Abstract
Background
This study sought to determine the prevalence of distribution of fertility preservation (FP) materials, source of the materials, and providers’ perceived relevance of the materials among a sample of US oncologists.
Methods
A 53-item survey was administered via mail and the Web to a stratified sample of oncologists from the American Medical Association Masterfile. This study represents a subset of results, reporting on three survey items.
Results
Among the 511 oncologists (32% response rate), only 13.5% (n = 69) reported ‘always or often’ giving their patients educational materials about FP. Among those who reported ever distributing materials, 39.5% used American Cancer Society materials, 11.0% used Fertile Hope, 6.4% used Lance Armstrong Foundation, and 11.8% used ‘other’. Among those who provided materials, only 27.4% believe the FP materials they provide are ‘relevant to patient’s specific cancer diagnosis’.
Conclusion
There is need to improve oncologists’ distribution of FP educational materials to patients with cancer.
Keywords: educational materials, fertility preservation, oncologists, cancer, communication
Introduction
Advancements in cancer treatment and early detection have increased the survival rates of young men and women diagnosed with cancer [1]. These improvements have shifted the focus in survivorship research to improving quality of life among this growing population of survivors of cancer [2]. The same treatments that have successfully increased cancer survival may also damage gonadal tissue, ultimately resulting in infertility. Approximately 40–80% of women and 30–75% of men of child-bearing age are infertile following cancer treatments, with those receiving pelvic radiation and chemotherapy at greatest risk for infertility [3,4]. Fortunately, advances in reproductive medicine allow fertility preservation (FP) options for both male and female patients with cancer; however, FP options often are limited to a narrow window of opportunity: after diagnosis and prior to treatment. Consequently, receiving timely information regarding these risks and options may influence patients’ ability to pursue FP.
Many patients with cancer at risk for fertility-related complications do not receive timely information and face devastating and irreversible fertility impairment [5,6]. The focus on immediate survival often overshadows quality-of-life issues such as future fertility; although, survivorship issues become paramount once the crisis of diagnosis subsides. Loss of fertility as a result of cancer treatment is a reported source of distress among survivors of cancer of childbearing age [7,8]. Further, many survivors of cancer who express interest in future parenthood report that their cancer experience would make them better parents and indicate that they prefer to have biological children [5,9]. Having the option to preserve fertility would offer some solace to a patient distressed by fertility-related side effects of cancer treatment [10].
In recognition of the distress caused by infertility and informational gap in the conveyance of fertility-related information to patients, the American Society for Clinical Oncology (ASCO) established guidelines regarding the oncologist’s role to convey fertility information to patients with cancer: ‘…as part of education and informed consent before cancer therapy, oncologists should address the possibility of infertility with patients…and be prepared to discuss possible fertility preservation options or refer…patients to reproductive specialists’ [10]. The oncologists’ role in these discussions is logical given that they primarily direct treatment planning, including writing the orders for chemotherapy and radiation. Furthermore, previous research highlights the value patients place on physician discussion above all other resources [11].
Despite ASCO guidelines, less than half of physicians refer patients of childbearing age for FP consults with a reproductive endocrinologist [12]. There are various barriers to FP referrals such as the treating physician’s knowledge and attitudes if it is outside their expertise, perceptions of the patient’s access to resources, or if it involves delaying treatment [6,13,14].
Even if communication is occurring, information may not be understood. Multiple studies demonstrate patients have a difficult time comprehending their medical information, particularly with respect to oncology and treatment-related terminology [12–15]. Furthermore, patients typically recall less than 50% of important information given to them verbally [6,14]. The role of cancer education materials is to empower the patient. Evidenced by these studies, the method of transmitting information is just as important as the communication itself.
To assist physicians with this communication process and improve patient comprehension and recall, educational materials may be an effective and low burden method to convey critical fertility information. Educational materials have been shown to be an effective medium to convey important health messages, increase knowledge on a variety of health topics, and have the further advantage of being simplified to present information more effectively to low-literacy populations [15–19]. Furthermore, educational materials are specifically beneficial for FP as organizational websites, and additional contact information could be incorporated to facilitate patients locating medical facilities to pursue FP. Directly receiving educational materials from one’s physician compared with receiving mailed educational materials is an important element of the patient’s perception that their physician agrees with and supports the content of the education, and corresponds with increased patient satisfaction [11–20].
Although educational materials provide a potentially effective method to convey critical information, the distribution of educational materials about FP is undocumented. The primary aims of the present study were to determine the prevalence of providers’ distribution of FP materials to patients and to assess physician and practice characteristics associated with distribution.
