Abstract
Post-traumatic stress disorder (PTSD) is a chronic and debilitating condition characterized by persistent intrusive memories. Although effective treatments exist for PTSD, there is a need for development of alternative treatments. Diminished ability to control proactive interference may contribute to re-experiencing symptoms and may be a novel intervention target. The present study tested an intervention designed to modify proactive interference control. Forty-two women with PTSD were randomly assigned to a computerized cognitive training or a control condition. The impact of these programs on cognitive performance and symptoms was assessed. PTSD re-experiencing symptoms and interference control performance improved significantly more for individuals in the training group relative to those in the control group. Other PTSD and general distress symptoms improved equally over time in both groups. Cognitive training of this type may hold promise as a novel intervention for reducing PTSD symptoms, although the mechanism of action and implications for models of PTSD requires future study.
Keywords: PTSD, cognitive control, executive functioning, treatment, cognitive training
1. Introduction
Epidemiological estimates of exposure to trauma (defined by the APA DSM-IV (2000) “Criterion A”) range from 55 to 89% (Breslau et al., 1998; Kessler, Sonnega, Bromet, & Hughes, 1995; Stein, Walker, Hazen, & Ford, 1997). Though many individuals experience PTSD-like symptoms in the immediate aftermath of a traumatic stressor (e.g., distressing memories), only a minority goes on to develop the chronic, debilitating symptoms that constitute PTSD (Kessler et al., 1995; McNally, Bryant, & Ehlers, 2003). Individual differences in characteristics present before, during, or after a traumatic event may be important in understanding why some individuals go on to develop PTSD while others recover naturally.
The ability to regulate thought content, including the emergence and dismissal of memories, is one such factor that may account for variability in PTSD development. Persistence of distressing intrusive thoughts may stem from ineffective utilization of cognitive systems - specifically aspects of executive functioning - to inhibit or down-regulate information (e.g., Anderson & Levy, 2008; Joormann, Yoon, & Siemer, 2010; Verwoerd, de Jong, & Wessel, 2008). Recurrently accessing traumatic memories, potentially due to diminished executive functioning control, may conversely contribute to PTSD etiology or maintenance (e.g., McFarlane, Yehuda, & Clark, 2002). Executive functioning refers to domain-general control faculties that govern cognitive sub-processes used in higher order cognition (Miyake, Friedman, Emerson, Witzky, & Howerter, 2000). For the present purposes, the term interference control refers to the specific inhibitory sub-function of executive functioning designed to prevent irrelevant, incorrect, or otherwise unwanted but competing information from intruding into or persisting in working memory (e.g., Friedman & Miyake, 2004i). Interference control is a critical aspect of executive functioning that enables individuals to regulate unwanted thoughts by preventing these thoughts from entering consciousness and removing these thoughts once they come to mind (Unsworth, 2010).
In the case of PTSD, converging evidence implicates interference control as a key regulatory process involved in modulating intrusive cognitions (i.e., re-experiencing symptoms). First, compared to healthy controls, individuals with PTSD demonstrate deficits in interference control (e.g., Aupperle, Melrose, Stein, & Paulus, 2012), and exhibit differences in recruitment of brain regions thought to form the neural substrates of executive functioning (Etkin & Wager, 2007). Individuals with PTSD show difficulty controlling proactive interference, or difficulty regulating interference from previously learned stimuli when attempting to remember more recently learned stimuli (e.g., Bunting, 2006), and difficulty controlling proactive interference is associated with the re-experiencing PTSD symptom cluster (Bomyea, Amir, & Lang, 2012; Vasterling, Brailey, Constans, & Sutker, 1998). However, existing studies do not specify if interference control difficulty is a pre-existing risk factor for PTSD development, a maintenance factor, or a consequence of the disorder.
Second, interference control ability is inversely associated with intrusive thoughts about stressful experiences. Studies find that greater ability to control proactive interference is associated with fewer intrusive memories after an analogue traumatic stressor (e.g., Verwoerd, Wessel, & de Jong, 2009; Verwoerd, Wessel et al., 2011; Wessel et al., 2008). Performance during working memory capacity (WMC) tasks is similarly associated with intrusive thoughts during deliberate though suppression attempts. WMC tasks assess the amount of information that can be kept in working memory, and are highly dependent on one’s ability to utilize interference control (Bunting, 2006; Conway et al., 2005; Friedman & Miyake, 2004; Lustig, May, & Hasher, 2001; May, Hasher, & Kane, 1999). Results from two studies by Brewin and colleagues indicated that better WMC performance was associated with fewer intrusive thoughts while participants attempted to suppress neutral and negative, personally-relevant thoughts (Brewin & Beaton, 2002; Brewin & Smart, 2005). The association between proactive interference control and intrusive thoughts is consistent with the hypothesis that re-experiencing symptoms are manifestations of a breakdown or deficiency in this cognitive process.
Although existing literature posits that an association exists between proactive interference control and intrusive thoughts, it does not speak to the potential causal role of interference control in recurrent intrusive cognitions. Studies examining cognitive mechanisms of anxiety have addressed the question of causality through randomization of participants to experimental cognitive retraining programs, wherein participants repeatedly practice engaging in specific tasks to manipulate the target cognitive process (e.g., attentional bias, interpretation bias; Beard, 2011; MacLeod, 2012; Macleod & Mathews, 2012). Data from other psychiatric and healthy samples suggests that aspects of executive functioning performance are malleable with practice (e.g., Keshayan, Vinogradov, Rumsev, Sherrill, & Wagner, 2014). Moreover, one study found that executive functioning training impacted regulation of intrusive thoughts in non-clinical samples (Bomyea & Amir, 2011). Reductions in intrusive thoughts as a result of interference control training in a clinical sample would substantiate theoretical accounts of interference control as a potential mechanism for dysregulation of intrusive thoughts in psychopathology (e.g., Verwoerd et al. 2008). However, the clinical applications of executive functioning training programs for PTSD symptoms have yet to be explored.
Examining proactive interference control as an intervention target in PTSD has the potential to contribute to our understanding and treatment of the disorder in a number of ways. Existing psychosocial treatments focus on the content of trauma-related cognitions – that is, the types of negative beliefs and expectations an individual has about trauma-related stimuli and cues. While these cognitive behavioral treatments (e.g., prolonged exposure, cognitive processing therapy) are effective and empirically supported (Ponniah & Hollon, 2009), they require considerable time and effort from patients and may not be universally feasible, well received, or effective (Bradley, Greene, Russ, Dutra, & Westen, 2005; Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008). In contrast, interference control training would aim to alter the functioning of basic cognitive systems hypothesized to regulate re-experiencing symptoms. If effective, this type of training would inform models of interference control in PTSD, and potentially provide a novel approach to treatment that complements existing intervention techniques.
The current study reports the results of a pilot randomized controlled trial of a computer-based proactive control training program in women with PTSD secondary to sexual trauma (clinicaltrials.gov Identifier: NCT02139137). The sample was limited to a specific trauma type for a number of reasons. Given that sexual assault confers a higher risk for PTSD than many other trauma types, it is critical to conduct clinical research in this population (e.g., Breslau et al., 1998; National Center for Posttraumatic Stress Disorder, 2005). Results from the current trial can also be compared to a substantial body of literature of randomized controlled trials in this population. Participants were assigned to an eight-session cognitive training (high interference control; HIC) or control program (low interference control; LIC). The primary goal was to assess preliminary efficacy of the training on cognitions and symptoms from baseline to post-training. We hypothesized that individuals in the training condition would demonstrate improved cognitive performance (indexed by a WMC task) and decreased PTSD re-experiencing symptoms (indexed by the Clinician Administered PTSD Scale- Re-experiencing subscale), relative to the control condition. Secondary goals were to assess the clinical significance of PTSD symptom change, examine generalizability of symptom change to other PTSD symptom clusters, general distress and functional impairment, and understand the feasibility and tolerability of the training program.
