Abstract
Study objective
We determine the proportion of successful intubations with the C-MAC video laryngoscope (C-MAC) compared with the direct laryngoscope in emergency department (ED) intubations.
Methods
This was a retrospective analysis of prospectively collected data entered into a continuous quality improvement database during a 28-month period in an academic ED. After each intubation, the operator completed a standardized data form evaluating multiple aspects of the intubation, including patient demographics, indication for intubation, device(s) used, reason for device selection, difficult airway characteristics, number of attempts, and outcome of each attempt. Intubation was considered ultimately successful if the endotracheal tube was correctly inserted into the trachea with the initial device. An attempt was defined as insertion of the device into the mouth regardless of whether there was an attempt to pass the tube. The primary outcome measure was ultimate success. Secondary outcome measures were first-attempt success, Cormack-Lehane view, and esophageal intubation. Multivariate logistic regression analyses, with the inclusion of a propensity score, were performed for the outcome variables ultimate success and first-attempt success.
Results
During the 28-month study period, 750 intubations were performed with either the C-MAC with a size 3 or 4 blade or a direct laryngoscope with a Macintosh size 3 or 4 blade. Of these, 255 were performed with the C-MAC as the initial device and 495 with a Macintosh direct laryngoscope as the initial device. The C-MAC resulted in successful intubation in 248 of 255 cases (97.3%; 95% confidence interval [CI] 94.4% to 98.9%). A direct laryngoscope resulted in successful intubation in 418 of 495 cases (84.4%; 95% CI 81.0% to 87.5%). In the multivariate regression model, with a propensity score included, the C-MAC was positively predictive of ultimate success (odds ratio 12.7; 95% CI 4.1 to 38.8) and first-attempt success (odds ratio 2.2; 95% CI 1.2 to 3.8). When the C-MAC was used as a video laryngoscope, a Cormack-Lehane grade I or II view (video) was obtained in 117 of 125 cases (93.6%; 95% CI 87.8% to 97.2%), whereas when a direct laryngoscope was used, a grade I or II view was obtained in 410 of 495 cases (82.8%; 95% CI 79.2% to 86.1%). The C-MAC was associated with immediately recognized esophageal intubation in 4 of 255 cases (1.6%; 95% CI 0.4% to 4.0%), whereas a direct laryngoscope was associated with immediately recognized esophageal intubation in 24 of 495 cases (4.8%; 95% CI 3.1% to 7.1%).
Conclusion
When used for emergency intubations in the ED, the C-MAC was associated with a greater proportion of successful intubations and a greater proportion of Cormack-Lehane grade I or II views compared with a direct laryngoscope.
Introduction
Background
Direct laryngoscopy is the primary method for performing intubation in the emergency department (ED).1-4 The direct laryngoscope blade is used to compress and displace the tongue, with the goal of allowing operators to obtain a direct line of sight from their eye to the laryngeal inlet. Many anatomic or pathologic factors can make direct visualization of the airway difficult and sometimes even impossible. For example, anything that increases the size of the tongue and soft tissues of the upper airway can make visualizing the laryngeal inlet with direct laryngoscopy more challenging. Likewise, the presence of cervical immobilization, as is common with most patients with blunt trauma, prevents movement of the cervical spine and makes alignment of the airway axes extremely difficult.5
In the last decade, multiple video laryngoscopes have been introduced into clinical practice and have become more common in ED intubations.6-8 One recent study revealed that 43% of EDs affiliated with an emergency medicine residency have a video laryngoscope available.8 Video laryngoscopes incorporate a micro video camera on the undersurface of the laryngoscope blade and thus bring a view of the airway out of the patient and onto a video monitor. This provides the operator with an indirect view of the airway and thus circumvents the problems associated with achieving a direct line of sight to the airway.
The C-MAC video laryngoscope (C-MAC) (Karl Storz, Tuttlingen, Germany) is a recently introduced video laryngoscope that is conceptually and structurally different from other video laryngoscopes. Rather than using blades with acute angles, the C-MAC incorporates a conventional Macintosh-type blade, with the addition of a micro video camera on the distal portion of the blade.9 Because it incorporates a standard Macintosh-type blade, the C-MAC has the advantage of being able to be used as a direct laryngoscope, as well as a video laryngoscope. This could be useful if the video view becomes obscured by gross contamination of the camera lens during video laryngoscopy. Additionally, this allows supervising physicians to monitor direct laryngoscopy when trainees are using the C-MAC. Preliminary studies of the C-MAC in the operating room and out-of-hospital setting have demonstrated promising results.10,11 However, patients in the ED frequently are more difficult to intubate because of pathologic conditions and reduced physiologic reserves. To our knowledge, there are no published articles reporting the efficacy of the C-MAC for ED intubations.
Importance
Airway management is a crucial, lifesaving procedure performed daily in the ED. Failure to quickly establish an airway can result in hypoxemia, aspiration, neurologic damage, cardiovascular complications, and death.12 Despite its limitations, direct laryngoscopy has been the primary technique to perform intubation in the ED. In recent years, several video laryngoscopes have been introduced into clinical practice, with the goal of improving airway management. It is important to evaluate these new devices as they emerge to determine their efficacy in the high-risk patients intubated in the ED.
Goals of This Investigation
The goal of this investigation was to compare the clinical performance of the C-MAC video laryngoscope to the Macintosh direct laryngoscope in patients intubated in the ED. The primary outcome measure was successful intubation. Secondary outcome measures were successful intubation on the first attempt, the Cormack-Lehane view, and immediately recognized esophageal intubations.
Materials and Methods
Study Design
This is a retrospective analysis of 1,117 ED intubations prospectively recorded in a continuous quality improvement database from February 2009 to June 2011. This project was granted exemption by the University of Arizona institutional review board.
Setting
This study was conducted at the University of Arizona Medical Center in Tucson, AZ. The hospital has a 61-bed tertiary care academic ED with an annual census of approximately 70,000 visits. The ED, also a Level I trauma center, has an Accreditation Council for Graduate Medical Education accredited 3-year emergency medicine residency program, as well as a 5-year combined pediatric/emergency medicine residency program.
