Abstract
Objectives
Head-up tilt test (HUT) has been reported to be useful in the evaluation of syncope of unknown origin (SUO). However, the sensitivity of HUT with no pharmacologic provocation was relatively low and variable, ranging 32–70%. Therefore, several protocols of HUT with different degrees and durations of the tilt and modes of provocation were proposed. The purpose of this study was to determine the value of the multi-stage head-up tilt test with isoproterenol provocation (HUT-isp) in the evaluation of SUO and drug efficacy.
Methods
Sixty-seven patients presenting with SUO and 30 control subjects with no history of syncope underwent the HUT-isp. Blood pressure (BP) was measured every 2 min and whenever the patient complained of any symptom, and cardiac rhythm was continuously monitored. The HUT-isp consisted of 3 stages: first for 20 min with no provocation, second and third stages with infusion of isoproterenol for 10 min each at a rate of 2 μg/min and 5 μg/min, respectively. A positive HUT-isp was defined when syncope or presyncope was reproduced, accompanied by hypotension (< 80 mmHg) or bradycardia (< 40/min) or both, and positive responses were classified into vasodepressive, cardioinhibitory and mixed type.
Results
The HUT-isp was positive in 56 (83.6%) of 67 patients with SUO and 10 (33.3%) of 30 control subjects. The type of positive responses was vasodepressive in 41 (73.2%), cardioinhibitory in 4 (7.1%) and mixed in 11 (19.6%). The sensitivity of the HUT-isp in diagnosing vasovagal syncope was 83.6%, specificity 66.7% and positive predictive value 84.8%. Positive responses were developed most frequently in the 3rd stage: 76.8% in patients, 70% in controls. The effect of 3 drugs (carteolol, aminophylline and disopyramide) was evaluated in 27 patients with a repeat HUT-isp. Carteolol was effective in 12 (85.7%) of 14 patients, disopyramide in 7 (58.3%) of 12 and aminophylline in 1 (14.3%) of 7. During the follow-up period of 175±212 days (26–623 days), none of the 20 patients with a negative repeat HUT-isp developed a recurrent syncope.
Conclusion
The HUT-isp is thought safe and useful to evaluate syncope of unknown origin and to guide effective drug therapy.
Keywords: Head-up tilt test, Vasovagal syncope, Isoproterenol
INTRODUCTION
Syncope is one of common medical problems, defined as a sudden and temporary loss of consciousness with a deficit of postural tone which is spontaneously recovered without electrical or chemical cardioversion1,2). Syncope is experienced by 3% of adult males and 3–5% of adult females and syncope is the main reason for admission in 1% of inpatients of general hospitals and in 3% of patients visiting an emergency room3).
The cause of syncope is often very difficult to determine. Therefore, syncope remains still unexplained in 40–50% of the cases, in spite of thorough noninvasive and invasive diagnostic investigations, because the mechanism or cause of syncope is various and complex, the episodes are brief and unpredictable, spontaneous remission rate is high and there is no reliable diagnostic method4–7).
Unexplained syncope or syncope of unknown origin (SUO) has been most commonly reported to be vasovagal syncope and head-up tilt test (HUT) has been utilized as a valuable diagnostic test of vasovagal syncope2,8–13). The sensitivity of HUT, however, is rather low, ranging from 32 to 70%. Therefore, several protocols of HUT with or without pharmacologic provocation were developed to improve the sensitivity, thereby reaching 90%2,8–16). This study was performed to determine the value of the HUT-isp in evaluation of patients with SUO and predicting the efficacy of long-term drug therapy using beta-blocker, aminophylline or disopyramide.
SUBJECTS AND METHODS
1. Subjects
From Oct., 1993 through July, 1995 at the Chonnam University Hospital, 67 patients (31 males, 36 females; mean age: 37±23 years) presenting with one or more episodes of syncope and 30 control subjects (18 males, 12 females; mean age: 39±18 years) with no history of syncope were included in this study. The patients were thoroughly evaluated with a physical examination, including neurologic examination, blood chemistry, standard 12-lead EKG, signal averaged EKG, Holter monitoring and echocardiography. CT scan and/or magnetic resonance imaging of the brain and clinical electrophysiologic study were also performed in some patients, if indicated. All the patients had no underlying structural and electrical heart disease.
