Abstract
Context
The high number of repetitions and high forces associated with overhead throwing lead to anatomical adaptations, such as humeral retrotorsion and posterior-capsule thickness, in elite and professional baseball athletes. However, little is known about the origin and progression of these changes that may account for the increasing trend of chronic shoulder injuries in youth baseball and precipitate subsequent pathologic conditions throughout a young athlete's lifetime.
Objective
To investigate the relationship of age and upper extremity dominance on humeral retrotorsion, posterior-capsule thickness, and glenohumeral range of motion.
Design
Cross-sectional study.
Setting
Research laboratory, local baseball fields, and training facilities.
Patients or Other Participants
Thirty-six boys (mean age = 10.94 ± 1.34 years, height = 151.31 ± 12.17 cm, mass = 42.51 ± 10.32 kg) ranging in age from 8 to 12 years and involved in organized youth baseball.
Main Outcome Measure(s)
Diagnostic ultrasound was used to determine humeral retrotorsion and posterior-capsule thickness. Glenohumeral internal rotation and external rotation were measured using a handheld inclinometer. We used 2 × 2 mixed-model analyses of variance to compare the influence of limb dominance and age on the dependent variables of humeral retrotorsion, posterior-capsule thickness, internal rotation, and external rotation.
Results
The dominant shoulders of youth throwers exhibited less glenohumeral internal rotation but greater humeral retrotorsion, posterior-capsule thickness, and glenohumeral external rotation than the nondominant shoulders. Dominant internal rotation was greater in the 8- to 10-year-old group than in the 11- to 12-year-old group, and results trended toward a difference (F1,33 = 4.12, P = .05). Correlations existed between humeral retrotorsion and range of motion (P < .05).
Conclusions
The structural adaptations in the dominant shoulders of younger baseball players were similar to adaptations observed in older baseball athletes, indicating that more examination is needed in younger athletes. We are the first to demonstrate greater posterior-capsule thickness in the dominant shoulders of youth baseball athletes.
Key Words: humeral retrotorsion, posterior-capsule thickness, glenohumeral range of motion, baseball, diagnostic ultrasound
Key Points
Youth baseball athletes exhibited adaptations to overhead throwing that were similar to those of older athletes.
The dominant shoulder of the youth cohort had greater posterior-capsule thickness than the nondominant shoulder.
Glenohumeral internal rotation in the dominant limb was greater in boys aged 8 to 10 years than in those aged 11 to 12 years.
Scrutiny of anatomical and physiologic changes at an earlier age should continue.
An increasing number of children in the United States are participating in overhead physical activities, and athletes are beginning to specialize in sports earlier than in previous generations.1 This rise in the number of children participating and increased specialization correspond with an observed increase in overuse pathologic conditions affecting the upper extremity.2 Pediatric athletes aged 6 to 12 years are at an increased risk of developing overuse injuries due to the high torques required during the overhead throwing motion, which create repetitive stress on immature musculoskeletal structures.1,3 One site at which young athletes experience adaptations is the humerus. At birth, the humeral head demonstrates large retrotorsion values, but throughout physical maturation, the osseous tissue of the humeral head rotates into a position of relative antetorsion.4 Analysis of the anthropologic data on the humeri of children has revealed that most antetorsion is complete by 8 years of age, but the process continues slowly until 16 years of age. However, the forces acting on the shoulder during overhead throwing are strong enough to damage the epiphysis,5,6 so they may cause epiphyseal changes that limit the natural physiologic rotation during maturation.7
The restriction of normal antetorsion has been documented in older baseball athletes and may be a positive adaptation that allows for greater glenohumeral external rotation while decreasing tension on the anterior-inferior capsuloligamentus structures of the joint.4,5,7–9 Humeral retrotorsion (HR) may also have deleterious effects, as it is correlated negatively with glenohumeral internal rotation (IR). This negative relationship may lead to a shorter follow-through phase, which means the rotator cuff is unable to properly absorb the forces required for overhead throwing.10,11 If the posterior musculature of youth athletes cannot adequately mitigate these forces, other structures must compensate. One of these structures is the posterior joint capsule, which can assist with joint stability, particularly during end-range IR. Burkhart et al12 proposed that posterior-capsule hypertrophy is the seminal soft tissue adaptation in overhead throwers, and Thomas et al11 recently observed that posterior-capsule thickness (PCT) in adult baseball players was greater in the dominant than in the nondominant limb. However, the evidence for these biomechanical and anatomical adaptations is limited because the variables have not been substantiated in a preadolescent cohort.