Selection of Participants
The C-MAC was introduced in our ED on February 1, 2009. Only patients who were intubated with the C-MAC or the Macintosh direct laryngoscope as the initial device from February 1, 2009, until June 30, 2011, were included in this study. For most of the study period, the C-MAC was available only in Macintosh-type blade sizes 3 or 4. To allow a fair comparison of devices in this study, only intubations performed with either the C-MAC (size 3 or 4 blade) or a direct laryngoscope Macintosh (size 3 or 4 blade) were included in this analysis. Intubations with the Miller blade, Macintosh size 1 or 2 blade, Grandview blade, or the recently introduced C-MAC size 2 and C-MAC D-blade were excluded from this study.
The majority of intubations are performed by emergency medicine residents. All ED intubations are supervised by an emergency medicine attending physician. Residents in this program participate in a 1-month rotation on the anesthesiology service, where they learn and practice airway management techniques. On this rotation, residents average approximately 30 intubations, with virtually all (>95%) performed with direct laryngoscopy. A simulation laboratory is also available to all residents to practice using a variety of airway devices. During the course of residency, emergency medicine residents perform an average of 30 intubations in the ED, half of which are with a direct laryngoscope and half of which are with a video laryngoscope. Before starting their emergency medicine residency, no resident had experience with the C-MAC. On rare occasions, rotating residents from other specialties, medical students, or paramedics are permitted to intubate at the discretion of the emergency medicine attending physician. One morning per week, while the residents are attending academic conferences, the ED is staffed only by emergency medicine attending physicians, who perform the intubations.
Methods of Measurement
After each intubation, the operator completed a data collection form, which included the following information: patient demographics, operator specialty, operator postgraduate year, indication for intubation, method of intubation, paralytic agent, sedative agent, device(s) used, reason for device selection, presence of certain difficult airway characteristics, the Cormack-Lehane view of the airway, number of attempts at intubation, and the outcome of each attempt.
The categorical 3-year emergency medicine residents indicated their experience level as an emergency medicine resident 1, 2, or 3. In terms of months spent in the ED, our combined pediatric/emergency medicine residents equate to an emergency medicine resident 1 during postgraduate years 1 and 2, emergency medicine resident 2 during postgraduate years 3 and 4, and emergency medicine resident 3 during postgraduate year 5.
Methods of intubation included rapid sequence intubation in which a paralytic agent was used, oral intubation in which a sedative agent was used, and oral intubation in which no medications were used.
The operator had 3 options to choose from for the reason for device selection. If the intubation was a routine airway with no prediction of difficulty, then the device selection was marked “standard.” If the device was selected with the expectation of a difficult airway, the reason for device selection was “difficult.” If the operator was using the device to gain educational experience with the device, then it was classified as “education.”
Standard preoperative difficult airway predictors such as the Mallampati score, thyromental distance, and neck mobility have been shown to be challenging to apply in the emergency setting because of lack of patient cooperation and the urgency to complete the intubation rapidly.13,14 Thus, we developed a list of difficult airway characteristics that were feasible for the operator to determine before intubation in an emergent setting by simple examination of the patient. These include the presence of cervical immobility (intrinsic or because of a cervical collar), obesity, large tongue, short neck, small mandible, facial or neck trauma, airway edema, blood in the airway, and vomit in the airway.
An attempt was defined as insertion of the laryngoscope blade into the oropharynx regardless of whether an attempt was made to pass the endotracheal tube. Each attempt was documented with one of 3 possible outcomes: successful intubation (no additional attempts required), inability to intubate (additional attempt[s] required), or inadvertent esophageal intubation (additional attempt[s] required). Successful intubation was defined as correct placement of the endotracheal tube in the trachea, as confirmed by end-tidal CO2 capnometry, pulse oximetry, chest auscultation, observation of chest excursion, absence of epigastric sounds, and misting of the endotracheal tube. If there was uncertainty about endotracheal tube placement by the operator and the tube was removed and replaced, the attempt was considered to have been an esophageal intubation. First-attempt success was defined as successful intubation, as defined above, on the initial attempt. Ultimate success was defined as successful intubation with the initial device, regardless of number of attempts required.
When the C-MAC was used as a video laryngoscope, lens contamination and degree of fogging were evaluated by the operator. Lens contamination was defined as gross contamination of the camera lens with liquid or particulate matter such as blood or vomit. Lens contamination was categorized as none, mild, moderate, or severe. Degree of fogging was defined as the degree of moisture condensation on the camera lens, causing clouding of the video view. Degree of fogging was documented on a 10-cm visual analog scale ranging from none (0) to complete fogging (10).
The data forms were reviewed by the senior author (J.C.S.). If the form had any missing data, it was returned to the operator for completion. If information on the form contained inconsistencies, the operator was interviewed by the senior author (J.C.S.) for clarification. The data forms were cross-referenced to professional billing and pharmacy records to identify any intubations performed without a corresponding data form. If an intubation was identified without a data form, the operator was given a data form to complete as soon as possible to ensure a maximal capture rate. Historically, approximately 90% of our continuous quality improvement forms are completed at intubation. The remaining 10% of forms are completed on a delayed basis.
The data were entered into the electronic database program HanDBase (version 4; DDH Software, Wellington, FL) for the Palm Pilot and iPad and then subsequently transferred to Microsoft Excel 2010 (Microsoft, Redmond, WA).
Outcome Measures
The primary outcome measure was successful intubation. Secondary outcome measures were successful intubation on the first attempt, Cormack-Lehane view, and immediately recognized esophageal intubation.
Primary Data Analysis
Summary statistics were generated for patient, intubation, and operator characteristics. Multivariate logistic regression analyses were performed for each of the outcome variables: ultimate intubation success and first-attempt intubation success. The predictor variable of interest was intubation device (C-MAC or direct laryngoscope). Other predictor variables added to each model to adjust for confounding included age, sex, trauma status, indication for intubation, method of intubation, paralytic agent, induction agent, presence of at least 1 difficult airway characteristic, operator specialty, emergency medicine resident level, and operator-specified reason for device selection. In addition, to account for the nonrandom selection of the intubation device, a propensity score was calculated for device selection, using all the predictor variables described above. The multivariate analyses were repeated with the propensity score included as a composite independent variable and intubation device as the predictor variable of interest.
