Abstract
Intranasal vaccination generates immunity across local, regional and distant sites. However, nasal dendritic cells (DC), pivotal for the induction of intranasal vaccine- induced immune responses, have not been studied in detail. Here, using a variety of parameters, we define nasal DCs in mice and humans. Distinct subsets of “classical” DCs, dependent on the transcription factor zbtb46 were identified in the murine nose. The murine nasal DCs were FLT3 ligand-responsive and displayed unique phenotypic and functional characteristics including the ability to present antigen, induce an allogeneic T cell response and migrate in response to LPS or live bacterial pathogens. Importantly, in a cohort of human volunteers, BDCA-1+ DCs were observed to be the dominant nasal DC population at steady state. During chronic inflammation, the frequency of both BDCA-1+ and BDCA-3hi DCs was reduced in the nasal tissue, associating the loss of these immune sentinels with chronic nasal inflammation. The present study is the first detailed description of the phenotypic, ontogenetic and functional properties of nasal DCs and will inform the design of preventative immunization strategies as well as therapeutic modalities against chronic rhinosinusitis.
INTRODUCTION
Dendritic cells play a pivotal role in immune homeostasis, marshaling immunity against pathogens, while maintaining tolerance to commensals. The nasal associated lymphoid tissue (NALT) serves as a site for the induction of nasal (1, 2), pharyngeal (3), respiratory (4), oral (2), gastrointestinal (5, 6), genitourinary (7, 8) and systemic (9) immunity. It follows therefore that the nose should contain a significant population of dendritic cells, capable of priming and disseminating immune responses. However, nasal dendritic cells have not yet been characterized and are the focus of the present study.
The murine NALT consist of paired lymphoid structures, resting on the nasal surface of the soft palate on either side of the nasal septum (10–12). The NALT is covered by follicle-associated epithelium (FAE) (13) interspersed with M cells (14) (15, 16), goblet cells (17, 18) and intra-epithelial lymphocytes (IEL) (19). Within the NALT, B cells predominate over T cells at steady state (7, 20, 21), with IgD+ and IgM+ B cells constitutively present and IgA+ B cells readily inducible following intranasal vaccination (8, 22). Among T cells, Th0 CD4+ T cells, CD8+αα, CD8+αβ and CD8+γδ T cells have been described in the NALT, with CD4+ T cells predominating over CD8+ T cells at steady state (19, 23, 24). While structural similarities between the NALT and Peyer’s patches are noted (21, 23), important differences exist with regards to development (13) and lymphocyte homing (25, 26).
Dendritic Cells (DC)s initiate the adaptive immune response (27). Since the initial description of DCs as “CD11c+ cells”, we have come to recognize the complexity and lineage diversity of DCs in various tissues (28, 29). Among the nasal DCs, while studies have alluded to CD11c+ cells in the NALT (30) (20), there are no descriptions of DC phenotype, subsets or function.
Here, using a variety of assays, we have defined the morphology, phenotype, ontogeny and function of mouse nasal DCs. In doing so, we demonstrate the complexity of nasal DCs and their behavior in the face of inflammatory stimuli such as LPS. Additionally, we have examined putative DC subsets in surgically resected human nasopharyngeal tissue from normal volunteers as well as patients with chronic rhinosinusitis (CRS). The data presented herein is the first description of nasal DCs and will inform the design of novel intranasal vaccines for prevention and treatment of diseases.
RESULTS
Morphology of nasal DCs in mice
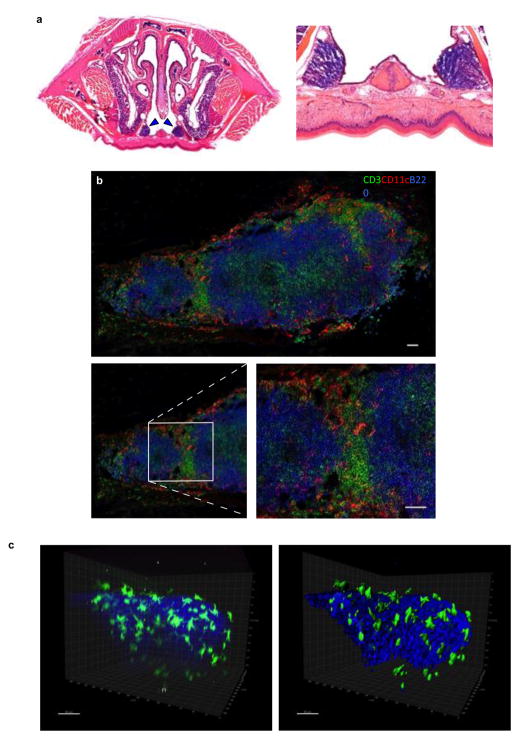
The NALT were identified on the nasal surface of the palate, between the incisors and first molar teeth as tridimensional, oval structures on Hematoxylin and Eosin (H&E) staining. Higher magnification (400x) revealed aggregates of mononuclear cells, populating the NALT (Figure 1a). To further study these mononuclear cells, nasal cryosections were stained with combinations of fluorescent antibodies identifying putative CD11c+ DCs, CD3+ T cells and B220+ B cells. Respective isotype controls confirmed the specificity of staining (data not shown). Distinct T and B areas were noted in the NALT as reported previously (30). Notably, DCs were predominantly seen in the T cell areas or in the periphery of the NALT (Figure 1b). Three-dimensional imaging using two-photon microscopy revealed a high density of CD11c-eYFP+ cells uniformly distributed on the NALT surface (Figure 1c). The majority of CD11c-eYFP+ cells were embedded among collagen fibers visualized by second harmonic generation and displayed numerous dendrites (Supplementary figure 1). However, upon deeper imaging through the NALT, CD11c-eYFP+ cells reduced in frequency and showed a less ruffled and condensed morphology (data not shown). To further study the peripherally distributed CD11c+ cells, nasal sections were double-labeled with anti-mouse keratin 18 and CD11c. A dense network of CD11c+ cells was found subjacent to the epithelium (Figure 1d). Fortuitously, in some of the sections we detected that nasal DCs were extending dendrites across the nasal epithelium, into the lumen of the nose (Figure 1d). Since extension of DC-dendrites was observed infrequently, we are unable to quantify this in the present study. We next studied the association of nasal CD11c+ cells with blood vessels (anti-PECAM-1) and lymphatic channels (anti-LYVE-1), and found nasal DCs clustering with lymphatic vessels in the posterior aspects of the NALT (Figure 1e) as well as the blood vessels distributed throughout the NALT (Figure 1f). Thus, a high density of putative DCs, positioned to sample the airway antigens, was noted within the murine nose.
Figure 1. DCs in murine nasal-associated lymphoid tissue (NALT).
(a) Hematoxylin and Eosin (H&E) staining was used to define the morphology of murine NALT (indicated with blue arrowheads) at 200x magnification (left) and at 400x magnification (right) (b) Immunofluorescent staining to define the relationship of NALT associated dendritic cells (DC) with T and B cells. Confocal micrograph of the entire longitudinal section of NALT is depicted here by combining individual images in Adobe Photoshop CC. CD3+ T cells (green), B220+ B cells (blue), and CD11c+ cells (red) are shown. Inset highlights a magnified area demonstrating that the CD11c+ cells are predominantly located in the T cells zones and in the periphery of the NALT. Each figure is representative of at least five experiments. Bars, 50μm. (c) Three dimensional reconstruction from two-photon microscopy data showing spatial distribution of nasal CD11c+ cells (green) from eYFP transgenic mice and collagen second harmonic generation (blue). Raw fluorescent image (left) and reconstructed image (right) are depicted. (d,e,f) Immunofluorescent staining to define the relationship of NALT DCs with the nasal epithelium, blood vessels and lymphatic channels. (d) Shows the relationship of CD11c+ cells (red) with the cytokeratin 18+ nasal epithelial cells (green) and B220+ B cells (blue). White arrowhead shows the extension of CD11c+ dendrites across the epithelium into the nasal lumen. (e) Depicts the relationship of CD11c+ cells (red) with LYVE1+ lymphatic channels (green) and B220+ B cells (blue) and (f) shows the proximity of CD11c+ cells (red) to PECAM1+ blood vessels (green) and B220+ B cells (blue). In panels d, e and f, confocal micrographs of the entire longitudinal section of NALT are depicted by combining individual images in Adobe Photoshop CC. A= Anterior, P=Posterior. Each figure is representative of at least three experiments. Bars, 50μm.