Materials and methods
A stratified random sample of US oncologists obtained from the American Medical Association Masterfile was recruited by US mail. The sample included physicians specializing in hematology/medical oncology, gynecologic oncology, surgical oncology, radiation oncology, and musculoskeletal oncology. In addition to specialty, other eligibility criteria included (i) graduation from medical school after 1945, (ii) practicing medicine in the USA, including Puerto Rico, and (iii) those who list patient care as their primary job and locum tenens.
Recruitment
A three-phased recruitment approach patterned after the Dillman method was utilized [21]. Study packets were mailed in Phase 1; packets included a letter explaining the study, paper survey, and pre-addressed postage-paid envelope. The letter included a website for participants to access an electronic version of the survey. A $100 honorarium was offered to those completing the survey. Requests for the honorarium could be made by returning the pre-addressed postcard provided in the study packet or by sending an email with contact information to the study team.
Measures
A 53-item survey was developed to measure the practice patterns related to FP and included five sections including demographic and clinical characteristics, attitudes, knowledge, barriers, and practice behaviors related to FP in patients with cancer of childbearing age (16–44 years). The survey development and survey items are detailed in a previous publication [12]. This study represents a subset of results focused on three practice behavior items measuring provision, source, and relevance of educational materials.
Provision of educational materials
Provision of educational materials was measured by physicians’ agreement using a five-point Likert-style system (always–never) to the question: ‘I provide my patients with educational materials about fertility preservation’. Those who responded ‘never’ were instructed to skip other educational material items. For data analysis, responses were dichotomized by those who ‘never’ or ’rarely’ provide educational materials compared with those who ‘sometimes’, ‘often’, or ‘always’ provide these materials.
Source of educational materials
Source of educational materials was measured by physicians’ response to ‘If educational materials are provided, where is this information from?’ Response options included ‘American Cancer Society, Fertile Hope,1 Lance Armstrong Foundation, I do not provide information to my patients, and Other: please specify’.
Relevance of educational materials
Relevance of educational materials was measured using physicians’ level of agreement with the question: ‘Do you believe the educational materials you provide to your patients are relevant to their specific cancer diagnosis?’ Responses were captured using a five-point Likert-style system (always–never) and an additional response option, ‘I do not provide any materials’.
Data analyses
Frequencies were obtained to determine the proportion of physicians who reported distribution of FP educational materials. A chi-square test of homogeneity was performed to determine whether educational material sources were related to perceived material relevance. Simple logistic regression models were conducted to determine if ‘rarely/never’ providing educational materials was related to demographic and clinical characteristics. A multiple logistic regression was used to determine which variables were statistically significant predictors of ‘never’ providing educational materials whereas controlling for other independent variables. Considering the exploratory nature of these analyses, a backward elimination process was used. Analyses were conducted using SPSS v.17.0, and all tests were two-sided with a declared significance at the 5% level.
Results
Of the 1979 physicians recruited, 613 completed the survey, yielding a response rate of 32%. This rate is slightly higher than the average response rate in previous physician samples [22,23]. After exclusions for missing data and providers who did not report treating patients of reproductive age, the final analyses included 511 physicians. The majority of the sample was male (70.8%), White (76.7%), not Hispanic or Latino (94.5%), Catholic (29.8%), and had children (85.1%). Most physicians graduated from medical school in 1991 or earlier (68.2%) and specialized in medical oncology or hematology (31.9%). The primary practice location for most participants was a teaching hospital, university-affiliated cancer center, National Cancer Institute-designated cancer center, or another location other than a private oncology practice (68.1%). The majority of physicians were unaware of ASCO guidelines (62.8%). A complete description of demographic characteristics can be obtained from a previous publication [12].
