Abstract
BACKGROUND
Randomized trials and observational studies have shown that perioperative morbidity and mortality are lower with endovascular repair of abdominal aortic aneurysm than with open repair, but the survival benefit is not sustained. In addition, concerns have been raised about the long-term risk of aneurysm rupture or the need for reintervention after endovascular repair.
METHODS
We assessed perioperative and long-term survival, reinterventions, and complications after endovascular repair as compared with open repair of abdominal aortic aneurysm in propensity-score–matched cohorts of Medicare beneficiaries who underwent repair during the period from 2001 through 2008 and were followed through 2009.
RESULTS
We identified 39,966 matched pairs of patients who had undergone either open repair or endovascular repair. The overall perioperative mortality was 1.6% with endovascular repair versus 5.2% with open repair (P<0.001). From 2001 through 2008, perioperative mortality decreased by 0.8 percentage points among patients who underwent endovascular repair (P = 0.001) and by 0.6 percentage points among patients who underwent open repair (P = 0.01). The rate of conversion from endovascular to open repair decreased from 2.2% in 2001 to 0.3% in 2008 (P<0.001). The rate of survival was significantly higher after endovascular repair than after open repair through the first 3 years of follow-up, after which time the rates of survival were similar. Through 8 years of follow-up, interventions related to the management of the aneurysm or its complications were more common after endovascular repair, whereas interventions for complications related to laparotomy were more common after open repair. Aneurysm rupture occurred in 5.4% of patients after endovascular repair versus 1.4% of patients after open repair through 8 years of follow-up (P<0.001). The rate of total reinterventions at 2 years after endovascular repair decreased over time (from 10.4% among patients who underwent procedures in 2001 to 9.1% among patients who underwent procedures in 2007).
CONCLUSIONS
Endovascular repair, as compared with open repair, of abdominal aortic aneurysm was associated with a substantial early survival advantage that gradually decreased over time. The rate of late rupture was significantly higher after endovascular repair than after open repair. The outcomes of endovascular repair have been improving over time. (Funded by the National Institutes of Health.)
The use of endovascular repair of abdominal aortic aneurysms is increasing. By 2010, endovascular repair accounted for 78% of all intact repairs.1,2 Randomized, controlled trials comparing endovascular repair with open repair generally have shown a perioperative benefit of endovascular repair over open repair.3-5 Long-term survival, however, is similar with the two approaches.6-9 As data on long-term outcomes accumulate, concerns have been raised about endovascular repair with respect to the increased rate of late failure leading to rupture and higher rates of reintervention.
In our previous analyses performed with the use of Medicare data, which account for more than 83% of repairs of abdominal aortic aneurysms performed in the United States,10,11 the findings with respect to survival outcomes were similar to those observed in other trials,3-9 but we also found that at the 4-year follow-up there was an increased rate of reintervention related to the management of the aneurysm or its complications (aneurysm-related intervention) in the endovascular-repair group, which was balanced by an increased rate of reintervention for complications related to laparotomy in the open-repair group. Long-term data from the randomized Open Versus Endovascular Repair (OVER) trial confirmed this finding,7 although long-term data derived from the Endovascular Aneurysm Repair 1 (EVAR-1) trial9 and the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial6 did not include all complications related to laparotomy. In addition, our previous analysis did not account for prior laparotomy, which is a variable that might have had an influence on the choice of treatment.11
In the current observational study, we compared endovascular repair with open repair with respect to the long-term (up to 8 years) outcomes of each procedure, accounting for prior laparotomy, in propensity-score–matched cohorts of Medicare beneficiaries. We also examined whether perioperative and 2-year outcome event rates have changed over time as practitioners have gained experience with this evolving technology.
METHODS
STUDY DESIGN AND OVERSIGHT
In this retrospective propensity-score–matched cohort study, we identified all traditional Medicare beneficiaries who underwent elective endovascular repair or open repair of abdominal aortic aneurysm between January 1, 2001, and December 31, 2008. The study was approved by the institutional review board at Harvard Medical School. The authors attest to the accuracy and completeness of the data and the analyses.
PATIENTS
Patients were included in the study if they had been continuously enrolled in traditional Medicare Parts A and B for at least 2 years before the repair, had received a discharge diagnosis of abdominal aortic aneurysm, and had undergone open repair or endovascular repair. We excluded all patients who had ruptured abdominal aortic aneurysms, thoracic aneurysms, thoracoabdominal aortic aneurysms, or aortic dissections. In addition, we excluded those who had undergone visceral bypass or renal bypass. Data on beneficiaries who enrolled in Medicare Advantage during the follow-up period (see the Methods section in the Supplementary Appendix, available with the full text of this article at NEJM.org) were censored from the analyses of complications and reinterventions because subsequent claims data were not available.