Summary statistics were calculated with InStat (version 3.10; GraphPad Software, San Diego, CA). Ninety-five percent confidence intervals (CIs) for all counts and proportions were calculated with the “exact” method. Multivariate logistic regression and calculation of propensity scores were performed with Stata (version 12; StataCorp, College Station, TX).
Results
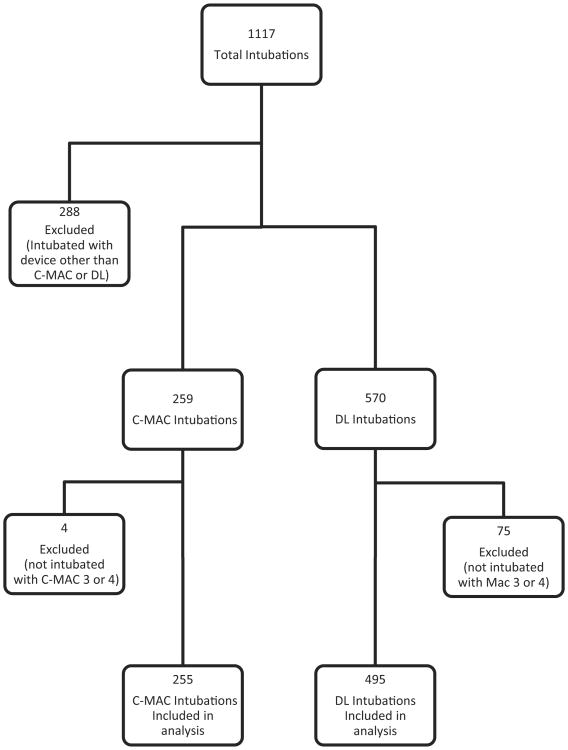
During the 28-month study period, a total of 750 patients were intubated with an initial device of either the C-MAC (Macintosh-type size 3 or 4) or a direct laryngoscope (Macintosh size 3 or 4). Of these, 255 patients were intubated with the C-MAC and 495 patients were intubated with a direct laryngoscope (Figure 1). The patient, intubation, and operator characteristics of the C-MAC group and the direct laryngoscope group were similar (Table 1). The mean age, proportion of male to female patients, and indication for intubation was similar between groups. However, 47.1% (95% CI 41.2% to 53.8%) of C-MAC intubations were trauma patients, whereas 37.8% (95% CI 33.5% to 42.2%) of direct laryngoscope intubations were trauma patients. In addition, 64.7% (95% CI 58.5% to 70.6%) of patients intubated with the C-MAC had at least 1 difficult airway characteristic, whereas 56.8% (95% CI 52.3% to 61.2%) of patients intubated with a direct laryngoscope had at least 1 difficult airway characteristic. In 36.9% (95% CI 30.9% to 43.1%) of C-MAC cases, the C-MAC was selected because the airway was expected to be difficult, whereas in 1.2% (95% CI 1.1% to 3.9%) of direct laryngoscope cases, a direct laryngoscope was selected because the airway was expected to be difficult.
Figure 1.
Patients included in the analysis. DL, Direct laryngoscope.
Table 1.
Patient, intubation and operator characteristics.
| Characteristic | C-MAC, % (n=255) | 95% CI* | DL, % (n=495) | 95% CI* |
|---|---|---|---|---|
| Mean age, y | 46.4 (range (14–94) | 43.9–48.9 | 48.9 (range (3–95) | 47.0–50.8 |
| Sex | ||||
| Male | 63.9 (163) | 57.7–69.8 | 66.9 (331) | 62.5–71.0 |
| Medical/trauma | ||||
| Trauma patients | 47.1 (121) | 41.2–53.8 | 37.8 (187) | 33.5–42.2 |
| DACs | ||||
| None | 35.3 (90) | 29.4–41.2 | 43.2 (214) | 38.9–47.6 |
| ≥1 | 64.7 (165) | 58.5–70.6 | 56.8 (281) | 52.3–61.2 |
| C-collar | 32.6 (83) | 26.8–38.7 | 25.0 (124) | 21.3–29.1 |
| Blood in airway | 23.9 (61) | 18.8–29.6 | 21.6 (107) | 18.1–25.5 |
| Vomit in airway | 18.4 (47) | 13.9–23.7 | 14.3 (71) | 11.4–17.8 |
| Facial trauma | 16.9 (43) | 12.5–22.0 | 9.9 (49) | 7.4–12.9 |
| Obesity | 12.5 (32) | 8.7–17.3 | 14.7 (73) | 11.7–18.2 |
| Short neck | 11.0 (28) | 7.4–15.5 | 10.1 (50) | 7.6–13.1 |
| Large tongue | 8.2 (21) | 5.2–12.3 | 8.9 (44) | 6.5–11.8 |
| Airway edema | 2.7 (7) | 1.1–5.6 | 2.6 (13) | 1.4–4.5 |
| Small mandible | 2.0 (5) | 0.6–4.5 | 3.6 (18) | 2.2–5.7 |
| Reason for intubation | ||||
| Airway protection | 56.1 (143) | 49.8–62.3 | 60.8 (301) | 56.4–65.1 |
| Respiratory failure | 17.7 (45) | 13.2–22.9 | 18.6 (92) | 15.3–22.3 |
| Cardiac arrest | 15.3 (39) | 11.1–20.3 | 10.7 (53) | 8.1–13.8 |
| Patient control | 9.4 (24) | 6.1–13.7 | 8.9 (44) | 6.5–11.8 |
| Hypoxia | 1.6 (4) | 0.3–4.9 | 1.0 (5) | 0.2–2.8 |
| Reason for device Selection | ||||
| Standard | 26.7 (68) | 21.3–32.5 | 96.2 (476) | 94.1–97.7 |
| Difficult | 36.9 (94) | 30.9–43.1 | 2.2 (11) | 1.1–3.9 |
| Education | 36.5 (93) | 30.6–42.7 | 1.6 (8) | 0.7–3.2 |
| Method of intubation | ||||
| Rapid sequence intubation | 81.2 (207) | 75.8–85.8 | 86.3 (427) | 82.9–89.2 |
| Oral intubation (sedation only) | 3.9 (10) | 1.9–7.1 | 1.2 (6) | 0.5–2.6 |
| Oral intubation (no medications used) | 14.9 (38) | 10.8–19.9 | 12.5 (62) | 9.7–15.8 |
| Operator specialty | ||||
| Emergency medicine | 96.1 (245) | 92.9–98.1 | 96.6 (478) | 94.6–98.0 |
| Nonemergency medicine | 3.9 (10) | 1.9–7.1 | 3.4 (17) | 2.0–5.4 |
| EMR level | ||||
| 1 | 27.4 (67) | 21.9–33.4 | 21.3 (102) | 17.8–25.3 |
| 2 | 37.1 (91) | 31.1–43.5 | 35.4 (169) | 31.1–39.8 |
| 3 | 34.7 (85) | 28.8–41.0 | 41.4 (198) | 37.0–46.0 |
| Attending | 0.8 (2) | 0.04–3.7 | 1.9 (9) | 0.9–3.5 |
DL, Direct laryngoscope; DAC, difficult airway characteristic; EMR, emergency medicine resident.