Provision of educational materials
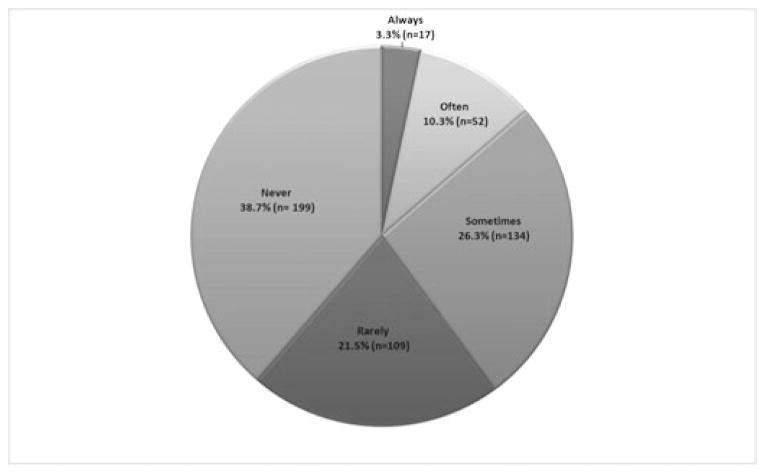
Among the 511 oncologists, 13.6% (n = 69) reported ‘always’ or ‘often’ giving their patients educational materials about FP, whereas 26.3% (n = 233) reported ‘sometimes’, and 60.2% (n = 308) reported ‘rarely’ or ‘never’ providing educational materials (Figure 1).
Figure 1.
Physician provision of FP-related educational materials
Source of educational materials
The majority of the sample indicated they do not provide FP educational materials on a regular basis (n = 244, 47.3%). Physicians mostly reported receiving educational material from one source (n = 203, 39.3%), and 64 (13.4%) used multiple sources. Among those who reported ever giving materials, 204 (39.5%) used American Cancer Society (ACS) materials, 57 (11%) used Fertile Hope, 33 (6.4%) used Lance Armstrong Foundation, and 61 (11.8%) used ‘other’. Only 15 out of 61 of those who specified ‘other’ provided information about source: local specialist (n = 2), local publication (n = 7), Internet (n = 2), literature (n = 1), own data (n = 2), and ASCO (n = 1).
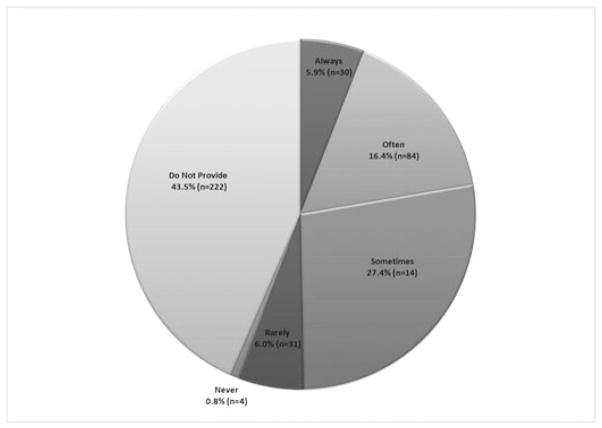
Physicians’ perceived relevance of materials
Among those who provided materials, 27% believed the FP materials they provided were ‘relevant to patient’s specific cancer diagnosis’ (Figure 2). Chi-square analyses were conducted among providers who listed one source for educational materials (physicians who reported using multiple sources were excluded). Physicians who reported using the ACS as the primary educational material source perceived the material to be more relevant to a patient’s diagnosis compared with physicians who use ‘other’ sources (p < .01). Physicians did not indicate a difference in relevance of ACS, Fertile Hope, or Lance Armstrong Foundation materials (p > .05).
Figure 2.
Physicians’ opinion of the relevance of FP educational materials
Simple bivariate analyses
Results from simple logistic regression analyses indicated that significant predictors of ‘rarely/never’ providing educational materials were specialty in surgery and musculoskeletal/orthopedic oncology, size of practice setting, and being unaware of ASCO guidelines. Compared with those specializing in medical oncology/hematology, those specializing in surgical oncology (odds ratio (OR) = 1.67; 95% CI, 1.04–2.77) and musculoskeletal/orthopedic oncology (OR = 4.87; 95% CI, 1.06–2.44) had a greater odds of reporting ‘rarely/never’ providing materials. Physicians practicing in a medium (OR = 0.64; 95% CI, 0.40–0.99) or large (OR = 1.99; 95% CI, 0.41–0.95) setting had a greater odds of ‘rarely/ never’ providing materials relative to physicians practicing in a small setting. Finally, those who reported being unaware of the ASCO guidelines had a higher odds of ‘rarely/never’ providing materials compared with those aware of the guidelines (OR = 3.56; 95% CI, 2.37–5.33).
Multivariate analyses
A multiple logistic regression was conducted to ascertain significant predictors associated with physicians who reported they ‘rarely’ or ‘never’ provide educational materials compared with those who responded otherwise. Using the backward elimination method, factors that significantly predicted physicians ‘rarely/never’ providing educational materials included specialty in radiology (p < .001), size of practice setting (p < .05), and those unaware of ASCO guidelines (p < .001). Physicians specializing in radiology (OR = 0.51; 95% CI, 0.32–0.82) were half as likely to state that they ‘rarely’ or ‘never’ provided educational materials. Physicians unaware of guidelines were about four times as likely to state they ‘rarely/never’ provide education materials (OR = 3.97; 95% CI, 2.60–6.06) compared with physicians aware of guidelines.
