Abstract
Background & objectives
The pathogenic mechanism of aspirin-sensitive asthma (ASA-BA) remains to be further defined. To evaluate the role of circulating immune complex (CIC) in ASA-BA.
Subjects & Methods
We measured IgG- and IgA-IC level by ELISA using anti-C3 antibody in 33 ASA-BA patients whose sensitivity was confirmed by lysine-aspirin bronchoprovocation test, and compared with those of 74 allergic, 14 intrinsic asthma patients and 7 healthy controls.
Results
There was no significant difference in IgG-IC level among the four groups (p>0.05), while IgA-IC levels of aspirin-sensitive asthma were higher than those of other groups (p=0.0035). Patients with nasal polyp had significantly higher IgG-IC than those without it (p=0.02). No differences were found according to medication and symptom scores, and presence of atopy, rhino-sinusitis, urticaria or concurrent sensitivity to sulfite (p>0.05). Insignificant correlation was found between IgG-IC level and asthma duration, total IgE level, or circulating eosinophil count.
Conclusion
These findings suggest a possible contribution of IgG-IC to the development of nasal polyp in ASA-BA. Further study will be needed to clarify the role of IgA-IC in the pathogenesis of ASA-BA.
Keywords: circulating immune complex, aspirin-sensitive asthma, nasal polyp
INTRODUCTION
ASA and non-steroidal anti-inflammatory drugs(NSAIDs) can induce bronchoconstriction in 10–20% of adult asthmatic patients1,2). The mechanism of ASA-induced bronchoconstriction is partly clarified. Appreciable numbers of aspirinsensitive asthma had rhino-sinusitis and/or nasal polyp3–6). Immunohistochemical study7) of the bronchial tissue from ASA-BA showed increased inflammatory cell infiltrations, including eosinophil, mast cell and lymphocyte, similarly to non-aspirin sensitive asthma. In this study, in order to further understand the pathogenic mechanism of ASA-BA, we tried to detect C3-containing IgG- and IgA-IC level in sera from ASA-BA patients and analyzed them based upon various clinical characteristics seen in ASA-BA.
METHODS
Subjects
Thirty three ASA-BA patients, aged between 23 and 72 years, participated in this study. All showed positive responses on lysine-aspirin (L-ASA) bronchoprovocation test (BPT), and they were compared with 14 allergic asthma patients sensitive to house dust mite, 14 intrinsic asthma patients and seven healthy controls. Their sera were collected and stored at −20°C. Atopy was defined on the basis that they showed more that 2+ skin prick test reactions to more than two common inhalant allergens, such as Dermatophagoides farinae, alder, oak, rye grass, mugwort, ragweed, Aspergillus spp. (Bencard Allergy Service, Bredford, Middlesex, UK).
L-ASA bronchoprovocation test
L-ASA BPT was performed according to the method with some modifications8–10). Pulmonary functions were measured with a spirometer (Chest), the FEV1 and maximum midexpiratory flow (MMEF), before and during the provocation. The test solution was delivered by a De Vilbiss 646 nebulizer (DeVilbiss Co., Somerset, Penn., USA) and connected to a compressed air source (5 1/min). Normal saline was inhaled as a placebo solution. The patients were asked to breathe the nebulized aerosol up to their vital capacity, 10 times L-ASA (Young Jin Pharmaceutical Co. Korea), as a powder containing 1800 mg L-ASA was made up freshly on each challenge day. The challenges with the placebo were performed seven days before the L-ASA BPT. L-ASA BPT from 11.25 up to 180 mg/ml was performed to induce more than a 20% fall of FEV1. The FEV1 and MMEF were measured frequently during the first hour, and then hourly for 8 hours.