Phenotypic characterization of murine nasal DCs identifies distinct subsets of myeloid DCs
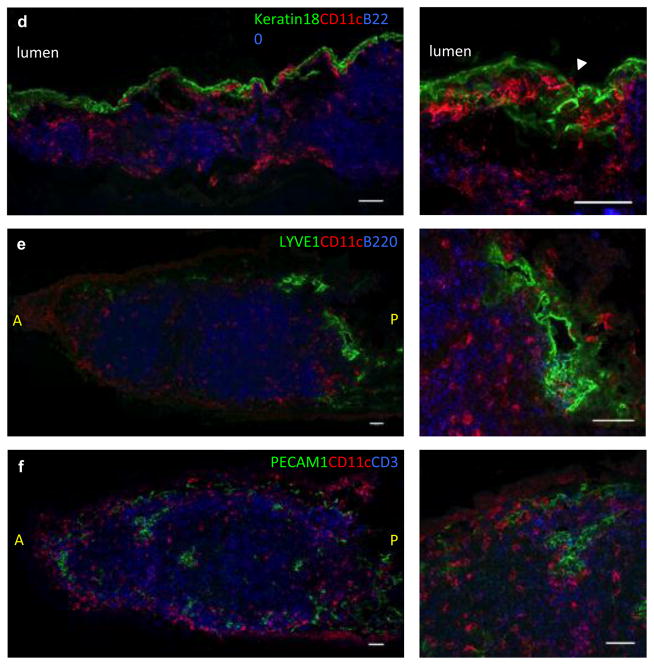
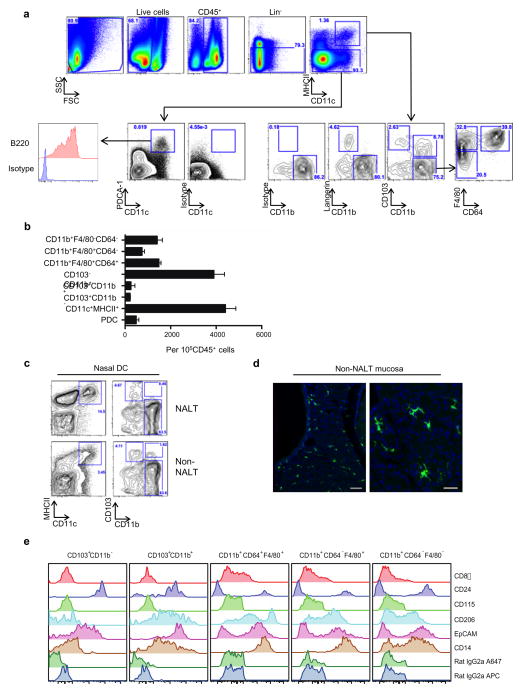
Using multi-parameter flow cytometry, we first examined DCs from the entire nose and gated on live, CD45+, lymphocyte lineage-negative, CD11c+MHCII+ cells isolated from mechanically disrupted and collagenase-digested whole nasal tissue. Three distinct populations of putative DCs could be identified using anti-CD103 and anti-CD11b antibodies: CD103+CD11b− cells, CD11b+CD103− cells and CD103+CD11b+ double positive cells (Figure 2a), with CD11b+CD103− cells being the predominant population. However, CD11b+CD103− cells are heterogeneous and comprise of both classical DCs (cDC) and macrophages (Mϕ). CD64 (FcγR1) has been shown to recognize Mϕ selectively (7, 26, 31, 32) and can help distinguish cDCs from Mϕ within CD103−CD11b+ cells.
Figure 2. Phenotypic characterization of nasal DCs.
(a, b, c) Single cell suspension of nasal cells was obtained by mechanical disruption and collagenase-digestion of nasal tissue. Multiparameter flow cytometry was used to identify DC subsets within the murine nose. (a) Defines the gating strategy used to delineate myeloid DC (mDC) subsets based on the expression of CD103, CD11b, and CD64 on live, CD45+lineage−CD11c+MHCII+ cells. For identification of plasmacytoid DCs (pDCs), MHCII− cells were defined on the basis of CD11c and PDCA-1 staining. PDCA-1hiCD11c+B220+ cells were deemed putative pDCs. (b) Absolute number of all DC subsets including pDCs. Error bars = standard deviation (SD). (c) Shows identification of NALT and non-NALT DCs separately and (d) Shows eYFP+ cells in non-NALT mucosa. Bars, 50μm (left) and 25μm (right). (e) Shows detailed phenotypic characterization of the nasal APC subsets using a panel of monoclonal antibodies. (f) Wright-Geimsa stains were used to define the cellular morphology of putative nasal DCs and nasal Mϕ. Bars, 10μm. (g) CD11c+langerin+DCs were analyzed by immunofluorescence using confocal microscope where langerin+ cells are depicted in green, CD11c+ cells in red and CD3+ cells in blue. White arrowheads indicate the cells where co-localization of langerin with CD11c was observed. Bars, 50μm.
We initially tested the expression of CD64 and heat stable antigen or CD24, an important co-stimulatory molecule for the induction of T helper cells (33), on CD11c+MHCII+ gated CD103−CD11b+F4/80+ cells. As shown in supplementary figure 2, the CD103−CD11b+F4/80+ cells contained both, CD24+ and CD24− cells. Further, analyses revealed that the CD64+ cells were contained within the CD11b+F4/80+ cells while CD11b+F4/80− cells and CD103+CD11b− cells, both lacked CD64 expression (Supplementary figure 2). These data indicated CD11c+MHCII+ gated CD103−CD11b+ cells within the nose contain both cDC and Mϕ which could be defined as CD64−F4/80− cDC and CD64+F4/80+ Mϕ (Figure 2a). Additionally, plasmacytoid DCs (pDCs), were identified among MHCII− nasal cells as PDCA-1hiCD11c+B220+ cells (Figure 2a). The total number cells contained within each of the DC subsets are quantified in figure 2b. Next, we examined DCs in the inductive (NALT) and effector (nasal passages) sites of nose separately. As expected, the density of putative DCs was significantly greater in the NALT tissue, compared to the nasal passages. Interestingly, the CD103+CD11b+ cells were predominantly found in the nasal passages while the NALT and non-NALT tissue, both contained CD103+CD11b− and CD103−CD11b+ cells (Figure 2c). Confocal images from CD11c-eYFP mice confirmed that eYFP+ DCs were present in non-NALT nasal mucosa (Figure 2d).
A detailed phenotypic assessment of each of the putative DC subsets was performed next (Figure 2e). Interestingly, all subsets of nasal CD11c+MHCII+ cells lacked CD8α. While both the CD103+CD11b− and CD103+CD11b+ cells were CD24hi, among the CD11b+ cells, the CD64+F4/80+ and CD64−F4/80+ subsets were predominantly (~90% cells) CD24−. In contrast, CD64−F4/80− cells contained equal numbers of CD24+ and CD24− cells. CD115 was not expressed by any of the nasal CD11c+MHCII+ subsets. Further, the CD103+CD11b− cells were negative for macrophage mannose receptor, CD206, while CD11b+CD103+ cells were CD206int. Among the CD11b subsets, CD64+F4/80+ cells were CD206hi, both CD64−F4/80+ cells and CD64−F/40− cells were CD206lo to CD206int. CD103+CD11b− and CD103+CD11b+ cells were EpCAMhi while the CD11b+ subsets contained both EpCAMhi and EpCAMlo cells. Finally and expectedly, LPS receptor, CD14 was expressed by the CD11b+CD64+F4/80+ cells as well as CD11b+CD64−F4/80+ cells while the CD11b+CD64−F4/80− cells contained both CD14+ and CD14− cells. In contrast, CD103+CD11b− cells were CD14 negative.
Collectively, these data show that among the CD11chiMHCII+ nasal cells we could identify five distinct populations of antigen presenting cells (a) CD103+CD11b− cells expressing phenotypic markers associated with CD103+ DC (34), (b) the CD103−CD11b+ cells, a heterogeneous population, comprising of three distinct subsets- (i) CD64+F4/80+ cells that had the phenotypic markers associated with Mϕ, (ii) CD64−F4/80− cells that had markers associated with CD11b+ cDCs and (iii) CD64−F4/80+ cells that appeared to have both Mϕ and cDCs like cells. (c) Finally, the nose also contained CD103+CD11b+ cells that shared phenotypic characteristics of both CD103+ DC and CD11b+ DC.
