Abstract
Objectives
The expressions of bcl-2 have been reported recently in non-small cell lung carcinoma (NSCLC*). As oncogensis is believed to involve a number of genetic alterations, there can be differences in DNA ploidy or proliferative activity even in bcl-2 positive cases according to the superimposed genetic events.
Subjects and Methods
On the assumption that we might further discern the biologic behavior of bcl-2 positive NSCLC according to the status of DNA ploidy and proliferative activity, we conducted a study for bcl-2 expression with immunohistochemical staining and DNA analysis on 52 surgical specimens of NSCLC.
Results
The bcl-2 was positive in 52% (27/52) of specimens, According to the status of bcl-2 expression, there were no significant differences in tumor stages, performance status score and survival time. Among bcl-2 positive NSCLC, aneuploidy and high proliferative activity were noted in 40% and 44%, respectively. In cases with squamous cell carcinoma (SQC**), the proportion of aneuploidy was significantly higher in bcl-2 positive group compared to bcl-2 negative group (p<0.01), which could not be explained with the sole effect of bcl-2. In bcl-2 positive NSCLC, there was no significant survival difference by the status of DNA analysis results. With a Coxproportional hazard model, only T stage was an independent prognostic factor.
Conclusion
In bcl-2 expressed NSCLC, proliferative activity and DNA ploidy were not homogeneous, suggesting other genetic alterations. This may explain our results which showed no differences in survival according to the status of the bcl-2 expression.
Keywords: bcl-2 oncogene, DNA ploidy, proliferative acivity, non-small cell lung carcinoma
INTRODUCTION
The bcl-2 protein is known to have a functon to block the cell death pathway (apoptosis) and offer a survival advantage to the cells1). The bcl-2 proto-oncogene is normally expressed in hematopoietic stem cells, endocrine cells, neurons and basal cells in intestinal and bronchial epithelium2). However it is no longer expressed in more differentiated cells to prevent the accumulation of cells. If there is continued expression of bcl-2 proto-oncogene in differentiated cells, they may accumulate with survival advantage of bcl-2 protein and, with the additional genetic events, may grow to a malignancy3).
Although the expression of bcl-2 proto-oncogene has been known to be implicated in the oncogenesis of follicular lymphoma and diffuse B cell lymphoma, it is normally expressed both in hematopoietic stem cells and in epithelial basal cells. Recently, there have been studies about bcl-2 expression in bronchogenic malignancy. Pezzella et al.4) reported that the survival of bcl-2 expressed group of non-small cell lung carcinoma (NSCLC) was better than the bcl-2 negative group and they suggested that the reason for the good prognosis of the bcl-2 expressed group might be the effect of bcl-2 protein which gives rather a survival advantage than an effect on proliferation. However, oncogenesis is considered a result of multiple genetic insults5), so there should be additional genetic events in bcl-2 expressed tumors, and survival could be different according to the other superimposed genetic events even in bcl-2 expressed patients.
An animal study of mice transfected with a bcl-2-Ig minigene showed polyclonal B cell accumulation which was mostly in the resting phase (97% was in G0/G1 phase)6,7). To our knowledge, there is no report that the overexpression of bcl-2 has resulted from insults causing abnormal cellular DNA contents. Therefore, we presumed an abnormal DNA content or a high proliferative activity as a marker for genetic changes other than bcl-2.
The objective of this study is to analyze the DNA contents and proliferative activity in cases with bcl-2 expressed NSCLC. We assumed that we might further discern the biologic behavior of NSCLC according to the status of DNA ploidy and proliferative activity in bcl-2 expressed cases.
MATERIALS AND METHODS
We collected 52 cases of NSCLC who underwent surgical resection from March, 1986 to January, 1993 in Chonnam university hospital, Kwangju, Korea. Those patients who died within a month after surgery were excluded. Anatomic staging was recorded by the postoperative findings with the TNM staging system for NSCLC8) and performance staus of partients at the time of diagnosis was recorded as Karnofsky scale9). Most of the patients were within stage IIIa (Stage I: 22, II: 11, IIIa: 16, IIIb: 1, IV: 2) and adjuvant radiation therapy was done for 3 patients. There were 41 cases with squamous cell carcinoma (SQC) and 11 cases with adenocarcinoma (ADC). Forty-nine of 52 cases with NSCLC and 38 of 41 SQC were elgible for DNA analysis.
