Orthopedic surgery patients often experience severe postoperative pain, and effective analgesia is essential. In this study, the authors compared continuous fascia iliaca compartment block with patient-controlled intravenous analgesia using fentanyl postoperatively in patients with hip fractures. Changes in pain scores as well as delirium and postoperative nausea and vomiting were evaluated.
Keywords: Hip fracture, Iliaca compartment block, Patient-controlled intravenous analgesia
Abstract
BACKGROUND:
Effective analgesia is essential for the postoperative care of orthopedic patients.
OBJECTIVES:
To evaluate the efficacy of continuous fascia iliaca compartment block (FIB) as postoperative analgesia after hip fracture surgery, and to compare FIB with patient-controlled intravenous analgesia (PCIA) using fentanyl for 48 h postoperatively.
METHODS:
Patients with hip fractures who were scheduled for open reduction and internal fixation surgery using the antirotation proximal femoral nail technique were randomly assigned to the FIB or PCIA groups. Postoperative pain was assessed using a numeral rating scale at 2 h, 4 h, 6 h, 12 h, 24 h and 48 h after analgesia was started. Delirium, postoperative nausea and vomiting (PONV), and pruritus were also monitored.
RESULTS:
Patients in the FIB group reported less pain than those in the PCIA group (P=0.039, d=−0.3). The change in pain scores over time was similar between the two groups. There were six patients with PONV and five patients with pruritus in the PCIA group, while no PONV or pruritus was noticed in the FIB group (P=0.013). Ten (19.6%) patients in the FIB group and three (5.7%) patients in the PCIA group developed postoperative delirium (P=0.032, d=0.77).
CONCLUSION:
Continuous FIB is a safe and effective technique for postoperative analgesia after hip fracture surgery, making it an option for pain management in elderly patients with hip fractures.
Abstract
HISTORIQUE :
Il est essentiel d’assurer une analgésie efficace en orthopédie postopératoire.
OBJECTIFS :
Évaluer l’efficacité du bloc du compartiment ilio-fascial (BCIF) continu en analgésie postopératoire après une chirurgie pour fracture de la hanche, et comparer le BCIF à l’analgésie intraveineuse contrôlée par le patient (AICP) au fentanyl pendant les 48 heures suivant l’opération.
MÉTHODOLOGIE :
Les patients ayant une facture de la hanche qui devaient subir une chirurgie ouverte de réduction et de fixation interne par la technique du clou antirotation pour fracture du fémur proximal ont été répartis au hasard entre le groupe de BCIF et d’AICP. La douleur postopératoire a été évaluée au moyen d’une échelle d’évaluation numérique deux, quatre, six, 12, 24 et 48 heures après le début de l’analgésie. Le délire, les nausées postopératoires et les vomissements (NPOV) ainsi que le prurit ont également été surveillés.
RÉSULTATS :
Les patients du groupe du BCIF ont déclaré souffrir moins que ceux du groupe d’AICP (P=0,039, d=−0,3). Le changement dans les scores de douleur au fil du temps était similaire dans les deux groupes. Six patients souffraient de NPOV et cinq, de prurit dans le groupe d’AICP, mais aucun cas de NPOV ni de prurit n’a été observé dans le groupe de BCIF (P=0,013). Dix patients (19,6 %) du groupe de BCIF et trois (5,7 %) du groupe d’AICP ont souffert de délire postopératoire (P=0,032, d=0,77).
CONCLUSION :
Le BCIF continu est une technique d’analgésie postopératoire sécuritaire et efficace après une chirurgie pour fracture de la hanche, qui peut être utilisée pour gérer la douleur chez les patients âgés ayant une telle fracture.
Severe postoperative pain is often observed among orthopedic patients (1). Effective analgesia is essential for the postoperative care of orthopedic patients. Intravenous opioid therapy is frequently used to manage postoperative pain following orthopedic surgery in the majority of hospitals (1,2). However, opioid-related side effects, such as nausea, vomiting and pruritus, are common. Regional analgesic techniques have been shown to provide similar analgesia to systemic opioids (2). When performed by anesthesiologists, fascia iliaca compartment block (FIB) is reported to effectively block cutaneous lateral femoral and femoral nerves in adults (3,4). The innervations of the cutaneous lateral femoral nerve and femoral nerves cover the area involved in the hip fracture surgery. Continuous FIB with 0.2% bupivacaine over 48 h reduces opioid requirement in the postoperative period after total knee arthroplasty (5). Therefore, continuous FIB may provide efficient analgesic effects after orthopedic surgery for hip fractures as well. To evaluate the efficacy of this technique in hip fracture surgery, the present prospective, randomized study was designed to compare continuous FIB with patient-controlled intravenous analgesia (PCIA) using fentanyl for 48 h after the operation.