Whereas posterior-capsule thickening and subsequent tightening may help protect the shoulder by reducing eccentric loads during acceleration, it may lead to subsequent problems, such as subacromial (external) impingement, in youth athletes by increasing the contact pressure under the subacromial structures during the pitching motion.13 A tight and thick posterior shoulder has also been associated with reports of posterior (internal) impingement.14 Posterior-capsule thickness has not been examined in an adolescent population, so clinicians and researchers cannot confirm whether it actually exists in that population or when the potential adaptation occurs. Therefore, the purpose of our study was to investigate the relationship of age and upper extremity dominance on HR, PCT, and glenohumeral range of motion (ROM). A secondary purpose was to examine the relationships between the measures of anatomical adaptations (HR, PCT) and passive shoulder ROM in adolescent athletes. We hypothesized that the posterior capsule of youth baseball players would be thicker in the dominant than in the nondominant shoulder. We also hypothesized that PCT would be negatively correlated with glenohumeral IR and that PCT, HR, and glenohumeral IR would be greater in older than in younger athletes.
METHODS
Research Design
We used a 2-group, posttest-only experimental design to assess 2 independent and 4 dependent variables. The independent variables were limb (dominant, nondominant) and age group (8–10 years, 11–12 years). The dependent variables included HR, PCT, glenohumeral IR, and glenohumeral external rotation (ER). Limb dominance was defined as the limb with which participants threw baseballs.
Participants
Thirty-six healthy male participants (mean age = 10.94 ± 1.34 years, height = 151.31 ± 12.17 cm, mass = 42.51 ± 10.32 kg) ranging in age from 8 to 12 years volunteered to participate. Athletes were recruited from the local population of youth baseball athletes and had been participating in competitive baseball for an average of 6.00 ± 1.77 years. Of these athletes, 16 were pitchers and 20 were position players. Most of these athletes (n = 29 [81%]) reported that they played organized baseball for more than 7 months in a calendar year or played on multiple teams during the same year. Age was stratified into 2 groups (8–10 and 11–12 years old) to mimic the division between the traditional Little League baseball teams on which these youth athletes would be competing. Participants were excluded if they reported on a health history questionnaire that they had current or recent (in the 6 months before the study) bony, muscular, or joint injury to the elbow or shoulder; history of fracture to the humerus, ulna, radius, clavicle, or scapula; or previous surgery to the elbow or shoulder. One participant was removed from statistical analysis at the discretion of the primary investigator due to noncompliance with the testing protocol.
All participants and their parents or legal guardians provided written informed assent and consent, respectively, and the study was approved by the Institutional Review Board of the University of Delaware. In addition to having the participants read the study outline, the primary investigator read the testing procedures to them to ensure understanding. The parent or legal guardian of each participant completed a health history questionnaire to ensure eligibility and was required to be present throughout testing.
Instrumentation
A commercially available compact ultrasound system (model Titan; Sonosite Inc, Bothell, WA) with a 13-MHz linear transducer was used to collect and measure HR and PCT. Humeral retrotorsion, IR, and ER were measured using a digital inclinometer application for the iPhone 4s (IntegraSoft; Apple Inc, Cupertino, CA). A priori intraclass correlation coefficients (ICCs) were calculated and used to assess the intratester reliability of the primary investigator for all measurements.
Procedures
All testing was completed in the university laboratory, at local baseball fields, or at training facilities. Testing sessions lasted approximately 30 minutes per participant. Each variable was measured twice to ensure a reliable measurement and the values averaged for data analysis.
