Abstract
A 38-year-old man was admitted with coingestive heart failure due to infective endocarditis. Echocardiography with color Doppler imaging revealed severe aortic regurgitation, mitral valve premature closure and diastolic mitral regurgitation. The flow of the diastolic mitral regurgitation was directed to the posterior wall of the left atrium through just behind the posterior mitral leaflet. The diastolic mitral regurgitation was observed only in the period of late diastole and no mitral regurgitation could be detected in the systolic phase. After successful aortic valve replacement, the diastolic mitral regurgitation disappeared completely.
Keywords: Diastolic mitral regurgitation, Acute aortic regurgitation, Aortic valve replacement, Color Doppler echocardiography
INTRODUCTION
Diastolic mitral regurgitation has been described in patients with acute aortic regurgitation and those with atrioventricular block or atrial fibrillation with slow ventricular responses1–3). Evidence of diastolic mitral regurgitation in these patients has been demonstrated previously by left ventriculography and recently by pulse Doppler echocardiography4,5). The mechanisms of diastolic mitral regurgitation in patients with acute aortic regurgitation have been considered to be the summation of the following pathophysiology: reversed atrio-ventricular pressure gradient due to aortic regurgitation in the non-compliant ventricle, increased mitral annulus due to ventricular relaxation and lack of papillary muscle tension6,7). That of the patients with atrioventricular block or atrial fibrillation has been considered to be lack of atrial factors for mitral valve closure8). We documented diastolic mitral regurgitation by color Doppler echocardiography in a patient with acute aortic regurgitation. Color Doppler flow imaging is highly useful in detecting valvular regurgitation, especially in determining flow direction. Therefore, this technique may provide additional information regarding the mechanism by which diastolic mitral regurgitation is produced. Reversibility of diastolic mitral regurgitation after correction of hemodynamic loading, that was widely believed but not actually demonstrated, was also observed.
CASE REPORT
A 38-year-old japanese man with no previous cardiovascular disease was admitted to our hospital because of paroxysmal nocturnal dyspnea and low grade fever of four weeks duration. He had the history of the resection of subcutaneous abscess in the neck, several days before the onset of symptom. On admission, blood pressure was 104/40mmHg with a regular pulse of 102/min. His body temperature was 37.4C. An early systolic murmur and a diastolic blowing murmur with thrill were detected at the left parasternal border. Increased pulmonary vascular marking was observed in his chest X-ray and the cardio-thoracic ratio was 50%. Electrocardiogram revealed a prolonged P-Q interval of 0.28 second, left ventricular hypertrophy and ST depression in the left precordial leads. After admission, first-degree of atrioventricular block normalized in 0.18 second of P-Q interval. Echocardiography was performed with a Tohshiba 65A after normalization of P-Q interval, which revealed the dilated and hyperkinetic left ventricle and the slightly dilated left atrium. M-mode echocardiography showed premeature mitral valve closure (Fig. 1), and the left ventricular end diastolic dimension was 6.4 cm and the end systolic dimension was 4.4 cm. The right coronary cusp and left coronary cusp of the aortic valve were extremely elongated and the left Valsalva sinus was dilated. Both aortic cusps were prolapsing and no coaptation was seen. Severe aortic regurgitation was observed on color Doppler flow imaging. In late diastole, mitral regurgitation which ran just behind the posterior mitral leaflet and extended to the posterior wall of the left atrium was detected (Fig. 2-A). The diastolic mitral regurgitation began with the atrial systole and disappeared with the ventricular systole (Fig. 2-B).
Fig. 1.
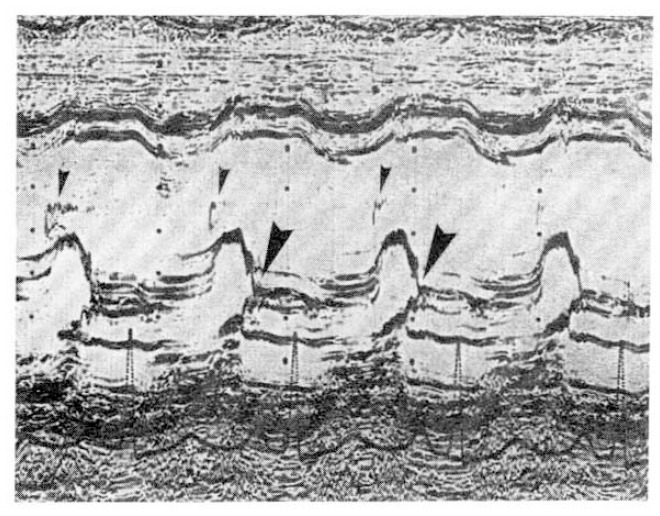
M-mode tracing of the mitral valve revealed mitral valve premature closure (large arrow head). The P-Q interval was 0.18 second. The prolapsing cusp of the aortic valve was also observed (small arrow head).