METHODS
The study protocol was approved by the ethics committee of the authors’ hospital. All patients provided written informed consent. The trial was not registered with a trial registry.
Inclusion criteria were patients who had hip fractures and were scheduled for open reduction and internal fixation surgery using the antirotation proximal femoral nail technique. Patients who underwent the full protocol were included in the analysis. Sample size was calculated as 44 per group with power = 0.9, f=0.25 and α=0.05. Patients who met the inclusion criteria were randomly assigned to either the PCIA or FIB group according to a computer-generated random number table. Blinding could not be conducted due to differences in the analgesia procedures and infusion pumps used. Presurgery cognitive status was estimated using the mini-mental state examination before and after surgery. The Confusion Assessment Method was used to diagnose delirium pre- and postsurgery.
Exclusion criteria were: neuropathy involving the lower extremities; bladder dysfunction; coagulopathies; and known allergy to amide local anesthetic drugs or opioids. Patients who did not cooperate and those who had psychological disorders or linguistic difficulties that may interfere with pain assessment were excluded.
Patients admitted from December 2012 to December 2013 were included in the present study. All patients who met the inclusion criteria were given general anesthesia and underwent the same type of surgery procedure. The regional surgery guideline was followed. There was no specific time requirement from admission to operation. Both groups received flurbiprofen 40 mg at the end of surgery. No other analgesia was provided in the operating room or recovery room.
Induction of anesthesia was achieved in a standardized manner using fentanyl (210 μg to 240 μg), propofol (53.2 mg to 58.9 mg) and atracurium besylate (7.8 μg to 11.8 μg). Anesthesia was maintained with remifentanil (638.4 μg to 1060.2 μg) and propofol (238.5 mg to 356.2 mg). Propofol and remifentanil were discontinued 15 min and 5 min before the end of surgery, respectively.
The procedure and technique of the continuous FIB has been described by Cuignet et al (6). After closure of the surgical wound, the FIB was initiated using a bullet-tipped needle and plastic catheter (TuoRen, TuoRen Ltd, China). A line was drawn on the skin from the pubic tubercle to the anterior superior iliac spine and divided into three equal sections. The puncture site was located 2 cm to 3 cm caudal to the medial one-third point of this line. The needle was inserted following a ‘double pop’ sensation to enter the fascia iliac. The cannula was advanced at least 5 cm cranially, and then a 16-gauge styletted catheter was inserted through the tip of the cannula for 10 cm. The catheter was secured with medical tape. One bolus of 20 mL (body weight <50 kg), 25 mL (body weight 50 kg to 70 kg) or 30 mL (body weight >70 kg) 0.5% ropivacaine solution was then infused, after which an electronic pump (Apon, Apon Ltd, China) with prefilled solution at a concentration of 0.25% ropivacaine was connected to the catheter. The infusion was then started at a speed of 0.1 mL/kg/h. After 48 h, catheters were carefully removed and 1 cm of the distal portion was cut and cultured.
In the PCIA group, fentanyl (110 μg to 120 μg) and 4 mg tropisetron were mixed with saline water for infusion for 48 h using an infusion pump (TuoRen, TuoRen Ltd, China). The parameters of PCIA were set at a base infusion rate of 2 mL/h and bolus application of 2 mL/15 min.
Postoperative pain (primary outcome) was screened by a nurse using a numerical rating scale (NRS) on which 0 indicated “no pain” and 10 indicated “worst pain ever”. Pain assessments were repeated at 2 h, 4 h, 6 h, 12 h, 24 h and 48 h after analgesia was started. The opioid related symptoms (secondary outcome), such as postoperative nausea and vomiting (PONV), and pruritus, were also monitored. After admission, patients were screened daily by the nurse on duty for delirium. Satisfaction with analgesia was noted as an overall rating of “Yes” or “No”.
Oral analgesia (acetaminophen and dihydrocodeine tartrate tablets) was given when postoperative pain reached 4 of 10 on an NRS. Five milligrams of intramuscular morphine was given when pain reached 6 of 10 on an NRS on routine pain assessment. Additional analgesia was recorded to evaluate the efficacy of the main analgesic technique. The dose of additional analgesia was indicated as morphine (mg) opioid equivalents for comparison between groups.