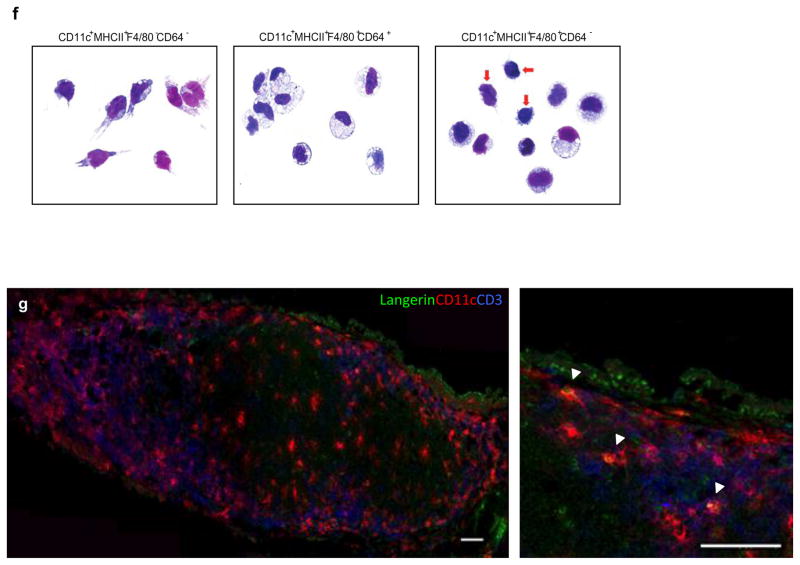
We next identified the morphological characteristics of putative nasal DCs and nasal Mϕ. Wright-Geimsa staining of cytospins of the FACS-sorted nasal DCs (defined as MHCII+CD11c+F4/80−CD64− cells based on the criteria defined above) as well as putative nasal Mϕ (defined as MHCII+CD11c+F4/80+CD64+ cells) revealed clear morphological differences. While nasal DCs had abundant cytoplasm and “dendrites”, nasal Mϕ showed an eccentric, reni-form nucleus with intracellular granules and lack of significant membrane extensions or dendrites. Further, since the CD11c+MHCII+CD64− F4/80+ cells were a major population (figure 2a), we examined them separately as well. While a majority of CD11c+MHCII+CD64−F4/80+ cells displayed the morphology of Mϕ with a granulated cytoplasm and reniform nucleus, cells with cytoplasmic extensions and less vacuolated cytoplasm, resembling DCs could also be seen (Figure 2f). Thus, the CD11c+MHCII+CD64−F4/80+ cells were a mixed population comprised of Mϕ and DCs both.
Finally, we wanted to determine the location CD103+CD11b− cells within the NALT. Since CD103+CD11b− cells exclusively expressed langerin, we used a combination of antibodies specific to CD11c, langerin and CD103 to denote putative CD103+ DCs in the NALT. The frequency of langerin+ cells that co-labeled with CD11c was rare. When found, the langerin+CD11c+ cells were mostly located toward the periphery of the NALT (Figure 2g), consistent with the expression of EpCAM by these cells, as noted by flow cytometry.
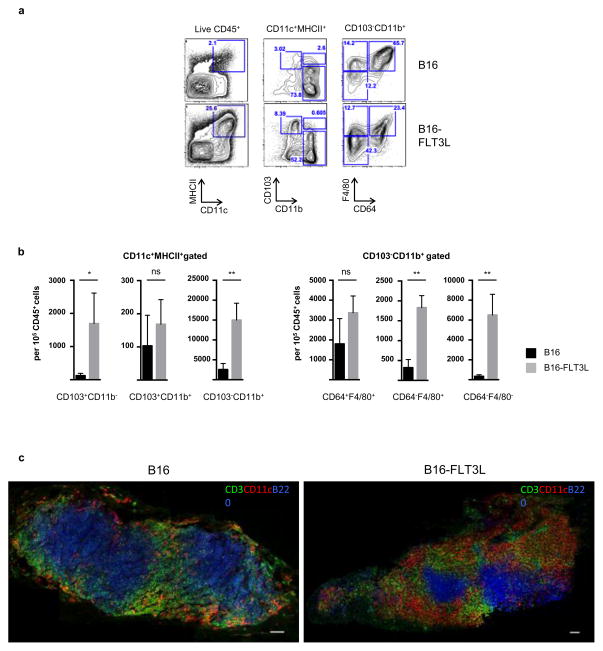
Fms-related tyrosine 3 kinase (FLT3) ligand expands CD103+CD11b− nasal DCs as well as CD103−CD11b+F4/80−CD64− nasal DCs
FLT3 ligand, a key cytokine in DC differentiation (35) has also been used as a potent adjuvant in nasally administered vaccines (29, 33, 36). To determine the effect of FLT3 ligand on nasal DCs, we implanted mice with 5–7x106 B16-FLT3L melanoma (B16-FLT3L) cells (37) and used mice implanted with B16 melanoma (B16) cells or wild type (WT) mice as controls. Nasal CD11c+MHCII+ cells were increased 12-fold in the B16-FLT3L mice compared to WT or B16 mice (Figure 3a). Among the CD11c+MHCII+ gated cells, the frequency of all nasal DC subsets was increased in B16-FLT3L mice, with CD103+CD11b− cells and CD103−CD11b+ cells showing the most appreciable increase in numbers (Figure 3a,b). Among the CD103−CD11b+ gated cells, a dramatic expansion in CD11b+CD64− cells was seen (both CD64−F4/80+ and CD64−F4/80− subsets). This further supported that CD64 is useful to distinguish between cDCs and Mϕ among the nasal CD103−CD11b+ cells. Immunofluorescent staining of the NALT further confirmed the dramatic increase in CD11c+ cells seen in the B16-FLT3L mice but not the B16 melanoma implanted mice (Figure 3c).
Figure 3. Identification of Fms-related tyrosine kinase 3 ligand (FLT3L) responsive nasal DC subsets.
C57BL/6 wild type (WT) mice were implanted with 5–7x106 B16-FLT3 ligand melanoma cells (B16-FLT3L), or B16 melanoma cells (B16) and the nasal DC subsets were analyzed by multiparameter flow cytometry (a and b) or immunofluorescence (c) after ten to fourteen days of tumor implantation. (a) Representative flow cytometry panels comparing the expansion of putative nasal DCs in B16 or B16-FLT3L mice and (b) shows cumulative data from three individual experiments Error bars = SD. *=p<0.05, **=p<0.01, ns= not significant. (c) Nasal cryosections from mice implanted with B16-FLT3L or B16 melanoma cells were stained for CD3 (green), CD11c (red), and B220 (blue). Scale bars, 50μm. The entire NALT is depicted here by combining individual images in Adobe Photoshop CC.
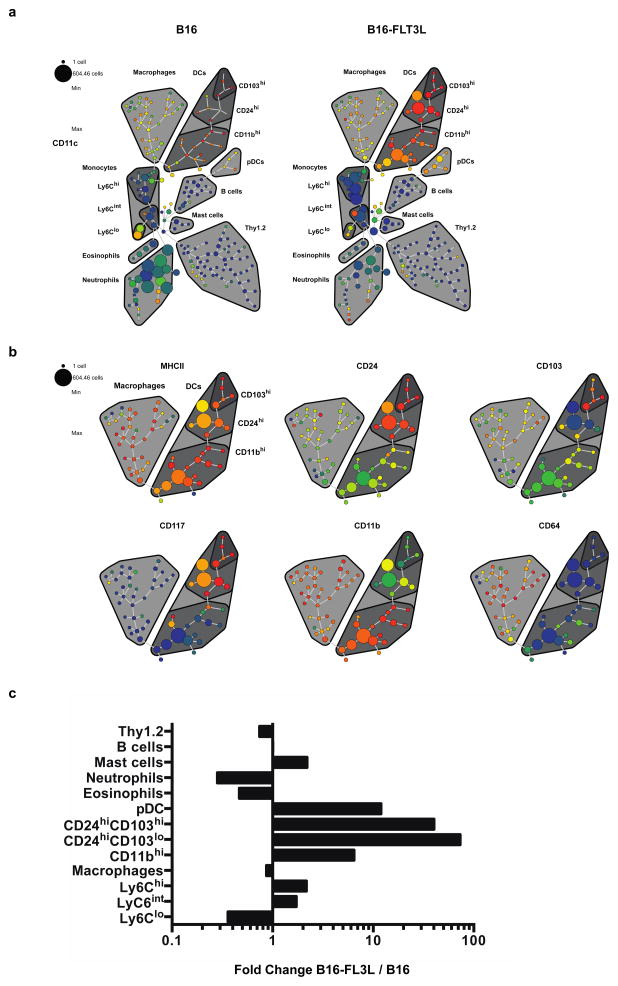
In order to further confirm these data, we performed additional experiments comparing the nasal populations of B16 and B16-FLT3L mice using mass cytometry (CyTOF), a novel, potentially paradigm changing technology that combines the principles of flow cytometry with mass spectrometry, thereby allowing the simultaneous examination of significantly more variables per cell than is possible by conventional flow cytometry (38). We analyzed nasal cell suspensions using a 20-parameter CyTOF panel focused on DC and Mϕ associated markers (supplementary table 4). We clustered DNA+CD45+ events into a minimum-spanning tree of phenotypically related nodes using spanning-tree progression analysis of density-normalized events (SPADE) (24) (Figure 4). Node clusters corresponding to definable cell populations were manually annotated on the basis of canonical marker expression while preserving visualization of unidentified clusters within the data set. The SPADE trees showed a clear and striking expansion of the CD11c-expressing dendritic cell populations following FLT3L treatment (Figure 4a). The expanding populations also expressed high levels of MHCII, and further delineation of the underlying phenotypic heterogeneity revealed a distribution of CD24, CD103, CD117 and CD11b expression among the expanding subsets, whereas there was no expansion in the CD64-expressing populations. For the sake of representation, only FLT3L treated mice, focusing on putative cDC and Mϕ are shown in figure 4b. These data are summarized in figure 4c, comparing the fold-change differences in the annotated cell populations as a percentage of total CD45+ cells between the B16-FLT3L and B16 mice. Fold change differences showed a dramatic expansion in CD24hiCD103lo (73 fold) nasal cells in the B16-FLT3L treated mice. Notably, these cells were MHCIIhiCD11c+CD11b+ thus confirming the flow cytometry data. Additionally, FLT3L treatment resulted in expansion in CD24hiCD103hi cells (40 fold).