Measurement of C3-containing IgG- and IgA immune complex: (IC)
C3 containing IgG-IC was measured according to previously described methods with some modifications11–13). A 96-well microplate (Dynatech, Alexandria, Va, USA) in 0.05M carbonate buffer (pH 9.6) at 4°C was used. After washing with phosphate-buffered saline with 0.05% Tween 20(PBST), the wells were blocked with 1% bovine serum albumin-PBST. The wells were then incubated with undiluted sera overnight at 4°C. After washes with PBST, they were incubated with 50 μl biotin-conjugated anti-IgG or anti-IgA antibodies (Vector laboratories, Burlingame, CA, USA) at a dilution of 1: 1000 (w/v) for 1 hour. The washing step was repeated, and streptavidin-conjugated peroxidase (Sigma, St. Louis, MO, USA) at a dilution of 1:1000 w/v was added into the wells and incubated for 30 minutes. After another wash, 50 μl of 0.01M ABTS (2,2′-azino bis-3 ethyl-benzthiazoline sulfonic acid) in 0.07M citrate-phosphate buffer, pH 4.2 containing 0.03% H2O2 was added to the wells. The color reaction was stopped with 0.002M sodium azide and the plate was read at 410 nm using a microtiter reader (Dynatech Laboratories, Virginia, USA). The standard for quantification of C3-IgG- or IgA-IC was established by pooling systemic lupus erythematous patients sera with high IgG-IC levels, and arbitrarily defining the standard as 100 AU (arbitrary unit)/ml. Optical density of the test sera was compared to that from serially diluted standard and presented as AU/ml.
Statistical Analysis
The ANOVA and Mann-Whitney tests were applied using the SPSS version 7.0 (Chicago) to evaluate statistical significance. A p value of 0.05 or less was regarded as significant.
RESULTS
This study demonstrated IgG-IC and IgA-IC levels in three asthmatic groups and seven healthy controls as shown in Fig. 1. IgG-IC levels tended to be higher than those of IgA-IC. There was no significant difference in the IgG-IC level among the four groups (p>0.05). However, IgA-IC level was significantly higher in ASA-BA than in other groups (p=0.0035).
Fig. 1.
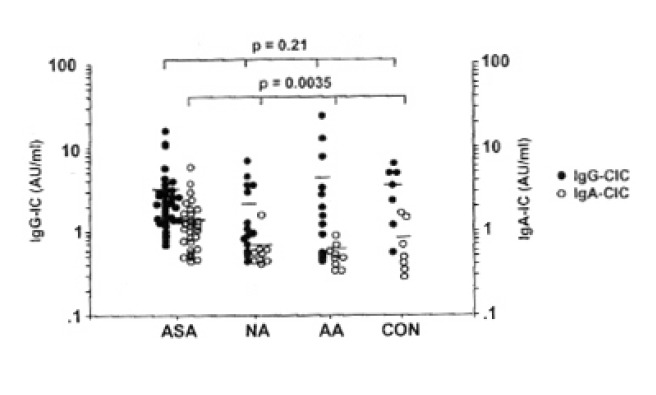
IgG- and IgA-immune complex (IC) levels in aspirin-sensitive asthma (ASA), non-allergic asthma (NA), allergic asthma (AA), and healthy controls (CON). There was no significant difference in IgG-IC levels among the four groups (p>0.05). However, IgA-IC level of aspirin-sensitive asthma was significantly higher than those of other groups. (p=0.035). Bar indicates mean value of each group.
IgG-IC level was compared according to the presence of rhino-sinusitis, urticaria or nasal polyp. No significant difference was found in IgG-IC level, whether the patients have rhino-sinusitis or urticaria (p=0.39, p=0.97, respectively). However, the patients having nasal polyp had significantly higher IgG-IC level than those without it (p=0.02). No significant difference was found between IgG-IC level and atopic status or concurrent sensitivity to sulfite (p=0.32 p=0.95, respectively) as shown in Fig. 2.
Fig. 2.

Comparison of IgG-IC levels according to the associated conditions in aspirin-sensitive asthma patients. No significant difference was found according to presence of atopy, rhino-sinusitis, urticaria or concurrent sensitivity to sulfite. Patients having nasal polyp had significantly higher IgG-IC than those without it (P = 0.02)
Fig. 3 shows the distribution of IgG-IC level according to medication and symptom scores. Most patients had high symptoms and medication scores (Class 3 or 4). No significant difference was found among the four groups (p>0.05).