1. Immunohistochemical Stain
We used paraffin blocks made from surgical specimens which had been fixed in 10% neutral-buffered formalin. They were cut in 3 μm thickness and put on the ProbeOn Plus slides (Fisher Scientific). All steps for staining procedure were done in Microprobe system (Fisher Scientific) by the principle of capillary action gap10), which is produced by two approximated ProbeOn Plus slides. After dewaxing and hydration, antigen retrieval system was used by boiling the slides with an 0.01 M citrate buffer (pH 6.0) in a microwave oven (Samsung, 630W) for 10 minutes. Then they were reacted with anti-bcl-2 primary antibody (DAKO-bcl-2, 124, monoclonal mouse, amino acid 51, 54 of bcl-2 protein) for 20 minutes. For the detection of antigen and antibody complexes, we reacted them with secondary antibody (anti-mouse IgG) for 10 minutes, in Redusol (Biomeda) for 5 minutes to block the endogenous alkaline phosphatase and then they were incubated in avidin alkaline phosphatase11) for 12 minutes. The tissue sections were then ready for the chromogen reaction (Fast Red TR Salt for 20 minutes). They were counterstained with 30 second applications of hematoxylin and mounted in Universal Mount (Research Genetics). All reactions were incubated at 50°C. For positive and negative control reactions, normal human spleen tissue sections were routinely stained with and without primary antibody.
2. DNA Ploidy and Cell Cycle Analysis
After meticulously collecting the paraffin blocks which contained tumor tissues, we cut the paraffin blocks with the thickness of 50 μm, dewaxed them in test tubes with xylene for 1 hour in room temperature and then hydrated them with graded concentration of alcohol solutions (100%, 90%, 70%, 50%, 30% and 10%). The specimens were reacted in citrate buffer for 1 hour, then centrifuged. After removing the supernatants, 2ml of 0.25% trypsin was added and overnighted at 37°C. Next morning, tissue suspension was filtered through a nylon mesh of 40 nm pore size, stained for DNA with propidium iodide and lastly, using FACScan (Fluorescent Activated Cell Scanner, Becton Dickinson Immunocytometry System, USA), stimulated With 488 nm argon laser and expressed the signal strength of fluoresence with the number of channels12–14). Samples were considered as aneuploid when the G0/G1 peak was detected in more than 2 peaks of DNA histogram or when the ratio of G2M/G0G1 channel was less than 1.8515). For cell cycle analysis, we used Cellfit software (Beet on Dickinson Immunocytometry systems) for diploid specimens and Multicycle software (Phoenix flow systems) for the aneuploid specimens to eliminate tissue fragment fractions and background noise. Because of the difference in software between aneuploid and diploid group, the cell cycle fractions were not eligible for analysis with their actual values, so we divided them into high and low proliferative activity groups by the median values of S phase fraction in each ploid group (aneuploidy: 3.5–24.8%, median: 16.4% / diploidy: 4.9–48.4%, median 28.3%).
3. Statistical Analysis
Survival times were calculated from the day of surgery. Statistical analysis was performed for the patients with NSCLC and for the group with Squamous ceil carcinoma, but not for the group with adenocarcinoma since there were only 11 Cases of adenocarcinoma. We used SAS statistical analysis package (SAS Institute, Cary, N.C.) for the frequency tables, t-test and univariate analysis. Life tables and analysis of survival functions were done by the Kaplan-Meier product limit method. Comparison of survival functions were done by the method of Breslow, Mantel-Cox, Peto-Prentice, Tarone-Ware. For the calculation of relative risks, we used Cox proportional hazard model with BMDP statistical software. The statistical significance was defined as p value less than 0.05 except Cox proprotional hazard model in which p value limit for entering covariates into the model was set to p<0. 1. In the hazard model, maximum partial likelihood ratio test was used after screening covariates with Peduzzi-Hardy-Holford statistic16).