Figure 4. CYTOF plots comparing nasal populations in B16 melanoma and FLT3L-B16 melanoma mice.
(a) SPADE plots showing the expression of CD11c in nasal mononuclear cell populations as indicated. (b) Macrophage and DC focused spade trees showing the expression of the indicated markers in FLT3L treated mice. The size of each node represents the number of cells and the strength of expression of the respective marker is indicated by the color as specified in the legend (c) Summary of the CYTOF data showing fold changes in the respective populations, comparing nasal populations in B16 and B16- FLT3L mice.
Together, these data show that the nasal cDCs include a FLT3L responsive, minor CD103+ population as well as a major CD11bint population that is CD24+ and CD64−. Additionally, within the CD11b+ population, CD64+ cells are FLT3L unresponsive, Mϕ-like cells. Ontogenic and functional data shown below further confirm these results.
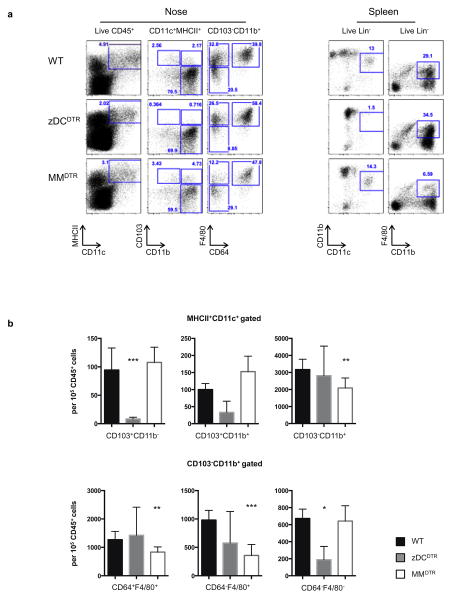
Zbtb46-DTR and LysmCre x Csf1rLsL-DTR identify cDC and ϕ respectively in the nose
Within the hematopoietic compartment, the zinc finger transcription factor Zbtb46 is specifically expressed by cDC as opposed to the overlapping expression of CD11c on DCs, Mϕ and activated monocytes (39, 40). Additionally, a recently described LysmCre x Csf1rLsL-DTR (MMDTR) mouse model identifies monocytes and Mϕ (41). Using a cell niche depletion approach, we defined cDC and Mϕ in the nose using zDCDTR-WT (referred to as zDCDTR), LysmCre x Csf1rLsL-DTR -WT (MMDTR) and WT-WT (WT) bone marrow chimeric mice. Nasal mononuclear cells were examined 24h-post administration of diphtheria toxin (DT). In the zDCDTR mice, among the CD11c+MHCII+ gated cells, CD103+CD11b− cells (called CD103+ DC henceforth) were depleted significantly and CD103+CD11b+ cells (called CD103+11b+ DC) tended to reduced also. In contrast, in the MMDTR mice, the CD103+ DC, CD103+11b+ DC were not depleted while the CD103−CD11b+ cells were significantly depleted. (Figure 5a,b). Upon further examining the CD103−CD11b+ cells we found that in the zDCDTR mice CD11b+CD64−F4/80− cells were significantly depleted while they were unaffected in the MMDTR mice, confirming these cells to be cDCs. Additionally, the CD11b+CD64+F4/80+ cells and CD11b+CD64−F4/80+ cells were significantly depleted in the MMDTR mice, confirming these cells to be derived from the macrophage/monocytic lineage. Thus, based on ontogeny, we could define CD103+CD11b− cells, and CD11b+CD64−F4/80− cells as cDC in the nose.
Figure 5. Identification of “classical DCs” and ϕ in the murine nose.
zDCDTR (Zbtb46-DTR) Tg or MMDTR (LysmCre x Csf1rLsL-DTR) or WT bone marrow chimeric mice were injected intraperitoneally (i.p.) with 500ng DT and live, CD45+ nasal cells were analyzed for expression of CD11c, MHCII, CD103, CD11b, F4/80, and CD64 one-day post DT administration. Numbers represent the percentage of cells in the indicated gate. (a) Representative flow cytometry plots comparing the percentage of nasal APCs between WT, zDCDTR, and MMDTR mice. (b) Cumulative data from three individual experiments is depicted here. Error bars = SD. *=p<0.05, **=p<0.01, ***=p<0.001.
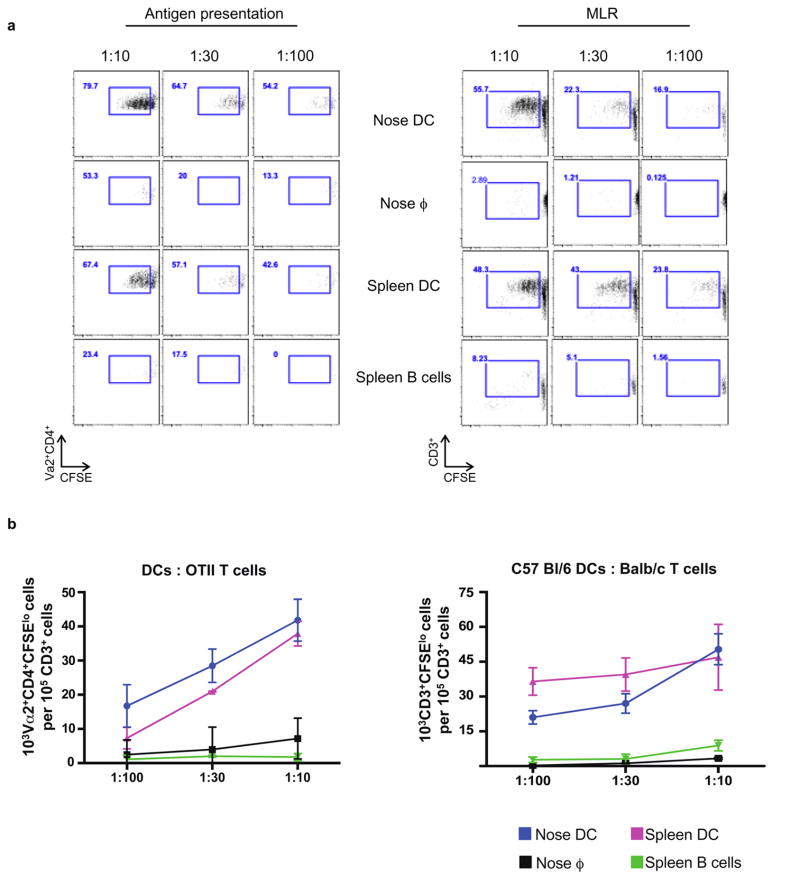
Nasal DCs present soluble antigen to OVA-transgenic T cells and induce mixed leukocyte reaction to allogeneic T cells
Having examined the anatomical, phenotypic, morphological and ontogenetic features of nasal “DCs”, we sought to use functional assays to confirm that these cells were indeed bona fide DCs. Antigen presentation to syngeneic T cells and mixed leukocyte reaction (MLR) to allogeneic T cells is among the most distinctive characteristics of DCs, and distinguishes them from the closely related Mϕ (42). In order to obtain sufficient numbers of cells to run functional assays and guided by the results of our FLT3L experiments, mice were implanted with B16-FLT3L melanoma cells. Nasal DCs (defined as CD11c+MHCII+F4/80−CD64− cells), nasal Mϕ (defined as CD11c+MHCII+F4/80+ CD64+ cells), splenic DCs (defined as Lin−CD11chiCD11bint cells, used as a positive control) and splenic B cells (negative control) were obtained by flow cytometric sorting. Notably, among the CD11c+MHCII+ cells, the CD103+ and CD11b+ subsets could not be used for co-cultures separately due to cell number limitations.