Assessment of HR
Humeral retrotorsion was measured as described by Thomas et al15 and validated against computerized tomography scans as described by Myers et al,16 with participants lying supine on a treatment table. The shoulder was abducted to 90° and kept in 0° of ER. The elbow was flexed to 90° with the palm facing toward the participant and the forearm positioned vertically. Standard acoustic coupling gel was applied, and the ultrasound transducer was placed on the anterior aspect of the shoulder (Figure 1A). The transducer was maintained in a vertical position while the upper extremity was moved passively into IR or ER until the bicipital groove was oriented vertically on the ultrasound monitor. We verified the transducer to be vertical by placing the digital inclinometer on the shaft of the ultrasound head. If the inclinometer read 90°, the ultrasound head was verified as vertical. When the bicipital groove was pointed vertically on the ultrasound monitor, we placed the digital inclinometer immediately proximal to the ulnar styloid process and along the shaft of the ulna. We recorded the degree of rotation, with negative numbers closer to 0 indicating a greater amount of HR.
Figure 1.
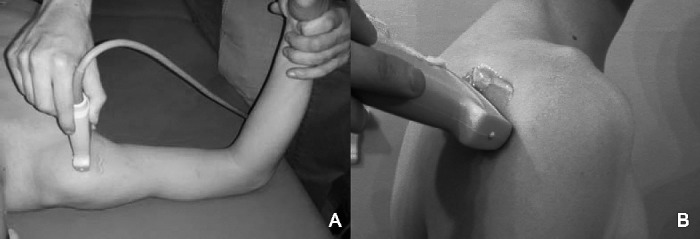
Ultrasound placement for measurement of A, retrotorsion, and B, posterior-capsule measures.
Assessment of PCT
To measure PCT, we followed previously established procedures described by Thomas et al15 that were validated by cadaver study. Participants were seated upright with their arms resting at their sides and forearms resting on their thighs to control for humeral rotation. With the aid of standard acoustic coupling gel, the primary investigator placed the ultrasound transducer on the posterior aspect of the shoulder (Figure 1B). The ultrasound head was adjusted on the posterior aspect of the shoulder until the investigator could visualize the humeral head, glenoid labrum, and rotator cuff musculature. The posterior capsule was identified as the tissue immediately lateral to the edge of the labrum between the humeral head and rotator cuff musculature (Figure 2). When the capsule was identified via the ultrasound screen, the digital image was saved. The thickness of the posterior capsule then was measured using the standard caliper software on the Sonosite Titan (Sonosite Inc). The investigator manually placed the calipers on the edges of the posterior capsule and directly next to the edge of the glenoid labrum, as described by Thomas et al.15 The image was stored on a portable hard drive, and the thickness of the posterior capsule was recorded.
Figure 2.
Ultrasonography of posterior capsule. The bracketed line indicates the posterior capsule.
Assessment of ROM
Passive glenohumeral IR and ER measurements were performed with the participants lying supine on a treatment table. Their shoulders were abducted to 90° and kept in 0° of ER. Their elbows were flexed to 90° with their palms facing toward them and their forearms positioned vertically. The investigator placed 1 of his hands on the coracoid process of the scapula for stabilization and the other hand on the distal wrist to rotate the extremity into IR or ER as described by Awan et al.17 When scapular motion was detected, the investigator stopped the rotation and placed an inclinometer on the shaft of the ulna with its distal edge at the base of the styloid process of the ulna. The measurement on the inclinometer was recorded.
Data Analysis
We used a 2-way, mixed-model analysis of variance (ANOVA) with the α level set a priori at .05 to determine differences within participants and between age groups for HR, PCT, glenohumeral IR and ER, and posterior-shoulder tightness. The main effects of limb dominance for these ANOVAs were used to determine if all youth baseball players displayed differences in the 4 dependent variables between sides. The interaction effects of the ANOVAs were used to determine whether these adaptations changed due to age. Given that 4 ANOVA models were run, we applied a Bonferroni correction to the α level. Therefore, ANOVA models that were different needed to have an α level less than .0125. Pearson product correlation coefficients were calculated among all dependent variables to determine potential relationships. We calculated ICC values (3,1) and standard errors of the means to ensure the reliability of the primary investigator. Data were analyzed using SPSS statistical software (version 19.0; IBM Corporation, Armonk, NY).
