1.1 Introduction
Cancers of the oral cavity and pharynx (International Classification of Diseases, 10th edition codes: C00–C14) constitute a serious, global public health concern. These anatomically-related cancers are collectively the sixth most common type of cancer worldwide (1). In 2008, there were an estimated 260,000 oral cavity and 136,000 pharyngeal incident cancer cases globally, with approximately two-thirds occurring in developing countries (2). In the United States (U.S.), it is estimated that 41,380 persons were newly diagnosed and 7,890 died from these cancers in 2013 (3).
The anatomic location of these cancers largely influences their associated risk factors, treatment options, and related epidemiologic characteristics (4). The head and neck region consists of the oral cavity, pharynx, larynx, nasal cavity, and paranasal sinuses (5). The term “oral cavity” generally refers to the lips, anterior 2/3 of the tongue, buccal and labial mucosa, gingiva, hard palate, retromolar pad, and floor of the mouth (5). The pharynx is comprised of the nasopharynx, hypopharynx, and oropharynx with the term “oropharynx” generally referring to the posterior 1/3 of the tongue, palatine and lingual tonsils, soft palate, and the posterior pharyngeal wall (5). The vast majority (>90%) of cancers of the oral cavity and oropharynx are squamous cell carcinomas (SCCs) (2).
Tobacco and alcohol use are well-accepted and documented major risk factors for oral cavity cancers (6), however, their role as risk factors are less clear for cancers of the oropharynx (7). Over the last 30 years, oral cavity cancer incidence rates in the U.S. have decreased in conjunction with decreases in cigarette smoking and alcohol consumption (7, 8). In contrast, incidence rates for oropharyngeal cancer have been increasing over the same time period (7, 8), suggesting that other risk factors independent of the traditional ones may be at play. Indeed, human papillomavirus (HPV) has been found to be a major etiologic factor associated with oropharyngeal cancers (7–10), with recent North American studies having detected HPV in up to 80% of oropharyngeal cancers (5, 11–13), and HPV Type 16 observed in approximately 90% of HPV-positive oropharyngeal cancers (6).
Historically, African American males have had higher oral cancer incidence rates than their white counterparts (14). However, recent studies have documented changes in the distribution by race/ethnicity (15–17). A study by Brown et al. examined racial/ethnic and gender trends for oral cavity and oropharyngeal cancer incidence using SEER 9 and 13 data (1975–1991 and 1992–2008) (16). During 1992–2008, total incidence rates were found to decrease significantly for all race/ethnic-gender groups except white men, with strong declining trends observed in African Americans (16). This finding was driven by a substantial increase in oropharyngeal cancer incidence in white males, while rates for these cancers either declined or remained stable for other race/ethnic-gender groups (16).
Given these demographic shifts in incidence, the primary goal of this study is to provide a comprehensive understanding of the incidence and trends for oral cavity and oropharyngeal cancer in the U.S. by anatomic subsites and demographic factors from 2000–2010. Additionally, this study will use Poisson regression to examine differences in incidence risk by demographic factors, with particular emphasis on racial/ethnic and gender disparities. It is the authors’ hope that this study’s findings can provide dentists with epidemiologic information to be used in conjunction with their clinical experience to help them better identify patients at risk for oral cancer, and diagnose oral cancer at early stages when chances for survival are much greater (2).
2.1 Materials and Methods
2.2 Study Sample
Surveillance, Epidemiology, and End Results (SEER) cancer registries actively follow-up with and receive cancer-related data from local hospitals, physicians, and laboratories on individuals diagnosed with cancer, who are residents of the geographic area covered by the SEER registry at the time of diagnosis (18). This study used the SEER 18 registries, which provide cancer information for approximately 28% of the U.S. population from 18 geographic regions (18, 19).
SEER*Stat software (version 8.1.5) was used to access publically available, de-identified data from the National Cancer Institute’s SEER program (20). Oral cancer cases diagnosed during the 2000–2010 time period were included for analysis. International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) codes were used to identify cases by anatomic subsite (21). The anatomic subsite classification was based primarily on a scheme used by Chartuvedi et al., and the cancers were further grouped into oral cavity (OC) and oropharyngeal (OP) regions (8).
The following anatomic sites were examined in the OC region: Lip (ICD-O-3 codes: C000–C009), Oral Tongue (C020–023, C028–029), Floor of Mouth (C040–049), and Gums/Hard Palate/Other sites (C030–C039, C050, C058–C059, C060–C069). The OP region included the following anatomic subsites: Base of Tongue (C019), Tonsil (C024, C090–C099), and Oropharynx [excluding base of tongue and tonsil] (C051, C052, C100–109, C142). Cancers of the Salivary glands were excluded from analysis because they tend to have a different histopathology (non-SCC) (2). A total of 75,468 incident oral cancer cases diagnosed from 2000–2010 from the SEER 18 geographic regions were used to generate frequency and incidence statistics.
2.3 Study Variables
Oral cancer cases were characterized according to: Age at diagnosis, Gender, Race/Ethnicity, and Stage at diagnosis. Age was categorized into <50 years, 50–59 years, 60–69 years, and 70+ years groups, consistent with age categories from a previous study of oral cancer SEER data (9). Race/ethnicity was created by merging a race variable (consisting of White, Black, and Other race categories) with a Hispanic ethnicity variable (consisting of Hispanic and non-Hispanic categories) to create the following categories: non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Other (which consisted of both Asian/Pacific Islanders and American Indian/Alaskan Natives due to the smaller sample size of each individual group). Finally, the stage of diagnosis variable used “SEER Historic Stage” categories: Localized, Regional, Distant, Unstaged.
2.4 Data Analysis
Cases diagnosed from 2000–2010 were characterized by the demographic variables (Section 2.3) using the Frequency Session in SEER (22). SAS Version 9.3 (SAS Institute, Inc., Cary, NC) was used to perform chi-square tests to compare the distribution of the demographic factors for cases diagnosed in the OC region and the OP region. The level of statistical significance used was P ≤ 0.05.