2. Materials and Methods
2.1 Participants
Participants included 47 women between the ages of 18 and 65 diagnosed with PTSD secondary to sexual trauma. The study was approved by the institutional review boards (IRB) at the University of California, San Diego and San Diego State University (SDSU). Individuals were recruited to participate through several sources, including the university subject pool at SDSU and referrals through affiliated mental health providers. IRB-approved recruitment materials were also posted on multiple college campuses in San Diego County, CA, in community posting areas, and through online websites (e.g., www.craigslist.org). All recruitment materials and the informed consent documents indicated that participants would be participating in an experimental study testing the effects of a computer-based program on anxiety and traumatic stress symptoms.
At the initial intake assessment, diagnostic status was determined by a doctoral-level trainee under the supervision of a licensed clinical psychologist (A.J.L.). The Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams,1994), a semi-structured interview that assesses past and present diagnostic criteria, was used to collect information about Axis-I disorders and treatment history. PTSD diagnosis was determined using the Clinician-Administered PTSD Scale for DSM-IV (CAPS; Blake, Weathers, & Nagy, 1995). Interviews were videotaped, and a portion of the tapes were rated by a second independent clinician to assess inter-rater agreement for PTSD diagnoses. Interviewers agreed on diagnostic status in all cases. The Life Events Checklist (Gray, Litz, Hsu, & Lombardo, 2004) was used to assess trauma history as part of the CAPS administration. Eligible participants were required to meet primary DSM-IV diagnosis of PTSD secondary to a traumatic sexual experience. In the case where a participant had experienced multiple traumatic events, she was considered eligible for the study if sexual assault was subjectively considered the most distressing event. Exclusion criteria included current trauma- or PTSD-focused psychosocial treatment, recent change in non-trauma focused psychosocial treatment, active suicidality (i.e., expression of intent or plan to commit suicidal gestures, or suicide attempt within the past 6 months), evidence of substance dependence in the past 6 months, and evidence of current or past schizophrenia, bipolar disorder, or organic mental disorder. Individuals with additional diagnoses were not excluded so long as PTSD was the primary diagnosis. Participants taking medications (N = 6) were required to meet a six-week stability criterion. In addition, all participants were required to meet English-language proficiency criteria due to the linguistic requirements of the cognitive tasks (i.e., ability to accurately comprehend and respond to all questions during the clinical assessment, and to comprehend and follow instructions during the practice phase of the computer tasks).
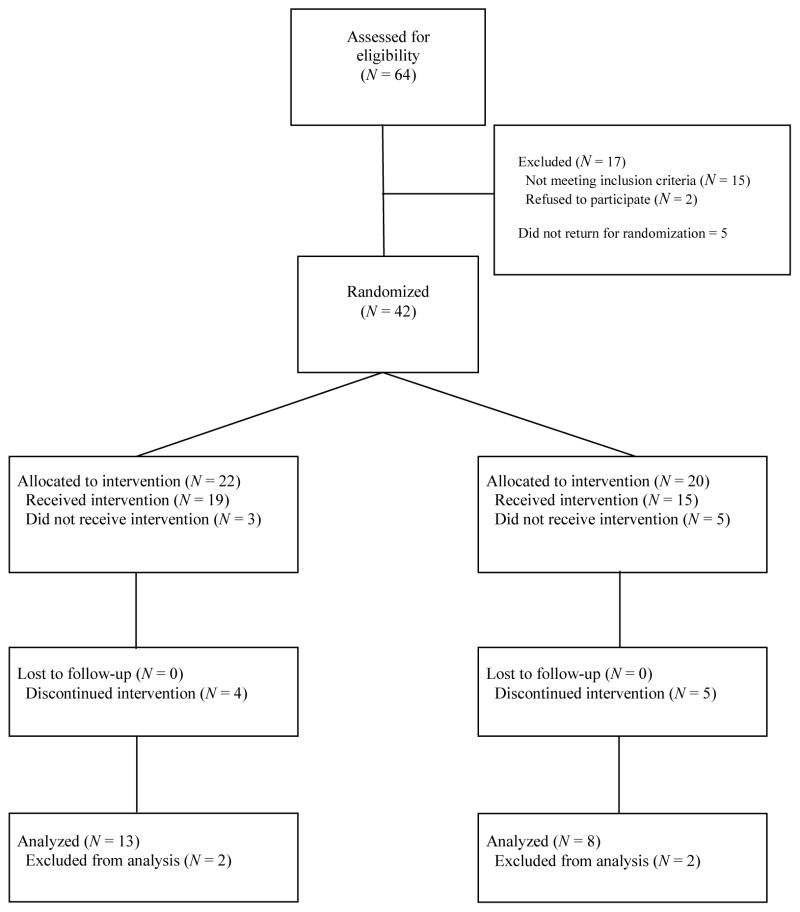
In total, 202 women inquired about the program and 139 were screened for participation. Sixty-four women were interviewed to assess eligibility (see Figure 1). Of those, 15 were excluded because they did not meet eligibility criteria (PTSD not primary or sub-clinical: N = 9, met diagnostic criteria for Bipolar disorder: N = 2, had recent medication or therapy changes: N = 2, reported that she had been diagnosed with dementia: N = 1, met multiple exclusion criteria: N = 1), and two participants declined further participation after the initial interview. Of the 47 women who were eligible and consented to participate, 42 attended the baseline assessment session and were subsequently randomized to the HIC or LIC condition. Of these, eight did not return to begin the intervention (HIC: N = 3, LIC: N = 5), nine additional participants dropped out after treatment initiation and were unavailable for subsequent assessments (HIC: N = 4, LIC: N = 5), and four were removed for not following study instructions or experiencing a change that would meet exclusion criteria (e.g., initiating new treatment). Although most individuals who dropped out of the study could not be reached, reasons provided for dropping included unexpectedly leaving the San Diego area (N = 1), obtaining new work that conflicted with appointment scheduling (N = 3), sudden medical illness unrelated to the study (N =1), being advised by a provider or family member not to participate (N = 2). There were no statistically significant differences in demographic characteristics, baseline clinical characteristics, or initial perceived treatment acceptability (all ps > .10) between women who completed the study and those who dropped out of treatment prematurely.
Figure 1.
Flow chart of the progression of participants through the study
2.2 Measures
2.2.1 Interviewer administered measures
The CAPS was administered during pre- and post- training assessments to determine PTSD diagnosis and symptom severity; this served as the primary symptom dependent measure. The CAPS is a structured interview designed to measure symptoms of PTSD (Weathers, Keane, & Davidson, 2001). Severity was determined using a total score of frequency and intensity ratings for each symptom item. Dichotomous PTSD diagnosis was determined by converting severity and intensity ratings using the “F1/I2” scoring rule (i.e., a symptom is considered present if the frequency is scored at least 1 and intensity is scored at least 2; Weathers, Ruscio, & Keane, 1999). The SCID-IV was employed at the pre-training assessment to determine presence/absence of comorbid Axis-I disorders according to DSM-IV criteria and to determine inclusion/exclusion criteria.