RESULTS
All ICC values (3,1) measured greater than 0.92. Standard error of the mean values for glenohumeral IR and ER ranged from 1.4° to 2.4°. The SEM values for the dominant limb were 0.04 mm for PCT and 2.3° for HR and for the nondominant limb were 0.03 mm for PCT and 1.8° for HR.
Comparisons between dominant and nondominant limbs are presented in Table 1 and Figure 3. We observed main effects for limb dominance in HR (F1,33 = 25.52, P < .001), IR (F1,33 = 54.83, P < .001), ER (F1,33 = 116.64, P < .001), and PCT (F1,33 = 9.87, P = .004). Specifically, HR was greater in the dominant (−11.18° ± 13.39°) than in the nondominant (−24.04° ± 10.58°) limb. Glenohumeral ER and PCT were also greater in the dominant (ER = 152.47° ± 14.08°; PCT = 1.29 ± 0.24 mm) than in the nondominant (ER = 131.50° ± 12.14°; PCT = 1.18 ± 0.19 mm) limb. Conversely, IR was less in the dominant (61.93° ± 12.01°) than in the nondominant (75.10° ± 8.50°) limb.
Table 1.
Range of Motion and Posterior-Capsule Thickness in the Dominant and Nondominant Upper Extremities
| Variable |
Dominant Upper Extremity |
Nondominant Upper Extremity |
P Value |
F1,33 Value |
||||
| Mean ± SD |
95% Confidence Interval |
Mean ± SD |
95% Confidence Interval |
|||||
| Lower |
Upper |
Lower |
Upper |
|||||
| Humeral retrotorsion, ° | −11.18 ± 13.39 | −15.14 | −5.70 | −24.04 ± 10.58 | −27.22 | −19.87 | <.001a | 25.52 |
| Glenohumeral internal rotation, ° | 61.93 ± 12.01 | 58.14 | 66.22 | 75.10 ± 8.50 | 71.68 | 77.63 | <.001a | 54.83 |
| Glenohumeral external rotation, ° | 152.47 ± 14.08 | 147.26 | 156.82 | 131.50 ± 12.14 | 127.51 | 135.61 | <.001a | 116.64 |
| Posterior-capsule thickness, mm | 1.29 ± 0.24 | 1.21 | 1.53 | 1.18 ± 0.19 | 1.11 | 1.35 | .004a | 9.87 |
Indicates difference.
Figure 3.
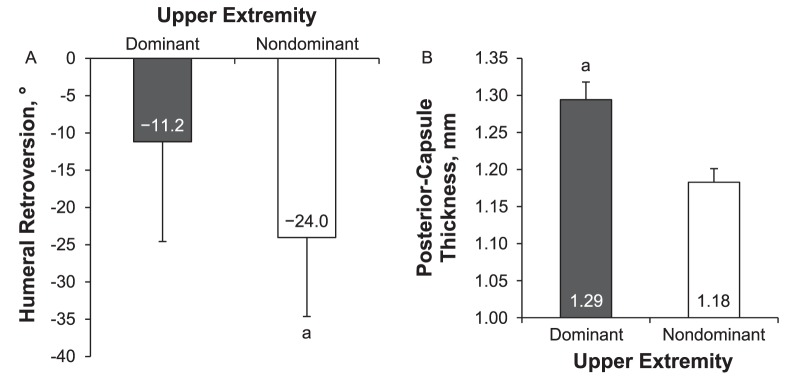
A, Humeral retroversion, and B, posterior-capsule thickness of the dominant and nondominant upper extremities. a Indicates difference.