2. Multi-Stage Head-up Tilt Test with Isoproterenol Provocation (HUT-isp)
The manually operated tilt table with a supporting foot board and belts to prevent a patient from falling down was designed and used in this study. Head-up tilt test was performed at 80 degrees after securing an intravenous line to the arm vein, with monitoring the cardiac rhythm continuously and atropine standby. Blood pressure (BP) was monitored with a noninvasive BP monitor (Dynamap®, Criticon, USA) every 2 min and whenever the patient complained of any symptom. Cardiac rhythm was continuously monitored with an EKG monitor-defibrillator (Lifepak-9B®, Physiocontrol, USA). The HUT-isp consisted of 3 stages: first stage for 20 min with no pharmacologic provocation, second and third with infusion of isoproterenol. If the baseline HUT was negative, then isoproterenol was infused at a rate of 2 μg/min (2nd stage) and 5 μg /min (3rd stage) using an infusion pump, and the patient was tilted again for 10 minutes in each stage. The patient was kept lying flat for 10 minutes between each stage. If frank syncope or imminent syncope occurred, the tilt table was lowered to horizontal position immediately (< 10 sec).
Positive responses to the HUT-isp were classified into 3 types, based on the previously reported criteria17); vasodepressive type was defined when systolic BP fell more than 30 mmHg compared with the baseline systolic BP or systolic BP fell down to < 80 mmHg; cardioinhibitory type, HR fell down to < 40/min; mixed type, when both vasodepressive and cardioinhibitory responses occurred.
3. Assessment of Drug Effect of Vasovagal Syncope
The short-term drug effect was assessed by a repeat HUT-isp after administering one of 3 drugs: carteolol (Mikelan®), aminophylline (Asthcontin®) and disopyramide for 2–4 weeks. The long-term efficacy of drug therapy was assessed by following the patients who were on one of 3 drugs for recurrence of syncope and side effects of the drug.
4. Statistical Analysis
The Student t-test was used to evaluate the difference of numeric parameters between groups. The p-value less than 0.05 was considered significant.
RESULTS
Twenty-nine out of 67 patients presenting with SUO had various prodromal symptoms such as palpitation in 12 patients, cold sweating in 10, dizziness in 9, dyspnea in 8, nausea in 5, abdominal pain in 2, general weakness in 2 and visual blurring in 2.
Thirty-six patients who developed syncope during the HUT-isp complained of various discomforts such as dizziness in 24 patients, nausea in 18, blurred vision in 14, diaphoresis in 12, headache in 2 and general weakness in 2, as a prodromal symptom. Fifty-six (83.6%) of 67 patients developed positive vasovagal response to the HUT-isp, which was also observed in 10 (33.3%) of 30 control subjects (Table 1). Type of positive responses in the patient group (n=56) was vasodepressive type in 41 (73.2%), mixed in 11 (19.6%), and cardioinhibitory in 4 (7.1%) (Table 1). The sensitivity of the HUT-isp was 83.6%, specificity 66.7%, accuracy 78.4% and positive predictive value 84.8%.
Table 1.
The Results of the HUT-isp in Patients with SUO and Control Subjects
| SUO group (n=67) | Control group (n=30) | p value | |
|---|---|---|---|
| Positive HUT-isp | 56 (83.6%) | 10 (33.3%) | < 0.001 |
| at stage 1 | 4 (7.1%) | 2 (20.0%) | NS |
| stage 2 | 9 (16.1%) | 1 (10.0%) | NS |
| stage 3 | 43 (76.8%) | 7 (70.0%) | NS |
| types | |||
| vasodepressive | 41 (73.2%) | 3 (30.0%) | < 0.001 |
| cardioinhibitory | 4 (7.1%) | 1 (10.0%) | NS |
| mixed | 11 (19.6%) | 6 (60.0%) | < 0.001 |
NS: non-significant
The positive responses in patients group were developed in the 3rd stage in 43 (76.8%) patients, 2nd stage in 9 (16.1%), and 1st stage in 4 (7.1%) and, in control subjects, 3rd stage in 7 (70%), 2nd stage in 1 (10%), and 1st stage in 2 (20%). There was no significant difference in the degree of fall in BP and HR at the onset of positive responses between patients group and control group (Table 2).