A full list of the diagnostic and procedural codes that were used in these analyses is provided in the Supplementary Appendix; the list includes diagnostic and complication codes from the International Classification of Diseases, Ninth Revision, Clinical Modification, and Current Procedural Terminology codes used by the physicians. To improve coding accuracy for repair type, we compared the claims made by the physicians with the corresponding hospitalization codes. In cases in which the codes used by the hospital conflicted with those used by the physician, we assigned procedures on the basis of the physicians’ claims.
PROPENSITY-SCORE MATCHING
To control for the nonrandom assignment of patients, we constructed logistic-regression models that predicted the likelihood of endovascular repair (the propensity score) and matched patients in each cohort by this score. We used as explanatory variables all demographic and clinical characteristics of beneficiaries that were available from the 2-year period before their aneurysm repair, except for diagnoses from the index admission.12 We also identified abdominal operations (excluding the index operation) during the previous 2 years, which were classified according to a three-level categorical variable that was based on the likelihood of late complications (i.e., laparoscopic, minor open, or major open surgery), as well as prior retroperitoneal and hernia operations, which also confer an increased risk of subsequent complications.13 We determined the rates of coexisting conditions using a version of the Elixhauser algorithm that was adapted to include diagnoses from the outpatient setting.14,15 The propensity-score models also included an indicator variable for year to control for time. To ensure close matches, we required that the estimated log-odds scores predicting endovascular repair for matched pairs be within 0.60 standard-deviation units of each other, which ensures that approximately 90% of bias due to differences in observed covariates will be removed in estimates of effects.16,17
OUTCOMES
Outcomes of interest included perioperative and long-term survival, complications, length of hospital stay, repeat hospitalizations, and reinterventions. Perioperative death was defined as death during the index admission or within 30 days after surgery. Death in the long term included all deaths during the follow-up period, for which the data were available from the Medicare Beneficiary Summary File.
We identified perioperative surgical complications (e.g., conversion from endovascular to open repair or return to the operating room) and medical complications (e.g., myocardial infarction or pneumonia) with the use of relevant diagnostic and procedural codes as described above. We also recorded length of stay in the hospital and whether patients were discharged home.
We identified all hospitalizations and outpatient interventions that occurred after repair and were potentially related to the abdominal aortic aneurysm; these included hospitalizations for aneurysm rupture, major reinterventions (e.g., open repair of the aneurysm or pseudoaneurysm or repair of graft-enteric fistula or graft infection), and minor reinterventions (e.g., stent-graft extension, embolization, aortic or iliac angioplasty, or graft thrombectomy). We also identified complications related to laparotomy that required procedures (e.g., lysis of adhesions, bowel resection, or repair of hernia of the abdominal wall) and readmissions for bowel obstruction that did not lead to surgery.
STATISTICAL ANALYSES
We compared the characteristics of the unmatched cohorts using the chi-square test or Student’s t-test, as appropriate. To account for the dependence of the matched pairs, between-group differences after propensity-score matching were tested with the McNemar’s test for categorical variables or with a paired Student’s t-test for continuous variables. We estimated the association between the initial treatment strategy and the rates of the outcomes of interest for the matched pairs and determined the significance of the differences using the McNemar’s test. P values of less than 0.05 were considered to indicate statistical significance. Rates of survival, freedom from rupture, and reintervention related to abdominal aortic aneurysm were estimated with the use of Kaplan–Meier life-table methods, and comparisons were made with the use of a log-rank analysis. To evaluate changes in event rates over time, we analyzed the perioperative and 2-year postoperative outcomes for each year in which the repairs were performed, from 2001 through 2008, with the use of individual-level multivariable models that controlled for clinical and demographic characteristics that might have changed over time. We also performed separate survival analyses on data from patients in whom repairs were performed during the period from 2001 through 2004 and those in whom repairs were performed during the period from 2005 through 2008.
We hypothesized that survivors of open repair might have a decreased risk of death once they had survived the surgery. We therefore used an adaptation of the Cox model that allows the effect of endovascular repair (vs. open repair) to change over time by using break points that were determined on the basis of empirical analyses.18 Additional details are provided in the Statistical Analysis section in the Supplementary Appendix.
To estimate the overall survival benefit of endovascular repair in the presence of time-varying treatment effects (or hazards), we computed the restricted mean survival time, which is defined as the total amount of time over a given follow-up period that a patient with given characteristics is expected to survive.19 The restricted mean survival time (or its proportional equivalent obtained by dividing by the follow-up time) may be plotted against the follow-up time to show the way in which the net (or aggregate) advantage of endovascular repair relative to open repair changes with the length of follow-up.