Discussion
Approximately 60% of physicians surveyed reported they rarely or never provide educational materials about FP to their patients of childbearing age. The provision of patient-based education materials is a prime component of patient-centered care and quality cancer care [24]. Education materials are particularly important when dealing with issues of fertility for patients with cancer as FP procedures are performed outside of the oncology setting. The patient is then connected with a specialized physician or printed resources that can address to specific FP-related concerns, whereas their treating oncologist may not know all the available information. A recent review of cancer communication and health literacy identified one of the most effective means of providing education to patients was a combination of physician–patient discussion followed by the provision of printed materials [25]. Considering that most patients retain less than 50% of critical information provided to them and the stress of a cancer diagnosis, the need for take-home materials is essential for improved understanding and decision making [26].
Among the 53% of physicians who do provide materials at least occasionally, the majority offer information from the ACS; however, only 27% perceive these materials to be relevant to their patient’s cancer diagnosis. Although the ACS materials were identified as the most widely distributed, ACS, Fertile Hope, and Lance Armstrong all provide FP education materials that are patient-oriented. These national organizations are a trusted source of information for many patients; however it is not clear why ACS materials are preferred or why some materials are deemed more relevant than others.
It is significant that the primary source of distributed FP materials is produced by the ACS, a reputable organization that patients may feel confident in. However, further research is needed to determine what happens after educational materials are distributed and if systems are in place to assist patients with navigation.
Limitations
Although these results provide insight into the practice behaviors of physicians regarding provision of FP educational materials, our study has limitations. The self-report nature of this study may have elicited socially desirable responses rather than an accurate representation of physician practice behaviors. Yet, the anonymity of the survey likely reduced the potential for social response bias. A second and related consideration of this study is the discrepancy in provision of educational material reports dependent on how the question was presented. When asked directly about the rate of provision of educational materials, about 39% (n = 199) reported ‘never’ providing educational materials; however, when asked to disclose the source of educational materials, 47% (n = 244) report that ‘they do not provide educational materials on a regular basis’ and thus, could not provide a source of educational materials. Further, 45% (n = 222) of physicians reported they ‘do not provide educational materials’ in a question pertaining to physicians’ opinion on relevance of educational materials. Wording of questions is an important consideration for future research on physician practice behavior. Another consideration of this study is the low response rate, even though our 32% return in this study is comparable with previous studies with physician respondents [22,23]. Moreover, it is possible that physicians with particular interest in the topic of FP may have been inclined to reply to the survey, thereby limiting the generalizability of our results. Although these associations are important additions to the knowledge of FP practice behaviors, a temporal relationship between variables cannot be determined.
Conclusions
The results of this study highlight the need to improve oncologists’ offering of FP educational materials to patients with cancer. Future research is needed to probe physicians’ and patients’ opinions of educational materials to further refine available materials to perhaps improve relevance. These results demonstrate that knowledge of FP practice guidelines is an important factor in predicting use of educational materials. This study establishes the need for the propagation of FP educational materials and further suggests that dissemination of ASCO guidelines and possible refinement of materials may be effective routes to increase provision of FP educational materials.
Acknowledgments
This research was supported by a grant from the American Cancer Society [RSGPB07-019-01-CPPB].
Footnotes
As of 2009, Fertile Hope is an initiative of the Lance Armstrong Foundation and Livestrong.
References
- 1.Greenlee R, Hill-Harman M, Murray T. Cancer statistics, 2001. CA Cancer J Clin. 2001;51:15–36. doi: 10.3322/canjclin.51.1.15. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Institute. What you need to know about cancer: an overview. http://www.cancer.gov/cancertopics/wyntk/overview.
