 10 | 40 | NSAID | TKRA |
| 9 | 51/F | 13 | 192 | NSAID, pred 7.5mg, bucillamine 200mg | THRA |
| OA | |||||
| 1 | 68/M | 2 | – | NSAID | TKRA |
| 2 | 62/F | 5 | – | NSAID | TKRA |
| 3 | 64/F | 6 | – | NSAID | TKRA |
| 4 | 71/F | 12 | – | NSAID | TKRA |
| 5 | 54/F | 10 | – | NSAID | TKRA |
RA: Rheumatoid arthritis, OA: Osteoarthritis, RF: Rheumatoid factor, NSAID: Nonsteroidal an-tiinflammatory drug HCQ: Hydroxychloroquine,
Triple: hydroxychloroquine 400mg, sulfasalazine 1.0g/day, methotrexate 10mg/week pred: Prednisone, THRA: Total hip replacement arthroplasty, TKRA: Total knee replacement arthroplasty
2. Immunohistochemistry
Commercial p53 monoclonal antibody(DO-1) was purchased from DACO(A/S, USA) and p53 monoclonal antibody(DO-7) was purchased from Santa-Cruz (Biotechnology, USA). They react with wild type and mutant type of p53 protein. We also purchased DACO LSAB plus kit, Peroxidase(DACO A/S, USA).
Consecutive 5 μm thick paraffin embedded sections were prepared, using standard methods. The avidin-biotin complex(ABC) immunoperoxidase staining were performed using the DO-1, DO-7 monoclonal antibodies for p53 and DACO LSAB plus kit according to the manufacturer’s protocol for paraffin sections. p53 positive reaction was recorded when nuclear or cytoplasmic staining was present. Intensity of staining in the synovial lining, inflammatory mononuclear cells, subsynovial fibroblast-like cells and vascular endothelial cells was judged on a 0 to 4+ scale as follows by the pathologist who was blinded to the clinical diagnosis and disease activity: 0, no staining; 1+, rare positive cells or trace staining; 2+, scattered clusters of positive cells; 3+, moderate staining in a specific region; 4+, extensive staining throughout a region.
3. Inflammation index
One section was stained with haematoxylin and eosin for histologic features of inflammation. Six variables were assessed, based on a protocol described previously15,16), with the modification that a grading system of 0–3 was used. Grading was based on polymorphonuclear cell infiltration, hyperemia, fibrin deposition, mononuclear cell infiltration, synovial proliferation and fibrosis. The assessment was made on the whole specimen, both at low power and high power by the pathologist who was blinded to the clinical data(Table 2).
Table 2.
Histologic scoring system for 6 features
| Feature, Score |
|---|
| Polymorphonuclear cell infiltration |
| 0 = none |
| 1 = scanty |
| 2 = focal clusters |
| 3 = widespread |
| Hyperemia |
| 0 = no vessels dilated/congested |
| 1 = occasional |
| 2 = intermediate |
| 3 = all vessels affected |
| Fibrin deposition |
| 0 = none |
| 1 = scanty and focal |
| 2 = focal with polymorphonuclear cells |
| 3 = extensive |
| Mononuclear cell infiltration |
| 0 = occasional |
| 1 = focal |
| 2 = confluent |
| 3 = confluent with follicles |
| Synovial cell proliferation |
| 0 = 2–3 cell layers |
| 1 = 4–5 cell layers |
| 2 = 6–7 cell layers |
| 3 = >7 cell layers |
| Fibrosis |
| 0 = scant perivascular |
| 1 = discreet isolated bands |
| 2 = broad bands |
| 3 = confluemt |
4. Statistical analysis
Data were expressed as mean ± SEM and statistical analysis was performed using Sperman rank order test. Differences were considered to be significant when p < 0.05.
RESULTS
In histologic appearance, synovial tissues, hyperemia, mononuclear cell infiltration, synovial proliferation and fibrosis were observed in the synovial tissues of rheumatoid arthritis more than in those of osteoarthritis, and polymorphonuclear cell infiltration and fibrin deposition were seen in the synovial tissues of osteoarthritis more than in those of rheumatoid arthritis, but there was no significant difference between the two groups(p > 0.05)(Table 3).