Fig. 2.
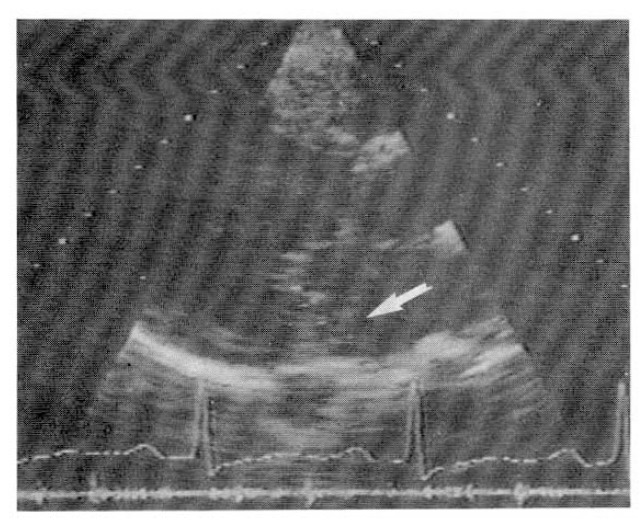
Two-dimensional color Doppler echocardiography revealed left ventricular enlargement and mitral regurgitation running just behind the posterior mitral leaflet and reaching the posterior atrial wall (arrow).
Although several blood cultures were all negative, the diagnosis of acute aortic regurgitation due to infective endocarditis was made from the clinical history and destructive changes of the aortic valve. After intensive antibiotic therapy for three weeks, aortic valve replacement was performed. At surgery, commissural rupture between the right coronary cusp and the left coronary cusp was detected and an abscess was present in the root of the left coronary cusp. No abnormalities were detected in the mitral apparatus. After aortic valve replacement, the diastolic mitral regurgitation disappeared completely.
DISCUSSION
Diastolic mitral regurgitation in patients with acute aortic reguritation in patients with acute aortic regurgitation is considered to be produced by hemodynamic abnormalities, not by intrinsic abnormalities of mitral leaflets. However, the proof of this consideration is somewhat obscure. In most reported cases with diastolic mitral regurgitation, the concurrent presence of systolic mitral regurgitation, which indicates the presence of intrinsic abnormalities of mitral leaflets or apparatus, was reported2–5,7). If the mitral valve is truly normal, systolic mitral regurgitation should be absent and diastolic mitral regurgitation should disappear with resolution of the hemodynamic abnormalities.
The reversibility of diastolic mitral regurgitation after aortic valve replacement has never been described. In this case, the mitral regurgitation was observed only in the period of late diastole, disappearing with the ventricular systole. Furthermore, the diastolic mitral regurgitation in this case could not be detected after the successful aortic valve replacement. Our case clearly indicates that acute aortic regurgitation can produce diastolic mitral regurgitation in a normal mitral valve.
In this case, the flow of the diastolic mitral regurgitation was directed to the posterior wall of the left atrium through just behind the posterior mitral leaflet. From above mentioned mechanisms of diastolic mitral regurgitation in acute aortic regurgitation, if intrinsic abnormalities of the mitral leaflets are absent, regurgitant flow should be directed to the center of the left atrium. Extreme deviation of mitral regurgitant flow is observed in cases of mitral valve prolapse or those with severely restricted mitral valve leaflets, as is seen in rheumatic mitral disease. Because this case showed no abnormalities in the mitral leaflets under echocardiography, severely restricted movement of the mitral leaflets is unlikely. We speculated either that the aortic regurgitant jet might depress the anterior mitral leaflet toward the left atrium or that acute left ventricular enlargement due to aortic regurgitation might retract the chordae connecting to the posterior mitral leaflet9). These processes would result in the dislodgment of the tips of both leaflets, creating extreme deviation of the mitral regurgitant flow similar to mitral prolapse. There are a few reports on the observation of diastolic mitral regurgitation by color Doppler echocardiography, but no comments for the flow direction10). We focused on the flow direction of diastolic mitral regurgitation using color Doppler echocardiography. This case indicated the possibility of additional mechanisms of diastolic mitral regurgitation, namely, depression of the anterior mitral leaflet or retraction of the chordae connecting to the posterior mitral leaflet.