Fig. 3.
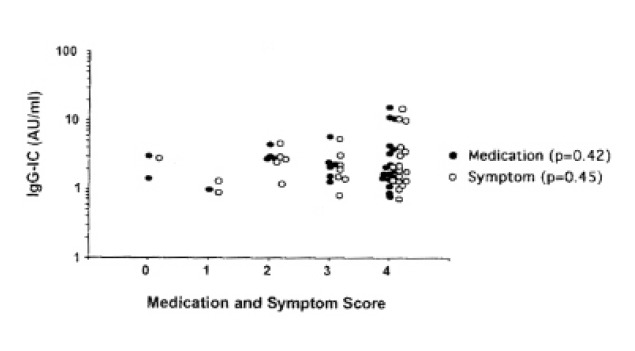
IgG-IC levels according to medication and symptom scores in aspirin-sensitive asthma patients. No significant difference was found.
Fig. 4 shows the relationship between IgG-IC level and duration of asthma symptoms, total IgE level or eosinophil count. The correlation was insignificant with asthma symptom duration (r=0.19, p=0.31), total IgE level (r=0.13, p=0.49), or total eosinophil count (r=0.18, p=0.33)
Fig. 4.
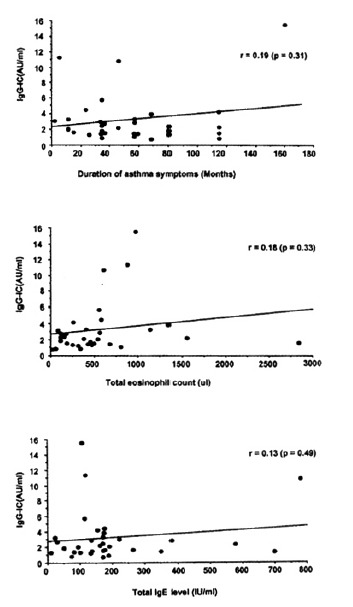
Correlation between IgG-IC level and asthma duration, total eosinophil count, total IgE level in aspirin-sensitive asthmatic patients. No significant correlations were noted (p>0.05)
DISCUSSION
The pathogenic significance of CIC in allergic diseases is unclear. Several investigators have reported IC, especially IgE-IC, increased in patients with allergic asthma and food allergy, especially after the food challenge test14–16). In food allergy patients, IgE IC could activate the complement system and bind to the conglutinin column after the addition of fresh human sera, suggesting a participation of C3 in IgE-IC. Our previous study13) showed that C3-containing IgE-IC was more elevated in house dust mite-sensitive asthma than in non-allergic asthma. There have been some in vitro data supporting the possible involvement of IC in allergic inflammation. IC containing IgE could activate inflammatory cells, including monocyte, neutrophil17), and eosinophil18). Preformed allergen-IgE complex could induce immediate erythema and wheal reaction19). Moreover, activated C3 fragment could degranulate mast cell and activate monocyte, neutrophil and eosinophil20). Furthermore, there has been a report suggesting that an IC-mediated mechanism may contribute to late skin reaction on the basis that late reaction to the house dust mite on intradermal test could be accentuated when autologous serum was mixed with the allergen in sensitive individuals21). These results might suggest a possible involvement of C3-containing IC in the pathogenesis of atopic asthma. However, there have been very few reports to study the role of circulating immune complex in patients with ASA-BA. In the present study, we tried to detect C3-containing IgG- and IgA-IC levels in ASA-BA, and compared them with allergic and non-allergic asthma, as well as healthy controls. IgG-IC level was higher than IgA-IC in each group. No significant difference was noted in IgG-IC level among the four groups but, interestingly, IgA-IC was significantly higher in ASA-BA than in other groups. Further studies will be needed to identify the role of IgA-IC in airway inflammation of ASA-BA.