Ninety-five percent CIs calculated with the “exact” method.
The C-MAC was ultimately successful in 248 of 255 patients (97.3%; 95% CI 94.4% to 98.9%), whereas a direct laryngoscope was ultimately successful in 418 of 495 patients (84.4%; 95% CI 81.0% to 87.5%). C-MAC intubations were successful on the first attempt in 202 of 255 patients (79.2%; 95% CI 73.7% to 84.0%), and direct laryngoscope intubations were successful on the first attempt in 362 of 495 patients (73.1%; 95% CI 69.0% to 77.0%).
Of the 248 successful C-MAC intubations, 202 were accomplished in 1 attempt (81.5%; 95% CI 76.1% to 86.1%), 39 in 2 attempts (15.7%; 95% CI 11.4% to 20.9%), and 7 in 3 or more attempts (2.8%; 95% CI 1.1% to 5.7%). Of the 418 successful direct laryngoscope intubations, 362 patients were intubated in 1 attempt (86.6%; 95% CI 83.0% to 89.7%), 40 in 2 attempts (9.6%; 95% CI 6.9% to 12.8%), and 16 in 3 or more attempts (3.8%; 95% CI 2.2% to 6.1%).
In the multivariate regression model, with the inclusion of the propensity score, the C-MAC was predictive of ultimate success (odds ratio [OR] 12.7; 95% CI 4.1 to 38.8) and first-attempt success (OR 2.2; 95% CI 1.2 to 3.8). No other variables were found to be positive predictors of success. The following variables were found to have a negative predictive value for ultimate success: presence of at least 1 difficult airway characteristic (OR 0.53; 95% CI 0.3 to 0.9), male sex (OR 0.5; 95% CI 0.3 to 0.9), and reason for device selection being suspected difficult airway (OR 0.3; 95% CI 0.1 to 0.8) (Table 2).
Table 2.
Logistic regression model for successful intubation.
| Ultimate Success | First-Attempt Success | |||
|---|---|---|---|---|
|
|
|
|||
| Variable | OR | 95% CI | OR | 95% CI |
| Age | 1.0 | 0.97–1.0 | 1.0 | 0.98–1.0 |
| ≥1 DAC* | 0.5 | 0.3–0.9 | 0.4 | 0.3–0.7 |
| Male† | 0.5 | 0.3–0.9 | 0.7 | 0.5–1.0 |
| Trauma‡ | 1.6 | 0.9–2.9 | 1.2 | 0.8–1.8 |
| Specialty=EM§ | 5.3 | 0.8–34.2 | 8.0 | 1.7–38.3 |
| Operator EMR | ||||
| 0 | [Reference] | [Reference] | ||
| 1 | 0.2 | 0.02–2.0 | 0.2 | 0.04–1.5 |
| 2 | 0.1 | 0.01–1.7 | 0.4 | 0.06–2.5 |
| 3 or attending | 0.2 | 0.02–2.7 | 0.4 | 0.06–2.8 |
| Paralytic used | ||||
| Succinylcholine | [Reference] | [Reference] | ||
| Rocuronium | 0.6 | 0.4–1.1 | 0.8 | 0.5–1.2 |
| None | 0.5 | 0.1–2.8 | 0.6 | 0.2–1.7 |
| Sedative used | ||||
| Etomidate | [Reference] | [Reference] | ||
| Other | 1.5 | 0.4–5.0 | 1.3 | 0.6–2.6 |
| None | 1.3 | 0.2–7.0 | 2.4 | 0.7–8.1 |
| Indication for intubation | ||||
| Airway control | [Reference] | [Reference] | ||
| Cardiac arrest | 0.9 | 0.3–2.8 | 0.4 | 0.2–0.8 |
| Patient control | 1.0 | 0.4–2.8 | 1.4 | 0.7–3.0 |
| Hypoxia‖ | 1.0 | NA* | 1.0 | NA* |
| Respiratory failure | 1.6 | 0.8–3.3 | 1.09 | 0.7–1.8 |
| Reason for device | ||||
| Standard | [Reference] | [Reference] | ||
| Difficult | 0.3 | 0.1–0.8 | 0.3 | 0.1–0.5 |
| Education | 0.4 | 0.1–1.7 | 0.6 | 0.3–1.2 |
| Device used | ||||
| Device=CMAC¶ | 17.6 | 5.3–58.2 | 3.4 | 1.8–6.7 |
| Device=C-MAC¶ (propensity score regression) | 12.7 | 4.1–38.8 | 2.2 | 1.2–3.8 |
Reference=0 DACs.
Reference=female.
Reference=medical.
Reference=nonemergency medicine specialty.
When entered into the regression model, hypoxia as an indication for intubation perfectly predicted success.
Reference = DL
When the C-MAC was used for patients with no difficult airway characteristics, it was ultimately successful in 89 of 90 intubations (98.9%; 95% CI 94.0% to 100.0%). When a direct laryngoscope was used for patients with no difficult airway characteristics, it was ultimately successful in 189 of 214 intubations (88.3%; 95% CI 83.2% to 92.3%). When the C-MAC was used for patients with 1 or more difficult airway characteristics, it was ultimately successful in 159 of 165 intubations (96.4%; 95% CI 92.3% to 98.7%). When a direct laryngoscope was used for patients with 1 or more difficult airway characteristics, it was ultimately successful in 229 of 281 intubations (81.5%; 95% CI 76.5% to 85.9%). See Tables 3 and 4 for a breakdown by number of difficult airway characteristics and specific difficult airway characteristics. For patients with restricted cervical mobility, the C-MAC was ultimately successful in 82 of 83 cases (98.8%; 95% CI 93.5% to 100.0%), whereas a direct laryngoscope was ultimately successful in 103 of 124 cases (83.1%; 95% CI 75.3% to 89.2%).