RESULTS
Overall survival time ranged between 40 to 2218 days. As only 27% (14/52) of patients were confirmed dead during the follow-up period, median survival time was not estimated. According to the anatomic stage, the group with a stage of less than IIIa showed a tendency of prolonged survival compared to the group with more advanced stages (Breslow p=0.06, Fig. 1). In the immunohistochemical stain for bcl-2 on human spleen tissue, the positive reactions were observed in T and B cell areas (mantle zone) and red pulp, but not in germinal centers17). The positive reaction in NSCLC specimens showed as a diffusely or focally positive staining for bcl-2 protein (Fig. 2) the bcl-2 protein was positive in 51.9% (27/52) of NSCLC and no difference was noted in positive rate between SQC 56.1% 23/41) and ADC (36.4% 4/11).
Fig. 1.
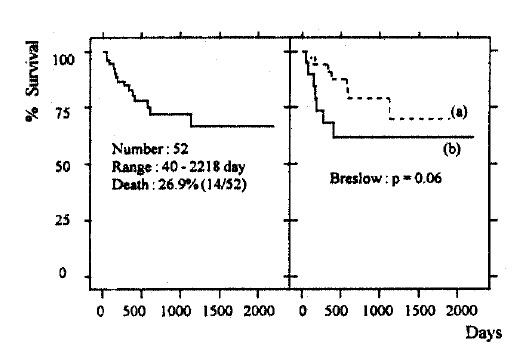
Survival of 52 patients with non-small cell lung carcinoma (left) and comparison of survival according to anatomical stage (right)
(a) stage <IIIa, N =33 3/4 survival time: 1125 day
(b) stage≥IIIa, N=19 3/4 survival time: 177 day
Fig. 2.
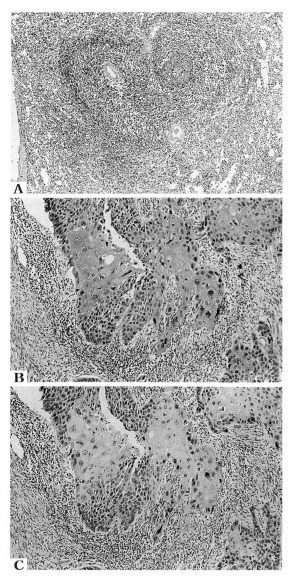
Immunohistochemical stain of human spleen and squamous cell lung carcinoma tissue with a monoclonal antibody for bcl-2 protein (alkaline phosphatase, avidin alkaline phosphatase method, chromogen: Fast Red TR salt, counterstained with hematoxylin);
A: shows a normal human spleen expressing bcl-2 protein in mantle zone and red pulp but not in germinal center. (LM × 40)
B: shows a squamous cell carcinoma expressing bcl-2 protein in tumor cell nest. (LM × 200)
C: shows a squamous cell carcinoma same as panel B, stained without primary antibody. (LM × 200)
According to the status of bcl-2 expression, the distributions of age, anatomic stages and performance status scores and the proportions of smokers were not different. However, the dose of smoking (pack-year) in smokers (N=40) was significantly higher in bcl-2 negative patients than positive patients (Table 1). The survival difference was not noted in 52 cases with NSCLC and in 41 cases with SQC according to the status of bcl-2 expression (Fig. 3).
Table 1.
Characteristics of 52 Patients with Non-Small Cell Lung Carcinoma and 41 Patients with Squamous Cell Carcinoma According to Status of bcl-2 Expression
| Number | Non-Small Cell 52 | Squamous Cell 41 | ||
|---|---|---|---|---|
|
| ||||
| bcl-2 | Positive | Negative | Positive | Negative |
| Sex (M/F) | 24/3 | 22/3 | 21/2 | 18/0 |
| Age (years(SD)) | 56.8(8.7) | 55.7(10.2) | 57.9(8.9) | 58.6(2.1) |
| Smoking (Y/N) | 21/6 | 19/5 | 20/3 | 16/2 |
| Pack Years (mean(SD)) | 35.4(15.3) | 48.5(21.0)* | 35.7(15.6) | 50.7(20.9)* |
| T Stage (1–4) | 1/20/5/1 | 2/18/4/0 | 0/17/5/1 | 1/12/4/0 |
| N Stage (0–2) | 12/6/8 | 10/7/7 | 11/4/7 | 6/6/5 |
| PS score# (≥80/<80) | 21/6 | 18/7 | 18/5 | 12/6 |
Fig. 3.