2.2.2 Self-report measures
Participants completed a demographics form pre-training, which included questions regarding participant age, ethnicity, marital status, and years of education. Anxiety and depression were measured at pre- and post- training assessments. The State Trait Anxiety Inventory (STAI-T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) was administered to assess general anxiety. The STAI is a 40-item self-report measure of anxiety with items scored on a one to four scale; the 20 items assessing feelings of trait anxiety were used in the present study to assess general anxiety level. Total scores for state and trait anxiety reflect the sum of items on respective scales. This measure possesses adequate psychometric characteristics (Spielberger et al., 1983). In addition, the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was administered to assess symptoms of depression. The BDI-II is a 21-item scale assessing symptoms over the previous two weeks. All items are multiple-choice and scored on a scale of zero to three; total scores are based on the sum of items, ranging from zero to 63. The BDI-II is a reliable and well-validated measure of depressive symptoms (Beck et al., 1996).
At the pre- and post-training assessment sessions, participants completed a brief treatment credibility measure (TCM; adapted from Borkovec & Nau, 1972). This 3-item measure assesses how logical the treatment seems, how confident the individual feels that the treatment will be effective, and how confident the individual would be recommending the treatment to a friend. Each item is rated on a zero to eight scale. As an additional measure of acceptability, the number of sessions the participant attended was calculated after the individual completed participation.
2.2.3 Working memory capacity assessment: Ospan
Proactive interference control was assessed before and after the training program using a computerized WMC task (Ospan; Unsworth et al., 2005) to determine whether cognitive gains from the training task would be observed on a similar task with novel stimuli. In this task, each trial begins with a fixation cross in the center of the screen for 500ms. Then, a completed math problem (e.g., “1+3 = 6”) appears on the screen. Half of the equations presented are correct and half are incorrect. The participant determines whether the math solution is correct by selecting a box on the screen using the mouse (left box for “yes,” right box for “no”). Once the participant completes the math problem, a letter (e.g., “L”) appears on the screen for 500ms. Then the next trial begins with another equation and letter, until the end of the set. At the end of each set, a recognition screen listing twelve letters appears. Using the mouse, participants select the letters that were presented in the correct serial order. Once the recognition for the set is completed, the next set of trials begins in the same manner. The participant receives feedback about their math accuracy and memory at the conclusion of each set. Consistent with prior studies using this task, the assessment tested working memory span sizes from two to seven (Conway et al., 2005). Performance was measured as the percent of items correctly identified in the correct order. Sets and trials appeared in a different random order for each participant.
2.3 Training Program
Participants were randomized to complete an eight-session version of the training program described by Bomyea & Amir (2010). These paradigms consisted of two modified Reading Span WMC tasks designed to vary in the amount of proactive interference control required (Rspan tasks; Daneman & Carpenter, 1980, adapted by Lustig, et al., 2001). In this task, each trial begins with a fixation cross in the center of the screen for 500ms. Then, a sentence (e.g., “Jane walks her car in the park”) appears on the screen. The participant is asked to determine whether the sentence makes sense by selecting a box on the screen using the mouse (left box for “yes,” right box for “no”). Half of the sentences presented were grammatically correct (i.e., made sense) and half were not. Once the participant completes the sentence problem, an item appears on the screen for 500ms. Then the next trial begins with another sentence and item, until the end of the set. At the end of each set participants view a recognition screen listing twelve items. Using the mouse, participants select the items that were previously presented in the correct serial order. Once the recognition for the set is completed, the next set of trials begins in the same manner. During the task, the participant receives feedback about their sentence accuracy and memory at the conclusion of each set. Participants completed three blocks of training in each session. Within each block, participants trained on span sizes of two to six, with three repetitions of each span size presented in random order. Thus, during the three blocks the participant completed 45 trials total. Items and sentences used in the training task derived from four sets (one for each week), with the order of sets counterbalanced across participants. Prior studies suggest that WMC such as Rspan require proactive interference control to perform accurately as trials progress. Item similarity is one factor that determines the amount of interference exists within the task – stimuli that are more similar create more interference, while less similar stimuli create less (Bunting, 2006).
2.3.1 High interference control (HIC) condition
The HIC condition, the experimental training condition, was designed to contain high proactive interference across trials by including item memoranda for all trials that were words (Bunting, 2006). Words used in the training task were selected from the MRC Psycholinguistic Database and included semantically unrelated words within the following parameters: length between four to eight words, frequency ratings between 30 to 100, and familiarity ratings between 400 and 700.
2.3.2 Low interference control (LIC) condition
The LIC condition, the control condition, was designed to contain relatively less proactive interference across trials, by alternating item memoranda between words and numbers (digits one through 12) every three trials (Bunting, 2006). Thus, although participants were required to remember the same total number of items as in the HIC (i.e., storage requirements were equivalent), there was relatively less proactive interference inherent in the task because trials with number memoranda interfere minimally on trials with word memoranda and vice versa.
2.4 Procedure
2.4.1 Baseline pre-training assessment session
Upon arrival, participants were informed about the study procedures, including a standardized description of the study rationale, and gave written informed consent. Participants completed the clinical interview and self-report assessments to ascertain current and past mental health diagnoses, anxiety, depression levels, and trauma history. Eligible participants returned for a second assessment session to complete the baseline Ospan assessment and additional self-report and cognitive assessments. Individuals who completed all baseline assessments were randomly assigned to the HIC condition or the LIC condition based on a computer-generated random number system prior to attending the first training session. Conditions were assigned by an independent third party using computer software, so that participants and research personnel remained blind to subjects’ conditions.
2.4.2 Training sessions
Participants returned to complete eight experimental sessions over four weeks (approximately twice weekly). Selection of eight biweekly sessions was based on prior research using cognitive bias modification techniques in anxious populations (e.g., Amir et al., 2008). During each session, which lasted approximately 30 minutes, the participant completed three blocks of the respective HIC or LIC task.
2.4.3 Post-training assessment session
One week after completion of the last training session, participants returned to complete the post-training assessment. At this point, participants completed a similar assessment battery to that used during the baseline pre-training assessment session, including a clinical interview (CAPS), self-report packet (STAI-T, BDI-II), and cognitive assessments (Ospan).
2.5 Statistical Analyses
Primary outcome measures included: 1) performance on the cognitive assessment of proactive interference control (Ospan), and 2) PTSD re-experiencing symptoms (CAPS symptom severity scores for re-experiencing items). Clinical significance of symptom change was evaluated based on change in diagnostic status and/or a reduction of 80% or more in total PTSD symptoms. Secondary analyses were conducted to examine the generalization of the manipulation to other PTSD symptom clusters, general distress and functional impairment (STAI-T, BDI-II, and SDS scores). All analyses were conducted using SPSS version 18.0. Prior to conducting primary analyses, data were examined using box plots. For one data point deemed to be an outlier in the cognitive task data (i.e., a value lying outside three standard deviations of the mean for that variable), a winsorizing procedure was applied by replacing the value with the next most extreme data point (Fox & Knight, 2005; Tabachnick & Fidell, 2007). Analysis of covariance (ANCOVA) was used to test group differences at post-training controlling for participants’ baseline scores for the measure of interest (Van Breukelen, 2006; Vickers & Altman, 2001). Because PTSD symptoms and education (as a proxy for vocabulary and reading ability) would be predicted to impact cognitive performance on WMC tasks, these were also included as covariates on analyses of Ospan score. Each analysis was conducted two ways. First, intent-to-treat (ITT) analyses were conducted on all randomized participants, with missing data imputed using the last observation carried forward (LOCF) method for individuals who did not complete the post-training assessment. Second, these analyses were repeated including only participants who completed all pre- and post-training assessments.
