Abstract
Objective
To present a case of ultrasonic diagnosis and nonoperative management of a complete proximal rectus femoris avulsion in a National Collegiate Athletic Association Division 1 soccer goalkeeper.
Background
While delivering a goal kick, a previously uninjured 24-year-old collegiate soccer goalkeeper had the sudden onset of right anterior thigh pain. He underwent rehabilitation with rapid resolution of his presenting pain but frequent intermittent recurrence of anterior thigh pain. After he was provided a definitive diagnosis with musculoskeletal ultrasound, he underwent an extended period of rehabilitation and eventually experienced complete recovery without recurrence.
Differential Diagnosis
Rectus femoris avulsion, rectus femoris strain or partial tear, inguinal hernia, or acetabular labral tear.
Treatment
Operative and nonoperative options were discussed. In view of the player's recovery, nonoperative options were pursued with a good result.
Uniqueness
Complete proximal rectus femoris avulsions are rare. Our case contributes to the debate on whether elite-level kicking and running athletes can return to full on-field performance without surgery.
Conclusions
Complete proximal rectus femoris avulsions can be treated effectively using nonoperative measures with good preservation of function even in the elite-level athlete. In addition, musculoskeletal ultrasound is an excellent tool for on-site evaluation and may help guide prognosis and management.
Key Words: athletic injuries, rehabilitation, soccer
Complete proximal rectus femoris avulsions are infrequent. On-field examination can be challenging and may lead to inexact recommendations for rehabilitation and return to play. In addition to history and physical examination, musculoskeletal ultrasound can improve diagnostic accuracy and help direct management.
CASE REPORT
A previously uninjured 24-year-old National Collegiate Athletic Association Division I soccer goalkeeper described feeling as if he had been “hit with a baseball” in the front of his right thigh during a goal kick. He continued to play, and on the next kick, he reported feeling as if he had been “shot in the leg.” He was removed from play, and the on-site physician diagnosed a quadriceps strain without rupture. The athlete had difficulty walking for 1 week and pursued rehabilitation with ice, stretching, manual therapies, and a graduated strengthening program for 2 weeks. He returned to play, and while striking a goal kick 3 weeks later, he described feeling similar but less severe pain. The athlete was removed from play and underwent similar rehabilitation for 2 more weeks. He returned to full play asymptomatic and again experienced pain in the anterior thigh during a goal kick. Given the recurrent symptoms, he underwent 8 weeks of intensive rest and rehabilitation, including treatment of acute symptoms with rest and pain management, followed by a progressive rehabilitation program. He gradually returned to a full-kicking play and resistance-training program. At 5 months after the first injury, his symptoms were occasional soreness, achiness, and mild swelling in the front of his thigh after repetitive goal kicks or intense resistance training. He presented to the athletic training room for evaluation by a physician and to discuss using acupuncture to treat these symptoms.
On examination, his gait was nonantalgic with normal stride length and cadence. He was able to perform toe walk, heel walk, tandem gait, single-legged squat, and duck walk without pain or asymmetry. Lumbar and hip range of motion were full and without pain in all planes. A defect was noted in the proximal anterior quadriceps bulk, which increased with resisted knee extension and hip flexion (Figure 1). Manual muscle testing demonstrated 5/5 strength bilaterally in the L3–S1 myotomes. Resisted hip flexion, knee extension, and knee flexion were symmetric and without pain. Sensation to light touch was intact in the L3–S1 dermatomes; patellar and Achilles tendon reflexes were 2+; toes were down-going; and bilaterally, he had no clonus. Provocative testing demonstrated negative straight-leg raise and consisted of flexion, abduction, and external-rotation tests; flexion, abduction, and internal-rotation tests; Stinchfield test; Scour test; and femoral nerve stretch testing. On palpation, the proximal rectus femoris tendon was absent, and a defect in the muscle with distal redundancy was apparent. We used a dynamometer (System 4 Pro; Biodex Medical Systems Inc, Shirley, NY) to assess range of motion. Isokinetic testing demonstrated a deficit of 10.8% during concentric hip flexion at 60°/s and 40.3% at 180°/s in the right limb. Concentric knee extension demonstrated a 16.5% deficit at 60°/s and 12.0% at 180°/s in the right limb.