Table 2.
The Degree of Drop in Blood Pressure and Heart Rate at the Onset of Vasovagal Responses during the HUT-isp
| SUO group (n=56) | Control group (n=10) | p value | |
|---|---|---|---|
| ΔBP (mmHg) | |||
| systolic | 41.7±17.4 | 39.7±19.8 | NS |
| mean | 28.9±13.0 | 23.2±20.0 | NS |
| ΔHR (beats/min) | 38.9±28.3 | 34.9 ±24.0 | NS |
NS: non-significant, BP: blood pressure, HR: heart rate
One of 3 drugs (carteolol 10 mg/day, aminophylline 450 mg/day, disopyramide 300 mg/day) was randomly given to the 56 patients with a positive HUT-isp and their short-term effect was evaluated with a repeat HUT-isp in 27 patients after 2–4 weeks on medication (Fig. 1). Carteolol turned out to be effective in 12 (85.7%) of 14 patients, aminophylline in 1 (14.3%) of 7 and disopyramide in 7 (58.3%) of 12 (Fig. 1, 2). None of the 20 patients in whom the repeat HUT-isp became negative after medication developed a recurrent syncope during the follow-up period of 175±212 days (26–623 days).
Fig. 1.
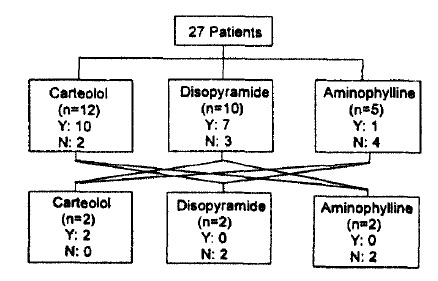
The results of serial drug testing with a repeat HUP-isp in the 27 patients. Y: effective, N: ineffective. Each line between boxes denotes a case allocated to the other drug.
Fig. 2.
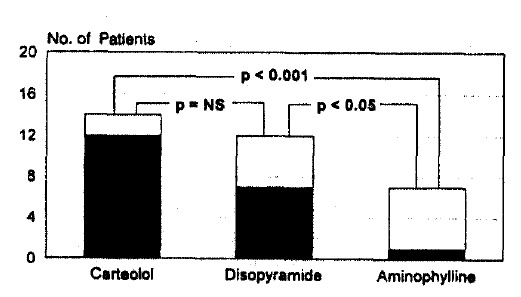
Evaluation of drug effect with a repeat HUT-isp. Carteolol is most effective in preventing vasovagal syncope.
DISCUSSION
Syncope is caused by various cardiac and non-cardiac diseases. Aortic stenosis, pulmonary embolism, mitral stenosis, ventricular tachycardia, cardiac conduction disturbances, myocardial infarction and mitral valve prolapse are reported as important causes of cardiac syncope. Non-cardiac causes of syncope are epilepsy, postural hypotension, cerebrovascular disease, carotid sinus hypersensitivity, vasovagal syncope, drug, hyperventilation and hypoglycemia3,18). However, vasovagal syncope is known as the most common cause of syncope in otherwise healthy people. Recently, HUT has been used as a useful test to evaluate patients with unexplained syncope, although the underlying mechanisms of tilt-induced hypotension in patients with vasovagal syncope are not clearly understood yet19).
When a normal man is standing, about 300 to 800 ml of blood is pooled in the lower extremities, resulting in decrease of venous return, cardiac output and temporary decrease of the arterial blood pressure in order. This is normally compensated by baroreceptor reflex-mediated increase in the sympathetic outflow that increases cardiac contractility, heart rate and peripheral vascular resistance. However, in a susceptible subject, activation of the left ventricular mechanoreceptors (C-fibers) due to increased cardiac contractility could override the baroreceptor reflex, resulting in peripheral vasodilation and/or bradycardia due to the resultant diminution of sympathetic tone and enhancement of parasympathetic activity20,21,34,38,40).