Data are presented as mean and SEM. Pain scores were analyzed using a repeated-measures ANOVA (RM-ANOVA) with condition (FIB or PCIA) and time (six time points). The age, body weight, time from admission to surgery, blood loss and wound length were analyzed between groups using a one-way ANOVA. The number of patients with PONV, pruritus or delirium, and satisfaction ratings were compared between groups using the χ2 test. The Newman-Keuls test was used as a post hoc test in case of significant ANOVA factors. P<0.05 was considered to be statistically significant.
RESULTS
A total of 106 patients were approached and assigned to either the FIB or the PCIA group (53 per group). Two patients in the FIB group did not complete the protocol due to catheter failure. Therefore, 51 patients in the FIB group completed the protocol. There was no significant difference in age, body weight, time from admission to surgery, duration of hospital stay, wound length and blood loss during surgery between the groups (Table 1). Patients in the FIB group reported less pain than those in the PCIA group (RM-ANOVA P=0.039; 95% CI −1.10 to −0.03). Pain score changed similarly over time in both groups; the peak score occurred at 6 h postsurgery (Figure 1). There were six patients with PONV (χ2 P=0.013) and five patients with pruritus (χ2 P=0.025) in the PCIA group, while no PONV or pruritus were observed in the FIB group. However, 20 (39.2%) patients in the FIB group required additional analgesia (six patients had morphine injected [5 mg/person] and 14 patients received oral analgesia). Twenty-two (41.5%) patients in the PCIA group received additional analgesia, including morphine injection in eight patients (5 mg/person) and oral analgesia in 14 patients. FIB groups received postoperative analgesia equivalent to 7.35±2.18 mg morphine, compared with 65.83±2.13 mg in the PCIA group (P<0.0001). No patients developed delirium before surgery in either group. Ten (19.6%) patients in the FIB group and three (5.7%) patients in the PCIA group (χ2 P=0.032) developed postoperative delirium. No patients reported irritation of the FIB catheter. There were no bacteria cultivated on the tip of catheter and no signs of infection were noted.
TABLE 1.
Comparison between fascia iliaca compartment block (FIB) and patient-controlled intravenous analgesia (PCIA) groups
| FIB | PCIA | P | |
|---|---|---|---|
| Patients | 51 | 53 | |
| Age, years | 73.6±2.1 | 68.2±2.1 | 0.07 |
| Body weight, kg | 54.6±1.4 | 57.5±1.4 | 0.14 |
| Time from admission to surgery, days | 7.6±0.5 | 7.7±0.5 | 0.92 |
| Duration of hospital stay, days | 23±1.2 | 21.5±1.2 | 0.37 |
| American Society of Anesthesiologists score | |||
| 1 | 3 | 1 | 0.307 |
| 2 | 20 | 31 | 0.062 |
| 3 | 28 | 21 | 0.165 |
| Blood loss, mL | 160±26.9 | 171±26.4 | 0.78 |
| Wound length, cm | 7.7±0.3 | 7.8±0.3 | 0.833 |
| Satisfaction, % | 92.5 | 94.3 | 0.79 |
| Side effects | |||
| Postoperative nausea and vomiting | 0 | 6 | 0.013* |
| Pruritus | 0 | 5 | 0.025* |
| Additional analgesia | 20 | 22 | 0.811 |
| Delirium | 10 | 3 | 0.032* |
Significant difference between FIB and PCIA groups
Figure 1).
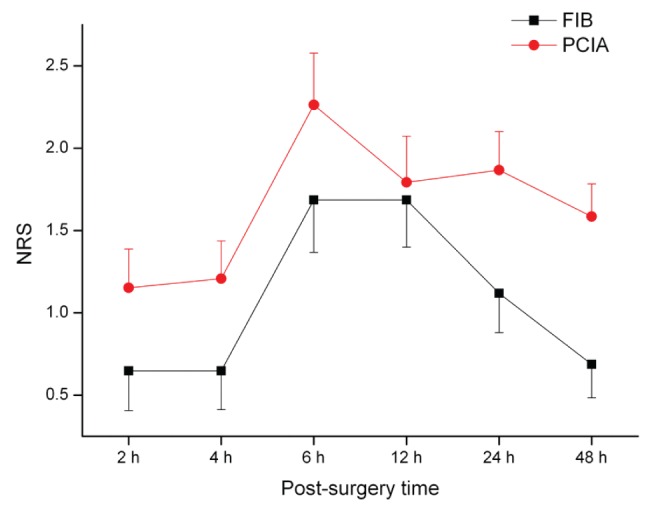
Pain rating after surgery for the fascia iliaca compartment block (FIB) and patient-controlled intravenous analgesia (PCIA) groups. NRS Numerical rating scale
DISCUSSION
Patients who received FIB reported less postoperative pain than those who received PCIA. Patients who received FIB did not experience PONV or pruritus after surgery. Nearly 40% of patients in both groups required additional analgesia. More patients developed delirium in the FIB group compared with the PCIA group.
