Abstract
Background:
The British Lung Foundation highlighted Southampton City as a hotspot for patients at future risk of chronic obstructive pulmonary disease (COPD) exacerbations due to severe deprivation levels and a high undiagnosed level of disease based on health economic modelling. We developed a strategy spanning primary and secondary care to reduce emergency admissions of patients with acute exacerbations of COPD and increase the diagnosed prevalence of COPD on general practitioner (GP) registers closer to that predicted from local modelling.
Methods:
A comprehensive 3-year audit of admissions was performed. Patients who had been admitted with an exacerbation to University Hospital Southampton three or more times in the previous 12 months were cohorted and cared for in a consultant-led, but community based, COPD service. Within primary care, a programme of education and case-based finding was delivered to most practices within the city.
Results:
Thirty-four patients were found to be responsible for 176 admissions (22% of total COPD admissions) to the hospital. These 34 patients required 185 active interventions during the 12-month period but only 39 hospital admissions. The 30-day readmission rate dropped from 13.4 to 1.9% (P<0.01), confirming the contribution the cohort made to readmissions. Prior to the project, the registered Quality Outcomes Framework prevalence of COPD within the city was 1.5; after just 1 year of the project, the prevalence increased from 1.5 to 2.27%.
Conclusions:
The use of medical intelligence to investigate the underlying processes of COPD hospital admissions led to an effective intervention delivered in a consultant-led model.
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are the second most common reason for patients to be admitted to the emergency department in the United Kingdom1 and cost up to £800 million to the NHS.2–4 There are very few published peer-reviewed papers on admission avoidance strategies. Recent papers have investigated the use of telehealth5 and self-management plans6 with mixed results. Self-management especially has caused recent controversy, with some studies showing a decrease in hospitalisation,7 some showing little or no impact8 and some showing possible harm.9
Southampton was identified1 as having the highest at-risk population for future admissions for an acute exacerbation of chronic obstructive pulmonary disease (COPD) on the South Coast. This was due to the high smoking prevalence and higher than average deprivation levels within the city.4 There was also a lower than expected recorded prevalence of COPD within the city, suggesting that diagnostic processes were not working effectively.1
Currently, there are 835,000 people diagnosed with COPD in the United Kingdom and an estimated 2,200,000 people with COPD who remain undiagnosed, which is equivalent to 13% of the population of England aged 35 years and over.10
Our aim for this 12-month project was to make an impact on three specific areas of COPD care. These were as follows: (i) improving the diagnosis of COPD, (ii) facilitating optimal management of COPD patients in primary care, and (iii) identifing the main drivers behind the COPD admissions to University Hospital Southampton Foundation Trust and instigating an appropriate strategy to reduce them.
Materials and Methods
This project was consultant led and co-delivered with a full-time equivalent respiratory nurse specialist in COPD and a specialist registrar in respiratory medicine. Existing community teams (comprising four full-time equivalent specialist nurses) were also involved in delivering parts of the project across both primary and secondary care.
The project was broken down into two specific work streams. The first was working with primary care to improve the diagnosis and management of COPD.
This part of the project was delivered within general practices lying within the boundaries of Southampton City PCT. We utilised Doctor Foster Reports (provider of health-care information in the United Kingdom), practice-level Quality Outcomes Framework reports (a voluntary annual reward and incentive programme for all general practitioner (GP) surgeries in England, detailing practice achievement results) and Hospital Episode Statistics (a data warehouse containing details of all admissions, outpatient appointments and Emergency Department attendances at NHS hospitals in England) to evaluate how the practices differed in their disease prevalence and analyse hospital admission episodes. Practices that had a lower than average diagnosed disease prevalence and a higher than average admission statistics were prioritised for intervention. Baseline Quality Outcomes Framework prevalence of COPD was monitored each quartile for 1 year. Bias was minimised with results being assessed by an independent data manager within University Hospital Southampton.
The team visited each surgery to evaluate how the practice managed respiratory disease. At these visits the following work packages were offered.
1. GP and nurse education. This was delivered on the diagnosis and management of COPD. This comprised lectures delivered to nurses within surgeries reinforced with interactive CD-ROMS and an educational web portal www.copdeducation.org.uk. The GPs were educated by consultants through large regional teaching groups and focused work within surgeries.
2. Within-practice education on spirometry—including calibration and interpretation. This was performed on their own in house spirometer to ERS taskforce guidelines11 and interpretation in line with NICE 2010.12
3. Review of patients on the COPD register. This was to confirm diagnosis and optimise treatment in line with the NICE 2010 guidelines.12
4. Within-practice screening programs. These were carried out on patients with significant smoking history (>10 pack years), aged >45 years, with a previous history of chest infection treated by their GP in the last year without a diagnosis of airways disease.