In addition, an exploratory mediation analysis was conducted in the ITT sample to examine the potential effect of changes in cognitive functioning on changes in re-experiencing symptoms. To determine the presence of mediation, analysis was conducted to determine whether or not the potentially mediating variable (i.e., residualized change in Ospan) partially or fully accounted for the relationship between the independent variable (i.e., condition, HIC or LIC) and the outcome of interest (i.e., residualized change in CAPS re-experiencing symptoms). Originally described by Baron and Kenny (1986), mediation traditionally involves demonstration that the relationship between a given independent variable and the outcome of interest is reduced when the mediator and independent variable are modeled simultaneously (see also Mackinnon, Fairchild, & Fritz, 2007 for an updated description of mediated effects). We used bootstrapping procedures to test the indirect effect of group (HIC, LIC), on change in CAPS re-experiencing severity scores through change in Ospan performance (Preacher & Hayes, 2008).
3. Results
3.1 Baseline Characteristics
Tables 1 and 2 present descriptive data for sociodemographic and clinical variables. Comorbid DSM-IV diagnoses included major depressive disorder or other mood disorders (N = 22, 52.4%), anxiety disorders (N = 20, 47.6%), substance abuse (N = 4, 9.5%), and eating disorders (N = 2, 4.8%). Separate one-way analyses of variance (ANOVAs) indicated that participants in the two groups did not differ on age or measures of clinical features, including CAPS total severity, duration of PTSD symptoms, number of trauma types experienced, STAI-T, BDI-II, SDS, or Ospan performance (all ps > .10). Chi-square analyses did not reveal differences in participant ethnic background, education, income, or marital status (all ps > .20). On average, participants reported a level of PTSD severity considered to be in the low end of “severe” (i.e., a CAPS total score of 60–79; Weathers et al., 2001), although there was considerable variability (range: 34 – 94). BDI-II scores suggested participants were on average in the moderately severe range of depression (Beck et al., 1996).
Table 1.
Baseline characteristics of ITT sample.
| Variable | HIC (N = 22) | LIC (N = 20) |
|---|---|---|
| Mean Age (SD) | 29.82 (1.71) | 26.00 (10.6) |
|
| ||
| Education | n | n |
| < 12 years | 0 | 1 |
| 12 years | 3 | 4 |
| 13 –15 years | 11 | 8 |
| 16 years | 6 | 5 |
| > 16 years | 2 | 2 |
|
| ||
| Racial category | ||
| Caucasian | 16 | 13 |
| Black | 2 | 1 |
| Asian | 4 | 5 |
| Other/Biracial | 0 | 1 |
|
| ||
| Marital Status | ||
| Single | 16 | 8 |
| Married | 2 | 6 |
| Divorced | 1 | 1 |
| Cohabitating | 2 | 2 |
| Other/declined to respond | 1 | 3 |
|
| ||
| Income (thousands per year) | ||
| > $50 | 5 | 2 |
| $20–50 | 8 | 6 |
| < $15 | 8 | 12 |
|
| ||
| Mean number of traumas (SD) | 5.33 (2.52) | 4.50 (1.92) |
|
| ||
| Mean months duration of PTSD (SD) | 146.91 (159.33) | 97.25 (113.46) |
Table 2.
Descriptive statistics in ITT and completer samples.
| Variable | HIC (NITT = 22) | (NC = 13) | LIC (NITT = 20) | (NC = 8) |
|---|---|---|---|---|
| Mean CAPS total severity score at pre (SD) | 61.41 (12.54) | 61.00 (13.40) | 67.35 (15.0) | 68.00 (19.86) |
| Mean CAPS total severity score at post (SD) | 45.32 (19.92) | 33.77 (15.67) | 58.50 (18.61) | 45.88 (20.55) |
| Within-group pre-post effect size | d = .92*** | d = 1.85*** | d = .52* | d = 1.10** |
|
| ||||
| Mean CAPS Avoidance severity score at pre (SD) | 24.32 (7.31) | 23.69 (7.89) | 26.90 (6.75) | 27.00 (7.48) |
| Mean CAPS Avoidance severity score at post (SD) | 18.73 (9.49) | 14.23 (8.59) | 22.95 (8.31) | 17.13 (7.43) |
| WIthin-group pre-post effect size | d = .64** | d = 1.14** | d = .52* | d = 1.32* |
|
| ||||
| Mean CAPS Arousal severity score at pre (SD) | 20.91 (6.17) | 21.85 (5.96) | 22.00 (6.37) | 22.88 (8.79) |
| Mean CAPS Arousal severity score at post (SD) | 15.82 (7.19) | 13.23 (6.62) | 18.75 (7.13) | 14.75 (8.73) |
| Within-group pre-post effect size | d = .75** | d = 1.36*** | d = .48* | d = .92* |
|
| ||||
| Mean STAI- Trait at pre (SD) | 58.09 (9.66) | 56.00 (9.34) | 56.88 (13.41) | 59.50 (11.51) |
| Mean STAI- Trait at post (SD) | 52.05 (13.36) | 45.77 (11.99) | 53.93 (13.69) | 52.13 (12.65) |
| Within-group pre-post effect size | d = .48** | d = .92** | d = .22 | d = .61 |
|
| ||||
| Mean BDI at pre (SD) | 27.18 (11.33) | 24.46 (11.16) | 29.60 (10.84) | 32.13 (5.11) |
| Mean BDI at post (SD) | 20.36 (14.76) | 12.92 (12.41) | 25.05 (12.91) | 20.75 (11.67) |
| Within-group pre-post effect size | d = .48** | d = .97** | d = .37* | d = 1.20* |
|
| ||||
| Mean SDS at pre (SD) | 18.59 (7.71) | 18.46 (8.17) | 18.16 (6.09) | 20.71 (5.25) |
| Mean SDS at post (SD) | 15.40 (9.00) | 13.07 (9.48) | 15.85 (6.77) | 14.63 (7.76) |
| Within-group pre-post effect size | d = .37 | d = .60* | d = .26 | d = .67 |
Note: CAPS: Clinician Administered PTSD Scale; STAI: Spielberger State Trait Anxiety Inventory; BDI: Beck Depression Inventory; SDS: Sheehan Disability Scale. nITT = N of intent-to-treat sample, nC = N of completer sample. Effect size d refers to Cohen’s d for repeated measures designs, which compares the difference between means within each group from pre- to post-training, accounting for the correlation between measurements (Cohen, 1988).
Within group t-test Indicates p < .05,
p< .01,
p< .00
3.2 Credibility, Acceptability, and Adherence
On a scale of 0 (not at all) to 8 (very), participants on average rated the treatment as moderately logical (M = 5.33, SD = 1.62), indicated that they were moderately confident that the treatment would work (M = 4.73, SD = 1.71), and reported that they were moderately confident in recommending the program to others (M = 5.27, SD = 1.43) at baseline. No significant group differences were found on confidence, logic, or recommendation items of the treatment credibility questionnaire at the pre-training assessment (ps > .10), but results suggested that individuals in the LIC condition rated the program as more logical than those in the HIC at the post-training assessment, F (1, 24) = 8.42, p < .01. Number of completed sessions was assessed to determine if the HIC and LIC groups demonstrate differential drop-out rates. Results suggested that there were no group differences in drop rate between the HIC and LIC groups (p > .4).