Cumulative, age-standardized incidence rates per 100,000 for 2000–2010 time period were generated in Rate Session in SEER (22). The 2000 U.S. standard population was used for age-standardization. Associated 95% confidence intervals (CIs) were also generated using the Tiwari et al., 2006 modification for CIs (23). SEER generated these rates by summing the incidence proportions for each individual year (2000–2010), and then age-standardizing. The incidence proportion for each individual year was the case count divided by the population for that year. The case count information was obtained from the SEER 18 cancer registries, while the corresponding population information for the SEER 18 registry regions was obtained through U.S. Census figures from the U.S. Census Bureau (24). Rates were displayed as cases per 100,000, rounded to the nearest tenth decimal place.
Cumulative, age-standardized incidence rates and 95% CIs were displayed for Total OC and OP cancer, individual anatomic subsites, and OC and OP regions by the demographic factors. Incidence rates were plotted over the time period by anatomic subsite, anatomic region, and race/ethnicity-gender groups.
Poisson multivariate regression analysis was used to determine the independent association between demographic covariates and incidence for OC and OP cancer during the time period. Count and population figures obtained from SEER were used to conduct the regression analysis using SAS version 9.3. Crude and fully adjusted incidence proportion ratios (IPRs) and 95% CIs were determined for age, gender, race/ethnicity, and stage at diagnosis categories, as compared to a reference category in each covariate. This study was reviewed and approved by the National Institutes of Health Institutional Review Board.
3.1 Results
Frequencies for incident oral cancer cases diagnosed from 2000–2010 in total, and by OC and OP regions are displayed by demographics characteristics in Table 1. Of the total cases diagnosed (N=75,468), the tonsil was the most frequently diagnosed anatomic subsite (23.1%) followed by base of the tongue (18.4%) and oral tongue (17.8%). The demographic profile for total oral cancer cases diagnosed was as follows: Males (69.0%), Whites (78.9%), and at the Regional (46.6%) and Localized (32.3%) stages of diagnosis. Important differences in demographic characteristics were noted between OC cancer cases and those in the OP region. The greatest proportion of cases in the OC region were diagnosed in the 70+ year age group. Conversely, the greatest proportion of cases in the OP region were diagnosed among individuals 50–59 years of age. In both regions, a substantially higher proportion of cases were diagnosed in males than females, however, this difference was greatest in the OP region. About six out of ten OP cases were diagnosed at the regional stage (60.7%) while more than half of the OC cases were diagnosed at the localized stage (51.2%). The distributions for all demographic factors differed significantly between cases in the OC and OP (P< .0001).
Table 1.
Comparison of oral cavity and oropharyngeal cancer cases by demographic factors and anatomic region: 2000–2010 (SEER 18)
| Demographic factor | Total cases (N= 75,468) n (%) |
Oral cavity region a (n=38,016) n (%) |
Oropharyngeal b region (n=37,452) n (%) |
P-value c |
|---|---|---|---|---|
| Age at diagnosis (yrs.) | <.0001 | |||
| <50 | 12,615 (16.7) | 6,074 (16.0) | 6,541 (17.5) | |
| 50–59 | 20,306 (26.9) | 8,030 (21.1) | 12,276 (32.8) | |
| 60–69 | 18,910 (25.1) | 8,745 (23.0) | 10,165 (27.1) | |
| 70+ | 23,637 (31.3) | 15,167 (39.9) | 8,470 (22.6) | |
| Gender | <.0001 | |||
| Male | 52,063 (69.0) | 23,128 (60.8) | 28,935 (77.3) | |
| Female | 23,405 (31.0) | 14,888 (39.2) | 8,517 (22.7) | |
| Race/Ethnicity | <.0001 | |||
| non-Hispanic, White | 59,512 (78.9) | 30,119 (79.2) | 29,393 (78.5) | |
| non-Hispanic, Black | 6,626 (8.8) | 2,591 (6.8) | 4,035 (10.8) | |
| Hispanic d | 4,995 (6.6) | 2,557 (6.7) | 2,438 (6.5) | |
| non-Hispanic, Other e | 3,474 (4.6) | 2,133 (5.6) | 1,341 (3.6) | |
| Unknown | 861 (1.1) | 616 (1.6) | 245 (0.7) | |
| Stage at diagnosis | <.0001 | |||
| Localized | 24,373 (32.3) | 19,481 (51.2) | 4,892 (13.1) | |
| Regional | 35,142 (46.6) | 12,417 (32.7) | 22,725 (60.7) | |
| Distant | 8,199 (10.9) | 2,592 (6.8) | 5,607 (15.0) | |
| Unstaged | 7,754 (10.3) | 3,526 (9.3) | 4,228 (11.3) | |
| Anatomic subsite | N/A | |||
| Lip | 6,834 (9.1) | 6,834 (18.0) | -- | |
| Oral Tongue | 13,400 (17.8) | 13,400 (35.3) | -- | |
| Floor of Mouth | 5,801 (7.7) | 5,801 (15.3) | -- | |
| Gums/Palate/Other | 11,981 (15.9) | 11,981 (31.5) | -- | |
| Base of Tongue | 13,893 (18.4) | -- | 13,893 (37.1) | |
| Tonsil | 17,425 (23.1) | -- | 17,425 (46.5) | |
| Oropharynx | 6,134 (8.1) | -- | 6,134 (16.4) |
Oral cavity region: lip (C000–C009), oral tongue (C020–023, C028–029), floor of mouth (C040–049), gums/palate/other mouth (C030–C039, C050–C059, C060–C069).
Oropharyngeal region: base of tongue (C019), tonsil (C024, C090–C099), oropharynx (C051, C052, C100–109, C142).
Chi-square P-value to test independent association between demographic factors and anatomic region calculated using SAS v 9.3 (SAS Institute, Inc., Cary, NC.)
Hispanic ethnicity consists of all Hispanics (regardless of race)
Other race/ethnicity group consists of non-Hispanic Asian/Pacific Islanders and American Indian/Alaska Natives.
Because incidence could not be calculated for Insurance and Marriage variables in SEER, they were not included in the analysis.