The 2 × 2 ANOVA results are shown in Table 2. We did not observe interaction effects between age groups (8–10 versus 11–12 years old) and limb dominance for HR (F1,33 = 0.53, P = .47), ER (F1,33 = 2.50, P = .12), or PCT (F1,33 = 1.65, P = .21). However, results for IR trended toward a difference (F1,33 = 4.12, P = .05). Specifically, older athletes trended toward exhibiting less IR than the younger group on the dominant side (60.2° ± 2.79° and 64.2° ± 10.88°, respectively). No apparent differences were observed between groups for IR of the nondominant side.
Table 2.
Age-Group Comparison for the Dominant Upper Extremity
| Variable |
8- to 10-Year-Old Group |
11- to 12-Year-Old Group |
P Value |
F1,33 Value |
||||
| Mean ± SD |
95% Confidence Interval |
Mean ± SD |
95% Confidence Interval |
|||||
| Lower |
Upper |
Lower |
Upper |
|||||
| Humeral retrotorsion, ° | −11.43 ± 13.84 | −18.18 | −3.52 | −10.85 ± 13.23 | −17.90 | −4.95 | .47 | 0.53 |
| Glenohumeral internal rotation, ° | 64.23 ± 10.88 | 58.21 | 70.26 | 60.20 ± 12.79 | 54.22 | 66.18 | .05a | 4.12 |
| Glenohumeral external rotation, ° | 151.20 ± 14.26 | 146.33 | 162.00 | 154.17 ± 14.14 | 144.52 | 157.88 | .12 | 2.50 |
| Posterior-capsule thickness, mm | 1.29 ± 0.24 | 1.15 | 1.43 | 1.29 ± 0.25 | 1.19 | 1.41 | .21 | 1.65 |
Indicates trend toward difference.
Glenohumeral IR exhibited a negative correlation with ER (r = −0.395, P = .02) and HR (r = −0.431, P = .01) in the dominant limb. External rotation was correlated with HR in the dominant limb (r = 0.448, P = .007). Glenohumeral ER and PCT in the dominant limb trended toward a moderate, positive relationship, which was not different (r = 0.322, P = .059). Glenohumeral IR exhibited a negative correlation with HR that trended toward a difference in the nondominant limb (r = −0.334, P = .05).
DISCUSSION
Our primary finding confirmed the hypothesis that the dominant limb of adolescent overhead throwing athletes exhibited greater PCT than the nondominant limb. We also observed HR, ER, and IR differences in baseball athletes aged 8 to 12 years. However, these shoulder adaptations did not seem to change much as baseball athletes moved to teams in a different age group. Secondarily, we observed moderate relationships among IR, ER, and HR in the dominant limb. Secondarily, we observed moderate relationships among IR, ER, and HR in the dominant limb, but it is still unclear whether they are clinically important in a youth population. These data suggested that the glenohumeral-joint adaptations observed in high school, collegiate, and professional baseball athletes develop at a young age.
Our data agreed with those of the previous literature in which authors7,9,15,18 described greater HR in the dominant than in the nondominant limb. The difference of approximately 13° between limbs that we noted was greater than the previously observed 3° variation in a group of elite elementary and middle school–aged baseball athletes.7 The divergence between our results and those of Yamamoto et al7 may be attributable to the populations tested. Our participants had more years of baseball experience and had started pitching earlier than their participants.7 Opposing forces of a distal ER torque and proximal IR torque during the late cocking phase of throwing are theorized to be strong enough to cause microdamage to the epiphysis and slow the normal maturational derotation process, thereby leading to greater HR.4,7 In our sample, participants had approximately 2.7 years of additional throwing experience, which may account for the observed differences in HR when considering the summation of these repetitive stresses.
Whereas our results were different from those of another study of similarly aged overhead throwers, the variance in HR between shoulders was similar to the 10° to 17° variance demonstrated in high school, collegiate, and professional athletes.10,11,19,20 These data suggested that the differences observed in older athletes may occur at a much younger age than previously assumed. In addition to differences in the dominant and nondominant limbs, HR displayed a negative correlation with IR and a positive correlation with ER, an observation that has also been reported in collegiate baseball athletes.11 These correlations are moderate in a youth population; however, in light of these correlations combined with the large differences observed in HR at such a young age, clinicians should begin to examine HR at a younger age and recognize that a lack of glenohumeral IR may result from osseus adaptations in a youth population. Based on these results and the inconclusiveness of previous studies on HR,8,21 future research should be directed at determining the consequences of excessive HR in a youth population.