The definitive diagnostic test for respiratory sensitivity to ASA has been oral provocation with ASA and NSAIDs. L-ASA BPT has become an alternative diagnostic test to detect ASA sensitivity in asthmatic patients8,9,22). In our previous study10), L-ASA inhalation induced late asthmatic response as well as early reaction. The mechanism to induce late asthmatic response following L-ASA inhalation has been unknown. In the present study, 15 had early asthmatic response and 18 had a late onset asthmatic response (five dual and 13 late only). No difference was found in the IgG-IC level according to the type of asthmatic response following L-ASA inhalation. These results support that L-ASA BPT is a useful method to determine lower respiratory sensitivity to ASA, and IgG-IC may not be involved in the development of the late asthmatic response.
ASA-BA has a wide clinical spectrum23). High incidence of rhino-sinusitis and/or nasal polyp was reported in ASA-BA5,6,24). The frequency of polyp formation in patients with Samter’s syndrome has ranged from 50 to 95 percent. Our recent investigation(unpublished data) on immunohisto chemical analysis of nasal polyp from ASA-BA revealed that the number of mast cell and eosinophil tended to be higher than non-allergic polyp, although the statistical significance was not reached. In this study, the patients with nasal polyp had significantly higher IgG-IC level than those without it. These findings may support a possible involvement of IgG-IC in the nasal polyp formation in ASA-BA. Further investigations will be needed to detect these ICs within the nasal polyp tissue.
Acknowledgments
We are indebted to Mrs. Jong-Hee Choo for her excellent technical assistance and to Ms. Jin-Yoo for preparing the manuscript.
REFERENCE
- 1.McDonald JR, Mathison DA, Stevenson DD. Aspirin intolerance, detection by oral challenge. J Allergy din immunol. 1972;50:198–207. doi: 10.1016/0091-6749(72)90014-0. [DOI] [PubMed] [Google Scholar]
- 2.Spector SL, Wangaard CH, Farr RS. Aspirin and concomitant idiosyncrasies in adult asthmatic patient. J Allergy Clin Immunol. 1979;64:500–506. doi: 10.1016/0091-6749(79)90059-9. [DOI] [PubMed] [Google Scholar]
- 3.Delaney JC. The diagnosis of aspirin idiosyncrasy by analgesic challenge. Clin Allergy. 1976;6:177–181. doi: 10.1111/j.1365-2222.1976.tb01896.x. [DOI] [PubMed] [Google Scholar]
- 4.Weber RW, Hoffman M, Raine D. Incidence of bronchoconstriction due to aspirin, azo dyes, non-azo dyes, and preservatives in a population of perennial asthmatics. J Allergy Clin Immunol. 1979;64:32–37. doi: 10.1016/0091-6749(79)90080-0. [DOI] [PubMed] [Google Scholar]
- 5.Pleskow WW, Stevenson DD, Mathison DA. Aspirin-sensitive rhinosinusitis/asthma: spectrum of adverse reactions to aspirin. J Allergy Clin Immunol. 1983;71:574–579. doi: 10.1016/0091-6749(83)90439-6. [DOI] [PubMed] [Google Scholar]
- 6.Zettz HJ. Bronchial asthma, nasal polyps and aspirin sensitivity: Samter’s syndrome. Clin in Chest Med. 1988;9:567–576. [PubMed] [Google Scholar]
- 7.Shuaib Nasser SM, Pfister R, Christie PE, Sousa AR, Barker J, Schmitz-Schumann M, Lee TH. Inflammatory cell populations in bronchial biopsies from aspirinsensitive asthmatic subjects. Am J Respir Grit Care Med. 1996;153:90–96. doi: 10.1164/ajrccm.153.1.8542168. [DOI] [PubMed] [Google Scholar]
- 8.Dahlen B, Zetterstrom O. Comparison on bronchial and per oral provocation with aspirin in aspirin-sensitive asthmatics. Eur Respir J. 1990;3:527–534. [PubMed] [Google Scholar]