RESULTS
PATIENTS
We identified 128,598 patients, 67 years of age or older, who had undergone elective repair of abdominal aortic aneurysm from 2001 through 2008; a total of 79,463 patients had undergone endovascular repair, and 49,135 patients had undergone open repair. Baseline characteristics and coexisting conditions before propensity-score matching are shown in Table S1 in the Supplementary Appendix, and those after propensity-score matching are shown in Table 1. After matching, 79,932 patients remained in the study population (39,966 in each cohort); there were no clinically relevant differences in baseline characteristics between the two cohorts. A comparison of baseline characteristics of the matched and unmatched patients in the endovascular-repair cohort is shown in Table S2 in the Supplementary Appendix.
Table 1.
Baseline Characteristics of the Study Patients After Propensity-Score Matching.*
| Variable | Endovascular Repair (N = 39,966) |
Open Repair (N = 39,966) |
P Value |
|---|---|---|---|
| Year in which repair was performed — no. (%) | |||
| 2001 | 5,150 (12.9) | 5,166 (12.9) | 0.87 |
| 2002 | 5,860 (14.7) | 5,858 (14.7) | 0.98 |
| 2003 | 5,800 (14.5) | 5,839 (14.6) | 0.70 |
| 2004 | 6,073 (15.2) | 6,107 (15.3) | 0.74 |
| 2005 | 5,584 (14.0) | 5,663 (14.2) | 0.42 |
| 2006 | 4,588 (11.5) | 4,623 (11.6) | 0.70 |
| 2007 | 3,825 (9.6) | 3,731 (9.3) | 0.26 |
| 2008 | 3,086 (7.7) | 2,979 (7.5) | 0.15 |
| Male sex — no. (%) | 31,047 (77.7) | 31,012 (77.6) | 0.77 |
| Race or ethnic group — no. (%)† | |||
| White | 38,120 (95.4) | 38,093 (95.3) | 0.65 |
| Black | 1,119 (2.8) | 1,138 (2.8) | 0.69 |
| Hispanic | 227 (0.6) | 224 (0.6) | 0.89 |
| Other | 500 (1.3) | 511 (1.3) | 0.73 |
| Mean age — yr | 75.7 | 75.5 | <0.001 |
| Age category — no. (%) | |||
| 67–69 yr | 5,851 (14.6) | 5,968 (14.9) | 0.24 |
| 70–74 yr | 12,120 (30.3) | 12,192 (30.5) | 0.58 |
| 75–79 yr | 12,468 (31.2) | 12,297 (30.8) | 0.19 |
| 80–84 yr | 7,284 (18.2) | 7,217 (18.1) | 0.54 |
| ≥85 yr | 2,243 (5.6) | 2,292 (5.7) | 0.45 |
| Urgent admission — no. (%) | 2,071 (5.2) | 1,916 (4.8) | 0.01 |
| Prior abdominal aortic aneurysm — no. (%) | 27,534 (68.9) | 27,724 (69.4) | 0.15 |
| Coexisting conditions — no. (%) | |||
| MI in previous 6 mo | 629 (1.6) | 654 (1.6) | 0.48 |
| MI in previous 7–24 mo | 2,709 (6.8) | 2,686 (6.7) | 0.75 |
| Valvular heart disease | 3,467 (8.7) | 3,439 (8.6) | 0.73 |
| Congestive heart failure | 4,671 (11.7) | 4,630 (11.6) | 0.65 |
| Peripheral vascular disease | 7,897 (19.8) | 7,767 (19.4) | 0.25 |
| Neurovascular disease | 5,562 (13.9) | 5,544 (13.9) | 0.85 |
| Hypertension | 25,257 (63.2) | 25,137 (62.9) | 0.38 |
| Diabetes | 6,427 (16.1) | 6,373 (15.9) | 0.60 |
| COPD | 11,117 (27.8) | 11,102 (27.8) | 0.91 |
| Renal failure | 2,250 (5.6) | 2,197 (5.5) | 0.41 |
| End-stage renal disease | 165 (0.4) | 146 (0.4) | 0.28 |
| History of cancer | 6,710 (16.8) | 6,762 (16.9) | 0.62 |
| Obesity | 811 (2.0) | 787 (2.0) | 0.54 |
COPD denotes chronic obstructive pulmonary disease, and MI myocardial infarction.
Race or ethnic group was self-reported.
PERIOPERATIVE OUTCOMES
Perioperative mortality was 1.6% in the endovascular-repair cohort versus 5.2% in the open-repair cohort (relative risk of death with open repair, 3.22; 95% confidence interval [CI], 2.95 to 3.51; P<0.001). This benefit of lower mortality with endovascular repair was seen in all age groups (Table 2). The endovascular-repair cohort, as compared with the open-repair cohort, also had lower rates of perioperative medical and surgical complications (e.g., pneumonia in 3.8% vs. 12.9%, P<0.001), were more likely to have been discharged home (95.0% vs. 83.2%, P<0.001), and had a shorter length of stay in the hospital (3.5 days vs. 9.8 days, P<0.001) (Table 2). A comparison of the perioperative outcomes in the matched and unmatched patients in the endovascular-repair cohort is shown in Table S3 in the Supplementary Appendix.