Table 3.
Proportion of successful intubations with increasing difficult airway characteristics.
| DACs, No. | C-MAC, % (n=255) | 95% CI* | DL, % (n=495) | 95% CI* |
|---|---|---|---|---|
| 0 | 98.9 (89/90) | 94.0–100 | 88.3 (189/214) | 83.2–92.3 |
| 1 | 98.5 (73/74) | 92.7–100 | 84.7 (122/144) | 77.8–90.2 |
| 2 | 95.5 (42/44) | 84.5–99.4 | 82.1 (46/56) | 69.6–91.1 |
| ≥3 | 93.6 (44/47) | 82.5–98.7 | 75.3 (61/81) | 64.5–84.2 |
95% CIs calculated with the “exact” method.
Table 4.
Proportion of successful intubations with specific difficult airway characteristics.
| DAC | C-MAC, % (n=255) | 95% CI* | DL, % (n=495) | 95% CI* |
|---|---|---|---|---|
| Airway edema | 85.7 (6/7) | 42.1–99.6 | 46.2 (6/13) | 19.2–74.9 |
| Blood in airway | 93.4 (57/61) | 84.1–98.2 | 82.2 (88/107) | 73.7–89.0 |
| Cervical immobility | 98.8 (82/83) | 93.5–100 | 83.1 (103/124) | 75.3–89.2 |
| Facial/neck trauma | 95.3 (41/43) | 84.2–99.4 | 87.8 (43/49) | 75.2–95.4 |
| Large tongue | 90.5 (19/21) | 69.6–98.8 | 75.0 (33/44) | 59.7–86.8 |
| Obesity | 93.8 (30/32) | 79.2–99.2 | 78.1 (57/73) | 66.9–86.9 |
| Short neck | 92.9 (26/28) | 76.5–99.1 | 66.0 (33/50) | 51.2–78.8 |
| Small mandible | 100 (5/5) | 47.8–100 | 72.2 (13/18) | 46.5–90.3 |
| Vomit in airway | 93.6 (44/47) | 82.5–98.7 | 73.2 (52/71) | 61.4–83.1 |
Ninety-five percent CIs calculated with the “exact” method.
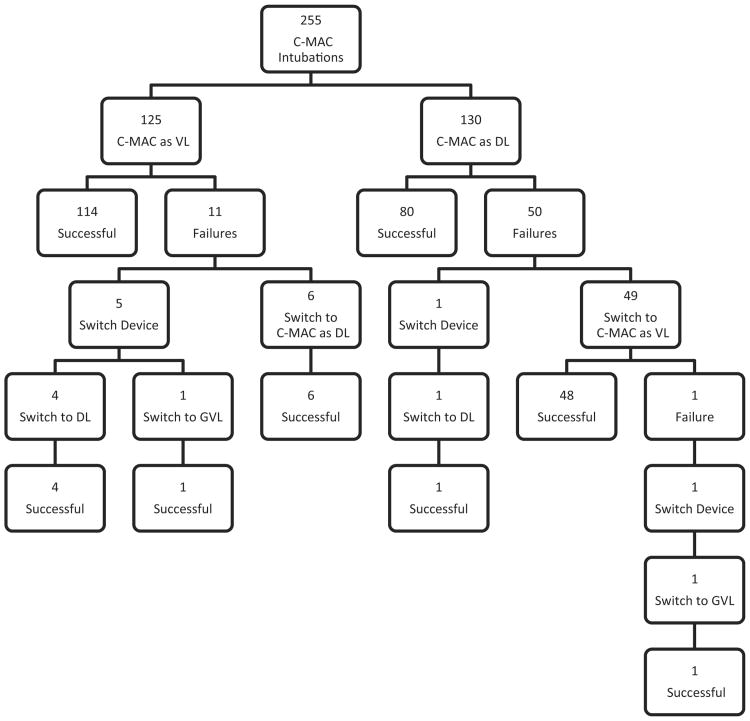
Of the 7 C-MAC failures, 5 patients were rescued with direct laryngoscope and 2 were rescued with the GlideScope video laryngoscope (Verathon Inc., Bothell, WA). One of the 7 C-MAC failures was due to equipment malfunction. Of the 77 direct laryngoscope failures, 60 patients were rescued with the GlideScope video laryngoscope, 15 were rescued with the C-MAC, 1 was rescued with an intubating–laryngeal mask airway, and 1 was rescued with a cricothyrotomy (Figure 2).
Figure 2.
C-MAC: DL vs video laryngoscope use. GVL, GlideScope video laryngoscope; VL, video laryngoscope.
Of the 255 C-MAC intubations, the C-MAC was used initially as a video laryngoscope for 125 patients and initially as a direct laryngoscope for 130 patients. When using the C-MAC as a video laryngoscope, operators obtained a Cormack-Lehane grade I or II view (video) in 117 of 125 cases (93.6%; 95% CI 87.8% to 97.2%). When using a direct laryngoscope, operators obtained a grade I or II view in 410 of 495 cases (82.8%; 95% CI 79.2% to 86.1%). See Table 5 for a complete breakdown of Cormack-Lehane views obtained.
Table 5.
Cormack-Lehane views.
| CL Grade | C-MAC, % (n=125)* | 95% CI† | DL, % (n=495) | 95% CI† |
|---|---|---|---|---|
| I | 79.2 (99) | 71.0–85.9 | 48.3 (239) | 43.8–52.8 |
| II | 14.4 (18) | 8.8–21.8 | 34.6 (171) | 30.4–38.9 |
| III | 4.8 (6) | 1.8–10.2 | 12.9 (64) | 10.1–16.2 |
| IV | 1.6 (2) | 0.2–5.7 | 4.2 (21) | 2.6–6.4 |
CL, Cormack-Lehane.
When C-MAC was used only as a video laryngoscope device.
95% CIs calculated using “exact” method.