3.3 Change in WMC
The effectiveness of the manipulation was assessed by comparing post-training WMC (Ospan) performance between the groups using ANCOVA analysis. Results of the ITT analysis revealed a significant effect of group, F(1, 42) = 8.45, p < .01, ηp2 = .03, such that individuals in the HIC group demonstrated higher Ospan scores than those in the LIC at post-training. Similarly, in the subsample of participants who completed the protocol, there was a significant effect of group, F(1, 20) = 4.81, p < .05, ηp2 = .05.
3.4 Change in PTSD Re-experiencing Symptoms
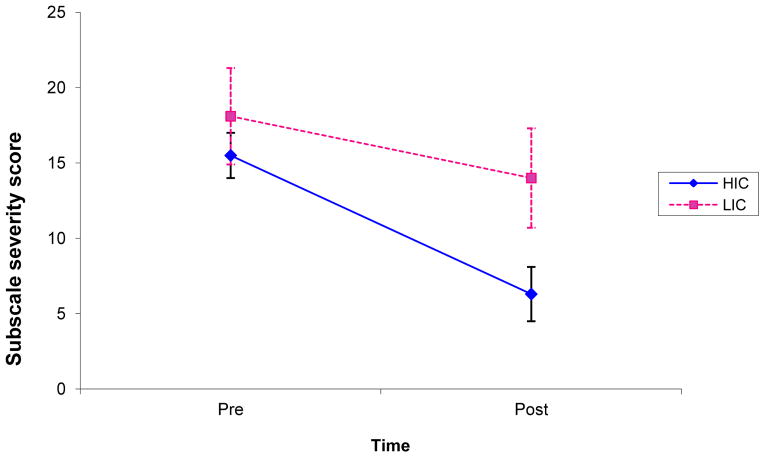
CAPS re-experiencing scale scores at post-training were submitted to ANCOVA analysis. Results of the ITT analysis revealed a significant effect of group F(1, 42) = 5.51, p < .03, ηp2 = .06, such that individuals in the HIC group demonstrated lower re-experiencing scale scores than those in the LIC at post-training. Similarly, in the subsample of participants who completed the protocol, there was a significant effect of group, F(1, 20) = 5.06, p < .04, ηp2 = .11. Figure 2 graphically depicts CAPS re-experiencing scale scores pre- and post-training.
Figure 2.
Mean severity score on the re-experiencing subscale of the Clinician Administered PTSD Scale for the HIC (N = 13) and LIC (N = 8) groups (bars represent standard errors).
3.5 Clinical Significance
To determine clinical significance of observed changes, the percentage of individuals in the HIC and LIC groups who no longer met diagnostic criteria for PTSD at post assessment was compared. Chi-squared analyses indicated no significant between-group difference in the number of individuals who no longer meet diagnostic criteria on the CAPS in the ITT (45% in HIC vs. 30% in LIC; Χ2(1) = 1.06, p = .30; Φ = .16, p = .30) or completer samples (77% in HIC vs. 63% in LIC; Χ2(1) = .51, p = .48; Φ = .16, p = .49). Recovery status chi-square analysis also indicated no significant difference in percentage of responders in the ITT (50% in HIC vs. 30% in LIC; Χ2(1) = 1.74, p = .19; Φ = −.20, p = .18) or completer samples (85% in HIC vs. 75% in LIC; Χ2(1) = 0.30, p = .59; Φ = −.12, p = .60). No participants experienced clinically significant deterioration.
3.6 Symptom Generalization
Symptoms from the avoidance and arousal clusters of the CAPS PTSD assessment were entered into separate ANCOVA analyses. In both ITT and completer samples, there was no significant effect of group on post-training avoidance (p > .3, .7, respectively) or arousal symptoms (p > .2, .7, respectively). Symptoms of anxiety, depression, and functional impairment post-training were also entered into separate ANCOVA analyses. Across all analyses, results revealed no significant effect of group on post-training measures, controlling for pre-training scores in the ITT (STAI-T: p > .2, BDI-II: p > .4, SDS: p > .4) or completer samples (STAI-T: p > .4, BDI-II: p > .7, SDS: p > .2). Table 2 presents descriptive information for CAPS total severity and SDS scores.
3.7 Exploratory Mediation Analysis
Overall, the mediation model accounted for a significant amount of the variance in predicting change in CAPS re-experiencing severity scores, R2 = .20 F(2, 39) = 4.76, p = .01. The direct path from the independent variable (group) to the mediator (change in Ospan score) was significant, a = −0.64, t = −2.17, p = .04. The direct path from the mediator to the dependent variable (change in CAPS re-experiencing scores) was marginally significant, b = 0.29, t = −1.93, p = .06. The total effect of group on change in CAPS re-experiencing scores was significant, c = −0.68, t = −2.33 p = .03, but the effect of group on change in CAPS re-experiencing scores while controlling for change in Ospan scores was not, c′ = −0.49, t = −1.65, p = .11. Examining the 95% confidence interval of the effect of change in Ospan performance on change in CAPS re-experiencing symptoms (i.e., the indirect or ab path) indicated that it overlapped with zero, 95% CI [−.55, .03]. Thus, the findings indicated that the mediated effect did not reach statistical significance.
4. Discussion
The current study sought to experimentally manipulate proactive interference control using a WMC task in order to modify re-experiencing symptoms in a sample of women with PTSD. Consistent with hypotheses, individuals in the HIC group demonstrated significantly better cognitive performance post-training relative to those in the LIC group, controlling for pre-training performance. Also consistent with hypotheses, individuals in the HIC condition reported significantly lower levels of re-experiencing symptoms than those in the LIC, controlling for initial re-experiencing symptom severity. Mediation analysis showed evidence of partial mediation according to the guidelines established by Baron and Kenny (1986); however, the indirect effect of change in WMC did not reach statistical significance using bootstrapping techniques. In addition, there was no differential change between groups in other types of PTSD symptoms, associated symptoms or clinical significance of improvements. Examination of the pattern of means suggests that this lack of between-group differences was driven in part by improvements in the LIC group. Findings represent the first published study to our knowledge that suggests a computerized cognitive control training program with neutral stimuli (i.e., “cold” or void of emotional valence) may have beneficial effects on re-experiencing symptoms in individuals with PTSD.