For the antigen presentation assays, respective cell populations were co-cultured with CFSE-labeled OVA-transgenic (OT-II) CD4+ T cells in the presence ovalbumin (OVA). To exclude the possibility that the OVA protein was degraded into peptides, which then bound spontaneously to MHCII molecules on T cells and induced T cell proliferation, we also included a control wherein OT-II cells were cultured in the presence of OVA alone, without DCs. The frequency of proliferating, Vα2+CD4+CFSElo T cells was quantified after 5 days of culture. A clear difference in antigen presenting ability was noted between nasal DCs and Mϕ. While nasal DCs, analogous to splenic DCs induced OT-II proliferation in the presence of OVA, nasal Mϕ analogous to splenic B cells did not (Figure 6a,b). OT-II cells cultured in the presence of OVA alone did not proliferate (data not shown). Nasal DCs showed poor ability to cross present to CD8+ T cells. This probably reflects the distribution of DCs in the nose- i.e. cross-presenting, CD8-priming, CD103+ DCs are a minority population whereas the CD4-priming CD11b+ DCs are the dominant population.
Figure 6. Nasal DCs present antigen to CD4+ T cells and induce proliferation of allogeneic T cells in a mixed leukocyte reaction (MLR).
(a) Nasal DCs from C57BL/6 mice were expanded with B16-FLT3L cells for ten to fourteen days before sorting. Nasal APCs were sorted into two subsets: CD11c+MHCII+ F4/80−CD64− cells, indicated as nose DCs and CD11c+MHCII+F4/80+CD64+ cells indicated as nose ϕ. Sorted cells were cultured in the indicated DC:T cell ratio for 5 days with CFSE-labeled splenic OT-II cells (left) or BALB/c splenic T cells (right). Spleen DCs were used as the positive control and spleen B cells were used as the negative control. Representative flow cytometry plots comparing the proliferation of Vα2+CD4+ T cells (left) or allogeneic T cells (right) by nasal DCs and ϕ. Cumulative data from one of three experiments is shown here. Error bars = SD. (b) Quantification of the number of proliferated (CFSElo) OT-II T cells (left) or Balb/c T cells (right). Cumulative data from one of three experiments is shown here. Error bars = SD.
For MLR assays, the nasal DCs, nasal Mϕ, splenic DCs and splenic B cells were cultured with CFSE-labeled BALB/c splenic T cells (as the allogeneic responders). Nasal DCs effectively stimulated allogeneic T cells similar to splenic DCs, while nasal Mϕ and splenic B cells were poor at inducing MLR (Figure 6a,b). These data highlight the functional differences between CD11c+MHCII+F4/80−CD64− cells and CD11c+MHCII+F4/80+ CD64+ cells and confirm the former to be bona fide DCs within the nose.
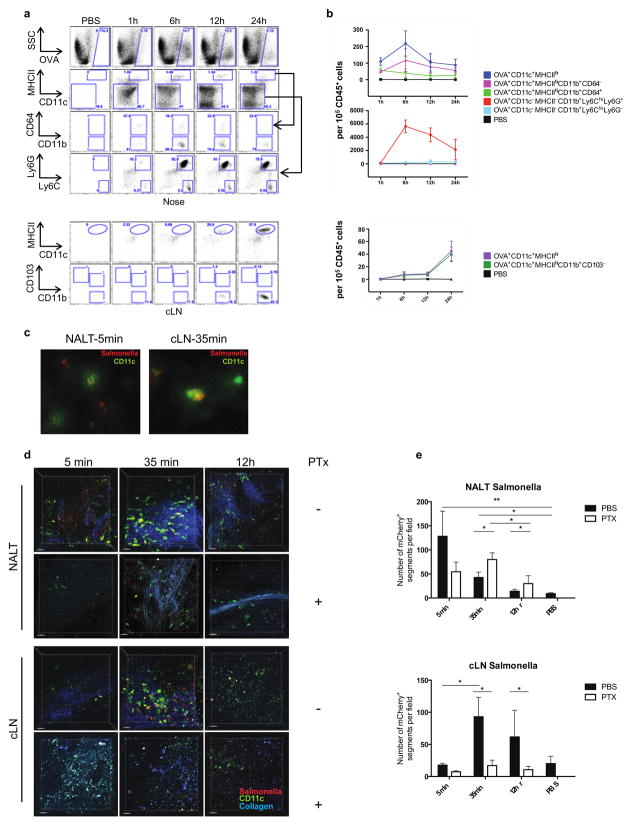
Nasal DCs migrate in response to lipopolysaccharide
Migratory behavior is a hallmark of DCs (43). To investigate this as yet another criteria to define nasal DCs, mice were administered OVA-Alexa 488 in combination with lipopolysaccharide (LPS) delivered intranasally. The nose and draining lymph nodes were examined at serial time points (1h, 6h, 12h and 24h post administration). PBS-administered mice were used as controls at each time point. In the nose, we assessed the uptake of OVA by live, CD45+ cells and found that a minority (~3%) of OVA+ nasal cells were CD11c+MHCII+, with peak labeling seen at 6h and declining by 24h. Further examination of the OVA+CD11c+MHCII+ cells revealed them to be predominantly CD11b+ (~99%). Among the CD11b+ cells, ~80% of OVA+ cells were CD64− bona fide DCs. Interestingly, a majority of the total OVA+ nasal cells were CD11c−MHCIIlo/intly6chily6GhiSSCint granulocytes. Peak uptake of OVA by granulocytes occurred at 6h and declined over 24h (although persisting well above baseline at 24h). Additionally, a small population of OVA+CD11c−MHCIIlo/intly6chily6G−SSClo monocytes appeared at 6h and persisted over 24h in the nose (Figure 7a,b).
Figure 7. Migration of nasal DCs to cervical draining LNs.
(a,b) Targeting of nasal DCs and Neutrophils following intranasal administration of OVA-Alexa 488 and migration of OVA+ DCs to the cervical lymph nodes. (a,b) At least three WT mice per time point were administered either OVA Alexa 488 plus LPS or were given PBS intranasally and analyzed at 1h, 6h, 12h, and 24h. (a) (Top) Shows representative flow cytometric analysis of OVA+ cells. Both nasal DCs (CD11c+MHCII+CD11b+CD64− cells) and neutrophils (CD11c−MHCII−Ly6ChiLy6Ghi cells) are shown. (Bottom) Shows representative flow cytometric analysis of OVA+ migratory DCs (CD11c+MHCIIhi cells) in the cLN at respective time points. (b) Cumulative data from three individual experiments is quantified here. Error bars = SD. (c) Three-dimensional reconstruction from two-photon microscopy data showed dramatic change in spatial distribution of CD11c-eYFP+ DCs (green) and mCherry expressing salmonella (red) between NALT and cervical lymph nodes (cLN). Second-harmonics signals from collagen are in blue. Scale bars, 30μm. (d) Numbers of mCherry+ cells in NALT (top) and cLN (bottom) were quantified using the Imaris software (Bitplane). Each figure is representative of at least three experiments. Error bars = SD. 400x magnification. (e) Uptake of Salmonella typhimurium by CD11c-eYFP+ cells derived from the murine nose and mediastinal lymph node is compared between PBS and PTX administered mice at 5 min, 35 min and 12h post administration using two-photon microscopy.