The C-MAC resulted in immediately recognized esophageal intubation in 4 of 255 cases (1.6%; 95% CI 0.4% to 4.0%), whereas a direct laryngoscope resulted in immediately recognized esophageal intubation in 24 of 495 cases (4.8%; 95% CI 3.1% to 7.1%). Of the 4 esophageal intubations that occurred with the C-MAC, in all 4 cases, the operator continued with the C-MAC and successfully intubated the trachea on the subsequent attempt. Of the 24 esophageal intubations that occurred with a direct laryngoscope, 8 operators were ultimately successful staying with a direct laryngoscope, whereas 16 operators switched to a different device, primarily a video laryngoscope (13 GlideScope video laryngoscopes, 2 C-MACs, and 1 intubating–laryngeal mask airway).
The C-MAC was used initially as a direct laryngoscope in 130 of 255 cases (51.0%; 95% CI 44.7% to 57.3%). It was successful as a direct laryngoscope device in 80 of these 130 cases (61.5%; 95% CI 52.6% to 69.9%). In 49 of these 130 cases, the operator switched to using the C-MAC as a video laryngoscope (37.7%; 95% CI 29.4% to 46.6%). The C-MAC was used initially as a video laryngoscope in 125 of 255 cases (49.0%; 95% CI 42.7% to 55.3%). It was successful as a video laryngoscope device in 114 of these 125 cases (91.2%; 95% CI 84.8% to 95.5%). In 6 of these 125 cases, the operator switched to using the C-MAC as a direct laryngoscope (4.8%; 95% CI 1.8% to 10.2%). See Figure 2 for a complete breakdown of the way the C-MAC was used.
When the C-MAC was used initially as a video laryngoscope, lens contamination of the C-MAC was assessed by the operator to be none in 99 of 125 cases (79.2%; 95% CI 71.0% to 85.9%), mild in 9 of 125 cases (7.2%; 95% CI 3.4% to 13.2%), moderate in 8 of 125 cases (6.4%; 95% CI 2.8% to 12.2%), and severe in 9 of 125 cases (7.2%; 95% CI 3.4% to 13.2%). The mean fogging score of the C-MAC was 1.2 cm on a 10-cm visual analog scale.
Limitations
This study has several important limitations. First, this was an observational study of C-MAC and direct laryngoscope use. Patients were not randomly assigned. The C-MAC is a newly introduced device; therefore, we thought it would not be safe to perform a randomized trial. We believed the observational design of this study would be able to demonstrate the efficacy of the C-MAC for ED intubations and that the results could lay the foundation for future randomized control trials. Because the data were observational, we performed a logistic regression to control for confounders. Furthermore, because the study was not randomized, we calculated a propensity score to incorporate into the logistic regression model. Although these statistical methods were used to account for the weaknesses inherent in an observational study, the results are still limited and must be interpreted with caution. We attempted to demonstrate that the clinical characteristics of the 2 patient groups were similar. However, there still may be selection bias because it is impossible to account for all characteristics, known and unknown, that would affect the success of intubations.
Second, because continuous quality improvement data collection forms were completed by residents after each intubation, the data are subject to self-report and recall bias. In addition, although 90% are filled out at intubation, 10% are filled out on a delayed basis and are further subject to recall bias. However, a comparison of the immediately completed and delayed completed forms showed no difference in our primary outcome variable (data not shown).
Third, this study was based on data that were collected at a single ED with a Level I trauma center where emergency medicine residents perform the majority of intubations. Residents in this program have a great deal of exposure to video laryngoscopy. Almost half of this ED's intubations are performed with video laryngoscopy. Thus, the results may not be generalizable to other clinical settings where operators have different levels of experience with direct or video laryngoscopy.
Fourth, when we compared the views obtained with the C-MAC to those obtained with a direct laryngoscope, we used the widely accepted Cormack-Lehane classification. This scoring system was designed and based on direct laryngoscopy only and thus may not entirely be applicable to video laryngoscopy. Furthermore, the Cormack-Lehane classification is a subjective evaluation of the view of the airway, and even experienced operators have been shown to have limited intra- and interobserver reliability.15 However, the Cormack-Lehane classification is the best available option for comparison.
Fifth, difficult airway characteristics were based on subjective assessment of the patient before intubation. This set of difficult airway characteristics has not been previously validated and is subject to a wide range of interpretation. However, several studies have shown the limitations of formal evaluation of traditional difficult airway predictors in the ED setting. Additionally, using our logistic regression model, the presence of at least 1 difficult airway characteristic, as earlier defined, proved to be a negative predictor for successful intubation.
Discussion
Intubation is the mainstay of airway management in the ED. It is accomplished daily in EDs throughout United States with a variety of airway devices, with a direct laryngoscope being the most common. Unfortunately, direct laryngoscopy has inherent limitations because it requires a direct line of sight between the operator's eyes and the laryngeal inlet.16 In many emergency patients, this is simply not possible, necessitating multiple attempts or a switch to an alternative airway device. Video laryngoscopes were designed to overcome the limitations associated with direct laryngoscopes and have shown great success in the operating room, ED, out-of-hospital environment, and simulation laboratory.6,7,10,17-26
In this study, the C-MAC was found to be associated with more successful intubations compared with a direct laryngoscope both in terms of ultimate success and first-attempt success. A multivariate regression analysis, with the inclusion of a propensity score, demonstrated a 12-fold increase in likelihood of successful intubation with C-MAC use compared with direct laryngoscope use (Table 2). In a randomized controlled crossover study of 150 patients undergoing intubation for anesthesia, the authors reported the proportion of ultimately successful direct laryngoscope intubations to be 88% (44 of 50) and C-MAC intubations to be 100% (55 of 55).27 The proportion of successful intubations is higher in this study than in ours, likely because this study involved patients undergoing routine intubation for elective anesthesia. Any patients who were considered to have difficult airways were excluded from the study. Furthermore, patients were intubated by one of 3 experienced anesthesiologists, each with at least 8 years of intubating experience.