Table 2 shows the cumulative, age-standardized incidence rates per 100,000 (2000–2010) for Total OC and OP cancer, and anatomic subsites by demographic characteristics. The overall, age-standardized cumulative incidence rate for Total OC and OP cancer during the study period was 8.4 cases per 100,000 (95% CI: 8.3, 8.4); with the tonsil displaying the highest individual rate (1.9/100,000; 95% CI: 1.9,1.9 ), followed by the base of tongue and oral tongue subsites. In the OC subsites, incidence tended to be highest among the oldest age category, however; in the base of tongue and tonsil, the 60–69 year age group displayed the highest incidence. Males had a higher incidence than females in each of the anatomic subsites. Whites had the highest overall rate of Total OC and OP cancer, with white males (14.1/100,000; 95% CI:14.0, 14.2) showing the highest rate among all race/ethnicity-gender groups.
Table 2.
Cumulative age-standardized a incidence rates (per 100,000) for Total OC and OP cancer and anatomic subsites by demographic factors: 2000–2010 (SEER 18)
| Demographic Factor | Total OC and OP Cancer | Lip | Oral Tongue | Floor of Mouth | Gums/Pa late/Other | Base of Tongue | Tonsil | Oropharynx |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | |
|
| ||||||||
| Total Incidence | 8.4 (8.3, 8.4) | 0.8 (0.8, 0.8) | 1.5 (1.5, 1.5) | 0.6 (0.6, 0.7) | 1.4 (1.3, 1.4) | 1.5 (1.5, 1.5) | 1.9 (1.9, 1.9) | 0.7 (0.7, 0.7) |
|
| ||||||||
| Age at diagnosis (yrs.) | ||||||||
| <50 | 2.0 (1.9, 2.0) | 0.2 (0.1, 0.2) | 0.4 (0.4, 0.4) | 0.1 (0.1, 0.1) | 0.3 (0.3, 0.3) | 0.3 (0.3, 0.3) | 0.6 (0.6, 0.6) | 0.1 (0.1, 0.1) |
| 50–59 | 18.2 (17.9, 18.4) | 1.0 (1.0, 1.1) | 2.9 (2.8, 3.0) | 1.5 (1.4, 1.5) | 1.8 (1.7, 1.9) | 3.9 (3.8, 4.0) | 5.6 (5.5, 5.7) | 1.5 (1.5, 1.6) |
| 60–69 | 27.6 (27.2, 28.0) | 2.0 (1.9, 2.2) | 4.5 (4.3, 4.7) | 2.5 (2.4, 2.6) | 3.8 (3.6, 3.9) | 6.1 (5.9, 6.2) | 6.2 (6.0, 6.4) | 2.5 (2.4, 2.7) |
| 70+ | 31.7 (31.3, 32.2) | 4.4 (4.3, 4.6) | 5.9 (5.7, 6.1) | 2.4 (2.3, 2.5) | 7.5 (7.4, 7.7) | 4.8 (4.7, 5.0) | 4.2 (4.0, 4.3) | 2.5 (2.3, 2.6) |
|
| ||||||||
| Gender | ||||||||
| Male | 12.5 (12.4, 12.6) | 1.3(1.3, 1.4) | 1.9(1.9, 1.9) | 1.0 (0.9, 1.0) | 1.6 (1.5, 1.6) | 2.6 (2.5, 2.6) | 3.1 (3.1, 3.2) | 1.0 (1.0, 1.1) |
| Female | 4.8 (4.7, 4.9) | 0.4(0.3, 0.4) | 1.1(1.1, 1.2) | 0.4 (0.4, 0.4) | 1.2 (1.1, 1.2) | 0.6 (0.6, 0.6) | 0.8 (0.8, 0.8) | 0.4 (0.4, 0.4) |
|
| ||||||||
| Race/Ethnicity | ||||||||
| non-Hispanic, White | 9.5 (9.4, 9.5) | 1.0 (0.9, 1.0) | 1.7 (1.6, 1.7) | 0.7 (0.7, 0.7) | 1.4 (1.4, 1.5) | 1.8 (1.8, 1.8) | 2.2 (2.1, 2.2) | 0.7 (0.7, 0.7) |
| non-Hispanic, Black | 7.5 (7.3, 7.6) | 0.1 (0.1, 0.1) | 0.9 (0.9, 1.0) | 0.7 (0.7, 0.8) | 1.2 (1.2, 1.3) | 1.4 (1.3, 1.5) | 1.9 (1.8, 2.0) | 1.2 (1.1, 1.2) |
| Hispanic | 5.0 (4.9, 5.2) | 0.4 (0.4, 0.4) | 0.9 (0.9, 1.0) | 0.4 (0.3, 0.4) | 1.0 (0.9, 1.0) | 0.8 (0.7, 0.8) | 1.2 (1.1, 1.3) | 0.4 (0.4, 0.5) |
| non-Hispanic Other | 4.4 (4.3, 4.6) | 0.1 (0.1, 0.2) | 1.3 (1.2, 1.4) | 0.3 (0.2, 0.3) | 1.0 (0.9, 1.1) | 0.5 (0.5, 0.6) | 0.9 (0.8, 0.9) | 0.3 (0.2, 0.3) |
|
| ||||||||
| Race/Ethnicity-Gender | ||||||||
| NHW Males | 14.1 (14.0,14.2) | 1.6 (1.6, 1.7) | 2.1 (2.1, 2.2) | 1.0 (1.0, 1.1) | 1.7 (1.6, 1.7) | 3.0 (3.0, 3.1) | 3.5 (3.5, 3.6) | 1.0 (1.0, 1.1) |
| NHW Females | 5.3 (5.2,5.4) | 0.4 (0.4, 0.5) | 1.3 (1.2, 1.3) | 0.4 (0.4, 0.4) | 1.2 (1.2, 1.3) | 0.7 (0.6, 0.7) | 0.9 (0.8, 0.9) | 0.4 (0.4, 0.4) |
| NHB Males | 11.9 (11.5,12.3) | 0.1 (0.1, 0.2) | 1.4 (1.2, 1.5) | 1.2 (1.1, 1.3) | 1.5 (1.3, 1.6) | 2.4 (2.3, 2.6) | 3.4 (3.2, 3.6) | 1.9 (1.8, 2.1) |
| NHB Females | 4.0 (3.8,4.2) | 0.1 (0.1, 0.1) | 0.6 (0.5, 0.7) | 0.3 (0.3, 0.4) | 1.0 (1.0, 1.1) | 0.6 (0.6, 0.7) | 0.7 (0.7, 0.8) | 0.6 (0.5, 0.6) |
| Hispanic Males | 7.2 (6.9,7.4) | 0.7 (0.6, 0.8) | 1.1 (1.0, 1.2) | 0.5 (0.5, 0.6) | 1.0 (0.9, 1.2) | 1.2 (1.1, 1.3) | 1.9 (1.8, 2.0) | 0.7 (0.6, 0.8) |
| Hispanic Females | 3.2 (3.0, 3.4) | 0.2 (0.2, 0.2) | 0.8 (0.7, 0.9) | 0.2 (0.2, 0.2) | 0.9 (0.8, 1.0) | 0.4 (0.3, 0.4) | 0.6 (0.5, 0.6) | 0.2 (0.2, 0.3) |
| NH Other Males | 6.0 (5.7, 6.2) | 0.2 (0.1, 0.2) | 1.6 (1.4, 1.7) | 0.4 (0.3, 0.5) | 1.2 (1.1, 1.3) | 0.9 (0.8, 1.0) | 1.3 (1.2, 1.5) | 0.4 (0.3, 0.5) |
| NH Other Females | 3.1 (3.0, 3.3) | 0.1 (0.1, 0.1) | 1.1 (1.0, 1.2) | 0.2 (0.1, 0.2) | 0.8 (0.8, 0.9 | 0.3 (0.2, 0.3) | 0.5 (0.4, 0.5) | 0.2 (0.1, 0.2) |