- 3.Brannigan RE. Fertility Preservation in Adult Male Cancer Patients. In: Woodruff TK, Snyder KA, editors. Oncofertility: Fertility Preservation for Cancer Survivors. Boston: Springer Press; 2007. [Google Scholar]
- 4.Sonmezer M, Oktay K. Fertility preservation in young women undergoing breast cancer therapy. Oncologist. 2006;11:422–434. doi: 10.1634/theoncologist.11-5-422. [DOI] [PubMed] [Google Scholar]
- 5.Schover LR, Brey K, Lichtin A, Lipshultz L, Jeha S. Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol. 2002;20:1880–1889. doi: 10.1200/JCO.2002.07.175. [DOI] [PubMed] [Google Scholar]
- 6.Quinn G, Vadaparampil S, Gwede C, et al. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1:146–155. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- 7.Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer LK. Fertility issues for young adult survivors of childhood cancer. Psycho-Oncology. 2004;13:689–699. doi: 10.1002/pon.784. [DOI] [PubMed] [Google Scholar]
- 8.Carter J, Chi DS, Brown CL, et al. Cancer-related infertility in survivorship. Int J Gynecol Cancer. 2010;20:2–8. doi: 10.1111/IGC.0b013e3181bf7d3f. [DOI] [PubMed] [Google Scholar]
- 9.Schover LR, Rybicki LA, Martin BA, Bringelsen KA. Having children after cancer. Cancer. 1999;86:697–709. doi: 10.1002/(sici)1097-0142(19990815)86:4<697::aid-cncr20>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 10.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 11.Terry P, Healey M. The physician’s role in educating patients: a comparison of mailed versus physician-delivered patient education. J Fam Pract. 2000;49:314–318. [PubMed] [Google Scholar]
- 12.Quinn GP, Vadaparampil ST, Lee JH, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–5957. doi: 10.1200/JCO.2009.23.0250. [DOI] [PubMed] [Google Scholar]
- 13.Quinn GP, Vadaparampil ST, Bell-Ellison BA, Gwede CK, Albrecht TL. Patient-physician communication barriers regarding fertility preservation among newly diagnosed cancer patients. Soc Sci Med. 2008;66:784–789. doi: 10.1016/j.socscimed.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20:1890–1897. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 15.Safeer R, Keenan J. Health literacy: the gap between physicians and patients. Am Fam Physician. 2005;72:463–468. [PubMed] [Google Scholar]
- 16.Schwartz MD, Benkendorf J, Lerman C, Isaacs C, Ryan-Robertson A, Johnson L. Impact of educational print materials on knowledge, attitudes, and interest in BRCA1/ BRCA2. Cancer. 2001;92:932–940. doi: 10.1002/1097-0142(20010815)92:4<932::aid-cncr1403>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 17.Barlow J, Wright C. Knowledge in patients with rheumatoid arthritis: a longer term follow-up of a randomized controlled study of patient education leaflets. Rheumatology. 1998;37:373–376. doi: 10.1093/rheumatology/37.4.373. [DOI] [PubMed] [Google Scholar]
- 18.Stewart DE, Lickrish GM, Sierra S, Parkin H. The effect of educational brochures on knowledge and emotional distress in women with abnormal Papanicolaou smears. Obstet Gynecol. 1993;81:280–282. [PubMed] [Google Scholar]
- 19.Hanrahan PF, Hersey P, Watson AB, Callaghan TM. The effect of an educational brochure on knowledge and early detection of melanoma. Aust J Public Health. 1995;19:270–274. doi: 10.1111/j.1753-6405.1995.tb00442.x. [DOI] [PubMed] [Google Scholar]
- 20.McVea KL, Venugopal M, Crabtree BF, Aita V. The organization and distribution of patient education materials in family medicine practices. J Fam Pract. 2000;49:319–326. [PubMed] [Google Scholar]
- 21.Dillman D. Mail and Telephone Surveys: The Total Design Method. Wiley; New York, NY: 1978. [Google Scholar]
- 22.McCloskey SA, Tao ML, Rose CM, Fink A, Amadeo AM. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J. 2007;13:130–137. doi: 10.1097/PPO.0b013e31804675d4. [DOI] [PubMed] [Google Scholar]
- 23.Thorpe C, Ryan B, McLean SL, et al. How to obtain excellent response rates when surveying physicians. Fam Pract. 2009;26:65–68. doi: 10.1093/fampra/cmn097. [DOI] [PubMed] [Google Scholar]
- 24.Rudd RE, Moeykens BA, Colton TC. Health and literacy: a review of medical and public health literature. In: Comings J, Garners B, Smith C, editors. Health and Literacy. Jossey-Bass; New York, NY: 1999. [Google Scholar]
- 25.Davis TC, Williams MV, Marin E, Parker RM, Glass J. Health literacy and cancer communication. CA Cancer J Clin. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 26.Tabak N. Decision making in consenting to experimental cancer therapy. Cancer Nurs. 1995;18:89–96. [PubMed] [Google Scholar]