Table 3.
Results obtained from histologic scoring and p53 immunohistochemical staining.
| Patient | PMN cell infiltration | Hyperemia | Fibrin deposition | Mononuclear cell infiltration | Synovial cell proliferation | Fibrosis | p53* |
|---|---|---|---|---|---|---|---|
| RA | |||||||
| 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 2 | 1 | 0 | 1 | 1 | 0 | 1 | 2+ |
| 3 | 0 | 3 | 1 | 0 | 0 | 0 | 0 |
| 4 | 2 | 1 | 2 | 3 | 0 | 2 | 2+ |
| 5 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| 6 | 2 | 1 | 0 | 2 | 1 | 2 | 0 |
| 7 | 1 | 2 | 0 | 2 | 0 | 2 | 0 |
| 8 | 0 | 1 | 1 | 1 | 0 | 3 | 0 |
| 9 | 0 | 1 | 1 | 1 | 0 | 1 | 1 + |
| mean(SEM) | 0.7(0.3) | 1.1(0.3) | 0.8(0.2) | 1.2(0.3) | 0.1(0.1) | 1.2(0.4) | 0.6(0.3) |
| OA | |||||||
| 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 2 | 2 | 1 | 3 | 1 | 0 | 0 | 1+ |
| 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 5 | 2 | 1 | 2 | 1 | 0 | 0 | 1+ |
| mean(SEM) | 0.8(0.5) | 0.8(0.2) | 1.0(0.6) | 0.4(0.2) | 0.0(0.0) | 0.0(0.0) | 0.4(0.2) |
| p-value | 0.79 | 0.71 | 1.00 | 0.32 | 1.00 | 0.18 | 0.41 |
RA: Rheumatoid arthritis, OA: Osteoarthritis, PMN: Polymorphonuclear
0, no staining; 1+, rare positive cells or trace staining; 2+, scattered clusters of positive cells; 3+, moderated staining in a specific region; 4+, extensive staining throught a region
Immunohistochemical evaluation was made with p53 positivity defined as nuclear or cytoplasmic(with or without nuclear staining) patterns, as detected with the DO-1 and DO-7 monoclonal antibodies. In comparing tissue immunoreactivity by DO-1 and DO-7, all the samples showed similar results with both antibodies.
In the synovial tissues of patients with rheumatoid arthritis, p53 positive cells were detected as cytoplasmic pattern in 3 out of 9 samples(33%). One case showed trace staining and two cases showed scattered staining, and the positively stained cells were small and round with characteristics of lymphocytes. Synovial lining cells, subsynovial fibroblast-like cells and vascular endothelial cells were p53 negative. In order to compare p53 expression in the synovial tissues of osteoarthritis, we also investigated synovial samples obtained from patients with osteoarthritis. p53 positive cells were observed as cytoplasmic pattern in 2/5 OA samples(40%). They were inflammatory mononuclear cells that had characteristics of lymphocytes and showed trace staining. In the synovial samples of osteoarthritis, the distribution of p53 positive cells was comparable to that seen in the synovial tissues of rheumatoid arthritis. There were no striking differences in the amount and pattern of p53 positive cells between rheumatoid arthritis and osteoarthritis, and there was no demonstrable correlation between the two groups with respect to inflammation scores and expression of p53 protein in synovial tissues(Fig. 1)(Table 3).
Fig. 1.
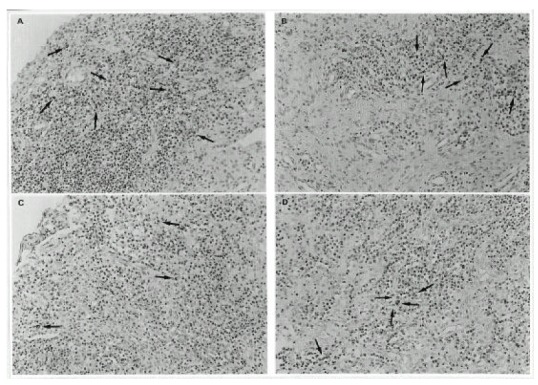
Immunohistochemical staining for p53 in representative synovial tissues from rheumatoid arthritis(A, B) and osteoarthritis(C, D). Positive immunoreactivity appears as brown color(arrows). The amount and pattern of p53 positive cells in rheumatoid arthritis synovial tissues were comparable to those seen in osteoarthritis synovial tissues (Original magnification, X200).