Several protocols of HUT which are different in tilt angle, duration of the test and drug used for provocation have been reported. We performed HUT with isoproterenol provocation to stimulate the mechanoreceptors in the heart more vigorously and to thereby reproduce reflex vasodilation and/or bradycardia22).
In our study, the HUT-isp was positive in 83.6% of SUO patients and in 33.3% of control subjects. Therefore, the sensitivity of our protocol of HUT-isp in diagnosing vasovagal syncope from SUO was 83.6%, specificity 66.7%, accuracy 78.4% and positive predictive value 84.8%. Four (7.1%) of the 56 patients with a positive HUT-isp were positive in the 1st stage of the HUT-isp with no isoproterenol infusion. The positive rate of 7.1% in baseline HUT with no provocation in our study is much lower than the 32–70% which were previously reported by other investigators2,8–16,22–27). This difference may be explained partly by the fact that this study included patients with only one episode of syncope and the duration of the baseline tilt was shorter than the others (20 min vs 40–60 min). According to the reports, the false positive rate of HUT ranged from 5 to 15%, which largely depends on the duration (30–90 min) and the tilt angle (40–80 degrees)2,10–12,23–25). In our study, false positive rate was 33.3%, which is somewhat higher than that of the previous report12). This relatively high false positive rate in our study was thought to be caused by the higher tilt angle (80 degrees) and higher infusion dose of isoproterenol.
Several studies have reported that beta-adrenergic receptor blockers, aminophylline or disopyramide can be used for long-term management of vasovagal syncope23,28). The exact mechanisms by which these drugs prevent vasovagal syncope are unclear. It has been, however, suggested that beta-blockers can lower the discharge frequency of mechanoreceptors and by allowing unopposed activation of alpha receptors, also elicit a peripheral vasoconstriction34,35). Disopyramide is known to have negative inotropic, anticholinergic and peripheral vasoconstricting effects, which may account for its efficacy in preventing vasovagal syncope36). Theophylline is the selective antagonist of adenosine A1 receptor through which adenosine evokes negative inotropic and chronotropic effect on the heart37). Adenosine is an endogenous cardioprotective agent, particularly in the event of myocardial ischemia. Although the exact role of adenosine in vasovagal syncope has not been determined yet, prevention of vasovagal syncope with theophylline has been reported.
In this study, carteolol, a beta-blocker, was most effective in preventing vasovagal syncope. The efficacy of oral disopyramide and aminophylline in preventing vasovagal syncope was reported to be 100% and 82%, respectively, in some uncontrolled trials28,37,41). In contrast, disopyramide was effective in 58% of the patients and aminophylline in 14% in our series. But this result should be interpreted with great caution because these drugs were administered in a small number of patients (12 and 7 cases, respectively) and more importantly, blood level of the drugs was not monitored. The cardiac pacing is barely used since it is not effective in preventing syncope. It is, however, applied to selected patients whose bradycardia or asystole are very serious in order to prevent sudden death2,23,29).
It is noteworthy that none of the patients who were put on one of 3 drugs based on the results of a repeat HUT-isp to evaluate the short-term drug effect developed a recurrent syncope. This finding is strong evidence that the HUT-isp can be used to assess and guide the long-term drug therapy in patients with vasovagal syncope.
LIMITATIONS
This study has some limitations. First of all, patients with only one episode of syncope were included, even though the episode was very recent (< 4 weeks). Inclusion of this patient population may increase false negativity or positivity of the test since non-recurrent syncope may be provoked by a transient derangement of autonomic nervous system which will neither persist nor recur after recovering from the syncope. Second, our protocol of the HUT-isp is rather aggressive in terms of tilt angle (80 degrees) and isoproterenol infusion dose (5 μg/min), which may contribute relatively high false positivity of our HUT-isp. Third, drug effect was tested without confirming whether the therapeutic blood level of the drugs was achieved or not. Nevertheless, long-term drug therapy based on the results of serial drug testing with a repeat HUT-isp was very successful.
CONCLUSIONS
Data from the present study suggest that the HUT-isp is safe and useful to evaluate patients with syncope of unknown origin and to guide long-term drug therapy in vasovagal syncope. However, further studies are needed to improve both sensitivity and specificity of the test and to standardize the protocol.