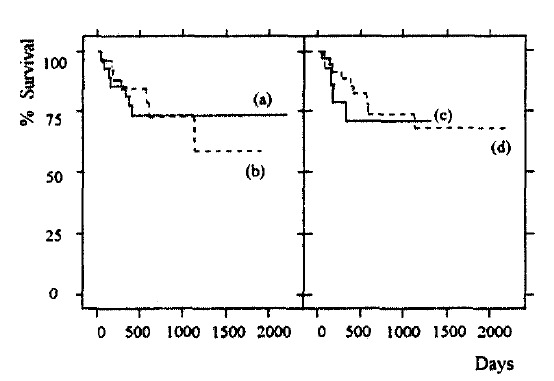
Survival of 52 patients with non-small cell lung carcinoma according to the status of bcl-2 expression (left) and DNA ploidy (right)
(a) bcl-2 positive (27) 3/4 survival time: 400 day
(b) bcl-2 negative (25) 3/4 survival time: 594 day
(c) Diploidy (35) 3/4 survival time: 594 day
(d) Aneuploidy (14) 3/4 survival time: 334 day
Of 49 NSCLC specimens which were eligible for DNA analysis, 28.6% (14/49) showed aneuploidy (SQC: 28.9%(11/38), ADC: 27.3%(3/11)). No significant differences were noted in the age, sex, smoking history, amount of smoking, anatomic stages and performance status scores by either the DNA ploidy (Table 2) or proliferative activity (Table 3). The survival was not different in cases with NSCLC and in cases with SQC according to the DNA ploidy (Fig. 3) or proliferative activities (data not shown).
Table 2.
Characteristics of 49 Patients with Non-Small Cell Lung Carcinoma and 38 Patients with Squamous Cell Carcinoma According to DNA Ploidy
| Number | Non-Small Cell 49 | Squamous Cell 38 | ||
|---|---|---|---|---|
|
| ||||
| DNA | Aneuploidy | Diploidy | Aneuploidy | Diploidy |
| Sex (M/F) | 12/2 | 32/3 | 11/0 | 26/1 |
| Age (years(SD)) | 56.7(10.9) | 56.5(8.6) | 60.5(8.3) | 57.9(8.5) |
| Smoking (Y/N) | 11/3 | 27/8 | 10/1 | 24/3 |
| Pack Years (mean(SD)) | 42.3(14.7) | 42.4(21.2)* | 43.5(14.9) | 43.1(21.6) |
| T Stage (1–4) | 1/9/3/0 | 1/28/6/0 | 0/7/3/0 | 0/21/6/0 |
| N Stage (0–2) | 7/1/5 | 15/12/8 | 6/1/3 | 11/9/7 |
| PS score# (≥80/<80) | 11/3 | 26/9 | 9/2 | 19/8 |
PS score: performance status score (Karnonfsky Scale) No variable showed significant differences.
Table 3.
Characteristics of 49 Patients with Non-Small Cell Lung Carcinoma and 38 Patients with Squamous Cell Carcinoma according to Proliferative Activity
| Number | Non-Small Cell 49 | Squamous Cell 38 | ||
|---|---|---|---|---|
|
| ||||
| Proliferative Activity | High | Low* | High | Low* |
| Sex (M/F) | 22/1 | 22/4 | 18/0 | 19/1 |
| Age (years(SD)) | 57.4(9.7) | 55.8(8.8) | 59.7(8.1) | 57.8(8.7) |
| Smoking (Y/N) | 18/5 | 20/6 | 16/2 | 18/2 |
| Pack Years (mean(SD)) | 46.4(23.2) | 38.7(14.8)* | 47.3(23.4) | 39.6(15.4) |
| T Stage (1–4) | 1/16/5/0 | 1/21/4/0 | 0/12/5/0 | 0/16/4/0 |
| N Stage (0–2) | 12/3/7 | 10/10/6 | 7/3/7 | 10/7/3 |
| PS score# (≥80/<80) | 18/4 | 19/7 | 13/5 | 15/5 |
Cut off value: median value of S phase fraction
PS score: performance status score (Karnofsky Scale) No variable showed significant differences.