Previous studies demonstrate that training on WMC tasks and cognitive processes more broadly have the potential to alter performance on similar tasks; the first goal of this study was to demonstrate the effectiveness of this specific program on WMC in a sample of individuals with PTSD. While much of the literature on training of executive functioning and cognitive control has conducted training with non-clinical samples (e.g., older adults, Buschkuehl et al., 2008; unselected adults, Jaeggi et al., 2008, Harrison, Shipstead, Hicks, Hembrick, Redick, & Engle, in press; Olesen, Westerberg, & Klingberg, 2004; Schweizer, Hampshire, & Dalgleish, 2011), preliminary evidence suggests that similar kinds of training protocols are beneficial for certain psychiatric patient populations (e.g., children with ADHD, Klingberg et al., 2005; individuals with schizophrenia, Dickinson et al., 2010; Vinogradov, Fisher, & de Villers-Sidani, 2012; depression, Siegle, Ghinassi, & Thase, 2007). Cognitive bias modification, using retraining of attention or interpretation of threat stimuli, has similarly demonstrated efficacy in altering cognitive processes (e.g., Amir & Taylor, 2011), but the use of non-valenced domain-general training (i.e., utilizing generic cognitive processes in the absence of threat), has not been explored in PTSD. This study represents the first piece of evidence suggesting that one specific cognitive process – proactive interference control – is malleable with practice in this population. Compared to the non-clinical participants who received a single session of training in Bomyea and Amir (2011), participants in the current study achieved smaller gains in WMC performance in spite of receiving seven more sessions. Effectively training the necessary proactive interference control may be more difficult in this population relative to healthy undergraduates, consistent with suggestions that individuals with certain types of psychopathology may be more resistant to training due to deficits in the cognitive systems that this type of training targets (Vinogradov et al., 2013). Alternatively, given that age detrimentally influences cognitive plasticity (Mahncke, Bronstone, & Merzenich, 2006), the difference in mean age across studies may account for differential training effects. Future study is needed to determine the optimal dose of such training procedures to achieve higher cognitive performance, and what level of cognitive performance is optimal for experiencing generalization to symptom reduction.
The second primary goal of the current study was to examine the effect of the HIC and LIC programs on re-experiencing symptoms. A growing body of literature supports theoretical models linking poor interference control ability to increased intrusive thoughts (e.g., Anderson & Levy, 2011). Existing data has been correlational in nature or experimental within non-clinical samples (e.g., Bomyea, Amir, & Lang, 2012; Eren-Kocak, Kilic, & Hizli, 2009). The present data are the first to indicate that manipulating interference control via training may lead to a reduction in re-experiencing symptoms for individuals with PTSD. Results are consistent with literature suggesting that modification of cognitive processes, such as attention or interpretation biases, leads to a reduction of psychological symptoms (Hallion & Ruscio, 2011). Unlike computerized cognitive bias modification programs, however, this current training program did not explicitly tap cognitive biases or processes in an effort to correct preferential processing of threat information. Instead, the training program aimed to target affectively neutral cognitive control processes. The reduction in symptoms suggests some degree of generalization of training gains may occur, such that processes involved in interference control more generally play a role in the regulation of emotionally-laden cognitive phenomena (e.g., traumatic memories).
Across both the HIC and LIC groups, most participants experienced reductions in overall PTSD symptoms and depression. Given that PTSD is typically a chronic unremitting disorder in the absence of treatment, the proportion of participants with clinical change and the degree of symptom change suggests both LIC and HIC may have conferred benefits. For example, response rates for the LIC were somewhat higher than typically reported for waitlist or active intervention control groups (e.g., 10% Rothbaum et al., 2005; 20% Schnurr et al., 2007; 26% Chard, 2005). Future work is needed to understand the course of change across each of the symptom clusters, including the extent to which reduction in re-experiencing symptoms might generalize to other symptom types over time. While no statistically significant differential improvement occurred over time between the HIC and LIC conditions, participants in the HIC group generally reported modestly greater improvements in overall severity and self-rated functional impairment. The lack of statistical differences between these two groups may reflect a combination of lack of statistical power and effects of the LIC being a less potent version of the HIC (i.e., some degree of interference control was still necessary for the task). However, firm conclusions about the contribution of the LIC program to symptom and functioning changes cannot be made in the absence of a waitlist control group.
In spite of differential change between the HIC and LIC groups on cognitive performance and re-experiencing symptoms, the mechanism of change remains unclear. Mediation analyses designed to test change in WMC as a mediator of the relationship between condition and re-experiencing symptoms did not reach statistical significance. Given the small sample, this type of analyses was likely underpowered to detect statistical significance of the indirect path in a mediation approach. Alternatively, the measure utilized to assess proactive interference control may not have optimally captured the purported cognitive process at work because of the additional cognitive capacities required for the task (e.g., memory). Other mechanisms may also account for the reduction in symptoms over time. These might be non-specific factors such as the behavioral activation required to come to the lab weekly, placebo expectancy effects from attending either the HIC or LIC sessions, or talking openly about traumatic experiences with the assessor. Regression toward the mean is another possible explanation for these changes, although it seems unlikely that this would fully account for the changes observed in participants based on the observed effect sizes. Although existing ranges for response rates in randomized controlled trials of psychosocial interventions for female patients with PTSD vary widely (e.g., 39% for female veterans in Schnurr et al., 2007; 73% for CPT for female sexual trauma survivors in Chard, 2005; 95% for female sexual assault survivors in Rothbaum et al., 2005), the response rate for both the HIC and LIC were within the range reported in other studies. The numbers in the present study may be slightly higher due to the relatively mild overall severity of the sample. Future study is needed to determine how the HIC and LIC tasks may differentially affect re-experiencing symptoms, and if and how these two training programs may affect general distress symptoms.
A number of limitations to the present study warrant consideration. First, the sample of women recruited for the study was relatively small and characterized by a high drop-out rate. Treatment drop-out rates are reported to be relatively high in some PTSD treatment outcome studies (up to 55%; Schottenbauer et al., 2008). The rate in the present study (40% of those randomized, 26% of those who began the intervention) is on the upper end of the published rates in prior research. The relatively high rate of voluntary withdrawal from the study could be due to a number of factors. First, given that avoidance is a cardinal feature of PTSD, participants may have felt that returning to the lab after completing difficult assessments (e.g., CAPS) was too difficult or unpleasant. Second, features of the study design may have contributed. The study was not recruiting from treatment-seeking groups. Thus, motivation to continue with the program may have been relatively diminished for some individuals, particularly for those who perceived the computer program as uninteresting or burdensome.
A number of characteristics of the sample also limit generalizability. The decision to select a sample homogenous in terms of trauma history is consistent with other treatment outcome studies for PTSD, and was done to maximize study power to detect an effect of the HIC/LIC manipulation. However, this selection process limits conclusions that can be made about the potential effects of the HIC or LIC programs in individuals with other types of trauma exposure. Similarly, the use of relatively stringent inclusion/exclusion criteria means that findings may not generalize to other samples with specific comorbid conditions or other features that were not included in this study. In addition, although the participants all met clinical diagnoses for PTSD, on average the level of symptomology was only moderate.
A final limitation of the study is the lack of a minimal-attention control group. Because the study was designed to test one specific aspect of cognitive control – proactive interference control – the two groups tested both completed similar programs with only this aspect modified. The addition of an alternative control group would bolster the conclusions regarding the role of proactive interference control relative to regression toward the mean, the effect of repeated testing, or other non-specific factors.
Debate exists regarding the effectiveness of intervention programs within the broader literature on cognitive training; some authors optimistically (and cautiously) advocate for the utility of such programs (Morrison & Chein, 2011), while others call into question the validity of existing evidence for cognitive training (Redick et al., 2013; Shipstead, Redick, & Engle, 2012). Although a recent meta-analysis provides support for the utility of training programs for short-term cognitive gains on “near-transfer” tasks (i.e., generalization to test that are very similar to trained tasks), evidence for the long-term benefit of completing such training programs and the generalization of training effects beyond trained tasks is weak (Melby-Lervâg & Hulme, 2013; Shipstead, Redick, & Engle, 2012). The methods used in the current study address some limitations of earlier cognitive training studies outlined in a critical review of cognitive training programs authored by Shipstead and colleagues (e.g., using a novel complex span task to assess working memory, using an active control comparison). Criticisms of cognitive training, however, highlight the need for multiple assessments to verify that training gains truly modify the underlying construct of interest, additional assessment across cognitive domains to determine far transfer (and beyond self report, in the case of symptoms), and examination of the long-term benefit of training. Inclusion of these criteria in future studies that evaluate cognitive training’s effects in PTSD are needed to bolster confidence that such programs do indeed operate via cognitive improvements.