The relationship between HR and glenohumeral ROM is evident in the differences observed in IR and ER when comparing the dominant and nondominant limbs. We found alterations in glenohumeral ROM between limbs consistent with the pattern of decreased IR and increased ER that has been documented in many studies of overhead athletes.15,19,22–25 Our average differences of 13° less IR and 21° greater ER in the dominant limb were larger than most reported in the literature. When investigating a similar age group, Meister et al25 found an average difference of 3° for IR and 4° for ER in a group of 11-year-old participants. The variations between our results and those of Meister et al25 may be attributable to our pooling of data from 8- to 12-year-old athletes. The pooling of data could have introduced greater variance due to the age and physical maturity range in our group compared with a homogeneous group of 11-year-old children. Nevertheless, the general trend of IR loss and ER gain in youth overhead athletes is still present. The similar trends in these studies continue to support the theory that ROM changes can occur at early ages. The shift in motion to decreased IR and increased ER that is associated with overhead sports may be detrimental,14 as it is believed to result in a decreased amount of rotational motion available after ball release during the follow-through phase. This decreased arc would then place additional stress on the posterior rotator cuff and posterior capsule, potentially increasing the risk of injury. It may also lead to stress-induced hypertrophy of the posterior structures in an attempt to absorb and decelerate the upper extremity.12
Our analysis of IR revealed that baseball players aged 8 to 10 years had an average of 4° more motion in the dominant limb than players aged 11 to 12 years. This finding is in agreement with previous literature in which researchers25 showed a decrease in IR of about 18° as adolescent baseball players increased in chronologic age from 8 to 16 years. Based on our results that IR trended toward decreasing with age while no age differences existed with HR or PCT, we propose that the differences in IR displayed by youth athletes may be attributable to a natural decrease in motion as they age. However, examining a broader age range may show that increased HR in the dominant limb and soft tissue contracture of the posterior capsule may affect IR as well.
The increased availability of diagnostic imaging techniques has allowed the posterior capsule to become a greater focus in research.11,15,26,27 Investigators15 have shown greater PCT in the dominant than in the nondominant limb. To our knowledge, we are the first to investigate adaptations to the posterior capsule in youth athletes. We observed that the dominant limb displayed greater PCT than the nondominant limb in these athletes. This finding is in agreement with previous literature15 on collegiate baseball athletes, who displayed an average difference of about 0.4 mm in PCT between dominant and nondominant limbs. Whereas our results on PCT were different, we recognize that the clinical implication will need further study for substantiation. No research has been conducted to determine the magnitude of a difference that has clinical relevance for PCT, so we cannot state whether the observed difference (0.111 mm) in PCT between the dominant and nondominant limbs in our participants was clinically meaningful. Given that our observed difference was 3 times less than that of college-aged baseball athletes, we can speculate that side-to-side differences in PCT begin in youth athletes and continue to progress at an unknown rate over time until they become much more pronounced in physically mature overhead throwers. This development of PCT may be a positive adaptation to attempt to reduce eccentric loads during deceleration. However, over time, a contracted or shortened posterior capsule may result in a posterior-superior shift in the positioning of the humeral head during simulated pitching positions or a decrease in IR, thereby leading to increased risk for subacromial and posterior impingement.13,21,26,28 Our participants were healthy, but future researchers should determine whether PCT actually leads to injury and whether a certain threshold that is related to pathologic shoulder conditions and pain in youth players exists for PCT.