| Stage at diagnosis | ||||||||
| Localized | 2.7 (2.7, 2.8) | 0.6 (0.6, 0.6) | 0.9 (0.8, 0.9) | 0.3 (0.2, 0.3) | 0.5 (0.5, 0.5) | 0.2 (0.2, 0.2) | 0.2 (0.2, 0.2) | 0.2 (0.2, 0.2) |
| Regional | 3.9 (3.8, 3.9) | 0.1 (0.1, 0.1) | 0.4 (0.4, 0.4) | 0.3 (0.3, 0.3) | 0.6 (0.6, 0.6) | 1.0 (1.0, 1.0) | 1.2 (1.1, 1.2) | 0.3 (0.3, 0.3) |
| Distant | 0.9 (0.9, 0.9) | 0.0 (0.0, 0.0) | 0.1 (0.1, 0.2) | 0.0 (0.0, 0.0) | 0.1 (0.1, 0.1) | 0.3 (0.3, 0.3) | 0.2 (0.2, 0.2) | 0.1 (0.1, 0.1) |
| Unstaged | 0.9 (0.9, 0.9) | 0.1 (0.0, 0.1) | 0.1 (0.1, 0.1) | 0.0 (0.0, 0.0) | 0.2 (0.2, 0.2) | 0.1 (0.1, 0.1) | 0.3 (0.3, 0.3) | 0.1 (0.1, 0.1) |
Age standardized to 2000 U.S. standard population
NH- Non-Hispanic; NHW- Non-Hispanic White; NWB- Non-Hispanic Black
Table 3 summarizes the age-adjusted incidence rates by anatomic region. Higher rates were seen in the 50–59 and 60–69 year age groups in the OP region compared to the OC region, while a higher rate was observed in the 70+ age group in the OC region compared to the OP region. In the OC region, incidence was greatest in the localized stage, while regional cancers displayed the highest incidence in the OP region.
Table 3.
Cumulative age-standardized a incidence rates (per 100,000) for Total OC and OP cancer and anatomic region by demographic factors: 2000–2010 (SEER 18)
| Demographic Factor | Total OC and OP Cancer | Oral Cavity Region | Oropharyngeal Region |
|---|---|---|---|
|
| |||
| Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | |
|
| |||
| Total Incidence | 8.4 (8.3, 8.4) | 4.3 (4.2, 4.3) | 4.1 (4.0, 4.1) |
|
| |||
| Age at diagnosis (yrs.) | |||
| <50 | 2.0 (1.9, 2.0) | 0.9 (0.9, 1.0) | 1.0 (1.0, 1.0) |
| 50–59 | 18.2 (17.9, 18.4) | 7.2 (7.0, 7.3) | 11.0 (10.8, 11.2) |
| 60–69 | 27.6 (27.2, 28.0) | 12.8 (12.5, 13.1) | 14.8 (14.5, 15.1) |
| 70+ | 31.7 (31.3, 32.2) | 20.3 (19.9, 20.6) | 11.5 (11.3, 11.7) |
|
| |||
| Gender | |||
| Male | 12.5 (12.4, 12.6) | 5.8 (5.7, 5.8) | 6.7 (6.6, 6.8) |
| Female | 4.8 (4.7, 4.9) | 3.0 (3.0, 3.1) | 1.8 (1.7, 1.8) |
|
| |||
| Race/Ethnicity | |||
| non-Hispanic, White | 9.5 (9.4, 9.5) | 4.8 (4.8, 4.9) | 4.7 (4.6, 4.7) |
| non-Hispanic, Black | 7.5 (7.3, 7.6) | 3.0 (2.9, 3.1) | 4.5 (4.3, 4.6) |
| Hispanic | 5.0 (4.9, 5.2) | 2.7 (2.5, 2.8) | 2.4 (2.3, 2.5) |
| non-Hispanic Other | 4.4 (4.3, 4.6) | 2.7 (2.6, 2.9) | 1.7 (1.6, 1.8) |
|
| |||
| Race/Ethnicity-Gender | |||
| NHW Males | 14.1 (14.0, 14.2) | 6.4 (6.4, 6.6) | 7.6 (7.5, 7.7) |
| NHW Females | 5.3 (5.2, 5.4) | 3.4 (3.3, 3.4) | 1.9 (1.9, 2.0) |
| NHB Males | 11.9 (11.5, 12.3) | 4.2 (4.0, 4.4) | 7.7 (7.4, 8.0) |
| NHB Females | 4.0 (3.8, 4.2) | 2.1 (1.9, 2.2) | 1.9 (1.8, 2.1) |
| Hispanic Males | 7.2 (6.9, 7.4) | 3.4 (3.2, 3.6) | 3.8 (3.6, 4.0) |
| Hispanic Females | 3.2 (3.0, 3.4) | 2.1 (1.9, 2.2) | 1.1 (1.0, 1.2) |
| Other Males | 6.0 (5.7, 6.2) | 3.3 (3.1, 3.5) | 2.6 (2.5, 2.8) |
| Other Females | 3.1 (3.0, 3.3) | 2.3 (2.1, 2.4) | 0.9 (0.8, 1.0) |
|
| |||
| Stage at diagnosis | |||
| Localized | 2.7 (2.7, 2.8) | 2.2 (2.2, 2.2) | 0.5 (0.5, 0.6) |
| Regional | 3.9 (3.8, 3.9) | 1.4 (1.4, 1.4) | 2.5 (2.4, 2.5) |
| Distant | 0.9 (0.9, 0.9) | 0.3 (0.3, 0.3) | 0.6 (0.6, 0.6) |
| Unstaged | 0.9 (0.9, 0.9) | 0.4 (0.4, 0.4) | 0.5 (0.5, 0.5) |
Age standardized to 2000 U.S. standard population
NH- Non-Hispanic; NHW- Non-Hispanic White; NWB- Non-Hispanic Black
Observing the age-standardized incidence trends by anatomic sites over time (Figure 1), the tonsil displayed the strongest positive trend, followed by the base of tongue; while other sites displayed stable or negative time trends. This translated into an increasing trend for incidence in the OP region, and a decreasing trend in the OC region during the time period examined (Figure 2). Figures 3 and 4 display race/ethnic-gender trends by OC and OP regions, respectively, over the time period. Black males showed the strongest decline in age-standardized incidence of OC cancers. White males also displayed a decline, however, it was more moderate than the decline observed in black males. In the OP region, black and white males displayed opposite trends. An increase in incidence for OP cancers was noted over time in white males, while a decline was observed in black males. All other race/ethnic–gender groups tended to display relatively stable rates over time in both regions.