The second work stream was delivered within the University Hospital Southampton Foundation Trust, a large teaching hospital on the outskirts of the city centre, and the main hospital accepting admissions from Southampton City PCT.
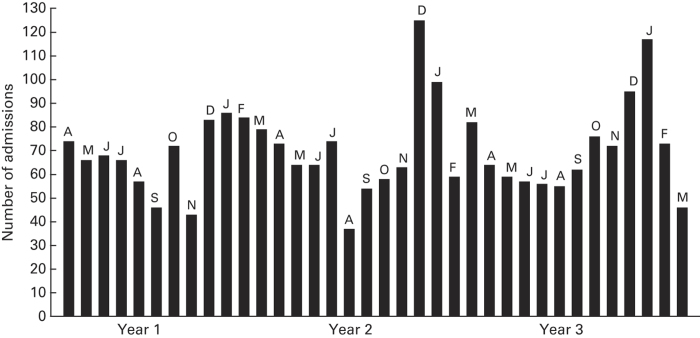
This part of the project concentrated on the main drivers behind admissions with acute exacerbations. We performed a comprehensive review of all COPD admissions to the trust from the previous 3 years. Each and every admission was confirmed by accessing individual notes, reviewing the radiology and spirometry records. The review was designed to identify the seasonal variation, timing of admissions, referral source, length of stay and identify individuals with multiple hospital admissions. The results of this audit identified marked seasonal variation in admissions with December and January in particular showing high levels (Figure 1).
Figure 1.
Three-year audit of COPD admissions to the University Hospital Southampton during the period before the initiation of the project.
A review identified 34 patients, each of whom had three or more admissions in the 12-month period leading directly into the project. This group was responsible for 176 admissions in this period (Figure 2). This group was cohorted, and an admission avoidance strategy was constructed for this group. This cohort had severe and very severe disease, and the vast majority (33) were current smokers. Patients had a spectrum of COPD phenotypes (Table 1). They were contacted individually and a 1.5-h consultant-led appointment was made in their own home to evaluate the root cause for the multiple admissions, optimise treatment and put interventions in place to reduce future admissions. The interventions included pharmacological optimisation, increased level of care provision, home non-invasive ventilation and priority access to pulmonary rehabilitation.
Figure 2.
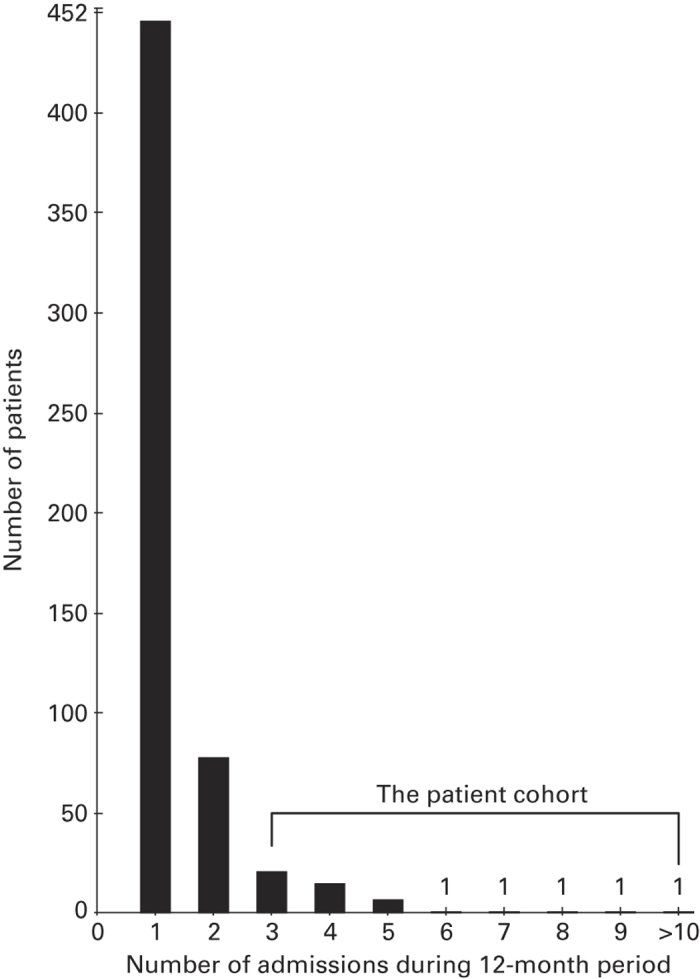
Number of admissions per patient to the University Hospital Southampton in the year prior to project initiation. Thirty-four patients accounted for 176 admissions.