These results indicate that p53 expression in RA synovial tissue is limited to inflammatory mononuclear cells, and the amount and pattern of p53 positive cells are not significantly different between the synovial tissues of rheumatoid arthritis and osteoarthritis.
DISCUSSION
The p53 gene acts as a molecular guardian for genomic integrity5). If DNA is damaged, p53 is induced, stabilized or activated and arrests the cell until the damage is repaired. If the damage cannot be repaired, p53 might initiate apoptosis. Wild-type p53 is thought to promote apoptosis, whilst mutant p53 has the inhibition of apoptosis6).
Mutant p53 protein, which takes on an abnormal conformation, has a half-life of several hours compared with 20 minutes for the wild-type p538). It accumulates in cells and thus becomes immunologically detective. So, positive immunostainning is indicative of abnormalities of the p53 gene and its product. Although immunohistochemical detection of p53 can be influenced by variables, p53 immunohistochemistry is of value in detecting p53 mutation if appropriate care is taken17). In our study, we used the immunohistochemistry with two monoclonal antibodies for p53, and all the samples showed similar results with both anti-p53 antibodies, DO-1 and DO-7.
Rheumatoid arthritis is a chronic, inflammatory, autoimmune disease characterized by abnormal proliferation of synovial cells that is important in pathogenesis of rheumatoid arthritis1). The rheumatoid arthritis synovium resembles properties of malignant tumor cells2–4). However, the mechanism of abnormal proliferation of synovial cells is not clear. Most p53 mutations are not inherited and, instead, they arise from a coping error or an attack by a carcinogen. Thus, mutations in p53 may occur in rheumatoid arthritis synovium as a consequence of inflammation and may be associated with synovial proliferation.
To our knowledge, there were five studies on p53 expression in rheumatoid arthritis synovium, but their studies showed different and various results9–13). Firestein et al revealed that p53 protein was detected in both cytoplasmic and nuclei of lining cells, lesser amounts of immunoreactive p53 were detected in the sublining mononuclear cells and p53 expression in rheumatoid arthritis synovium was significantly more than that in osteoarthritis tissues. So, they suggest that somatic mutations in the p53 genes might occur as a consequence of pathogenesis of rheumatoid arthritis9,10). Gonagle et al revealed that p53 is not demonstrable in early RA but seen in three of thirteen established rheumatoid arthritis by immunohistochemistry, and they suggest that p53 expression in rheumatoid arthritis may be secondary to DNA damage as a consequence of chronic inflammation, like the results of studies by Firestein et al11). On the other hand, Sugiyama et al showed that p53 expression in rheumatoid arthritis synovium was seen only in the cytoplasm of the subsynovial cells. Synovial lining cells and infiltrated lymphocytes did not react with anti-p53 antibodies, and they suggest that p53 oncogene is probably not implicated in the apoptosis process of synovium of rheumatoid arthritis12). Moreover, Murata et al demonstrated that any mutations in p53 gene were not found from exon 4 through 10 in both CD14-positive synoviocytes and fibroblasts of rheumatoid arthritis and, on the contrary, in some patients(2/13) p53 mRNA expression was significantly decreased in CD14-positive cells. They suggest that loss of function of p53 due to decreased p53 gene expression may contribute to the overgrowth of the synovial tissues in rheumatoid arthritis13). Our study indicates that p53 expression was detected in 33% of the synovial tissues of rheumatoid arthritis and it was limited to cytoplasms of inflammatory mononuclear cells, and there was no significant difference in the amount and pattern of p53 positive cells between the synovial tissues of rheumatoid arthritis and osteoarthritis. The expression of p53 protein was also unrelated to the degree of histologic scores in both groups. We do not know the reason why several studies, including our study on p53 expression in RA synovium, showed conflicting results.