The posterior capsule is important not only by itself but also because of its relationships to glenohumeral ROM. Our correlation analysis revealed a moderate positive relationship between PCT and ER that trended toward a difference. Similarly, Thomas et al11 observed both a strong positive correlation between PCT and ER and a strong negative correlation between PCT and IR. The lack of correlation between PCT and IR in our study may show that the effects of repetitive throwing at a young age have not yet accumulated to result in a meaningful relationship. Conceivably, other structures, such as the proximal humeral epiphysis, could be partly absorbing the stress,5 which would result in the HR differences that we observed, while limiting the development of PCT and preventing a relationship between PCT and IR. The age and physical maturation of the participants could also limit the observable differences.
Overall, our findings suggested that some shoulder adaptations normally associated with collegiate and adult baseball players also manifest in younger athletes. We are the first to detect PCT differences in youth throwers. The adaptation of PCT is concerning in terms of injury because after an average of 6 years of play, these young athletes are presenting with physical adaptations known to relate to pathologic shoulder conditions in adults. Our results also support the use of ultrasound to screen for risk factors and monitor the degree of adaptations to throwing in youths.
Future research on HR and PCT development in overhead throwers should focus on youth athletes and should follow their progression over time. If investigators can begin to identify the shoulder adaptations associated with youth athletes and precise age ranges for those changes, clinicians may be able to design more effective interventions for youth throwers.
Our study had some limitations. First, not using a standardized physical maturity scale, such as Tanner staging or maturational age, may have affected our age-group comparisons. Those methods would have provided a better prediction of physical maturity than chronologic age and would have allowed us to better compare developmental morphology. Second, the lack of adequate sample sizes to compare all variables with chronologic age limited the power and generalizability of the results to the 2 pooled age ranges. In addition, most athletes subjectively reported participating on multiple teams in multiple leagues, thereby limiting the applicability of the results to youth athletes who have similar playing histories.
CONCLUSIONS
We observed that youth baseball athletes exhibited adaptations to overhead throwing that were similar to those of older athletes. To our knowledge, we are the first to find differences in PCT between upper extremities in a youth cohort, with the dominant limb having greater PCT than the nondominant limb. Our healthy cohort demonstrated greater amounts of HR in the dominant limb and altered glenohumeral ROM, including greater IR, in a population of 8- to 10-year-old athletes compared with a population of 11- to 12-year-old athletes. Given that these adaptations in youth baseball athletes were similar to those observed in both healthy and injured adult baseball players, we advocate the continued scrutiny of anatomical and physiologic changes at an earlier age.
REFERENCES
- 1.Leonard J, Hutchinson MR. Shoulder injuries in skeletally immature throwers: review and current thoughts. Br J Sports Med. 2010;44(5):306–310. doi: 10.1136/bjsm.2009.062588. [DOI] [PubMed] [Google Scholar]
- 2.Brenner JS. American Academy of Pediatrics Council on Sports Medicine and Fitness. Overuse injuries, overtraining, and burnout in child and adolescent athletes. Pediatrics. 2007;119(6):1242–1245. doi: 10.1542/peds.2007-0887. [DOI] [PubMed] [Google Scholar]
- 3.Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 4.Edelson G. The development of humeral head retroversion. J Shoulder Elbow Surg. 2000;9(4):316–318. doi: 10.1067/mse.2000.106085. [DOI] [PubMed] [Google Scholar]
- 5.Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33(11):1716–1722. doi: 10.1177/0363546505275347. [DOI] [PubMed] [Google Scholar]
- 6.Zaremski JL, Krabak BJ. Shoulder injuries in the skeletally immature baseball pitcher and recommendations for the prevention of injury. PM R. 2012;4(7):509–516. doi: 10.1016/j.pmrj.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto N, Itoi E, Minagawa H, et al. Why is the humeral retroversion of throwing athletes greater in dominant shoulders than in nondominant shoulders? J Shoulder Elbow Surg. 2006;15(5):571–575. doi: 10.1016/j.jse.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26(2):247–253. doi: 10.1177/03635465980260021501. [DOI] [PubMed] [Google Scholar]