In twenty-five bcl-2 positive cases, aneuploidy was noted in 40%(10/25) and high proliferative activity in 44%(11/25). Especially in cases with SQC, 47.6% (10/21) of bcl-2 positive group showed aneuploidy as opposed to 5.9%(1/17) of bcl-2 negative group (p<0.01) (Table 4). Comparing the survival time according to the ploidy pattern and proliferative activities in bcl-2 positive cases, no significant differences were noted (data not shown).
Table 4.
Distribution of 49 Patients with Non-Small Cell Lung Carcinoma and 38 Patients with Squamous Cell Carcinoma according to Status of bcl-2 Expression and DNA ploidy, Proliferative Activity
| Number | Non-Small Cell49 | Squamous Cell38 | ||
|---|---|---|---|---|
|
| ||||
| bcl-2 | Positive | Negative | Positive | Negative |
| DNA ploidy | ||||
| Aneuploidy | 10 | 4 | 10 | 1* |
| Diploidy | 15 | 20 | 11 | 16 |
| Proliferative Activity | ||||
| High | 11 | 12 | 10 | 8 |
| Low | 14 | 12 | 11 | 9 |
p<0.01,
Cutoff value: median value of S phase fraction
In Cox regression analyses with NSCLC, SQC and bcl-2 positive subsets of subjects, only T stage was entered to the equation as an independent poor prognostic indicator (Table 5). However, histologic types, N stage, status of bcl-2 expression and DNA analysis results were not entered as significant prognostic factors.
Table 5.
List of Variables Predicting Survival According to Cox Proportional hazard Model (A) in 52 Patients with Non-Small Cell Lung Carcinoma (B) in 41 Patients with Squamous Cell Carcinoma (C) in 27 Patients with bcl-2 Expressed Tumors
| Variables | Score | RegressionCoefficients* | Significance | Relative Risk | |
|---|---|---|---|---|---|
| (A) T stage | 1(≤T2) | 2(≥T3) | 1.157 | 0.055 | 3.18 |
| (B) T stage | 1(≤T2) | 2(≥T3) | 1.385 | 0.036 | 3.99 |
| (C) T stage | 1(≤T2) | 2(≥T3) | 2.012 | 0.011 | 7.48 |
Coefficient estimated by Cox proportional hazard model.
p value limit for entering covariates into the model is p<0.1
DISCUSSION
Recent studies4,18) have suggested the possible role of bcl-2 in the oncogenesis of NSCLC as well as follicular lymphoma. Pezzella et al.4) studied surgically obtained fresh frozen tissue of 122 NSCLC with their own developed anti-bcl-2 primary antibody. They yielded the positive rate of 25%(20/80) in SQC and 12%(5/42) in ADC. Gaffney et al.18) examined 51 surgical formalin fixed specimen, using the commercial primary antibody (DAKO) which is the same as the authors, and reported the positive rate of bcl-2 in NSCLC as 25.5% (SQC: 31.7%, ADC: none). In this data, we observed 52% of positive rate which is more than twice that of previous studies. As described in Methods, we applied an antigen retrieval system using a microwave oven in an enhancer solution to obtain the best quality of staining results. The differeence in positive rate of bcl-2 may be due to the actual difference of positive rate between the study populations or may be due to higher sensitivity of our staining methods. The expression of bcl-2 is not limited to NSCLC. Ikegaki et al.19) observed the bcl-2 expression in 5 of 6 cell lines of small cell lung carcinoma.
Considering the relationship of the prognosis of NSCLC and the expression of bcl-2 oncogene, Pezzella et al.4) reported that the survival in bcl-2 positive group was better than the negative group. However, Gaffney et al.18) reported no difference in survival according to the status of bcl-2 expression, and implied that their finding was more rational since the apoptosis could be regulated by other genes and modulators of bcl-2 such as bcl-x20) or Bax21). Moreover, there should be other superimposed genetic alterations other than bcl-2 which could make the DNA pattern and survival variable.
Although we lacked enough numbers in the study population to observe statistically significant survival differences, we found that there was no survival difference according to the status of bcl-2 expression. In the DNA analysis, aneuploidy and high proliferative activity were seen in about half of bcl-2 positive cases. Especially in cases with SQC, the incidence of aneuploidy was significantly higher in the bcl-2 positive group than the negative group, which could not be explained with the sole effect of bcl-2. Although we expected that there should be survival differences according to the proliferative activity or DNA ploidy even in the bcl-2 positive group, there were no statistically significant differences. However, this may be a consequence of a small number of our subjects in obtaining a clear statistical data or due to a possible bias so that we could not observe the natural course of disease because the majority of our subjects were treated surgically in their early stage.