In parallel to the nose assessments, we also examined the draining lymph nodes (LN)- both cervical LN (cLN) and mediastinal LN (mLN) for migratory DCs (live, OVA+lin−MHCIIhiCD11c+ cells). As shown in figure 7a and quantified in 7b, a small population of OVA+ migratory DCs could be detected in the cLN at 6h with a progressive and striking increase at 24h. Further analyses of these migratory DCs within the cLN revealed them to be predominantly CD11b+CD64− with a small number of CD103+CD11b− and CD103+CD11b+ DCs as well, reflecting the numeric distribution of these DC subsets in the nose. As much as 40% of the OVA+ cells in the cLN at 24 hr were CD11cint/−MHC-IIint/lo (figure 7a). However, we did not include granulocyte-specific markers in the lymph node panel. Therefore, we are unable to confirm whether OVA+ neutrophils also migrate into the lymph node. Interestingly, we did not detect OVA+ migratory DCs within the mLN even at 24h (data not shown). Thus we were able to demonstrate clear uptake of a fluorescent antigen by nasal DCs and their subsequent migration to the draining LN.
Next, to examine the response of nasal DCs to gram-negative pathogens, Salmonella enterica serovar Typhimurium constitutively expressing mCherry (Salmonella-mCherry) was administered intranasally to CD11c-eYFP transgenic mice. To compare DC-associated or DC-independent clearance of Salmonella from the nose, we co-administered either PBS or Pertussis Toxin (PTX). The latter is a known inhibitor of DC motility (34). Using two-photon microscopy, Salmonella-mCherry were seen in the nasal cavity as early as 5 minutes after application, distributed within the nasal lumen (Figure 7d) as well as occasionally internalized within CD11c+ nasal cells (Figure 7c). With surprising kinetics, 35 minutes post-administration, in the PBS group, a (~50%) decline in mCherry+ cells was seen in the nose. In contrast, PTX-treated mice had a significantly greater number of mCherry+ cells compared to the nose of PBS treated mice. This difference persisted at 12h (Figure 7d,e). Analogously, within the cLN, a striking increase in mCherry+ cells was seen in the PBS-treated but not PTX-treated mice at 35min and 12h. These data demonstrate a rapid flux of Salmonella into the draining lymph nodes and highlights the rapid response of the antigen presenting cells in the nose to a bacterial challenge, which is attenuated by PTX, an inhibitor of DC migration.
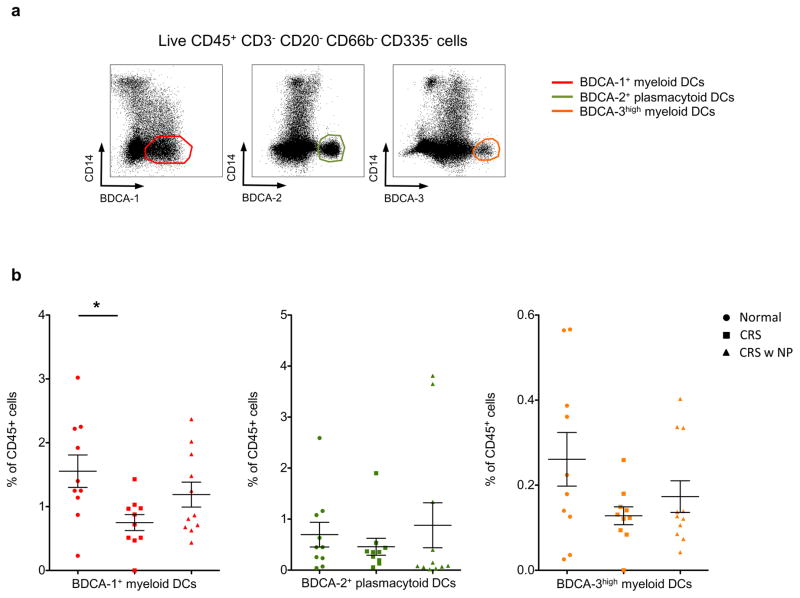
BDCA-1+ DCs form the predominant DC population in human nasopharyngeal tissue at steady state and are significantly reduced during chronic inflammation
To identify nasal DCs in humans, we analyzed nasopharyngeal and sinus tissues from 10 normal volunteers (a total of 10 tissue samples) and 10 patients with chronic rhino-sinusitis (CRS, a total of 21 tissue samples) (Supplementary Table 1). The CRS patients were further divided into patients with and without nasal polyps, since these two clinical entities show distinct phenotypes, with patients having nasal polyps being more refractory to treatment. The clinical parameters that were assessed included patient age, sex, tissue analyzed, indications for surgery and a thorough list of the concomitant medications immediately proximal to the surgery. The mean age of normal volunteers was 52 years (range 25–82), the mean age of patients with CRS was 52 years (range 40–75), while the mean age of patients with CRS/nasal polyps was 50 years (range 33–61). Patients with CRS demonstrated greater use of steroids and antibiotics. We performed a detailed multicolor flow cytometric analysis, first gating on single cells, live cells, CD45+, lymphocyte lineage-negative, BDCA-1+ cells, and we also surface labeled for BDCA-2+ and BDCA-3+. Three distinct populations of human nasal DCs were identified as BDCA-1+ myeloid DCs, BDCA-2+ plasmacytoid DCs, and BDCA-3hi myeloid DCs (Figure 8a). We observed a significantly higher frequency of BDCA-1+ DCs rather than BDCA-3hi DCs in normal volunteers as well as in patients with CRS. More importantly, when compared with normal volunteers, patients with CRS displayed a significantly lower frequency of BDCA-1+ DCs (p<0.05) and a trend towards lower BDCA-3hi DCs (p=0.07). These differences were not seen on comparing normal volunteers and patient with CRS with nasal polyps (Figure 8b). In addition to the DC subsets described above, a detailed analysis of nasal mononuclear cells was performed. This included monocyte subsets, neutrophils, T cells, B cells and NK cells. A decline in the BDCA-1+ and BDCA-3hi DCs was not accompanied by a corresponding increase in other inflammatory cells within the nose (Supplementary figure 3).
Figure 8. Identification of DCs in human nasal mucosa.
(a) Live CD45+ mononuclear CD3− CD20− CD335− CD66b− CD14− cells, i.e., T, B, NK, neutrophils and monocyte excluded cells were analyzed for BDCA-1, 2, 3 markers. Three DC populations are shown: BDCA-1+ myeloid DCs (left), BDCA-2+ plasmacytoid DCs (middle), BDCA-3hi myeloid DCs (right). (b) Frequency of BDCA-1+ cells, BDCA-2+ cells and BDCA-3hi cells as a percent of CD45+ mononuclear cells of Normal, CRS, or CRS with nasal polys. Composite data from 20 donors are shown. * p<0.05.
DISCUSSION
Mucosal vaccination is considered to be superior to systemic vaccines for the generation of local and perhaps disseminated mucosal immune responses. Due to its non-invasive nature and imminent antigen availability (most notably circumventing enzymatic degradation that precedes gastrointestinal mucosal absorption), intranasal antigen delivery appears to be the most feasible and clinically relevant of the various routes of mucosal vaccination and is supported by the rapid development of newer technologies to improve vaccine potency (chitosan derivatives) (44) and safety (nanogels) (45). In fact, a substantial research initiative funded by the Bill and Melinda Gates foundation focuses on the development of novel, needle free mucosal vaccines (37). In spite of these advances, basic descriptions of dendritic cells in the nasal mucosa are lacking.