Figure 1.
Photograph of the right thigh with a notable defect in the region of the rectus femoris during resisted hip flexion.
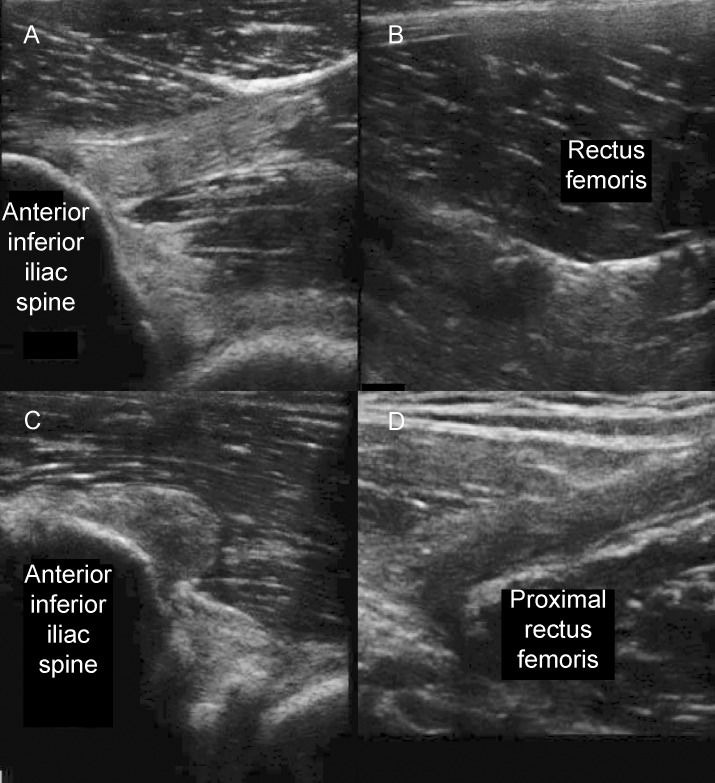
Ultrasonic examination demonstrated a normal-appearing rectus femoris in the left limb from the anterior-inferior iliac spine to insertion on the patella (Figure 2A and B). In the right limb, the direct head was torn at the musculotendinous junction, leaving a “stump” of attached tendon, and the indirect head was avulsed completely from the acetabular brim (Figure 2C). Approximately 10 cm distal to the anterior-inferior iliac spine, extensive scar tissue with invested neurovascular structures could be seen where the rectus femoris was scarred onto the underlying vastus intermedius (Figure 2D). With active knee extension, the distal rectus femoris contracted, pulling on the scar tissue without pain. Active hip flexion resulted in a shortening of the iliopsoas without activation of the rectus femoris.
Figure 2.
Ultrasound images of the left (unaffected) and right (affected) rectus femoris. A, The normal rectus femoris structure at the anterior-inferior iliac spine and B, 10 cm distal in the midthigh. C, The remaining stump of the right rectus femoris and D, a region of scarring 10 cm distal.
In view of his excellent recovery but persistent deficits on isokinetic testing, he was encouraged to continue maximizing core, pelvic, and thigh strength and stability, and he continued full participation, during which he reported no deficits or pain.
DISCUSSION
Muscular injuries of the lower extremity, and quadriceps strains specifically, are the leading injuries reported in elite soccer players.1 Previous injury, advancing age, kicking extremity, and incomplete or inappropriate rehabilitation of previous injuries predict injury.2 The rectus femoris is at particular risk for injury due to its biarthrodial nature and high percentage of type II muscle fibers. The direct head attaches to the anterior-inferior iliac spine, and the indirect head attaches to the acetabular brim. Hip extension and knee flexion elongate the muscle, and rapid concentric contraction during initiation of a kick or explosive sprinting may lead to strain, tear, or avulsion. Rectus avulsion injuries that involve the apophysis are more common in young athletes. However, as seen in our athlete, avulsion through the substance of the tendon occurs in skeletally mature athletes exposed to high-force muscle contractions. Proximal avulsion has been reported at both the origin and the musculotendinous junction.3,4 Our athlete possibly experienced an initial partial tear, which converted to a full avulsion and gradually retracted until it became scarred in place during his prolonged rehabilitation. Gamradt et al5 suggested that nonoperative management of proximal rectus femoris avulsion injuries predictably resulted in a full and complete return to sport in National Football League athletes, and that was our experience with this soccer goalkeeper. Other researchers6,7 have suggested that early operative management is preferable. Unlike early operative repair for proximal hamstrings avulsions, which has been well studied,8 operative management of proximal rectus femoris avulsions has not been shown to be superior to conservative treatment.