Table 1. COPD phenotypes in the cohort.
| Phenotype | Number of patients |
|---|---|
| Cachectic emphysema (BMI<20) | 11 |
| COPD (emphysema/bronchitis) mixed phenotype BMI>20 | 10 |
| Type II respiratory failure and chronic bronchitis | 7 |
| COPD and bronchiectasis | 3 |
| Very severe COPD with chronic respiratory failure requiring home NIV | 2 |
| COPD overlap syndrome with obstructive sleep apnoea | 1 |
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease.
Each patient was given open access to our respiratory centre manned 9am–5pm with access to clinical review by respiratory consultants and nurses; and out of hours had access to the 24-h COPD nurse community team (which comprises four full-time equivalent specialist respiratory nurses). The respiratory centre and the community team were not enhanced for the project and existing resources were utilised.
Statistical analysis
The data were analysed from the three previous years' hospital admission and readmissions using SPSS (Version 20, IBM). The Wilcoxon-sign test was used to analyse the paired data from the cohort and the previous years readmission data.
Results
Over the 1-year period of the project, we worked with nurses and GPs from 34 of the 36 practices within the city (two practices declined our invitation). The level of intervention (work packages 1–4) provided within surgeries was decided by each individual practice.
The 34 practices that accepted our invitation received work package 1 (education), 30 received package 2 (spirometry training), 7 received package 3 (patient reviews) and 4 received package 4 (screening).
Prevalence
Prior to the project the registered Quality Outcomes Framework prevalence of COPD within the city was 1.5%. Within the year of the project the prevalence increased from 1.5 to 2.27% (Figure 3).
Figure 3.
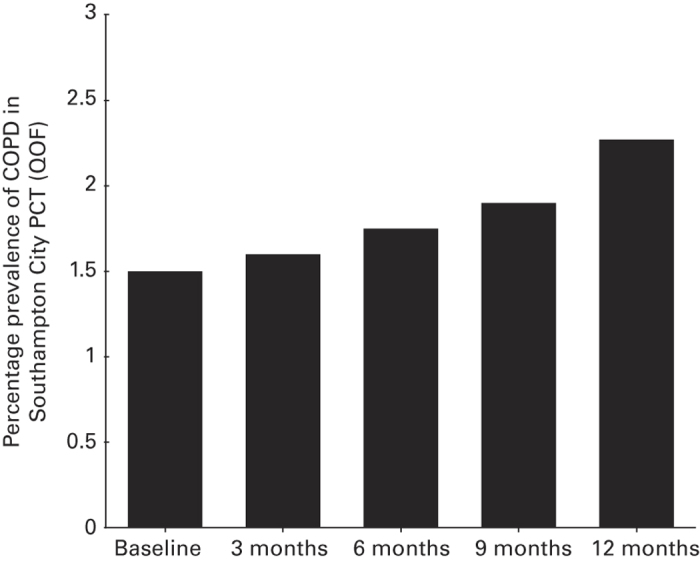
Quarterly COPD prevalence in Southampton City December 2010–2011 according to local Quality Outcomes Framework statistics.
Admissions
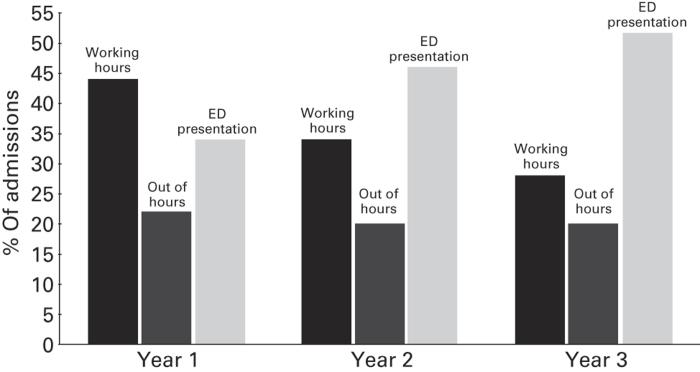
The study also revealed a year on year increase in patient self-presentation direct to the hospital (through ED) without consultation and referral from their GPs (See Figure 4). It also revealed that an increasing percentage of admissions occurred out of hours.
Figure 4.
COPD admission to the University Hospital Southampton according to route of referral in the 3-year period prior to the initiation of the project.