Table 2.
Perioperative Outcomes after Endovascular Repair or Open Repair of Abdominal Aortic Aneurysm in a Propensity-Score–Matched Study Population.*
| Perioperative Outcome | Endovascular Repair (N = 39,966) |
Open Repair (N = 39,966) |
Relative Risk (95% CI) |
P Value |
|---|---|---|---|---|
| Death — no./total no. (%) | ||||
| All ages | 651/39,966 (1.6) | 2094/39,966 (5.2) | 3.22 (2.95–3.51) | <0.001 |
| 67–69 yr | 51/5851 (0.9) | 168/5968 (2.8) | 3.23 (2.37–4.41) | <0.001 |
| 70–74 yr | 138/12,120 (1.1) | 424/12,192 (3.5) | 3.05 (2.52–3.70) | <0.001 |
| 75–79 yr | 191/12,468 (1.5) | 648/12,297 (5.3) | 3.44 (2.93–4.03) | <0.001 |
| 80–84 yr | 187/7284 (2.6) | 564/7217 (7.8) | 3.04 (2.59–3.58) | <0.001 |
| ≥85 yr | 84/2243 (3.7) | 290/2292 (12.7) | 3.38 (2.67–4.28) | <0.001 |
| Medical complications — no. of patients (%) | ||||
| Myocardial infarction | 1013 (2.5) | 2064 (5.2) | 2.04 (1.89–2.19) | <0.001 |
| Pneumonia | 1522 (3.8) | 5139 (12.9) | 3.38 (3.19–3.57) | <0.001 |
| Acute renal failure | 1726 (4.3) | 4531 (11.3) | 2.63 (2.49–2.77) | <0.001 |
| Hemodialysis | 174 (0.4) | 244 (0.6) | 1.40 (1.16–1.70) | <0.001 |
| Deep-vein thrombosis | 362 (0.9) | 718 (1.8) | 1.98 (1.75–2.25) | <0.001 |
| Surgical complications — no. of patients (%) | ||||
| Reoperation for bleeding | 232 (0.6) | 454 (1.1) | 1.96 (1.67–2.29) | <0.001 |
| Tracheostomy | 78 (0.2) | 636 (1.6) | 8.15 (6.45–10.31) | <0.001 |
| Embolectomy | 446 (1.1) | 659 (1.6) | 1.48 (1.31–1.66) | <0.001 |
| Conversion from endovascular to open repair | 445 (1.1) | NA | ||
| Mesenteric ischemia | 232 (0.6) | 853 (2.1) | 3.68 (3.18–4.25) | <0.001 |
| Major amputation | 15 (<0.1) | 43 (0.1) | 2.87 (1.59–5.16) | <0.001 |
| Complications related to laparotomy | ||||
| Lysis of adhesions without resection | 17 (<0.1) | 460 (1.2) | 27.06 (16.68–43.90) | <0.001 |
| Bowel resection, small | 43 (0.1) | 136 (0.3) | 3.16 (2.25–4.46) | <0.001 |
| Bowel resection, large | 114 (0.3) | 349 (0.9) | 3.06 (2.48–3.78) | <0.001 |
| Ileus or bowel obstruction without resection | 1071 (2.7) | 6422 (16.1) | 6.00 (5.63–6.39) | <0.001 |
| Length of hospital stay — days | ||||
| Mean | 3.5±5.3 | 9.8±8.9 | NA | <0.001 |
| Median | 2 | 7 | NA | <0.001 |
| Discharged home (as opposed to an alternative facility)† | ||||
| All ages | 37,517/39,506 (95.0) | 31,692/38,085 (83.2) | 0.88 (0.87–0.88) | <0.001 |
| 67–69 yr | 5703/5819 (98.0) | 5418/5822 (93.1) | 0.95 (0.94–0.96) | <0.001 |
| 70–74 yr | 11,689/12,022 (97.2) | 10,586/11,807 (89.7) | 0.92 (0.92–0.93) | <0.001 |
| 75–79 yr | 11,733/12,330 (95.2) | 9637/11,707 (82.3) | 0.87 (0.86–0.87) | <0.001 |
| 80–84 yr | 6539/7154 (91.4) | 4820/6709 (71.8) | 0.79 (0.77–0.80) | <0.001 |
| ≥85 yr | 1853/2181 (85.0) | 1231/2040 (60.3) | 0.71 (0.68–0.74) | <0.001 |
| Readmission within 30 days after discharge — no. of patients (%) |
4278 (10.7) | 4395 (11.0) | 1.03 (0.99–1.07) | 0.18 |
Plus–minus values are means ±SD. In the total cohort of Medicare beneficiaries (i.e., before propensity-score matching), 79,463 patients underwent endovascular repair and 49,135 underwent open repair. The rate of death among the patients of all ages in the total cohort was 1.6% (1270 patients) in the endovascular-repair cohort and 5.2% (2561 patients) in the open-repair cohort (relative risk, 3.26; 95% CI, 3.05 to 3.48; P<0.001). The data on death shown in this table, as well as data on all the other variables listed in the table, were assessed in the population that resulted from propensity-score matching (39,966 patients in each cohort). NA denotes not applicable.