The incision for hip fracture surgery is typically located on the lateral part of the hip, innervated by the lateral femoral cutaneous nerve. Block of the femoral cutaneous nerve using the FIB technique may produce effective analgesia in the innervated area because previous studies have shown that single FIB blocks are more effective than femoral nerve blocks in blocking the lateral femoral cutaneous nerve (7,8). Low pain scores were found for both groups at 2 h and 4 h postoperatively, which may be due to carry-over effects of general anesthesia plus flurbiprofen. However, continuous FIB effectively extended the duration of analgesic effects necessary for postoperative pain management. Foss et al (4) reported that a single FIB produced significant pain relief 180 min after hip fracture surgery. In the current study, continuous FIB produced significant pain relief at 12 h after surgery (maximum NRS score of 1.7 compared with the mean pain score of >2 in the study by Foss et al [4]), indicating that the continuous FIB technique provided longer analgesia than a single FIB and is suitable for postoperative management.
The cutaneous lateral femoral nerve and femoral nerve innervate the front and lateral portion of the thigh, including the skin, muscle and periosteum. The FIB technique targets mainly the cutaneous lateral femoral nerve and femoral nerves, blocking nociceptive input from those tissues. FIB has been used effectively as postoperative pain control in total knee arthroplasty (8). The approach of orthopedic surgery to correct hip fractures passes through the lateral part of the thigh. However, the sciatic nerve, which innervates the back portion of the thigh, is not blocked by FIB. Traction during surgery and hematomas at the surgery site may produce nociceptive stimulation to the receptors in the posterior periosteum of femoral bone, facilitating nociception transducted by the sciatic nerve. Insufficient blockage of the sciatic nerve may be the cause of additional analgesia needed. Nevertheless, patients were satisfied with both FIB and PCIA techniques in the current study. Postoperative pain intensity was not >2 on NRS in the FIB group. No adverse effects, such as pain at the insertion site or paresthesia, were observed in the FIB group. The FIB technique is associated with minimal risk because the puncture is made at a safe distance from the femoral artery and femoral nerve. Therefore, the FIB catheter was associated with fewer complications (such as vascular puncture and sensory block failure) in the current study compared with the femoral nerve block catheter described in a previous study (9). No positive cultures were observed with the FIB catheter tip, nor were there any signs of infection in the current study. This rate is considerably lower compared with 57% positive cultures of femoral nerve block catheters (9), providing evidence of safety with the FIB catheter technique.
Eleven patients in the PCIA group experienced PONV and pruritus. Those symptoms typically resolved after discontinuation of PCIA without intervention; therefore, they were considered to be opioid-related side effects. The FIB group did not experience these opioid-related side effects. The higher rate of opioid-related side effects was apparently due to the higher dose of opioid provided in the PCIA group. Caution should be taken to interpret these data because the number of patients who presented with symptoms of side effects was small. Nevertheless, the patients who received FIB were exposed to less opioids, while the postoperative analgesia effects were superior. This indicates the advantage of the FIB technique.
Ten patients in the FIB group and three patients in the PCIA group developed delirium. The development of delirium was related to risk factors such as recognition dysfunction, pain after an injury, mobility before injury, activities of daily living and comorbidities (10). The pain scores before surgery were similar for both groups (not reported), as were mobility and American Society of Anesthesiologists scores. Sieber et al (11) found that the opioid dose on postoperative day 2 was not predictive of incident delirium in elderly hip fracture patients. Therefore, the relatively higher opioid dose in the PCIA group would not be responsible for the lower incidence of delirium. In a previous study observing postoperative delirium performed in our department, 16 of 123 hip fracture patients receiving PCIA analgesia developed postoperative delirium (12). When data from both groups in the current study were pooled, 13 of 104 patients had postoperative delirium. The incidence of delirium was in accordance with our previous study (12). Therefore, the different incidence of delirium between two groups may be attributed to predisposing factors other than the analgesia techniques.