In the subgroup of patients with difficult airway characteristics, C-MAC use was also associated with a higher proportion of successful intubations. As the number of difficult airway characteristics increases, the efficacy of the C-MAC appears to be unaffected. However, the efficacy of a direct laryngoscope degrades significantly (Table 3). These data are consistent with the only study to date, to our knowledge, that has compared the performance of the C-MAC with a direct laryngoscope in difficult airways. In this operating room study, the authors found that in patients with predicted difficult airways, the C-MAC was more successful than a direct laryngoscope.28
We found that in patients with restricted cervical mobility, the C-MAC was associated with a higher proportion of successful intubations than a direct laryngoscope. These data appear to validate the idea that cervical immobilization hinders the ability to create a direct line of sight to the laryngeal inlet with a conventional direct laryngoscope.5,29 Because the C-MAC obtains a view of the airway indirectly with the use of a micro video camera, cervical immobilization theoretically would have less effect on the view of the airway. This suggests that the C-MAC may be preferable to a direct laryngoscope in cervical spine–immobilized patients with blunt trauma.
The C-MAC may be used either as a video laryngoscope or a direct laryngoscope, but its efficacy was much greater as a video laryngoscope. This is not surprising because the use of the C-MAC as a video laryngoscope takes advantage of all the benefits of video laryngoscopy. In particular, it provides a magnified, indirect, panoramic view of the airway and allows supervision and guidance by an attending physician. Because it uses a standard Macintosh-type blade, it has the ability to perform as a direct laryngoscope in the event of fogging or gross lens contamination without removal of the blade. It is not clear why some operators in our study switched to a conventional direct laryngoscope whereas others stayed with the C-MAC and used it is a direct laryngoscope.
When the C-MAC was used as a direct laryngoscope, it was successful in a lower proportion of cases than a standard Macintosh direct laryngoscope (62% versus 84%; Figure 2). There are 2 likely explanations for this result. One is that the micro video camera on the undersurface of the C-MAC blade occupies space and may partially block the direct view of the operator. Another possible explanation is that, because it is easy to switch from using the C-MAC as a direct laryngoscope to a video laryngoscope without removing the blade, operators may abandon the C-MAC as a direct laryngoscope more quickly than they would a conventional direct laryngoscope.
In this study, we observed a marked improvement in the Cormack-Lehane view obtained with the C-MAC as a video laryngoscope compared with a direct laryngoscope and a concomitant increase in the proportion of successful intubations with the C-MAC. This is in contrast to studies of other video laryngoscopes, in which the improved Cormack-Lehane view has not always corresponded to increased success of intubation.6,7,21-24,30-33 The GlideScope and McGrath Series 5 (Aircraft Medical Limited, Edinburgh, UK) have blades with very steep angles, and this makes directing the endotracheal tube to the laryngeal inlet more challenging. Indeed, the manufacturer of the GlideScope has produced a proprietary stylet, the GlideRite Rigid Stylet, to facilitate directing the endotracheal tube with the GlideScope. Because the C-MAC uses a Macintosh-type blade with a conventional curve, the soft tissues of the upper airway are compressed, creating a more direct approach to the airway. Thus, passage of the endotracheal tube may not be as difficult as it is with other video laryngoscopes that incorporate blades with steep angles, and a special stylet is not required to pass the endotracheal tube.
Esophageal intubation is of great clinical significance. One study demonstrated that a single episode of esophageal intubation is associated with an increase in the incidence of hypoxemia, aspiration, cardiac dysrhythmias, and cardiac arrest.34 In our study, we found a low incidence of esophageal intubation with both the C-MAC and a direct laryngoscope. The C-MAC was associated with a lower incidence of esophageal intubation than a direct laryngoscope. This is likely due to the fact that the magnified, panoramic view allows operators and supervisors to more accurately identify the appropriate anatomy. Although all of these esophageal intubations were immediately recognized, they put the patient at an increased risk of other adverse events.
To our knowledge, this is the only study evaluating the C-MAC for intubations performed in the ED. In this observational study, the C-MAC was associated with a high proportion of successful intubations both in terms of ultimate success and first-attempt success. Using a logistic regression model compared with a direct laryngoscope, the C-MAC was shown to be predictive of successful intubation. These data suggest that the C-MAC is a more effective device than a direct laryngoscope for ED intubations. These results should be validated by prospective, randomized trials.
Acknowledgments
The authors acknowledge Asad Patanwala, PharmD, and Uwe Stolz, PhD, MPH, for their assistance with statistical analyses.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. This work was funded in part by grant NIH T35 HL007479.
Footnotes
Author contributions: JCS conceived the study, designed the data collection instrument, and managed the database. JCS, JM, and SC performed statistical analysis in the study. JCS, JM, MC, and LK contributed to the drafting of the article. JCS, JM, and SC contributed to revisions of the article. JCS takes responsibility for the paper as a whole.