Better understanding of ways to optimize training, if effects are replicated, is also needed. As currently described and conceptualized by the authors (and others, see for example Melby-Lervâg & Hulme, 2013), training programs are considered akin to “strength training” of a muscle; training is analogous to a taxing, repetitive exercise designed to strengthen cognitive systems and underlying neural networks involved in complex cognition. In the case of PTSD, training effects may naturally be perpetuated by successful cognitive regulation over memories in daily life following training. Other, differing accounts of training may also apply. As one example, cognitive training could be conceptualized as a cognitive “vaccine” that is delivered, in a brief period, with the anticipation of enduring effects over timeii. In spite of growing literature on the effects of cognitive training in last several decades, understanding of how training delivers its effects is still in a nascent state, and research on this topic is a critical next step for this area.
In summary, this study experimentally tested two computerized programs designed to differentially train proactive interference control, with hypotheses derived from prior theory and empirical data suggesting a link between cognitive control and re-experiencing symptoms. Results indicated that participants in the HIC demonstrated gains in WMC and PTSD re-experiencing symptoms relative to those in the LIC, although both the HIC and LIC conditions improved in general distress symptoms and functional impairment over time. Results are promising in that participants completing this brief computerized intervention demonstrated clinically significant reductions in distress. Future research is needed to examine the mechanisms of action for such training, particularly within a larger and more diverse sample.
Highlights.
A novel cognitive training program (HIC) and control program (LIC) were tested
The HIC program improved cognition and re-experiencing symptoms, relative to the LIC program
Both groups showed reductions in general distress symptoms
Acknowledgments
This work was supported by a grant from the National Institute of Mental Health (F31 MH0881704; J. Bomyea). The authors thank Dr. Nader Amir for his consultation on training program development. We also thank Aimee Chabot, Haddas Elisha, and Raquel Good for their assistance with data collection.
Footnotes
Components of executive functioning utilized to regulate cognition have taken a variety of names based on different theoretical models (e.g., attention control, central executive, cognitive control; see Wessel, Overwijk, Verwoerd, & de Vrieze, 2008). The construct of interference control can be considered a type of inhibition; however, inhibition is multifaceted and may refer to inhibition of pre-potent responses, inhibition of interference from other cognitions or memories, or inhibition of interference from distractors. A thorough review of models (and controversies) related to executive functioning, inhibition and interference control is beyond the scope of this paper (see for example Friedman and Miyake, 2004).
We thank an anonymous reviewer for his or her thoughts on how to best conceptualize cognitive training effects.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jessica Bomyea, Email: jbomyea@ucsd.edu.
Murray B. Stein, Email: mstein@ucsd.edu.
Ariel J. Lang, Email: ajlang@ucsd.edu.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Beard C, Taylor CT, Klumpp H, Elias J, Burns M, Chen X. Attention training in individuals with generalized social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2009;77:961–973. doi: 10.1037/a0016685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Taylor CT. Interpretation training in individuals with generalized social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2012;80:497–511. doi: 10.1037/a0026928. http://dx.doi.org/10.1037/a0026928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson MC, Levy BJ. Suppressing unwanted memories. Current Directions in Psychological Science. 2008;18:189–194. doi: 10.1111/j.1467-8721.2009.01634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aupperle RL, Melrose AJ, Stein MB, Paulus MP. Executive function and PTSD: Disengaging from trauma. Neuropharmacology. 2012;62:686–694. doi: 10.1016/j.neuropharm.2011.02.008. http://dx.doi.org/10.1016/j.neuropharm.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beard C. Cognitive bias modification for anxiety: current evidence and future directions. Expert Reviews in Neurotherapy. 2011;11:299–311. doi: 10.1586/ern.10.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Bomyea J, Amir N. The effect of an executive functioning training program on working memory capacity and intrusive thoughts. Cognitive Therapy and Research. 2011;35:529–535. doi: 10.1007/s10608-011-9369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bomyea J, Lang AJ, Amir N. The relationship between cognitive control and posttraumatic stress symptoms. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:844–848. doi: 10.1016/j.jbtep.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy & Experimental Psychiatry. 1972;3:257–260. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM. The development of clinician -administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–89. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Beaton A. Thought suppression, intelligence, and working memory capacity. Behaviour Research and Therapy. 2002;40:923–930. doi: 10.1016/S0005-7967(01)00127-9. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Smart L. Working memory capacity and suppression of intrusive thoughts. Journal of Behavior Therapy and Experimental Psychiatry. 2005;36:61–68. doi: 10.1016/j.jbtep.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Bunting M. Proactive interference and item similarity in working memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 2006;32:183–196. doi: 10.1037/0278-7393.32.2.183. [DOI] [PubMed] [Google Scholar]
- Buschkuehl M, Jaeggi SM, Hutchison S, Perrig-Chiello P, Däpp C, Müller M, Breil F, Perrig WJ. Impact of working memory training on memory performance in old-old adults. Psychology and Aging. 2008;23:743–753. doi: 10.1037/a0014342. [DOI] [PubMed] [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic; 1988. [Google Scholar]
- Conway ARA, Kane MJ, Bunting MF, Hambrick DZ, Wilhelm O, Engle RW. Working memory span tasks: A methodological review and user’s guide. Psychonomic Bulletin & Review Special Issue: Memory Strength and Recency Judgments. 2005;12:769–786. doi: 10.3758/bf03196772. [DOI] [PubMed] [Google Scholar]
- Daneman M, Carpenter PA. Individual differences in working memory and reading. Journal of Verbal Learning & Verbal Behavior. 1980;19:450–466. doi: 10.1016/S0022-5371(80)90312-6. [DOI] [Google Scholar]
- Dickinson D, Tenhula W, Morris S, Brown C, Peer J, Spencer K, Bellack AS. A randomized, controlled trial of computer-assisted cognitive remediation for schizophrenia. The American Journal of Psychiatry. 2010;167:170–180. doi: 10.1176/appi.ajp.2009.09020264. [DOI] [PubMed] [Google Scholar]
- Etkin A, Wager TD. Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. The American Journal of Psychiatry. 2007;164:1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-patient edition (SCID-I/P, version 2.0) New York: Biometrics Research Department; 1994. [Google Scholar]
- Fox LS, Knight BG. The effects of anxiety on attentional processes in older adults. Aging and Mental Health. 2005;9:585–593. doi: 10.1080/13607860500294282. [DOI] [PubMed] [Google Scholar]
- Friedman NP, Miyake A. The relations among inhibition and interference control functions: A latent-variable analysis. Journal of Experimental Psychology: General. 2004;133:101–135. doi: 10.1037/0096-3445.133.1.101. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychological Bulletin. 2011;137:940–958. doi: 10.1037/a0024355. [DOI] [PubMed] [Google Scholar]