Figure 1.
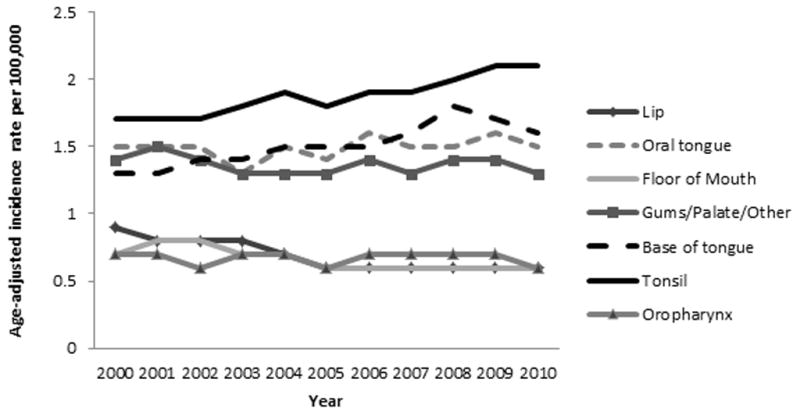
Age-standardized incidence rates by anatomic subsite (2000–2010)
Figure 2.
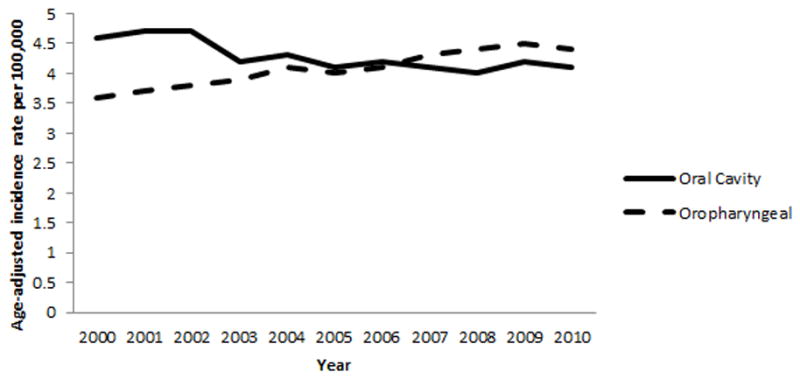
Age-standardized incidence rates by anatomic region (2000–2010)
Figure 3.
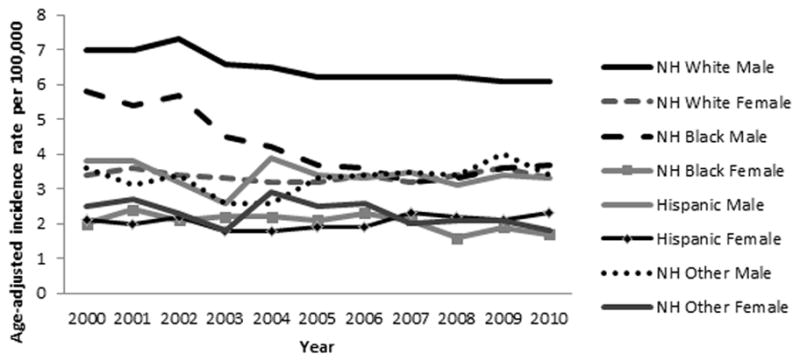
Age-standardized incidence rates by race/ethnicity-gender in oral cavity region (2000–2010)
Figure 4.