The limitation of the present study was the high proportion of patients who required additional analgesia. The low pain score recorded after surgery may reflect the combined effects of local anesthesia and additional systemic analgesia such as morphine injection or oral analgesia. Other analgesia, such as nonsteroidal anti-inflammatory drugs, was limited in the present trial to diminish the influence of different intake doses among patients. Multimodal pain management, as suggested by clinical pathways, may lead to greater patient satisfaction and less postoperative pain (13). The influence of femoral weakness due to FIB was not assessed because patients preferred to remain in bed, although the surgeon suggested mobilization immediately after surgery. Not ambulating during the 48 h after surgery was unlikely to be the reason for more delirium in the FIB group because patients in the PCIA group also did not ambulate.
CONCLUSION
Ccontinuous FIB is a safe and effective technique for postoperative analgesia after hip fracture surgery, making it an option for pain management in elderly hip fracture patients.
Acknowledgments
The study has been financed by Funds of Guiyang Science and Technology Department, Guiyang, People’s Republic of China.
Footnotes
DISCLOSURES: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Ekstein, Weinbroum AA. Immediate postoperative pain in orthopedic patients is more intense and requires more analgesia than in post-laparotomy patients. Pain Med. 2010;12:308–13. doi: 10.1111/j.1526-4637.2010.01026.x. [DOI] [PubMed] [Google Scholar]
- 2.Liu SS, Wu CL. The effect of analgesic technique on postoperative patient-reported outcomes including analgesia: A systematic review. Anesth Analg. 2007;105:789–808. doi: 10.1213/01.ane.0000278089.16848.1e. [DOI] [PubMed] [Google Scholar]
- 3.Morau D, Lopez S, Biboulet P, Bernard N, Amar J, Capdevila X. Comparison of continuous 3-in-1 and fascia iliaca compartment blocks for postoperative analgesia: Feasibility, catheter migration, distribution of sensory block, and analgesic efficacy. Reg Anesth Pain Med. 2003;28:309–14. doi: 10.1016/s1098-7339(03)00183-4. [DOI] [PubMed] [Google Scholar]
- 4.Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: A randomized, placebo-controlled trial. Anesthesiology. 2007;106:773–8. doi: 10.1097/01.anes.0000264764.56544.d2. [DOI] [PubMed] [Google Scholar]
- 5.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Cuignet O, Pirson J, Boughrouph J, Duville D. The efficacy of continuous fascia iliaca compartment block for pain management in burn patients undergoing skin grafting procedures. Anesth Analg. 2004;98:1077–81. doi: 10.1213/01.ANE.0000105863.04140.AE. [DOI] [PubMed] [Google Scholar]
- 7.Lako SJ, Steegers MA, van Egmond J, Gardeniers J, Staals LM, van Geffen GJ. Incisional continuous fascia iliaca block provides more effective pain relief and fewer side effects than opioids after pelvic osteotomy in children. Anesth Analg. 2009;109:1799–803. doi: 10.1213/ANE.0b013e3181bbc41a. [DOI] [PubMed] [Google Scholar]
- 8.Brisbane Orthopaedic & Sports Medicine Centre Writing Committee. McMeniman TJ, McMeniman PJ, Myers PT, et al. Femoral nerve block vs fascia iliaca block for total knee arthroplasty postoperative pain control: A prospective, randomized controlled trial. J Arthroplasty. 2010;25:1246–9. doi: 10.1016/j.arth.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 9.Cuvillon P, Ripart J, Lalourcey L, et al. The continuous femoral nerve block catheter for postoperative analgesia: Bacterial colonization, infectious rate and adverse effects. Anesth Analg. 2001;93:1045–9. doi: 10.1097/00000539-200110000-00050. [DOI] [PubMed] [Google Scholar]
- 10.Bruce AJ, Ritchie CW, Blizard R, Lai R, Raven P. The incidence of delirium associated with orthopedic surgery: A meta-analytic review. Int Psychogeriatr. 2007;19:197–214. doi: 10.1017/S104161020600425X. [DOI] [PubMed] [Google Scholar]
- 11.Sieber FE, Mears S, Lee H, Gottschalk A. Postoperative opioid consumption and its relationship to cognitive function in older adults with hip fracture. J Am Geriatr Soc. 2011;59:2256–62. doi: 10.1111/j.1532-5415.2011.03729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nie H, Zhao B, Zhang YQ, Jiang YH, Yang YX. Pain and cognitive dysfunction are the risk factors of delirium in elderly hip fracture Chinese patients. Arch Gerontol Geriatr. 2012;54:e172–4. doi: 10.1016/j.archger.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Alzahrani K, Gandhi R, Davis A, Mahomed N. In-hospital mortality following hip fracture care in southern Ontario. Can J Surg. 2010;53:294–8. [PMC free article] [PubMed] [Google Scholar]