Data are given as number who were discharged home among total number of survivors of the initial operation (percent), as opposed to being discharged to a rehabilitation center, nursing home, or secondary acute care hospital.
LONG-TERM SURVIVAL
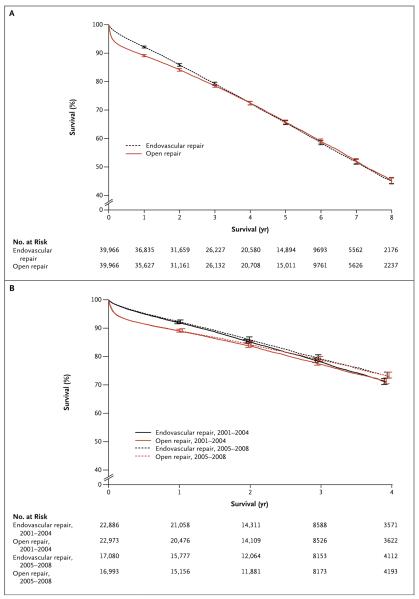
The probability of long-term survival in the two cohorts is shown in Figure 1A. The early survival benefit after endovascular repair persisted for approximately 3 years, after which time the estimated survival curves were similar. The probability of long-term survival decreased as age increased, and the early advantage of endovascular repair was larger with increasing age (Fig. S1 in the Supplementary Appendix). In a comparison of the results of repairs performed from 2005 through 2008 with those performed from 2001 through 2004, the overall survival rates were higher in the later period, but the findings were otherwise similar (Fig. 1B).
Figure 1. Survival after Endovascular Repair or Open Repair of Abdominal Aortic Aneurysm.
Shown are rates of survival among all patients who underwent endovascular repair or open repair of abdominal aortic aneurysms (Panel A) and among patients who underwent the procedure during the period from 2001 through 2004 and during the period from 2005 through 2008 (Panel B). I bars indicate 99% confidence intervals.
The early divergence and later convergence of the survival curves suggest that the hazards of death were not proportional. Endovascular repair was markedly superior to open repair for the first 30 days (hazard ratio for death after endovascular repair, 0.32; 95% CI, 0.29 to 0.35; P<0.001) and continued to be superior for the next 60 days (hazard ratio, 0.64; 95% CI, 0.58 to 0.71; P<0.001), after which time endovascular repair was associated with a slightly higher instantaneous risk (hazard) until year 4 (hazard ratio, 1.17; 95% CI, 1.13 to 1.21; P<0.001). After year 4, the hazard was significantly greater (at the 0.05 level) with endovascular repair (hazard ratio for death after endovascular repair, 1.05; 95% CI, 1.00 to 1.09; P = 0.03), but the difference was not meaningful in practical or clinical terms.
Because early survival confers an advantage in terms of the total amount of time patients are expected to survive, the restricted mean survival analyses showed that at 4 years, survival among patients in the endovascular-repair cohort was an average of 12.4 days longer (95% CI, 9.0 to 15.6) than survival among those in the open-repair cohort (P<0.001), and the difference remained significant through 7 years of follow-up (an average of 8.2 days longer among those in the endovascular-repair cohort than among those in the open-repair cohort; 95% CI, 1.5 to 14.4; P = 0.02) (Fig. S2 in the Supplementary Appendix). These analyses suggest that there is a substantial initial benefit of endovascular repair that endures for a considerable period, despite the fact that patients who undergo open repair and survive through 90 days of follow-up have a slightly lower risk of death over the next several years.
OTHER LONG-TERM OUTCOMES
We studied the risk of a variety of secondary outcomes after censoring the data for patients who died. Aneurysm rupture occurred in 5.4% of the patients in the endovascular-repair cohort versus 1.4% of patients in the open-repair cohort through 8 years of follow-up (P<0.001) (Table 3). After 8 years, aneurysm-related interventions were more common among patients who had undergone endovascular repair than among those who had undergone open repair (18.8% vs. 3.7%, P<0.001); these reinterventions included major reinterventions, which occurred in 2.3% versus 0.8% of patients (P<0.001), and minor reinterventions in 17.5% versus 3.1% (P<0.001). Reinterventions for complications related to laparotomy were more common among those who had undergone open repair than among those who had undergone endovascular repair (17.7% vs. 8.2%, P<0.001); the majority of these reinterventions were repairs of hernias of the abdominal wall. Through 8 years of follow-up, admission for bowel obstruction without surgery was also more common in the open-repair cohort (22.2% vs. 17.3%, P<0.001).