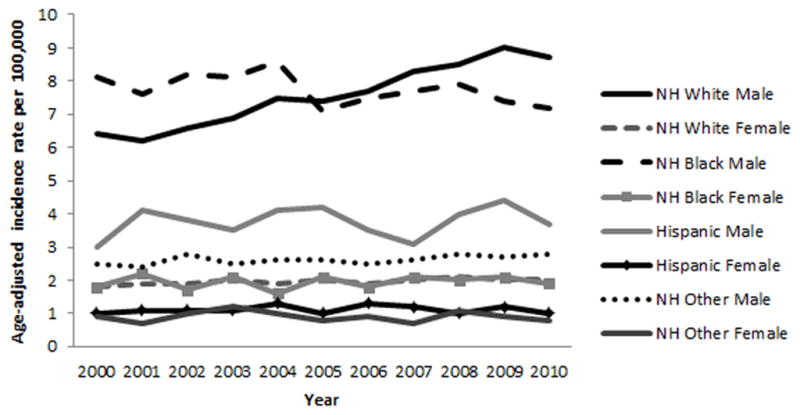
Age-standardized incidence rates by race/ethnicity-gender in oropharyngeal region (2000–2010)
Table 4 and Table 5 display the crude and fully adjusted IPRs and 95% CIs by demographic factors for OC and OP cancer, respectively. For both OC and OP, in the crude model with race/ethnicity as the only independent variable, all racial/ethnic groups displayed significantly lower risk of incidence relative to whites (reference group). In the fully adjusted models for OC and OP cancer (Tables 4 and 5), the IPRs increased for all racial/ethnic groups relative to whites, although each group still displayed a significantly lower risk relative to whites. For OC, all age groups showed a significantly higher risk of incidence relative to the youngest age group (<50, reference group) even after controlling for all other covariates, with a trend of increasing risk with age. For OP, all age groups showed a significantly higher risk of incidence relative to the youngest age group, however, the 60–69 age group showed the highest risk after controlling for all other covariates. For OC cancer, males had nearly twice the risk as compared to females in the fully adjusted model (Table 4: IPR=1.87, 95% CI: 1.83, 1.91). Males had nearly four times higher risk for OP cancer compared to females after adjusting for all other factors (Table 5: IPR=3.88, 95% CI: 3.79, 3.97). Finally, OC cancer had the greatest risk of being diagnosed at the localized stage, where OP cancer had the greatest risk of being diagnosed at the regional stage after controlling for all other factors.
Table 4.
Poisson regression models- crude and fully adjusted incidence proportion ratios (IPR) and 95% confidence intervals (CIs) for OC cancer by demographic factors: 2000–2010 (SEER 18)
| Crude IPR (95% CI) a | Fully Adjusted IPR (95% CI) b | |
|---|---|---|
| Race/Ethnicity | ||
| Non-Hispanic, White (ref) | 1.00 | 1.00 |
| Non-Hispanic, Black | 0.42 (0.41, 0.44) | 0.64 (0.61, 0.66) |
| Hispanics | 0.24 (0.23, 0.25) | 0.47 (0.45, 0.49) |
| Non-Hispanic, Other | 0.42 (0.40, 0.44) | 0.56 (0.53, 0.58) |
| Age | ||
| <50 years (ref) | 1.00 | 1.00 |
| 50–59 years | 7.77 (7.51, 8.03) | 7.21 (6.97, 7.46) |
| 60–69 years | 13.65 (13.21, 14.10) | 12.63 (12.21, 13.06) |
| 70+ years | 21.88 (21.24, 22.54) | 20.56 (19.94, 21.20) |
| Gender | ||
| Female (ref) | 1.00 | 1.00 |
| Male | 1.59 (1.56, 1.63) | 1.87 (1.83, 1.91) |
| Stage at diagnosis | ||
| Localized (ref) | 1.00 | 1.00 |
| Regional | 0.64 (0.62, 0.65) | 0.65 (0.63, 0.66) |
| Distant | 0.13 (0.13, 0.14) | 0.14 (0.13, 0.14) |
| Unstaged | 0.18 (0.17, 0.19) | 0.18 (0.17, 0.18) |
Crude model: individual demographic variable only
Fully adjusted model: contains all demographic variables in the model
Table 5.
Poisson regression models- crude and fully adjusted incidence proportion ratios (IPR) and 95% confidence intervals (CIs) for OP cancer by demographic factors: 2000–2010 (SEER 18)
| Crude IPR (95% CI) a | Fully Adjusted IPR (95% CI) b | |
|---|---|---|
| Race/Ethnicity | ||
| Non-Hispanic, White (ref) | 1.00 | 1.00 |
| Non-Hispanic, Black | 0.68 (0.66, 0.70) | 0.96 (0.93, 1.00) |
| Hispanics | 0.23 (0.22, 0.24) | 0.42 (0.40, 0.44) |
| Non-Hispanic, Other | 0.27 (0.26, 0.29) | 0.34 (0.33, 0.36) |
| Age | ||
| <50 years (ref) | 1.00 | 1.00 |
| 50–59 years | 11.03 (10.70, 11.36) | 10.31 (10.01, 10.63) |
| 60–69 years | 14.73 (14.28, 15.20) | 13.78 (13.35, 14.22) |
| 70+ years | 11.35 (10.99, 11.72) | 11.32 (10.96, 11.70) |
| Gender | ||
| Female (ref) | 1.00 | 1.00 |
| Male | 3.49 (3.40, 3.57) | 3.88 (3.79, 3.97) |
| Stage at diagnosis | ||
| Localized (ref) | 1.00 | 1.00 |
| Regional | 4.65(4.50, 4.79) | 4.66 (4.52, 4.81) |
| Distant | 1.15 (1.10, 1.19) | 1.15 (1.11, 1.20) |
| Unstaged | 0.86 (0.83, 0.90) | 0.85 (0.82, 0.89) |
Crude model: individual demographic variable only
Fully adjusted model: contains all demographic variables in the model
4.1 Discussion
This study found differences in OC and OP cancer incidence rates and trends in the U.S. during the 2000–2010 time period based on age, gender, race/ethnicity, stage at diagnosis, and anatomic subsite. Such epidemiologic findings are important for dentists, as they can potentially affect clinical examinations, patient education, and the risk profiles of persons with oral cancer.
Two distinct trend patterns were observed for OC and OP cancers. Similar to previous studies, an increase in the incidence of OP cancers in conjunction with a decrease in the incidence of OC cancers was seen over time (8, 9, 25). The increasing incidence observed in the OP region was driven by the tonsil, which was found to be the most frequently diagnosed oral cancer site and the site with the highest cumulative incidence, and the base of the tongue, the second most frequently diagnosed site. Both the tonsil and the base of the tongue displayed increasing incidence over the study period, in contrast to the trends for other anatomic sites. There has been particularly strong evidence for the association between HPV and tonsillar and base of tongue cancers (9, 26–28). While no information on the HPV status of cancers was available for the present study, given the strong association between HPV and oropharyngeal cancers (9, 26–28) dentists should be aware of the etiologic role that HPV plays in these cancers and its likely impact on the noted trends.