However, there are several areas of potential concern with this study. Firstly, reflecting the higher incidence of bcl-2 expression in NSCLC, we are more concerned about the dysregulation of bcl-2 in the oncogenesis of NSCLC. Secondly, we do not know how to explain the higher cumulative dose of cigarette smoking in the bcl-2 negative group than the positive group. Although the associations of smoking with mutations of K-ras22) and p5323) have been reported, that with bcl-2 is not known to us. As results from DNA analysis suggest, examining other concurrent genetic alterations would give us a more clear idea about the biologic behavior of NSCLC.
In conclusion, with an immunohistochemical stain for bcl-2 protein on surgically obtained NSCLC specimens, we obtained 52% of positive rate. The heterogeneous DNA ploidy and proliferative activity patterns in the bcl-2 positive tumors suggested the addition of other genetic alterations. This may explain our results which showed no difference in survival according to the status of the bcl-2 expression.
Acknowledgments
This manuscript was supported by the Research Institute of Clinical Medicine, Chonnam University Hospital, Kwangju, Korea.
The authors thank F. Pezzella, M.D. for advice and suggestions and also Y.I. Go, M.D. and A.S. Jang, M.D. for faithful assistance.
Footnotes
Part of this manuscript was presented at the 1995 American Thoracic Society (ATS) International Conference, (Am J Respir Crit Care Med 1995; 151:A277)
NSCLC; Non-Small Cell lung carcinoma,
SQC: Squamous cell carcinoma, ADC: Adenocarcinoma
REFERENCES
- 1.Hockenbery D, Nunez G, Milliman C, Schreiber RD, Korsmeyer SJ. Bcl-2 is an inner mitochondrial membrane protein that blocks programmed cell death. Nature. 1990;348:334–336. doi: 10.1038/348334a0. [DOI] [PubMed] [Google Scholar]
- 2.Hockenbery DM, Zutter M, Hickey W, Nahm M, Korsmeyer SJ. BCL2 protein is topographically restricted in tissues characterized by apoptotic cell death. Proc Natl Acad Sci USA. 1991;88:6961–6965. doi: 10.1073/pnas.88.16.6961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korsmeyer SJ. Bcl-2 initiates a new category of oncogenes: regulators of cell death. Blood. 1992;80:879–886. [PubMed] [Google Scholar]
- 4.Pezzella F, Turley H, Kuzu I, Tungekar MF, Dunnill MS, Pierce CB, Harris A, Gatter KC, Mason DY. bcl-2 protein in non-small-cell lung carcinoma. N Engl J Med. 1993;329:690–694. doi: 10.1056/NEJM199309023291003. [DOI] [PubMed] [Google Scholar]
- 5.Korsmeyer SJ. Genes and neoplasia. In: Isselbacher KJ, Braunwald E, Wilson JD, Martin JB, Fauci AS, Kasper DL, editors. Harrisons principles of internal medicine. 13th ed. McGraw Hill; 1994. pp. 374–380. [Google Scholar]
- 6.McDonnell TJ, Nunez G, Platt FM, Hockenberry D, London L, McKearn JP, Korsmeyer SJ. Deregulated bcl-2-immunoglobulin transgene expands a resting but responsive immunoglobulin M and D expressing B-cell population. Molec Cell Biol. 1990;10:1901–1907. doi: 10.1128/mcb.10.5.1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDonnell TJ, Korsmeyer SJ. Progression from lymphoid hyperplasia to high-grade malignant lymphoma in mice transgenic for the t (14; 18) Nature. 1991;349:254–256. doi: 10.1038/349254a0. [DOI] [PubMed] [Google Scholar]
- 8.Mountain CF. Prognostic implications of the international staging system for lung cancer: a new international staging system for lung cancer. Semin Oncol. 1988;15:236–245. [PubMed] [Google Scholar]