Table 3.
Eight-Year Outcomes after Endovascular and Open Repair of Abdominal Aortic Aneurysm.
| Outcome | Endovascular Repair (N = 39,966) |
Open Repair (N = 39,966) |
P Value |
|---|---|---|---|
| no. of patients (%) * | |||
| Death | 14,548 (54.9) | 14,681 (54.7) | 0.76 |
| Rupture of aneurysm | 962 (5.4) | 353 (1.4) | <0.001 |
| Any aneurysm-related intervention | 4,165 (18.8) | 754 (3.7) | <0.001 |
| Major reintervention | 392 (2.3) | 186 (0.8) | <0.001 |
| Minor reintervention | 3,924 (17.5) | 597 (3.1) | <0.001 |
| Minor reintervention for embolization | 1,857 (8.0) | 161 (1.0) | <0.001 |
| Hospitalization for abdominal aortic aneurysm without reintervention |
233 (1.2) | 55 (0.3) | <0.001 |
| Reintervention for complications related to laparotomy | 1,695 (8.2) | 4,427 (17.7) | <0.001 |
| Repair of a hernia of the abdominal wall | 610 (2.7) | 3,070 (11.2) | <0.001 |
| Lysis of adhesions without bowel resection | 238 (1.4) | 654 (3.1) | <0.001 |
| Bowel resection | 1,035 (5.2) | 1,199 (6.0) | 0.008 |
| Admission for bowel obstruction without surgery | 3,510 (17.3) | 4,805 (22.2) | <0.001 |
| Aneurysm-related intervention or intervention for compli cations related to laparotomy |
5,614 (25.1) | 5,034 (20.6) | <0.001 |
| Hospitalization related to aneurysm or for complications related to laparotomy, without intervention |
3,710 (17.9) | 4,846 (22.0) | <0.001 |
| Reintervention or hospitalization without intervention for rupture, aneurysm, or complications related to laparotomy |
6,279 (27.8) | 5,355 (21.8) | <0.001 |
Percentages are 8-year Kaplan–Meier estimates.
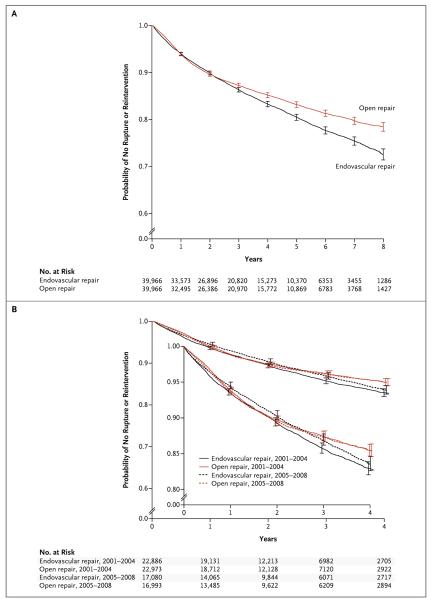
The overall combined rate of aneurysm-related interventions and interventions for complications related to laparotomy was 25.1% in the endovascular-repair cohort versus 20.6% in the open-repair cohort (P<0.001). As seen in the curves for the rate of rupture or reintervention in Figure 2A, the risk of late events was greater in the endovascular-repair cohort than in the open-repair cohort. A comparison of event rates at 1, 2, 5, and 8 years is shown in Table S4 in the Supplementary Appendix, and a comparison of event rates among matched and unmatched patients in the endovascular-repair cohort is shown in Table S5 in the Supplementary Appendix.
Figure 2. Freedom from Rupture, Aneurysm, or Reintervention for Complications Related to Laparotomy.
Data are shown for all patients who underwent endovascular repair or open repair of abdominal aortic aneurysms (Panel A) and for patients who underwent the procedure during the period from 2001 through 2004 and during the period from 2005 through 2008 (Panel B). The inset in Panel B shows the same data on an enlarged y axis. I bars indicate 99% confidence intervals.
TRENDS IN PERIOPERATIVE AND 2-YEAR OUTCOMES
Over the 8 years of follow-up, perioperative mortality with endovascular repair decreased by 0.8 percentage points, from 2.2% to 1.4% (P = 0.001), and perioperative mortality with open repair decreased by 0.6 percentage points, from 5.7% to 5.1% (P = 0.01) (Table S6 in the Supplementary Appendix). The rate of conversion from endovascular to open repair decreased significantly from 2.2% to 0.3% (P<0.001). The rate of reoperation for bleeding decreased in the endovascular-repair cohort from 0.8% to 0.2% (P<0.001), and the rate of readmission within 30 days after discharge decreased in the endovascular-repair cohort from 10.8% to 9.4% (P<0.001); however, the rate of readmission after open repair increased nonsignificantly from 9.6% to 10.5% (P = 0.24).