The observation that nasally delivered vaccines can induce antigen specific immunity across a wide variety of systemic and mucosal sites (21) led us to hypothesize that the nasal tissue would contain a high density of DCs. In support of our hypothesis, we observed that a robust population of DCs patrols the nasal cavity, anatomically distributed in sub-epithelial, peri-vascular and peri-lymphatic spaces, poised to respond to antigen. The latter was confirmed by the rapid kinetics of nasal DC mobilization following i.n. administration of LPS or pathogenic gram negative bacteria. Further, we observed nasal DCs to possess a high phenotypic diversity with distinct subsets contained within CD11c+MHCII+ cells. Specifically, CD11c+MHCII+ gated CD103+CD11b− nasal cells, and CD11b+CD64−F4/80− nasal cells are dependent on the transcription factor zbtb46 and show a preferential expansion by the cytokine FLT3L, defining these cells as “classical DCs”, capable of inducing a mixed leucocyte reaction and antigen presentation. Additionally, these cells demonstrate classical DC morphology (43) and migrate in response to antigen. In contrast to the DCs, CD11b+CD64+F4/80+ cells in the nose did not expand with FLT3L or deplete with DT in the zbtb46-DTR mice. However, this population was significantly depleted in the MMDTR mice. Morphologically, these cells demonstrated a vacuolated cytoplasm with an eccentric, reniform nucleus. Functionally, the CD11b+CD64+F4/80+ cells neither presented antigen, nor induced MLR. Based on these criteria, we confirm nasal CD11b+CD64+F4/80+ cells to be Mϕ. Additionally, a third population among the CD11b+ cells was seen- CD11b+CD64−F4/80+. Morphologically, this was a mixed population comprising of both DCs (minority of the cells) and Mϕ (majority of the cells). Accordingly, this population is FLT3L responsive on one hand, while being significantly depleted in the MMDTR mice on the other. Furthermore, while the CD11b+CD64−F4/80+ cells are also depleted in the zDCDTR mice, likely due to the lower number of DCs contained within this heterogeneous subset, the depletion does not meet statistical thresholds. Unexpectedly, the murine nose also contains CD103+CD11b+ DCs, particularly in the non-NALT nasal tissue that co-express CD11b and CD103 like the intestinal lamina propria DC subsets (46) and are partially zbtb46 dependent (perhaps reflecting their heterogeneous composition). Due to the small number of these cells, we are unable to perform functional assays specific to this population. However, nasal CD103+CD11b+ cells share phenotypic characteristics of CD103 and CD11b DCs; they co-express CD24, CD206 and EpCAM and appear to be intermediate for F4/80 and CD14 and thus share characteristics of both CD103+ DCs and CD11b+ DCs. Thus, we have identified 5 subsets of APCs within the murine nose. CD103+CD11b− cells, CD103+CD11b+ cells and CD11b+CD64−F4/80− cells identified as cDCs, CD11b+CD64+F4/80+ cells identified as Mϕ and CD11b+CD64−F4/80− cells being a mixed population, comprising of both, cDCs and Mϕ.
We also document BDCA-1+ and BDCA3hi myeloid DCs as well as BDCA-2+ plasmacytoid DCs within the human nasopharyngeal tissue and observe a decline in myeloid DCs to be associated with chronic rhinosinusitis. In light of these observations, we believe the present study to be the first comprehensive anatomic, phenotypic, ontogenic and functional assessments of nasal dendritic cells.
In addition to identifying distinct subsets of myeloid nasal DCs, we conclude that The CD11b+CD64−F4/80− DCs comprise of the majority of nasal DCs. In contrast to the Peyer’s patches (considered as immune inductive sites for the intestines), which have a high frequency of CD103+ DCs, the NALT (considered as inductive immune sites for the respiratory tract) contains a low frequency of CD103+ DCs. The nasal CD103+ DCs are langerin+CD24+EpCAM+TLR3+, zbtb46 dependent and FLT3L-responsive. Therefore, it would appear that the nasal cDCs are responsive to FLT3L, explaining and emphasizing the adjuvant role of FLT3L in nasally delivered vaccines (29, 33, 36, 47).
To define the anatomic relationships of nasal DCs with other cells, we have used two- and three-dimensional imaging. Two-dimensional micrographs suggested a sub-epithelial location of nasal DCs, both within- and extraneous to the NALT, in agreement with similar such observations (30). Further, a dense network of CD11chi cells, with a classical “dendritic” morphology was found by two-photon microscopy of the NALT with second harmonics suggesting a lumen-oriented distribution of nasal DCs. In fact, we documented the extension of dendrites across the NALT epithelium, suggesting that nasal DCs sample the luminal contents across intact epithelium akin to the gut resident CX3CR1+ cells (25). Additionally, we found nasal DCs to cluster around blood vessels and especially around the lymphatic channels, situated in the posterior aspects of the NALT and speculate, that in the absence of afferent lymphatics, perivascular DCs are entering the NALT while peri-lymphatic DCs are exiting it. Deeper areas within the NALT contained CD11c+ cells, albeit with a compact, rounded (as opposed to dendritic) appearance on two-photon imaging, perhaps suggesting that as the DCs contacted antigen, they became activated, lost their dendrites and migrated deeper within the nasal tissue.
As further evidence of function, we tested for DC migration by two sets of studies. In the first, fluorescent OVA was tracked in the nasal tissues as well as draining lymph nodes over time. A majority of the OVA+ nasal DCs (~99%) were CD103−CD11b+CD64− that appeared within the cLN by 6h and progressively increased over 12–24h. The kinetics of response to Salmonella-mCherry were however, much different. Within 5 minutes of application, although a majority of the bacteria were in the nasal lumen, we could also detect Salmonellae intracellularly within the nasal CD11c+ cells. Furthermore, ~50% of the administered bacteriae (109 cfu) were cleared from the nose within half an hour of administration and could be detected in local draining lymph nodes by 35min. The kinetics would suggest a DC-independent migration of Salmonellae into the draining LN. To further study this, we administered PTX, a known inhibitor of DC migration. This resulted in a significantly greater bacterial retention within the nose at 35 min and a corresponding reduction in the Salmonella count within the draining LN. This difference between PBS and PTX administered mice persisted over 12h. These data suggest a rapid transport of gram-negative bacteria into the draining LN by the nasal DCs.
To lend clinical relevance to our mouse studies, we studied nasal DCs in human volunteers over a 12-month period. The goal of our human studies was to define the DC subsets in nasopharyngeal tissue and to determine if a change in DC frequency is associated with chronic inflammation. Notably, previous studies have described human nasal DCs using a combination of HLA-DR, CD11c and CD1c expression(48) (49). Here, using a detailed, 12-color flow-cytometry panel we found that in addition to BDCA-2+ pDCs, human nose biopsies encompass 2 other subsets of DCs: a major BDCA-1+ population and a smaller BDCA-3hi population. Interestingly, patients with CRS had a significantly lower frequency of BDCA-1+ DCs than normal individuals, while the BDCA-3hi DC reduction also trended towards statistical significance. Detailed functional or transcriptomic assessments were limited by the number of cells available to us in this study. However, in many of the human biopsy samples that we studied for DC subsets, microbial studies done as part of clinical care demonstrated a persistence of coagulase-negative staphylococci. This, combined with the observed reduction in BDCA-1+ and BDCA-3hi DCs in CRS makes us hypothesize that a reduction in DCs, the key antigen presenting cells within the nose, may predispose to impaired pathogen clearance and chronic inflammation. An alternative possibility is that nasal DCs may migrate into the draining LN during chronic inflammation leading to falsely lowered numbers seen in the surgical specimens (22). Since obtaining tissue from patients prior to the onset of CRS is impossible, we are unable to test this hypothesis. Finally, although we tried to control for the effect of treatment by a careful analysis of all concomitant medications, it is likely that treatment may have confounding effect on our results. It is has been shown that nasal pDC and mDC subsets are significantly reduced following steroid use (22) and a number of patients in the CRS with nasal polyp group were treated with steroids prior to surgery. Regardless, further testing of the possibility that reduced nasal DC frequency may impair pathogen clearance from the nose and predispose to CRS may help identify the role of therapeutic vaccination strategies (targeting nasal DCs) to augment immune responses against specific pathogens in the treatment of patients with CRS.
To summarize, in this paper we provide the first detailed phenotypic and functional description of murine nasal DCs and describe a significant decrease in DC number to be associated with chronic naso-pharyngeal inflammation in humans. In doing so, we believe that the present study will direct the design of novel preventative and therapeutic vaccine strategies against human diseases.
MATERIALS AND METHODS
Human studies
Human nasal samples
Human nasal and nasopharyngeal tissue was obtained patients undergoing otorhinological surgery for clinically indicated reasons at the Mount Sinai Hospital. Clinical details of the patients are listed in Supplementary table 1. Informed consent was obtained from the patients. All samples were collected according to protocols approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai.
Analyses of human nasal dendritic cells
The human nasopharyngeal samples were processed immediately post-surgery. The tissue was minced, treated with 0.25 mg/ml of collagenase (Sigma-Aldrich, St. Louis, MO) at 37°C for 60 minutes and cell isolation was performed. Cells were surface stained with CD45, CD20, CD3, CD335, CD66b, BDCA-1, BDCA-2, BDCA-3, CD14, and Live/Dead Fixable Blue Dead Cell Stain (Life technologies, Grand Island, NY). Titrated Abs were added to the cells in 50 μl PBS 1% FCS for 30 min at 4°C. Washed cells were fixed in 2% formaldehyde and stored at 4°C until analysis, which was performed using an LSR II flow cytometer (BD Biosciences, San Jose, CA). The whole sample was acquired and analysis was preformed using Flow Jo 9.1 software (Tree Star, Ashland, OR). To identify human DC subsets, dead cells were excluded and CD3+, CD20+, CD335+, CD66b+, and CD14+ cells i.e., T, B, NK, neutrophils and monocytes were sequentially gated out; three DC populations were identified within the CD45+ mononuclear cells by gating respectively on either BDCA-1+ cells, BDCA-2+ cells or BDCA-3hi cells.