The decrease in OC cancer incidence over time, for which tobacco is a major risk factor, has been largely attributed to the success of public health programs aimed at reducing smoking (6). Oral health professionals can continue to contribute to lowering the incidence of these cancers by educating patients about the risk of using tobacco and alcohol products, and providing smoking cessation interventions as appropriate. It should be noted that sun exposure may play a greater etiologic role in lip cancers than smoking, particularly in portions of the external lip (29). Overall, these findings suggest that the dental community should no longer view “oral cancer” as a uniform classification of cancer, but rather should recognize that OC and OP cancers are two epidemiologically-distinct forms, typically with different major etiologies (2, 8, 9, 15, 16, 25).
In contrast to the well-documented, historical finding of highest oral cancer incidence in black males (14), this study found that white males had the highest overall incidence among all race/ethnicity- gender groups between 2000–2010. Declining trends for both oral cavity and OP cancers were observed among black males, in contrast to an increasing trend of OP cancer incidence in white males. Oral sexual behavior is considered to be a primary predictor of oral HPV16 infection (25, 30). While the exact cause of the increasing incidence of OP cancer in white males is unknown, an increase in oral sexual behavior in white males over time has been hypothesized to be driving this trend, as studies have shown that white males demonstrate greater levels of oral sexual behaviors associated with oral HPV16 and OP cancer as compared to other racial/ethnic- gender groups, and that these behaviors have increased over time (30–32). Although whites were found to have a highest risk of OC and OP cancer incidence relative to other racial/ethnic groups, the Poisson regression model showed that adjusting for other factors reduced the racial/ethnic differences in incidence risk. Future population-based studies examining oral cancer should consider collecting a wide range of socio-demographic variables and risk factors to determine if these factors can explain observed racial/ethnic and gender differences in oral cancer incidence.
Finally, a distinct difference in incidence was seen based on the age of diagnosis for OC cancers compared to OP cancers. The 50–59 and 60–69 age groups had a substantially higher risk for cancer in the OP region compared to the OC region. While in the OC region, the oldest age group (70+) displayed the highest risk. This finding of higher incidence in younger age groups in the OP region is in agreement with previous research (5).
4.2 Limitations
The major study limitation was the lack of information on major risk factors such as tobacco/alcohol use and HPV status of the cancers in the publically-available SEER data. Adjusting for available demographic factors in the Poisson regression model helped to explain much of the racial/ethnic differences in incidence risk, and it is likely that other risk factor information could have further explained observed risk differences (i.e. gender differences). Despite these limitations, this large dataset allowed for the characterization of important epidemiologic trends.
4.3 Conclusion
Results of this study are in alignment with and extend previous findings related to oral cancer trends (15, 16), using the most recently available SEER data when the study was initiated. The increasing incidence of cancers in the OP region suggest that oral health professionals should be particularly attentive to the portions of these posterior anatomic structures that they are able to visualize on clinical examination, in addition to anterior anatomic structures in the OC that are more visibly accessible. The distinct epidemiologic trends of OC and OP cancers dictate that oral cancer can no longer be viewed as a discrete entity. Additionally, oral health providers should be aware of the epidemiologic trends and risk factors associated with OC and OP cancers, so they can properly address potential questions that patients may have related to oral cancers and educate their patients accordingly.
Highlights.
The age-standardized cumulative incidence rate for oral cancers from 2000–2010 was 8.4 cases per 100,000.
The tonsil was the most frequently diagnosed oral cancer site, and the site with the greatest incidence from 2000–2010.
Cancers of the oral cavity showed a decreasing trend for incidence from 2000–2010.
Cancers of the oropharyngeal region showed an increasing trend for incidence from 2000–2010.
Racial/ethnic and gender disparities exist for oral cancers.
Acknowledgments
This study was supported by the National Institute of Dental and Craniofacial Research. The authors thank Drs. Margo Adesanya and Timothy Iafolla, National Institute of Dental and Craniofacial Research, for their comments and suggestions as well as Dr. Linda Morris Brown, RTI International and Dr. Lynn Ries, National Cancer Institute, for their input related to SEER data.
Footnotes
Disclaimer
The opinions expressed are those of the authors and do not necessarily reflect the views of the National Institute of Dental and Craniofacial Research, the National Institutes of Health, or the United States Government.
Conflict of Interest Statement
Conflicts of interest: none.
Author Contributions
Darien Weatherspoon- Acquisition of data; Concept and design; Analysis and interpretation of data; Drafting of manuscript; Editing of manuscript
Amit Chattopadhyay- Concept and design; Analysis and interpretation of data; Editing of manuscript
Shadi Boroumand- Concept and design; Editing of manuscript
A. Isabel Garcia- Concept and design; Editing of manuscript
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Darien J. Weatherspoon, Email: dweath3@uic.edu, Assistant Professor, University of Illinois at Chicago College of Dentistry, MC 621, Department of Pediatric Dentistry, Division of Prevention and Public Health Sciences, 801 S. Paulina St., Room 204-C, Chicago, IL, USA 60612, 312-996-3465.
Amit Chattopadhyay, Email: Amit.Chattopadhyay@dhcc.ae, Professor of Public Health & Consultant, Dubai Healthcare City Education Division, P.O. Box 66566, Dubai, United Arab Emirates.
Shahdokht Boroumand, Email: boroumands@mail.nih.gov, Dental Public Health Consultant, National Institute of Dental and Craniofacial Research, Bethesda, MD, USA 20892.
A. Isabel Garcia, Email: agarcia2@dental.ufl.edu, Dean, College of Dentistry, University of Florida, 1395 Center Drive, D4-6B, PO Box 100405, Gainesville, FL 32610-0405.
References
- 1.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4–5):309–16. doi: 10.1016/j.oraloncology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Lambert R, Sauvaget C, de Camargo Cancela M, Sankaranarayanan R. Epidemiology of cancer from the oral cavity and oropharynx. Eur J Gastroenterol Hepatol. 2011;23(8):633–41. doi: 10.1097/MEG.0b013e3283484795. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Institute. SEER Cancer Statistics Factsheets: Oral Cavity and Pharynx Cancer. [Accessed February 2014]; Available from: http://seer.cancer.gov/statfacts/html/oralcav.html.