Mortality at 2 years after endovascular repair decreased from 16.3% among patients who underwent procedures in 2001 to 14.6% among patients who underwent procedures in 2007 (P<0.001), but mortality at 2 years after open repair did not change significantly during that period (16.8% among patients who underwent procedures in 2001 and 15.4% among patients who underwent procedures in 2007; P = 0.24) (Table S6 in the Supplementary Appendix). The rate of total reinterventions at 2 years after endovascular repair decreased over time (10.4% among patients who underwent procedures in 2001 to 9.1% among patients who underwent procedures in 2007; P<0.001), a decrease that was driven by a decrease in minor reinterventions, primarily coil embolization. Rates of either rupture or reintervention during the period from 2001 through 2004 and during the period from 2005 through 2008 are shown in Figure 2B; the difference between the two cohorts in the long-term risk of either rupture or reintervention was smaller in the later period than in the earlier period.
DISCUSSION
In this large U.S. study of two approaches to the repair of abdominal aortic aneurysm, we found that the early survival benefit with endovascular repair as compared with open repair persisted for almost 3 years, after which time the survival was similar in the two groups. The overall rate of late complications, including aneurysm-related interventions, procedures for complications related to laparotomy, and admissions for bowel obstruction, was slightly lower after open repair than after endovascular repair, but the rates of adverse outcomes after endovascular repair, including perioperative mortality and rates of reintervention, decreased over time. Nonetheless, late rupture after endovascular repair occurred in 5.4% of patients through 8 years of follow-up.
Previous randomized trials showed that the early advantage with endovascular repair was lost after 1 to 2 years (the DREAM6 and EVAR-19 trials) or after 3 years (the OVER trial7). The OVER trial also showed improved survival after endovascular repair among patients younger than 70 years of age but not among those 70 years of age or older. In contrast, in our substantially larger population, which was not restricted to patients who would qualify for a clinical trial, we found an early survival advantage with endovascular repair among patients of all ages. This advantage increased with increasing age and lasted for approximately 3 years. When measured in terms of expected duration of survival or “area under the curve,” the survival advantage of endovascular repair is estimated to persist through 7 years.
Over the course of 8 years of follow-up, we found higher rates of aneurysm-related interventions after endovascular repair and offsetting higher rates of reinterventions for complications related to laparotomy after open repair. The overall rate of reintervention was higher in the endovascular-repair cohort than in the open-repair cohort. The EVAR-19 and DREAM6 trials showed higher rates of reintervention after endovascular repair, but the EVAR-1 trial did not account for reinterventions for complications related to laparotomy, and the DREAM trial included only hernia repairs. The recent report of long-term results from the OVER trial included hernia repair and readmission and reintervention for bowel obstruction and showed that the overall rates of reinterventions over time were similar in the endovascular-repair and open-repair groups.7 Our analysis suggests that the OVER trial may have been underpowered to detect a small difference in total reinterventions; our findings suggest that there is, indeed, a small difference, but that it may not be clinically significant.
The rate of late aneurysm rupture was significantly higher among the survivors in the endovascular-repair cohort than among the survivors in the open-repair cohort (5.4% vs. 1.4%) through 8 years of follow-up. Randomized trials and other studies have suggested that rates of late rupture after endovascular repair may continue to increase with longer follow-up.6,7,9,11 We confirmed this finding and believe that more data are needed on the risk of late rupture after repair of abdominal aortic aneurysm, because abdominal aortic aneurysms are repaired to prevent precisely that occurrence.20
We found reductions over time in perioperative mortality and the rate of conversion from endovascular to open repair, as well as in 2-year mortality and the rate of reinterventions after endovascular repair. The decline in reinterventions seemed to be driven by a decrease in the number of minor reinterventions, primarily coil embolization, which probably represents a more conservative attitude toward the management of type 2 (side branch) endoleak. The decline in perioperative mortality probably represents operators’ increased familiarity with the procedure and improvements in endografts over time. It is unlikely, however, that this reduction in perioperative mortality is driven by improved patient selection, because most patients are now being treated with the use of endovascular repair, and mortality after open repair was reduced over this period as well.
Our analyses, which were performed with the use of Medicare data, are subject to several limitations, including the fact that the data are observational, are subject to potential coding error, and lack anatomical details (e.g., aneurysm diameter, calcification, iliac involvement, and infrarenal neck anatomy) and some clinical details (e.g., regarding smoking status and status with respect to anemia, infections, and medications) that may be important determinants of patient selection and outcomes. Although our list of confounders was extensive, propensity analyses cannot account for selection bias related to unmeasured characteristics.