Evidence has been obtained of cytoplasmic p53 gene product localization, not necessarily ascribed to gene mutations18). p53 cytoplasmic localization may be due to binding to viral or cellular products, may be consequent to the ineffective nuclear translocalization and may depend on the conformational and phosphorylation status of the protein19). Therefore, in our study, there is the possibility that the expression of p53 cytoplasmic localization may be not due to mutations in RA and OA synovial tissues. The expression of other proto-oncogenes in rheumatoid arthritis synovial tissue has been documented in several studies, but it has remained unclear whether transforming oncogenes are also present20–22). Therefore, we also believe that the exact expression and role of p53 gene, as well as other proto-oncogenes, remain to be clearly established in the pathogenesis of rheumatoid arthritis.
It has been reported that the presence of anti-p53 antibodies may have been associated with the accumulation of mutant p53 proteins in the tumor and they can be considered a marker for the presence of mutations in cancers23,24). It will be also necessary and interesting to examine anti-p53 antibodies in rheumatic diseases, and that will be also helpful in understanding the pathogenesis of rheumatic diseases. We are continuing the study on anti-p53 antibodies in rheumatic diseases.
In conclusion, our study showed that, in contrast to other studies, p53 expression was only restricted to inflammatory mononuclear cells, the amount and pattern of p53 positive cells are not significantly different between the synovial tissues of rheumatoid arthritis and osteoarthritis and that there was no correlation between inflammation scores and expression of p53 protein in synovial tissues of both groups. These findings suggest that altered p53 expression may not play a significant role in the manifestation of rheumatoid arthritis synovium. However, these data need to be strengthened by increasing the number of samples and molecular biology approaches, and the precise role of p53 remains the subject of ongoing study.
REFERENCES
- 1.Gay S, Gay RE, Koopman WJ. Molecular and cellular mechanisms of joint destruction in rheumatoid arthritis: Two cellular mechanisms explain joint destruction? Ann Rheum Dis. 1993;52:39–47. doi: 10.1136/ard.52.suppl_1.s39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamilton JA. Hypothesis: in vitro evidence for the invasive and tumor-like properties of the rheumatoid pannus. J Rheumatol. 1983;10:845–51. [PubMed] [Google Scholar]
- 3.Bromley M, Woolley DE. Histopathology of the rheumatoid lesion: identification of cell types at sites of cartilage erosion. Arthritis Rheum. 1984;27:857–63. doi: 10.1002/art.1780270804. [DOI] [PubMed] [Google Scholar]
- 4.Lafyatis R, Remmers EF, Roberts AB, Yocum DE, Sporn MB, Wilder RL. Anchorage-independent growth of synoviocytes from arthritic and normal joints: stimulation by exogenous platelet derived growth factor and inhibition by transforming growth factor-beta and retinoids. J Clin invest. 1989;83:1267–76. doi: 10.1172/JCI114011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donehower LA, Bradley A. The tumor suppressor p53. Biochum Biophys Acta. 1993;1155:181–205. doi: 10.1016/0304-419x(93)90004-v. [DOI] [PubMed] [Google Scholar]
- 6.Greenblatt MS, Bennett WP, Hollstein M, Harris CC. Mutations in the p53 tumor suppressor gene: Clues to cancer etiology and molecular pathogenesis. Cancer Res. 1994;54:4855–78. [PubMed] [Google Scholar]
- 7.Roviski B, Benchimol S. Immortalization of rat embryo fibroblasts by the cellular p53 oncogene. Oncogene. 1988;2:445–52. [PubMed] [Google Scholar]