Color Doppler echocardiography is useful for the evaluation of diastolic mitral regurgitation. This technique may provide more precise infomation on the mechanisms of diastolic mitral regurgitation.
Fig. 3.
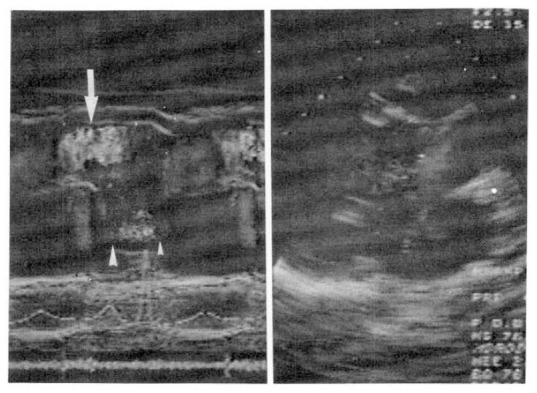
M-mode color Doppler tracing clarified the relationship between the diastolic mitral regurgitation and the events of the cardiac cycle. The diastolic mitral regurgitation began with the P wave (large arrow head) and disappeared with ventricular systole (small arrow head). Aortic regurgitant flow was also observed (arrow).
REFERENCES
- 1.Lochaya S, Igarashi M, Shaffer AB. Late diastolic mitral regurgitation secondary to aortic regurgitation: Its relatioinship to Austin Flint murmur. Am Heart J. 1967;74:161. doi: 10.1016/0002-8703(67)90273-6. [DOI] [PubMed] [Google Scholar]
- 2.Panidis IP, Ross J, et al. Diastolic mitral regurgitation in patients with atrioventricular conduction abnormalities: A common finding by Doppler echocardiography. J Am Coll Cardiol. 1986;7:768. doi: 10.1016/s0735-1097(86)80335-7. [DOI] [PubMed] [Google Scholar]
- 3.Sanada J, Kawahira M, et al. Late diastolic mitral regurgitation studied by pulsed Doppler echocardiography. Am J Cardiol. 1987;59:1366. doi: 10.1016/0002-9149(87)90921-0. [DOI] [PubMed] [Google Scholar]
- 4.Wong M. Diastolic mitral regurgitaiton. Haemodynamic and angiographic correlation. Brit Heart J. 1969;31:468. doi: 10.1136/hrt.31.4.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnittger I, Appleton CP, et al. Diastolic mitral and tricuspid regurgitation by Doppler echocardiography in patients with atrioventricular block: New insight into the mechanism of atrioventricular valve closure. J Am Coll Cardiol. 1988;11:83. doi: 10.1016/0735-1097(88)90170-2. [DOI] [PubMed] [Google Scholar]
- 6.Oliver GC, Gazetopoulos N, Deuchar C. Reversed mitral diastolic gradient in aortic incompetence. Brit Heart J. 1967;29:239. doi: 10.1136/hrt.29.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Downes TR, Nomeir AM, et al. Diastolic mitral regurgitation in acute but not chronic aortic regurgitation: Implications regarding the mechanism of mitral closure. Am Heart J. 1989;117:1106. doi: 10.1016/0002-8703(89)90869-7. [DOI] [PubMed] [Google Scholar]
- 8.Little RC. The mechanism of closure of the mitral valve: A continuing controversy. Circulation. 1979;59:615. doi: 10.1161/01.cir.59.4.615. [DOI] [PubMed] [Google Scholar]
- 9.Kaul S, Pearlman JD, et al. Prevalence and mechanisms of mitral regurgitation in the absence of intrinsic abnormalities of the mitral leaflets. Am Heart J. 1989;118:963. doi: 10.1016/0002-8703(89)90231-7. [DOI] [PubMed] [Google Scholar]
- 10.Covalesky VA, Ross J, Chandrasekaran K, Mintz GS. Detection of diastolic atrioventricular valvular regurgitation by “M-mode” color Doppler echocardiography. Am J Cardiol. 1989;64:809. doi: 10.1016/0002-9149(89)90771-6. [DOI] [PubMed] [Google Scholar]