Any discussion of management is predicated on accurate diagnosis. Our case highlights the complexity of field-side evaluation without diagnostic imaging. On initial evaluation, our player had intense pain but symmetric quadriceps bulk. With rest and appropriate rehabilitation, he quickly became pain free during training and scrimmage and returned to full participation. The indication for early imaging was minimal; however, we question if ultrasound evaluation on game day or in the athletic training room might have altered his management and possibly his outcome. Ultrasound examination offers both static and dynamic views of the quadriceps, and whereas it is imperfect,9 it offers insight into the severity of a tear and the presence of hemorrhage, bony avulsion, or retraction. Given the low cost and expanding availability of the technology, it is an excellent first step in evaluation.10
More research is needed to guide sports medicine providers in the best management of proximal rectus femoris avulsions. Our case provides further evidence that nonoperative management is an effective approach, even in an elite collegiate soccer player. It also highlights the potential value of early ultrasound evaluation in prompt and accurate diagnosis.
REFERENCES
- 1.Ekstrand J, Hagglund M, Walden M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–558. doi: 10.1136/bjsm.2009.060582. [DOI] [PubMed] [Google Scholar]
- 2.Hagglund M, Walden M, Ekstrand J. Risk factors for lower extremity muscle injury in professional soccer: the UEFA Injury Study. Am J Sports Med. 2013;41(2):327–335. doi: 10.1177/0363546512470634. [DOI] [PubMed] [Google Scholar]
- 3.Hasselman CT, Best TM, Hughes CT, Martinez S, Garrett WE. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23(4):493–499. doi: 10.1177/036354659502300421. [DOI] [PubMed] [Google Scholar]
- 4.Straw R, Colclough K, Geutjens G. Surgical repair of a chronic rupture of the rectus femoris muscle at the proximal musculotendinous junction in a soccer player. Br J Sports Med. 2003;37(2):182–184. doi: 10.1136/bjsm.37.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gamradt SC, Brophy RH, Barnes R, Warren RF, Thomas Byrd JW, Kelly BT. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37(7):1370–1374. doi: 10.1177/0363546509333477. [DOI] [PubMed] [Google Scholar]
- 6.Garcia VV, Duhrkop DC, Seijas R, Ares O, Cuqat R. Surgical treatment of proximal ruptures of the rectus femoris in professional soccer players. Arch Orthop Trauma Surg. 2012;132(3):329–333. doi: 10.1007/s00402-011-1372-8. [DOI] [PubMed] [Google Scholar]
- 7.Irmola T, Heikkila JT, Orava S, Sarimo J. Total proximal tendon avulsion of the rectus femoris muscle. Scand J Med Sci Sports. 2007;17(4):378–382. doi: 10.1111/j.1600-0838.2006.00564.x. [DOI] [PubMed] [Google Scholar]
- 8.Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures: a systematic review. Int J Sports Med. 2011;32(7):490–495. doi: 10.1055/s-0031-1273753. [DOI] [PubMed] [Google Scholar]
- 9.Swamy GN, Nanjayan SK, Yallappa S, Bishnoi A, Pickering SA. Is ultrasound diagnosis reliable in acute extensor tendon injuries of the knee? Acta Orthop Belg. 2012;78(6):764–770. [PubMed] [Google Scholar]
- 10.Bianchi S, Martinoli C, Waser NP, Bianchi-Zamorani MP, Federici E, Fasel J. Central aponeurosis tears of the rectus femoris: sonographic findings. Skeletal Radiol. 2002;31(10):581–586. doi: 10.1007/s00256-002-0559-z. [DOI] [PubMed] [Google Scholar]