- Harrison TL, Shipstead Z, Hicks KL, Hambtrick DZ, Redick TS, Engle RW. Working memory training may increase working memory capacity but not fluid intelligence. Psychological Science. 2013;25:2409–2419. doi: 10.1177/0956797613492984. [DOI] [PubMed] [Google Scholar]
- Jaeggi SM, Buschkuehl M, Jonides J, Perrig WJ. Improving fluid intelligence with training on working memory. Proceedings of the National Academy of Science. 2008;105:6829–6833. doi: 10.1073/pnas.0801268105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joormann J, Yoon KL, Siemer M. Cognition and emotion regulation. In: Kring AM, Sloan DM, editors. Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. New York, NY, US: Guilford Press; 2010. pp. 174–203. [Google Scholar]
- Keshayan MS, Vinogradov S, Rumsey J, Sherrill J, Wagner A. Cognitive training in mental disorders: update and future directions. American Journal of Psychiatry. 2014;171:510–522. doi: 10.1176/appi.ajp.2013.13081075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, Gillberg CG, Westerberg H. Computerized training of working memory in children with ADHD--A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:177–186. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Lustig C, May CP, Hasher L. Working memory span and the role of proactive interference. Journal of Experimental Psychology: General. 2001;130:199–207. doi: 10.1037/0096-3445.130.2.199. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. http://dx.doi.org/10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macleod C. Cognitive bias modification procedures in the management of mental disorders. Current Opinions in Psychiatry. 2012;25:114–120. doi: 10.1097/YCO.0b013e32834fda4a. [DOI] [PubMed] [Google Scholar]
- Macleod C, Mathews A. Cognitive bias modification approaches to anxiety. Annual Review of Clinical Psychology. 2012;8:189–217. doi: 10.1146/annurev-clinpsy-032511-143052. [DOI] [PubMed] [Google Scholar]
- Mahncke HW, Bronstone A, Merzenich MM. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Progress in Brain Research. 2006;157:81–109. doi: 10.1016/S0079-6123(06)57006-2. [DOI] [PubMed] [Google Scholar]
- May CP, Hasher L, Kane MJ. The role of interference in memory span. Memory & Cognition. 1999;27:759–767. doi: 10.3758/bf03198529. [DOI] [PubMed] [Google Scholar]
- McFarlane AC, Yehuda R, Clark CR. Biologic models of traumatic memories and post-traumatic stress disorder: The role of neural networks. Psychiatric Clinics of North America Special Issue: Recent Advances in the Study of Biological Alterations in Post-Traumatic Stress Disorder. 2002;25:253–270. doi: 10.1016/S0193-953X(01)00008-9. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Bryant RA, Ehlers A. Does early psychological intervention promote recovery from posttraumatic stress? Psychological Science in the Public Interest. 2003;4:45–79. doi: 10.1111/1529-1006.01421. [DOI] [PubMed] [Google Scholar]
- Melby-Lervâg M, Hulme C. Is working memory training effective? A meta-analytic review. Developmental Psychology. 2012;48:270–291. doi: 10.1037/a0028228. [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Morrison AC, Chein JM. Does working memory training work? The promise and challenges of enhancing cognition by training working memory. Psychonomics Bulletin Review. 2011;18:46–60. doi: 10.3758/s12423-010-0044-0. [DOI] [PubMed] [Google Scholar]
- National Center for Post Traumatic Stress Disorder. Epidemiological Facts About PTSD - A National Center for PTSD Fact Sheet. 2005 Retrieved April 1, 2005 from http://www.ncptsd.va.gov/facts/general/fs_epidemiological.html.
- Olesen PJ, Westerberg H, Klingberg T. Increased prefrontal and parietal activity after training of working memory. Nature Neuroscience. 2004;7:75–79. doi: 10.1038/nn1165. [DOI] [PubMed] [Google Scholar]
- Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: A review. Depression and Anxiety. 2009;26:1086–1109. doi: 10.1002/da.20635. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Redick TS, Shipstead Z, Harrison TL, Hicks KL, Fried DE, Hambrick DZ, Engle RW. No evidence of intelligence improvement after working memory training: A randomized, placebo-controlled study. Jouranl of Experimental Psychology: General. 2013;142:359–379. doi: 10.1037/a0029082. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress. 2005;18:607–616. doi: 10.1002/jts.20069. http://dx.doi.org/10.1002/jts.20069. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, Bernardy N. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. http://dx.doi.org/10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Schweizer S, Hampshire A, Dalglesigh T. Extending brain-training to the affective domain: Increasing executive control through emotional working memory training. PlosOne. 2011;6:1–7. doi: 10.1371/journal.pone.0024372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry: Interpersonal and Biological Processes. 2008;71:134–168. doi: 10.1521/psyc.2008.71.2.134. [DOI] [PubMed] [Google Scholar]
- Shipstead Z, Redick TS, Engle RW. Is Working Memory Training Effective? Psychological Bulletin. 2012;138:628–654. doi: 10.1037/a0027473. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Ghinassi F, Thase ME. Neurobehavioral therapies in the 21st century: Summary of an emerging field and an extended example of cognitive control training for depression. Cognitive Therapy and Research. 2007;31:235–262. doi: 10.1007/s10608-006-9118-6. [DOI] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1983. [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. The American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, Massachusetts: Allyn and Bacon; 2007. [Google Scholar]
- Unsworth N. Interference control, working memory capacity, and cognitive ability: A latent variable analysis. Intelligence. 2010;28:255–267. [Google Scholar]
- Unsworth N, Heitz RP, Schrock JC, Engle RW. An automated version of the operation span task. Behavior Research Methods. 2005;37:498–505. doi: 10.3758/bf03192720. [DOI] [PubMed] [Google Scholar]
- Van Breukelen GJP. ANCOVA versus change from baseline had more power in randomized studies and more bias in nonrandomized studies. Journal of Clinical Epidemiology. 2006;59:920–925. doi: 10.1016/j.jclinepi.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Vasterling JJ, Brailey K, Constans JI, Sutker PB. Attention and memory dysfunction in posttraumatic stress disorder. Neuropsychology. 1998;12:125–133. doi: 10.1037/0894-4105.12.1.125. [DOI] [PubMed] [Google Scholar]
- Verwoerd J, de Jong PJ, Wessel I. Low attentional control and the development of intrusive memories following a laboratory stressor. Journal of Psychopathology and Behavioral Assessment. 2008;30:291–297. doi: 10.1007/s10862-008-9080-6. [DOI] [Google Scholar]
- Verwoerd J, Wessel I, de Jong PJ. Individual differences in experiencing intrusive memories: The role of the ability to resist proactive interference. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:189–201. doi: 10.1016/j.jbtep.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Verwoerd J, Wessel I, de Jong PJ, Nieuwenhuis MMW, Huntjens RCJ. Pre-stressor interference control and intrusive memories. Cognitive Therapy and Research. 2011;35:161–170. doi: 10.1007/s10608-010-9335-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow up measurements. British Medical Journal. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinogradov S, Fisher M, de Villers-Sidani E. Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology. 2012;37:43–76. doi: 10.1038/npp.2011.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychological Assessment. 1999;11:124–133. doi: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]
- Wessel I, Overwijk S, Verwoerd J, de Vrieze N. Pre-stressor cognitive control is related to intrusive cognition of a stressful film. Behaviour Research and Therapy. 2008;46:496–513. doi: 10.1016/j.brat.2008.01.016. [DOI] [PubMed] [Google Scholar]