REFERENCES
- 1.Kapoor WN. Hypotension and syncope. In: Braunwald E, editor. Heart disease: A Textbook of Cardiovascular Medicine. WB Saunders Co; Philadelphia PA: 1991. pp. 875–876. [Google Scholar]
- 2.Abi-Samra F, Maloney JD, fouad-Tarazi FM, Castle LW. The usefulness of head-up tilt testing and hemodynamic investigations in the work-up of syncope of unknown origin. PACE. 1988;11:1202–1204. doi: 10.1111/j.1540-8159.1988.tb03973.x. [DOI] [PubMed] [Google Scholar]
- 3.Day SC, Cook EF, Funkenstein H, Goldman L. Evaluation and outcome of emergency room patients with transient loss of consciousness. Am J Med. 1982;73:15–23. doi: 10.1016/0002-9343(82)90913-5. [DOI] [PubMed] [Google Scholar]
- 4.Kapoor WN, Karpf M, Wieand S, Peterson JR, Levey GS. A prospective evaluation and follow up of patients with syncope. N Engl J Med. 1983;309:197–204. doi: 10.1056/NEJM198307283090401. [DOI] [PubMed] [Google Scholar]
- 5.Eagle KA, Black HR. The impact of diagnostic tests in evaluating patients with syncope. Yale J Biol Med. 1983;56:1–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Silverstein MD, Singer DE, Mulley AG, Thibault GE, Barnett GO. Patients with syncope admitted to medical intensive care units. JAMA. 1982;248:1185–1189. [PubMed] [Google Scholar]
- 7.Martin GJ, Adams SL, Martin HG, Mathews J, Zull D, Scanlon PJ. Prospective evaluation of syncope. Ann Emerg Med. 1984;13:499–504. doi: 10.1016/s0196-0644(84)80511-9. [DOI] [PubMed] [Google Scholar]
- 8.Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R. Methodology of head-up tilt in patients with unexplained syncope. J Am Coll Cardiol. 1991;17:125–130. doi: 10.1016/0735-1097(91)90714-k. [DOI] [PubMed] [Google Scholar]
- 9.Kenny RA, Ingram A, Bayliss J, Sutton R. Head-up tilt: a useful test for investigating unexplained syncope. Lancet. 1986;1:1352–1354. doi: 10.1016/s0140-6736(86)91665-x. [DOI] [PubMed] [Google Scholar]
- 10.Raviele A, Gasparini G, DiPede F, Delise P, Bonso A, Piccolo E. Usefulness of head up tilt test in evaluating patients with syncope of unknown origin and negative electrophysiologic study. Am J Cardiol. 1990;65:1322–1327. doi: 10.1016/0002-9149(90)91321-v. [DOI] [PubMed] [Google Scholar]
- 11.Strasberg B, Rechavia E, Sagie A, Kusniec J, Mager A, Sclarovsky S, Agmon J. The head up tilt table test in patients with syncope of unknown origin. Am Heart J. 1989;118:923–927. doi: 10.1016/0002-8703(89)90225-1. [DOI] [PubMed] [Google Scholar]
- 12.Almquist A, Goldenberg IF, Milstein S, Chen MY, Chen XC, Hansen R, Gornick CC, Benditt DG. Provocation of bradycardia and hypotension by isoproterenol and upright posture in patients with unexplained syncope. N Engl J Med. 1989;320:346–351. doi: 10.1056/NEJM198902093200603. [DOI] [PubMed] [Google Scholar]
- 13.Grubb BP, Temesy-Armos P, Hahn H, Elliot L. Utility of upright tilt testing in the evaluation and management of syncope of unknown origin. Am J Med. 1991;90:6–10. doi: 10.1016/0002-9343(91)90499-n. [DOI] [PubMed] [Google Scholar]
- 14.Waxman MB, Yao L, Cameron DA, Wald RW, Roseman J. Isoproterenol induction of vasodepressor type reaction in vasodepressor prone persons. Am J Cardiol. 1989;63:58–65. doi: 10.1016/0002-9149(89)91076-x. [DOI] [PubMed] [Google Scholar]