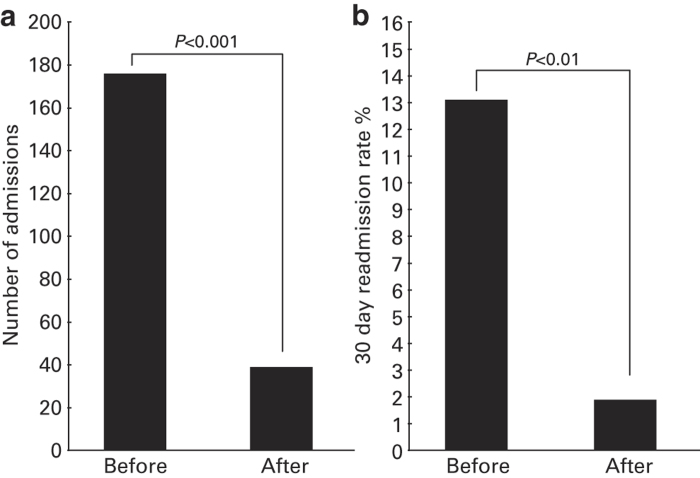
The 34 patients required 185 active interventions (Table 2) during this period but only 39 hospital admissions, compared with 176 the year before (Figure 5a). There was no obvious pattern to those admitted, with the 39 hospital admissions occurring among all phenotypes with similar frequency (data not shown). The overall hospital 30-day readmission rate dropped from 13.4 to 1.9% (P<0.01; Figure 5b), confirming the contribution the cohort made to readmissions.
Table 2. Details of active interventions in the 34-patient cohort.
| Intervention | Number | Percentage |
|---|---|---|
| Phone advice only | 16 | 8.65 |
| Phone advice and direction to take rescue pack of antibiotics and steroids ± nebuliser | 32 | 17.30 |
| Nurse-led home visit | 5 | 2.70 |
| Nurse-led home visit and direction to take rescue pack of antibiotics and steroids ± nebuliser | 71 | 38.38 |
| Doctor-led home visit | 3 | 1.62 |
| Doctor-led home visit and direction to take rescue pack of antibiotics and steroids ± nebuliser | 18 | 9.73 |
| Respiratory centre assessment | 40 | 21.62 |
| Total | 185 | 100.00 |
Figure 5.
(a) Admission rate in the cohort of 34 patients in the year immediately preceding the project and the following year. (b) Total 30-day COPD patient readmission rate over the same period.
Discussion
Main findings
Like most long-term conditions, COPD is in the spotlight as never before. The complexity of its management is enhanced by the presence of significant comorbidities and complex physiology. We present a new way of working in a vertically integrated fashion across both primary and secondary care, led by respiratory consultants who subspecialise in COPD and a COPD specialist nurse team. Using medical intelligence to first identify the key factors driving hospital admissions, as well as identifying key deficiencies across the whole care pathway, we have presented a model that can reduce admissions from acute exacerbations and improve the diagnostic processes in the community. Our COPD early discharge team supported this service redesign; this type of service is present in many hospitals in the United Kingdom to reduce length of stay and support patients at home.
Strengths and limitations of this study
These results were achieved in a city location, with a dense population of patients with COPD and a comprehensive early discharge service already in place. The results of this study may not be readily translatable into other settings (for example, rural) or other systems where such comprehensive services are not funded. These features are important to consider if commissioners are planning on replicating these findings in other areas. One weakness of this study is the absence of a control group. Control groups are difficult to source in studies such as this and require another region with similar demographics, geography, services and resources.
Interpretations of findings in relation to previously published work
The most important intervention that truly changes the disease trajectory and possibly admissions rates, is smoking cessation.13,14 Using appropriate support services (for example, quitters) and smoking cessation adjuncts it is possible to persuade many patients to quit. In our cohort of frequent attendees all but one of these patients were current smokers. If this is a true reflection of those nationwide, then intense support for these patients in abstinence is needed.
Changing pathways is not enough. During the project we encouraged our patients to adhere to prescribed medication and worked with the local practices to adhere to national guidelines. This also included the referral to pulmonary rehabilitation if appropriate. This is important because recent literature reports that appropriate prescribing may reduce the risk of death and hospital admissions.15,16
There are few similar published papers on community service transformation to compare both methods and outcomes. Some recent publications have focused on the development of end-of-life care in this patient group with some success,17 and a multidisciplinary approach to the management of patients with COPD in the community has been shown to be successful in improving a variety of outcomes, including hospitalisation and readmissions in a recent Cochrane review.18
Implications for future research, policy and practice
The data identified that in our hospital over the last 3 years many patients had become disengaged from their primary care practitioner, resulting in a reduction of admissions directly referred from their GP, and an increasing number of patients self-presenting to the Emergency Department for admission without any primary care consultation or contact.