References
- 1.Sakles JC, Laurin EG, Rantapaa AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325–332. doi: 10.1016/s0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 2.Tayal VS, Riggs RW, Marx JA, et al. Rapid-sequence intubation at an emergency medicine residency: success rate and adverse events during a two-year period. Acad Emerg Med. 1999;6:31–37. doi: 10.1111/j.1553-2712.1999.tb00091.x. [DOI] [PubMed] [Google Scholar]
- 3.Sagarin MJ, Barton ED, Chng YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46:328–336. doi: 10.1016/j.annemergmed.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Walls RM, Brown CA, 3rd, Bair AE, et al. Emergency airway management: a multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41:347–354. doi: 10.1016/j.jemermed.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 5.Manoach S, Paladino L. Manual in-line stabilization for acute airway management of suspected cervical spine injury: historical review and current questions. Ann Emerg Med. 2007;50:236–245. doi: 10.1016/j.annemergmed.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Sakles JC, Mosier JM, Chiu S, et al. Tracheal intubation in the emergency department: a comparison of GlideScope(R) video laryngoscopy to direct laryngoscopy in 822 intubations. J Emerg Med. 2012;42:400–405. doi: 10.1016/j.jemermed.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Platts-Mills TF, Campagne D, Chinnock B, et al. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16:866–871. doi: 10.1111/j.1553-2712.2009.00492.x. [DOI] [PubMed] [Google Scholar]
- 8.Raja AS, Sullivan AF, Pallin DJ, et al. Adoption of video laryngoscopy in Massachusetts emergency departments. J Emerg Med. 2012;42:233–237. doi: 10.1016/j.jemermed.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 9.Niforopoulou P, Pantazopoulos I, Demestiha T, et al. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–1061. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 10.Aziz M, Brambrink A. The Storz C-MAC video laryngoscope: description of a new device, case report, and brief case series. J Clin Anesth. 2011;23:149–152. doi: 10.1016/j.jclinane.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Cavus E, Callies A, Doerges V, et al. The C-MAC videolaryngoscope for prehospital emergency intubation: a prospective, multicentre, observational study. Emerg Med J. 2011;28:650–653. doi: 10.1136/emj.2010.098707. [DOI] [PubMed] [Google Scholar]
- 12.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. table of contents. [DOI] [PubMed] [Google Scholar]
- 13.Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med. 2004;44:307–313. doi: 10.1016/j.annemergmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Bair AE, Caravelli R, Tyler K, et al. Feasibility of the preoperative Mallampati airway assessment in emergency department patients. J Emerg Med. 2010;38:677–680. doi: 10.1016/j.jemermed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 15.Krage R, van Rijn C, van Groeningen D, et al. Cormack-Lehane classification revisited. Br J Anaesth. 2010;105:220–227. doi: 10.1093/bja/aeq136. [DOI] [PubMed] [Google Scholar]
- 16.Levitan RM, Heitz JW, Sweeney M, et al. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–247. doi: 10.1016/j.annemergmed.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 17.Nasim S, Maharaj CH, Malik MA, et al. Comparison of the GlideScope and Pentax AWS laryngoscopes to the Macintosh laryngoscope for use by advanced paramedics in easy and simulated difficult intubation. [Accessed April 24, 2012];BMC Emerg Med. 2009 9 doi: 10.1186/1471-227X-9-9. Available at http://www.biomedcentral.com/1471-227X/9/9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savoldelli GL, Schiffer E, Abegg C, et al. Comparison of the GlideScope, the McGrath, the Airtraq and the Macintosh laryngoscopes in simulated difficult airways. Anaesthesia. 2008;63:1358–1364. doi: 10.1111/j.1365-2044.2008.05653.x. [DOI] [PubMed] [Google Scholar]
- 19.Serocki G, Bein B, Scholz J, et al. Management of the predicted difficult airway: a comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol. 2010;27:24–30. doi: 10.1097/EJA.0b013e32832d328d. [DOI] [PubMed] [Google Scholar]
- 20.Malik MA, Subramaniam R, Maharaj CH, et al. Randomized controlled trial of the Pentax AWS, GlideScope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–768. doi: 10.1093/bja/aep266. [DOI] [PubMed] [Google Scholar]
- 21.Malik MA, Maharaj CH, Harte BH, et al. Comparison of Macintosh, Truview EVO2, GlideScope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–730. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- 22.Lim TJ, Lim Y, Liu EH. Evaluation of ease of intubation with the GlideScope or Macintosh laryngoscope by anaesthetists in simulated easy and difficult laryngoscopy. Anaesthesia. 2005;60:180–183. doi: 10.1111/j.1365-2044.2004.04038.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim JT, Na HS, Bae JY, et al. GlideScope video laryngoscope: a randomized clinical trial in 203 paediatric patients. Br J Anaesth. 2008;101:531–534. doi: 10.1093/bja/aen234. [DOI] [PubMed] [Google Scholar]
- 24.Kim HJ, Chung SP, Park IC, et al. Comparison of the GlideScope video laryngoscope and Macintosh laryngoscope in simulated tracheal intubation scenarios. Emerg Med J. 2008;25:279–282. doi: 10.1136/emj.2007.052803. [DOI] [PubMed] [Google Scholar]
- 25.Tan BH, Liu EH, Lim RT, et al. Ease of intubation with the GlideScope or Airway Scope by novice operators in simulated easy and difficult airways—a manikin study. Anaesthesia. 2009;64:187–190. doi: 10.1111/j.1365-2044.2008.05753.x. [DOI] [PubMed] [Google Scholar]
- 26.Deakin CD. The C-MAC videolaryngoscope for prehospital emergency intubation. Emerg Med J. 2011;28:643. doi: 10.1136/emj.2010.105221. [DOI] [PubMed] [Google Scholar]
- 27.Cavus E, Thee C, Moeller T, et al. A randomised, controlled crossover comparison of the C-MAC videolaryngoscope with direct laryngoscopy in 150 patients during routine induction of anaesthesia. BMC Anesthesiol. 2011;11:6. doi: 10.1186/1471-2253-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aziz MF, Dillman D, Fu R, et al. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. 2012;116:629–636. doi: 10.1097/ALN.0b013e318246ea34. [DOI] [PubMed] [Google Scholar]
- 29.Robitaille A, Williams SR, Tremblay MH, et al. Cervical spine motion during tracheal intubation with manual in-line stabilization: direct laryngoscopy versus GlideScope videolaryngoscopy. Anesth Analg. 2008;106:935–941. doi: 10.1213/ane.0b013e318161769e. table of contents. [DOI] [PubMed] [Google Scholar]
- 30.Cooper RM. Use of a new videolaryngoscope (GlideScope) in the management of a difficult airway. Can J Anaesth. 2003;50:611–613. doi: 10.1007/BF03018651. [DOI] [PubMed] [Google Scholar]
- 31.Lim Y, Yeo SW. A comparison of the GlideScope with the Macintosh laryngoscope for tracheal intubation in patients with simulated difficult airway. Anaesth Intensive Care. 2005;33:243–247. doi: 10.1177/0310057X0503300215. [DOI] [PubMed] [Google Scholar]
- 32.Powell L, Andrzejowski J, Taylor R, et al. Comparison of the performance of four laryngoscopes in a high-fidelity simulator using normal and difficult airway. Br J Anaesth. 2009;103:755–760. doi: 10.1093/bja/aep232. [DOI] [PubMed] [Google Scholar]
- 33.Malik MA, O'Donoghue C, Carney J, et al. Comparison of the GlideScope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: a manikin study. Br J Anaesth. 2009;102:128–134. doi: 10.1093/bja/aen342. [DOI] [PubMed] [Google Scholar]
- 34.Mort TC. Esophageal intubation with indirect clinical tests during emergency tracheal intubation: a report on patient morbidity. J Clin Anesth. 2005;17:255–262. doi: 10.1016/j.jclinane.2005.02.004. [DOI] [PubMed] [Google Scholar]