- 9.Karnofsky DA, Abelmann WH, Graver LF, Burchenal JH. The use of the nitrogen mustards in the palliative treatment of carcinoma. Cancer. 1948;1:634–656. [Google Scholar]
- 10.Reed JA, Manahan LJ, Park C-S, Brigati DJ. Complete one-hour immunocytochemistry based on capillary action. Biotechniques. 1992;13:434–445. [PubMed] [Google Scholar]
- 11.Guesdon JL, Ternynck T, Avrameas S. The use of avidin-biotin interaction in immunoenzymatic techniques. J Histochem Cytochem. 1979;27:1131–1139. doi: 10.1177/27.8.90074. [DOI] [PubMed] [Google Scholar]
- 12.Hedley DW. Flow Cytometry using paraffin-embedded tissue: Five years on. Cytometry. 1989;10:229–241. doi: 10.1002/cyto.990100302. [DOI] [PubMed] [Google Scholar]
- 13.Coon JS, Landay AL, Weinstein RS. Flow cytometric analysis of paraffin embedded tumors. Implications for diagnostic pathology. Human Pathol. 1986;177:435–437. doi: 10.1016/s0046-8177(86)80029-6. [DOI] [PubMed] [Google Scholar]
- 14.Vindelov LL, Christensen IJ, Nissen NI. A detergent-trypsin method for preparation of nuclei for flow cytometric DNA analysis. Cytometry. 1983;3:323–327. doi: 10.1002/cyto.990030503. [DOI] [PubMed] [Google Scholar]
- 15.Hedly DW, Friedlander ML, Taylor IW, Rugg CA, Musgrove EA. Method for analysis of cellular DNA content of paraffin-embedded pathological material using flow cytometry. J Histochem Cytochem. 1983;31:1333–1335. doi: 10.1177/31.11.6619538. [DOI] [PubMed] [Google Scholar]
- 16.Dixon WJ. BMDP user’s digest quick reference for the BMDP programs to accompany BMDP software release 7.0. University of Califormia press; 1992. [Google Scholar]
- 17.Pezzella F, Tse AG, Cordell JL, Pulford KA, Gatter KC, Mason DY. Expression of the bcl-2 oncogene protein is not specific for the 14;18 chromosomal translocation. Am J Pathol. 1990;137:225–232. [PMC free article] [PubMed] [Google Scholar]
- 18.Gaffney EF, O’Neill AJ, Staunton MJ. bcl-2 and prognosis in non-small-cell lung carcinoma (letter) N Engl J Med. 1994;330(24):1757. [PubMed] [Google Scholar]
- 19.Ikegaki N, Katsumata M, Minna J, Tsujimoto Y. Expression of bcl-2 in small cell lung carcinoma cells. Cancer Research. 1994;54:6–8. [PubMed] [Google Scholar]
- 20.Boise LH, Gonzalez-Garcia M, Postema CE, Ding L, Lindsten T, Turka LA, Mao X, Nunez G, Thompson CB. bcl-x a bcl-2 related gene that functions as a dominant regulator of apoptotic cell death. Cell. 1993;74:597–608. doi: 10.1016/0092-8674(93)90508-n. [DOI] [PubMed] [Google Scholar]
- 21.Oltvai ZN, Milliman CL, Korsmeyer SJ. Bcl-2 Heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell. 1993;74:609–619. doi: 10.1016/0092-8674(93)90509-o. [DOI] [PubMed] [Google Scholar]
- 22.Westra WH, Slebos RJ, Offerhaus GJ, Goodman SN, Evers SG, Kensler TW, Askin FB, Rodenhuis S, Hruban RH. K-ras oncogene activation in lung adenocarcinomas from former smokers. Evidence that K-ras mutations are an early and irreversible event in the development of adenocarcinoma of the lung. Cancer. 1993;72:432–438. doi: 10.1002/1097-0142(19930715)72:2<432::aid-cncr2820720219>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 23.Westra WH, Offerhaus GJ, Goodman SN, Slebos RJ, Polak M, Baas IO, Rodenhuis S, Hruban RH. Overexpression of the p53 tumor suppressor gene product in primary lung adenocarciomas is associated with cigarette smoking. American Journal of Surgical Pathology. 1993;17:213–220. doi: 10.1097/00000478-199303000-00001. [DOI] [PubMed] [Google Scholar]