The major piece of learning from the work we performed with our GP colleagues is that to deliver end-to-end care we must assist practice nurses in primary care, where, in our referring practices, the majority of the diagnosis and management of respiratory diseases were delivered.
Conclusions
There are two main conclusions that we have drawn from our work. The first is that the utilisation of medical intelligence to investigate the underlying processes of COPD hospital admissions can lead to an effective intervention. The second is that the impact of secondary care specialists working together with primary care to manage chronic disease can make an impact in a relatively short period of time.
Acknowledgments
The authors thank the Health Foundation for their generous funding of this project.
The authors declare no conflict of interest.
References
- Invisible Lives—Chronic Obstructive Pulmonary Disease (COPD)—finding the missing millions. British Lung Foundation. November 2007. Available at: http://www.blf.org.uk/Page/Special-Reports .
- Report of The National Chronic Obstructive Pulmonary Disease Audit 2008: Resources and Organisation of care in Acute NHS units across the UK, September 2008 Royal College of Physicians, British Lung Foundation and British Thoracic Society. Available at: https://www.rcplondon.ac.uk/sites/default/files/report-of-the-national-copd-audit-2008-resources-and-organisation-of-care-in-acute-nhs-units-across-the-uk.pdf .
- British Thoracic Society Burden of Lung Disease BTS, London, UK; 2006 . Available at: https://www.brit-thoracic.org.uk/document-library/delivery-of-respiratory-care/burden-of-lung-disease/burden-of-lung-disease-2006/ . [Google Scholar]
- UK National Statistics.
- Alrajab S, Smith TR, Owens M, Areno JP, Caldito G. A home telemonitoring program reduced exacerbation and healthcare utilization rates in COPD patients with frequent exacerbations. Telemed J E Health. 2012;18:772–776. doi: 10.1089/tmj.2012.0005. [DOI] [PubMed] [Google Scholar]
- Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060. doi: 10.1136/bmj.e1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice KL, Dewan N, Bloomfield HE, Grill J, Schult TM, Nelson DB. Disease Management Program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182:890–896. doi: 10.1164/rccm.200910-1579OC. [DOI] [PubMed] [Google Scholar]
- Bischoff EW, Hamd DH, Sedeno M, Benedetti A, Schermer TR, Bernard S. Effects of written action plan adherence on COPD exacerbation recovery. Thorax. 2011;66:26–31. doi: 10.1136/thx.2009.127621. [DOI] [PubMed] [Google Scholar]
- Fan V, Gaziano J, Lew R, Bourbeau J, Adams SG, Leatherman S. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med. 2012;156:673–683. doi: 10.7326/0003-4819-156-10-201205150-00003. [DOI] [PubMed] [Google Scholar]
- Shahab L, Jarvis MJ, Britton J, West R. Prevalence, diagnosis and relation to tobacco dependence of chronic obstructive pulmonary disease in a nationally representative population sample. Thorax. 2006;61:1043–1047. doi: 10.1136/thx.2006.064410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- CG101 Chronic Obstructive Pulmonary Disease (updated). National Institute for Health and Clinical Excellence. June 2010. Available at: http://www.nice.org.uk/guidance/CG101 .
- Godtfredsen NS, Vestbo J, Osler M, Prescott E. Risk of hospital admission for COPD following smoking cessation and reduction: a Danish population study. Thorax. 2002;57:967–972. doi: 10.1136/thorax.57.11.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher CM, Peto R, Tinker C, Speizer F. The Natural History of Chronic Bronchitis and Emphysema. Oxford University Press: Oxford, UK; 1976. [Google Scholar]
- Vestbo J, Anderson JA, Calverley PM, Celli B, Ferguson GT, Jenkins C. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax. 2009;64:939–943. doi: 10.1136/thx.2009.113662. [DOI] [PubMed] [Google Scholar]
- Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Anto JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61:772–778. doi: 10.1136/thx.2006.060145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boland J, Owen J, Ainscough R, Mahdi H. Developing a service for patients with very severe chronic obstructive pulmonary disease (COPD) within resources. BMJ Support Palliat Care. 2014;4:196–201. doi: 10.1136/bmjspcare-2012-000393. [DOI] [PubMed] [Google Scholar]
- Kruis AL, Smidt N, Assendelft WJ, Gussekloo J, Boland MR, Rutten-van Mölken M. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;10:CD009437. doi: 10.1002/14651858.CD009437.pub2. [DOI] [PubMed] [Google Scholar]