- 4.Moore SR, Pierce AM, Wilson DF. ‘Oral cancer’--the terminology dilemma. Oral Dis. 2000;6(3):191–3. [PubMed] [Google Scholar]
- 5.Cleveland JL, Junger ML, Saraiya M, Markowitz LE, Dunne EF, Epstein JB. The connection between human papillomavirus and oropharyngeal squamous cell carcinomas in the United States: implications for dentistry. J Am Dent Assoc. 2011;142(8):915–24. doi: 10.14219/jada.archive.2011.0298. [DOI] [PubMed] [Google Scholar]
- 6.Radoi L, Luce D. A review of risk factors for oral cavity cancer: the importance of a standardized case definition. Community Dent Oral Epidemiol. 2013;41(2):97–109. e78–91. doi: 10.1111/j.1600-0528.2012.00710.x. [DOI] [PubMed] [Google Scholar]
- 7.Sturgis EM, Cinciripini PM. Trends in head and neck cancer incidence in relation to smoking prevalence: an emerging epidemic of human papillomavirus-associated cancers? Cancer. 2007;110(7):1429–35. doi: 10.1002/cncr.22963. [DOI] [PubMed] [Google Scholar]
- 8.Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26(4):612–9. doi: 10.1200/JCO.2007.14.1713. [DOI] [PubMed] [Google Scholar]
- 9.Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–301. doi: 10.1200/JCO.2011.36.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356(19):1944–56. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 11.Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14(2):467–75. doi: 10.1158/1055-9965.EPI-04-0551. [DOI] [PubMed] [Google Scholar]
- 12.Scudellari M. HPV: Sex, cancer and a virus. Nature. 2013;503(7476):330–2. doi: 10.1038/503330a. [DOI] [PubMed] [Google Scholar]
- 13.Singhi AD, Westra WH. Comparison of human papillomavirus in situ hybridization and p16 immunohistochemistry in the detection of human papillomavirus-associated head and neck cancer based on a prospective clinical experience. Cancer. 2010;116(9):2166–73. doi: 10.1002/cncr.25033. [DOI] [PubMed] [Google Scholar]
- 14.Walker B, Figgs LW, Zahm SH. Differences in cancer incidence, mortality, and survival between African Americans and whites. Environ Health Perspect. 1995;103 (Suppl 8):275–81. doi: 10.1289/ehp.95103s8275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown LM, Check DP, Devesa SS. Oropharyngeal cancer incidence trends: diminishing racial disparities. Cancer Causes Control. 2011;22(5):753–63. doi: 10.1007/s10552-011-9748-1. [DOI] [PubMed] [Google Scholar]
- 16.Brown LM, Check DP, Devesa SS. Oral cavity and pharynx cancer incidence trends by subsite in the United States: changing gender patterns. J Oncol. 2012;2012:649498. doi: 10.1155/2012/649498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howlader N, Noone AM, Krapcho M, Garshell J, Neyman N, Altekruse SF, et al. SEER Cancer Statistics Review, 1975–2010. National Cancer Institute; Bethesda, MD: 2013. [Google Scholar]
- 18.Data Flow in NCI’s SEER Registries. National Cancer Institute; Bethesda, MD: [Accessed February 2014]. Available from: http://seer.cancer.gov/about/factsheets/SEER_Data_Flow_.pdf. [Google Scholar]
- 19.SEER Registry Groupings for Analyses. National Cancer Institute; Bethesda, MD: [Accessed February 2014]. Available from: http://seer.cancer.gov/registries/terms.html. [Google Scholar]
- 20.National Cancer Institute. SEER*Stat software Version 8.1.2. 2013. Surveillance Research Program. [Google Scholar]
- 21.ICD-O-3 Site Codes. National Cancer Institute; Bethesda, MD: [Accessed February 2014]. Available from: http://training.seer.cancer.gov/head-neck/abstract-code-stage/codes.html. [Google Scholar]
- 22.Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2013 Sub (2000–2011) 2014. [Google Scholar]
- 23.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Statistical methods in medical research. 2006;15(6):547–69. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 24.The U.S. Census Bureau. [Accessed February 2014]; Available from: http://www.census.gov/
- 25.Ryerson AB, Peters ES, Coughlin SS, Chen VW, Gillison ML, Reichman ME, et al. Burden of potentially human papillomavirus-associated cancers of the oropharynx and oral cavity in the US, 1998–2003. Cancer. 2008;113(10 Suppl):2901–9. doi: 10.1002/cncr.23745. [DOI] [PubMed] [Google Scholar]
- 26.Hammarstedt L, Lindquist D, Dahlstrand H, Romanitan M, Dahlgren LO, Joneberg J, et al. Human papillomavirus as a risk factor for the increase in incidence of tonsillar cancer. Int J Cancer. 2006;119(11):2620–3. doi: 10.1002/ijc.22177. [DOI] [PubMed] [Google Scholar]
- 27.Nasman A, Attner P, Hammarstedt L, Du J, Eriksson M, Giraud G, et al. Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int J Cancer. 2009;125(2):362–6. doi: 10.1002/ijc.24339. [DOI] [PubMed] [Google Scholar]
- 28.Ramqvist T, Dalianis T. An epidemic of oropharyngeal squamous cell carcinoma (OSCC) due to human papillomavirus (HPV) infection and aspects of treatment and prevention. Anticancer Res. 2011;31(5):1515–9. [PubMed] [Google Scholar]
- 29.Czerninski R, Zini A, Sgan-Cohen HD. Lip cancer: incidence, trends, histology and survival: 1970–2006. Br J Dermatol. 2010;162(5):1103–9. doi: 10.1111/j.1365-2133.2010.09698.x. [DOI] [PubMed] [Google Scholar]
- 30.D’Souza G, Cullen K, Bowie J, Thorpe R, Fakhry C. Differences in oral sexual behaviors by gender, age, and race explain observed differences in prevalence of oral human papillomavirus infection. PLoS One. 2014;9(1):e86023. doi: 10.1371/journal.pone.0086023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. Sexual behavior in the United States: results from a national probability sample of men and women ages 14–94. J Sex Med. 2010;7 (Suppl 5):255–65. doi: 10.1111/j.1743-6109.2010.02012.x. [DOI] [PubMed] [Google Scholar]
- 32.Leichliter JS, Chandra A, Liddon N, Fenton KA, Aral SO. Prevalence and correlates of heterosexual anal and oral sex in adolescents and adults in the United States. J Infect Dis. 2007;196(12):1852–9. doi: 10.1086/522867. [DOI] [PubMed] [Google Scholar]