- 8.Finlay CA, Hinds PW, Tan TH, Eliyahu D, Oren M, Levine AJ. Activating mutations for transformation by p53 produce a gene product that forms a hsc70-p53 complex with an altered half-life. Mol Cell Biol. 1988;8:531–9. doi: 10.1128/mcb.8.2.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Firestein GS, Nguyen K, Aupperle KR, Yeo M, Boyle DL, Zvaifler NJ. Apoptosis in rheumatoid arthritis. P53 overexpression in rheumatoid arthritis synovium. Am J Pathol. 1996;149:2143–51. [PMC free article] [PubMed] [Google Scholar]
- 10.Firestein GS, Echeverri F, Yeo M, Zvaifler NJ, Green DR. Somatic mutations in the p53 tumor suppressor gene in rheumatoid arthritis synovium. Proc Natl Acad Sci USA. 1997;94:10895–900. doi: 10.1073/pnas.94.20.10895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonagle DM, Raece R, Green M, et al. P53 is not demonstrable by immunohistochemistry in early rheumatoid arthritis[Abstract] Arthritis Rheum (suppl) 1997;40:S119. [Google Scholar]
- 12.Sugiyama M, Tsukazaki T, Yonekura A, Matsuzaki S, Yamashita S, Iwasaki K. Localization of apoptosis and expression of apoptosis related proteins in the synovium of patients with rheumatoid arthritis. Ann Rheum Dis. 1996;55:442–9. doi: 10.1136/ard.55.7.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murata S, Sawada T, Shinohara S, et al. Decreased p53 gene expression of CD 14-positive cells in rheumatoid synovium[Abstract] Arthritis Rheum (suppl) 1997;40:S294. [Google Scholar]
- 14.Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 15.Marok R, Winyard PG, Coumbe ML, et al. Activation of the transcription factor nuclear factor-kB in human inflamed synovial tissue. Arthritis Rheum. 1996;39:583–91. doi: 10.1002/art.1780390407. [DOI] [PubMed] [Google Scholar]
- 16.Rooney M, Condell D, Quinlan W, et al. Analysis of the histologic variation of synovitis in rheumatoid arthritis. Arthritis Rheum. 1988;31:956–63. doi: 10.1002/art.1780310803. [DOI] [PubMed] [Google Scholar]
- 17.Hall PA, Lane DP. P53 in tumor pathology: can we trust immunohistochemistry?-revisited. J Pathol. 1994;172:1–4. doi: 10.1002/path.1711720103. [DOI] [PubMed] [Google Scholar]
- 18.Barnes DM, Hanby AM, Gillett CE, et al. Abnormal expression of wild p53 protein in normal cells of a cancer family patient. Lancet. 1992;340:259–63. doi: 10.1016/0140-6736(92)92354-i. [DOI] [PubMed] [Google Scholar]
- 19.Fritsche M, Haessler C, Brandner G. Induction of nuclear accumulation of the tumor-suppressor protein p53 by DNA-damaging agents. Oncogene. 1993;8:307–18. [PubMed] [Google Scholar]
- 20.Roivainen A, Jarava J, Pirila L, Yli-Jama T, Tiusanen H, Toivanen P. H-ras oncogene point mutations in arthritic synovium. Arthritis Rheum. 40:1636–43. doi: 10.1002/art.1780400913. [DOI] [PubMed] [Google Scholar]
- 21.Roivainen A, Soderstrom KO, Pirila L, et al. Oncoprotein expression in human synovial tissue:an immunohistochemical study of different types of arthritis. Br J Rheumatol. 1996;35:933–42. doi: 10.1093/rheumatology/35.10.933. [DOI] [PubMed] [Google Scholar]
- 22.Isomaki P, Soderstorm KO, Punnonen J, et al. Expression of bcl-2 in rheumatoid arthritis. Br J Rheumatol. 1996;35:611–9. doi: 10.1093/rheumatology/35.7.611. [DOI] [PubMed] [Google Scholar]
- 23.Angelopnoulou K, Rosen B, Stratis M, Yu H, Solomou M, Diamandis EP. Circulating antibodies against p53 protein in patients with ovarian carcinoma. Cancer. 1996;77:2146–52. [PubMed] [Google Scholar]
- 24.Soussi T. The humoral response to the tumor-suppressor gene-product p53 in human cancer: implications for diagnosis and therapy. Immunol Today. 1996;17:354–6. doi: 10.1016/0167-5699(96)30019-4. [DOI] [PubMed] [Google Scholar]