- 9.Phillips GD, Foord R, Holgate ST. Inhaled lysine-aspirin as a bronchoprovocation procedure in aspirin-sensitive asthma: its repeatability, absence of a late-phase reaction and the role of histamine. J Allergy Clin Immunol. 1989;84:232–241. doi: 10.1016/0091-6749(89)90330-8. [DOI] [PubMed] [Google Scholar]
- 10.Park HS. Early and late onset asthmatic responses following lysine-aspirin inhalation in aspirin-sensitive asthmatic patients. Clin Exp Allergy. 1995;25:38–40. doi: 10.1111/j.1365-2222.1995.tb01000.x. [DOI] [PubMed] [Google Scholar]
- 11.Pereira AB, Theofilpoulos AN, Dixon FJ. Detection and partial characterization of circulating immune complexes with solid-phase anti-C3. J Immunol. 1980;125:763–770. [PubMed] [Google Scholar]
- 12.Hall RP, Lawley TJ. Characterization of circulating and cutaneous IgA immune complexes in patients with dermatitis herpetiformis. J Immunol. 1985;135:1760–1765. [PubMed] [Google Scholar]
- 13.Nahm DH, Park HS. C3-containing IgE immune complex in asthmatic patients. J Kor Med Sci. 1996;11:216–221. doi: 10.3346/jkms.1996.11.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brostoff J, Carini C, Wraith DG, Johns P. Production of IgE complexes by allergen challenge in atopic patients and the effect of sodium cromoglycate. Lancet. 1979;i:1268–1270. doi: 10.1016/s0140-6736(79)92229-3. [DOI] [PubMed] [Google Scholar]
- 15.Stevens WJ, Bridts CH. IgG-containing and IgE-containing circulating immune complexes in patients with asthma and rhinitis. J Allergy Clin Immunol. 1984;73:276–282. doi: 10.1016/s0091-6749(84)80020-2. [DOI] [PubMed] [Google Scholar]
- 16.Carini C, Brostoff J. Evidence for circulating IgE complexes in food allergy. La Ricerca Clin Lab. 1987;17:309–322. doi: 10.1007/BF02886914. [DOI] [PubMed] [Google Scholar]
- 17.De Clerck LS, Struyf NJ, Bridts CH, Stevens WJ. Activation of inflammatory cells by immune complex-escontaining IgE in serum and synovial fluid of patients with rheumatoid arthritis: a study using flow cytometric analysis. Ann Rheum Dis. 1991;50:379–382. doi: 10.1136/ard.50.6.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomassini M, Tsicopoulos A, Tai PC, Gruart V, Tonnel AB, Prin L, Capron A, Capron M. Release of granule proteins by eosmophils from allergic and non-allergic patients with eosinophilia on immunoglobulin-dependent activation. J Allergy Clin Immunol. 1991;88:365–375. doi: 10.1016/0091-6749(91)90099-a. [DOI] [PubMed] [Google Scholar]
- 19.Ishizaka K, Ishizaka T. Induction of erythema-wheal reactions by soluble antigen-~E antibody complexes in humans. J Immunol. 1968;101:68–78. [PubMed] [Google Scholar]
- 20.Fearon DT. Complement. J Allergy Clin Immunol. 1983;71:520–529. doi: 10.1016/0091-6749(83)90431-1. [DOI] [PubMed] [Google Scholar]
- 21.Nahm DH, Park JW, Hong CS. Effect of autologous sera on immediate and late skin reaction to the house dust mite in atopic individuals. Yonsei Med J. 1995;36:137–145. doi: 10.3349/ymj.1995.36.2.137. [DOI] [PubMed] [Google Scholar]
- 22.Melillo G, Padovano A, Cocoo G, Masi C. Dosimeter inhalation test with lysine acetylsalicylate for the detection of aspirin-induced asthma. Ann Allergy. 1993;71:61–65. [PubMed] [Google Scholar]
- 23.Park HS. Complete resolution of airway hyperresponsiveness in aspirin-sensitive asthmatic patients. Kor J Int Med. 1996;11:157–160. doi: 10.3904/kjim.1996.11.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lowalski ML. Aspirin-sensitive rhino-sinusitis/asthma syndrome-pathophysiology and management. ACI Int. 1996;8:49–56. [Google Scholar]