- 9.Whiteley RJ, Ginn KA, Nicholson LL, Adams RD. Sports participation and humeral torsion. J Orthop Sports Phys Ther. 2009;39(4):256–263. doi: 10.2519/jospt.2009.2821. [DOI] [PubMed] [Google Scholar]
- 10.Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30(3):347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- 11.Thomas SJ, Swanik CB, Kaminski TW, et al. Humeral retroversion and its association with posterior capsule thickness in collegiate baseball players. J Shoulder Elbow Surg. 2012;21(7):910–916. doi: 10.1016/j.jse.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology, part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 13.Muraki T, Yamamoto N, Zhao KD, et al. Effect of posteroinferior capsule tightness on contact pressure and area beneath the coracoacromial arch during pitching motion. Am J Sports Med. 2010;38(3):600–607. doi: 10.1177/0363546509350074. [DOI] [PubMed] [Google Scholar]
- 14.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 15.Thomas SJ, Swanik CB, Higginson JS, et al. A bilateral comparison of posterior capsule thickness and its correlation with glenohumeral range of motion and scapular upward rotation in collegiate baseball players. J Shoulder Elbow Surg. 2011;20(5):708–716. doi: 10.1016/j.jse.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 16.Myers JB, Oyama S, Clarke JP. Ultrasonographic assessment of humeral retrotorsion in baseball players: a validation study. Am J Sports Med. 2012;40(5):1155–1160. doi: 10.1177/0363546512436801. [DOI] [PubMed] [Google Scholar]
- 17.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83(9):1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 18.Roach NT, Lieberman DE, Gill TJ IV, Palmer WE, Gill TJ., III The effect of humeral torsion on rotational range of motion in the shoulder and throwing performance. J Anat. 2012;220(3):293–301. doi: 10.1111/j.1469-7580.2011.01464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 20.Oyama S, Hibberd EE, Myers JB. Changes in humeral torsion and shoulder rotation range of motion in high school baseball players over a 1-year period. Clin Biomech (Bristol, Avon) 2013;28(3):268–272. doi: 10.1016/j.clinbiomech.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 21.Myers JB, Oyama S, Rucinski TJ, Creighton RA. Humeral retrotorsion in collegiate baseball pitchers with throwing-related upper extremity injury history. Sports Health. 2011;3(4):383–389. doi: 10.1177/1941738111410636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hurd WJ, Kaplan KM, Eiattrache NS, Jobe FW, Morrey BF, Kaufman KR. A profile of glenohumeral internal and external rotation motion in the uninjured high school baseball pitcher: part I. Motion. J Athl Train. 2011;46(3):282–288. doi: 10.4085/1062-6050-46.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mair SD, Uhl TL, Robbe RG, Brindle KA. Physeal changes and range-of-motion differences in the dominant shoulders of skeletally immature baseball players. J Shoulder Elbow Surg. 2004;13(5):487–491. doi: 10.1016/j.jse.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 24.McConnell J, McIntosh B. The effect of tape on glenohumeral rotation range of motion in elite junior tennis players. Clin J Sport Med. 2009;19(2):90–94. doi: 10.1097/JSM.0b013e31819b9cd1. [DOI] [PubMed] [Google Scholar]
- 25.Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33(5):693–698. doi: 10.1177/0363546504269936. [DOI] [PubMed] [Google Scholar]
- 26.Clabbers KM, Kelly JD, Bader D, et al. Effect of posterior capsule tightness on glenohumeral translation in the late-cocking phase of pitching. J Sport Rehabil. 2007;16(1):41–49. doi: 10.1123/jsr.16.1.41. [DOI] [PubMed] [Google Scholar]
- 27.Muraki T, Yamamoto N, Zhao KD, et al. Effects of posterior capsule tightness on subacromial contact behavior during shoulder motions. J Shoulder Elbow Surg. 2012;21(9):1160–1167. doi: 10.1016/j.jse.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 28.Huffman GR, Tibone JE, McGarry MH, Phipps BM, Lee YS, Lee TQ. Path of glenohumeral articulation throughout the rotational range of motion in a thrower's shoulder model. Am J Sports Med. 2006;34(10):1662–1669. doi: 10.1177/0363546506287740. [DOI] [PubMed] [Google Scholar]