In conclusion, our analysis confirmed the findings of previous studies that have shown that perioperative mortality and rates of complications are lower with endovascular repair than with open repair of abdominal aortic aneurysms. Long-term mortality was similar in the two repair cohorts. The rates of reinterventions related to abdominal aortic aneurysm were higher in the endovascular-repair cohort, and these were partially balanced by a higher rate of reinterventions for complications related to laparotomy in the open-repair cohort. Perioperative mortality and the rate of conversion from endovascular to open repair, as well as 2-year mortality and rates of reinterventions, were reduced over time with endovascular repair, but late rupture after endovascular repair is a concern and warrants further study.
Supplementary Material
Acknowledgments
Supported by a grant (5R01HL105453-03) from the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH), by a NIH T32 Harvard–Longwood Research Training in Vascular Surgery grant (HL007734), and by a grant (1RC4MH092717-01) from the National Institute of Mental Health of the NIH.
We thank Lawrence Zaborski, M.S., from the Department of Health Care Policy, Harvard Medical School, Boston, for performing data analysis.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Schermerhorn ML, Bensley RP, Giles KA, et al. Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Ann Surg. 2012;256:651–8. doi: 10.1097/SLA.0b013e31826b4f91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dua A, Kuy S, Lee CJ, Upchurch GR, Jr, Desai SS. Epidemiology of aortic aneurysm repair in the United States from 2000 to 2010. J Vasc Surg. 2014;59:1512–7. doi: 10.1016/j.jvs.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Prinssen M, Verhoeven EL, Buth J, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351:1607–18. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 4.EVAR Trial Participants Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet. 2005;365:2179–86. doi: 10.1016/S0140-6736(05)66627-5. [DOI] [PubMed] [Google Scholar]
- 5.Lederle FA, Freischlag JA, Kyriakides TC, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302:1535–42. doi: 10.1001/jama.2009.1426. [DOI] [PubMed] [Google Scholar]
- 6.De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1881–9. doi: 10.1056/NEJMoa0909499. [DOI] [PubMed] [Google Scholar]
- 7.Lederle FA, Freischlag JA, Kyriakides TC, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med. 2012;367:1988–97. doi: 10.1056/NEJMoa1207481. [DOI] [PubMed] [Google Scholar]
- 8.Jackson RS, Chang DC, Freischlag JA. Comparison of long-term survival after open vs endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. JAMA. 2012;307:1621–8. doi: 10.1001/jama.2012.453. [DOI] [PubMed] [Google Scholar]
- 9.The United Kingdom EVAR Trial Investigators Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1863–71. doi: 10.1056/NEJMoa0909305. [DOI] [PubMed] [Google Scholar]
- 10.Buck DB, Darling J, Cronenwett JL, et al. Substantial variation exists between SVS VQI regions in patient selection and treatment of abdominal aortic aneurysms. J Vasc Surg. 2014;60:830. doi: 10.1016/j.jvs.2016.02.036. abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464–74. doi: 10.1056/NEJMoa0707348. [DOI] [PubMed] [Google Scholar]
- 12.Zhang JX, Iwashyna TJ, Christakis NA. The performance of different lookback periods and sources of information for Charlson comorbidity adjustment in Medicare claims. Med Care. 1999;37:1128–39. doi: 10.1097/00005650-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Bensley RP, Schermerhorn ML, Hurks R, et al. Risk of late-onset adhesions and incisional hernia repairs after surgery. J Am Coll Surg. 2013;216(6):1159.e12–1167.e12. doi: 10.1016/j.jamcollsurg.2013.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Baldwin LM, Klabunde CN, Green P, Barlow W, Wright G. In search of the perfect comorbidity measure for use with administrative claims data: does it exist? Med Care. 2006;44:745–53. doi: 10.1097/01.mlr.0000223475.70440.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gu XS, Rosenbaum PR. Comparison of multivariate matching methods: structures, distances, and algorithms. J Comput Graph Statist. 1993;2:405–20. [Google Scholar]
- 17.Cochran WG, Rubin DB. Controlling bias in observational studies: a review. Sankya Ser A. 1973;35:417–46. [Google Scholar]
- 18.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. Springer; New York: 2000. [Google Scholar]
- 19.Andersen PK, Hansen MG, Klein JP. Regression analysis of restricted mean survival time based on pseudo-observations. Lifetime Data Anal. 2004;10:335–50. doi: 10.1007/s10985-004-4771-0. [DOI] [PubMed] [Google Scholar]
- 20.Schermerhorn ML, Giles KA, Sachs T, et al. Defining perioperative mortality after open and endovascular aortic aneurysm repair in the US Medicare population. J Am Coll Surg. 2011;212:349–55. doi: 10.1016/j.jamcollsurg.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.