Fluorescent antibodies used
For human antibodies, we used mAbs conjugated to different fluorochromes to anti-BDCA-1 (L161- Biolegend, San Diego, CA), anti-BDCA-2 (AC144- Miltenyi Biotec, San Diego, CA), anti-BDCA-3 (AD5-14H12- Miltenyi Biotec, San Diego, CA), anti-CD45 (HI30- BD Horizon, San Jose, CA). The following antibodies of anti-CD3 (OKT3), anti-CD20 (2H7), anti-CD66b (G10F5), anti-CD335 (9E2) were obtained from Biolegend (San Diego, CA). The antibody to CD14 (TüK4) was obtained from Invitrogen (Grand Island, NY).
Mouse studies
Mice
Animal care and experimentation were consistent with guidelines of the US National Institutes of Health and were approved by the Institutional Animal Care and Use Committee (IACUC) of Mount Sinai School of Medicine. C57BL/6 mice (B6) and Balb/c mice were purchased from Taconic Farms (Hudson, NY) or bred at Mount Sinai School of Medicine. CD11c-EYFP reporter mice (14) were purchased from Jackson Laboratory (Bar Harbor, ME). C57BL/6-Tg(TcraTcrb)425Cbn/J (OT-II) mice were kindly provided by Dr. Shu-Hsia Chen (Mount Sinai School of Medicine). zDCDTR bone marrow chimeric mice were generously provided by Dr. M.C. Nussenzweig (39) (Rockefeller University). MMDTR (41) or C57BL/6 bone marrow chimeric mice were obtained from the laboratory of Dr. Daniel Mucida (Rockefeller University). All animals were housed under specific pathogen-free (SPF) conditions and sacrificed at the indicated time points.
Bone marrow chimeras were created by transferring bone marrow from zDCDTR, MMDTR and C57BL/6 mice into lethally irradiated WT C57BL/6 mice to avoid lethality associated with DT treatments of zDCDTR or MMDTR. In brief, 7 weeks old male C57BL/6 hosts underwent two treatments of 500 rads in an animal γ-irradiator 3-h apart, and 2.5 × 106 bone marrow cells from 8–12 weeks old zDCDTR, MMDTR and C57BL/6 (WT) donors, respectively, were transferred i.v. The resulting mice (referred to herein as zDCDTR, MMDTR and WT) were housed under SPF conditions. The chimeric mice were fully reconstituted and ready for experimental use after eight weeks.
Isolation of NALT
Mice were euthanized by CO2 inhalation and an incision was made at the angle of the mouth on both sides to open the mouth and expose the palate using established protocols (23). Using with curved fine forceps, the NALT bearing hard palate was slowly peeled and immediately embedded in to OCT (optimal cutting temperature; Sakura Finetek, Torrance, CA), and stored at −80°C. Nasal sections were cut at 10 μm thickness with a Leica cryostat (Leica Microsystems, Buffalo Grove, IL), and stored at −80°C.
Histology and immunofluorescence analysis
Nasal cryosections were stained with Hematoxylin and Eosin (H&E) and FACS-sorted CD11c+MHCII+CD11b+F4/80−CD64− and CD11c+MHCII+CD11b+F4/80+CD64+ nasal cells were centrifuged by cytospin onto glass sides, stained in Wright-Geimsa stain solution. Images were captured by brightfield microscope (Zeiss Axioplan2IE; Carl Zeiss, Thornwood, NY) and AxioVision software (Carl Zeiss). 10μm nasal sections were briefly air-dried, fixed in cold-acetone for 15 minutes, rehydrated in PBS for 10 minutes, blocked with 5% BSA/0.01% Tween/PBS for 30 minutes at room temperature. Sections were stained in a humidified chamber for 1 or 2 hours at room temperature or overnight at 4°C with primary antibodies (Supplementary table 2), washed with 0.01% Tween/PBS for 5 minutes three times, and stained for 1 hour at room temperature with secondary antibodies. If necessary, fluorochrome-labeled tertiary antibody was applied. T cells were immunostained with rabbit anti-mouse CD3 followed by anti-rabbit IgG Alexa Fluor 488, B cells with rat anti-mouse B220 followed by anti-rat IgG Alexa Fluor 647, and DCs with hamster anti-mouse CD11c followed by both biotinylated anti-hamster IgG and streptavidin Alexa Flour 555. Epithelial cells were immunostained with rabbit anti-mouse cytokeratin 18 followed by anti-rabbit IgG Alexa Fluor 488. Endothelial cells, lining lymphatic vessels were stained with rabbit anti-mouse LYVE-1 followed by anti-rabbit IgG Alexa Fluor 488. The longitudinal sections of NALT were stained with rat anti-mouse PECAM-1 followed by anti-rat IgG Alexa Fluor 488. Sections were stained with goat anti-mouse langerin (E17) followed by donkey anti-goat Alexa 488. Sections were mounted in ProLong Gold Antifade Mounting Medium with 4′, 6-diamidinio-2-phenylindole (DAPI) (Life technologies, Grand Island, NY). Fluorescent images were examined in laser scanning confocal microscope (SP5 DM; Leica Microsystems, Buffalo Grove, IL) and LAS AF software (Leica Microsystems) at the Microscopy Shared Resource Facility of Mount Sinai School of Medicine and epi-fluorescence microscope (Eclipse Ni-U; Nikon Instruments, Melville, NY) with NIS Elements BR software (Nikon Instruments) at the Immunology Institute of Mount Sinai School of Medicine.
Two-photon microscopy
After euthanizing mice, the NALT and lymph nodes were surgically isolated and transferred to an 25x25x1 mm imaging chamber (Grace Bio-Labs, Bend, OR) containing RPMI. Two-photon imaging was performed using an Olympus Fluoview FV1200MPE microscope with a 40X/0.8NA water emersion objective lens. For multiphoton excitation and second harmonic generation, a MaiTai Ti:sapphire laser (Newport/Spectra-Physics, Santa Clara, CA) was tuned to 790 and 890 nm for optimized excitation of mCherry expressing Salmonella and CD11c-eYFP+ cells, respectively. Emission filters were 420–460 for SHG, 495–540 nm for eYFP, and 575–630 nm for mCherry. Six-eight 80 μm z-stacks were acquired for each NALT and two-four 200 μm z-stacks were acquired for each lymph node with 2 μm z-spacing between each optical section (512x512 pixels). 3-D reconstruction and image analysis was performed using watershed segmentation algorithms in Imaris (Bitplane, South Windsor, CT) to quantify numbers of mCherry+ and CD11c-eYFP+ cells.
Nasal, splenic, and LN single cell preparation
After euthanizing mice, the entire nose was dissected out using previously reported methods (23). The organ was mechanically disrupted to a using scissors and transferred to conical tubes. The tissue pieces were re suspended in 10 ml of RPMI containing 0.3 mg/ml of collagenase (Sigma-Aldrich, St. Louis, MO) and shaken at 200 rpm for 60 minutes at 37°C. The tissue suspension was collected and passed through a 70-μm cell strainer and the cells were pelleted by centrifugation at 1600 rpm for 5 minutes. The nasal cells were then resuspended in RPMI. For analyses of NALT and non-NALT DCs separately, the NALT was dissected out as mentioned in the preceding sections. The remaining nasal tissue and NALT-tissue were then collagenase-digested and mentioned above.
For spleen cell preparation, ACK lysis of red blood cells was followed by washing twice and filtering undigested fibrous material through a 70-μm cell strainer.
For lymph node single cell preparation, LNs were isolated, mechanically disrupted. LN single-cell suspensions were prepared by incubation with 400 U/ml collagenase D at 37°C for 30 min. Cells were filtered through a 70-μm cell strainer.
Nasal dendritic cell isolation
Single cell suspensions were isolated from the nose as described above. Using magnetic beads (Miltenyi Biotec, San Diego, CA), CD11c+ cells were isolated as previously described (50). Briefly, the cells were washed in 1ml of MACS buffer (Miltenyi Biotec, San Diego, CA), prior to 30 minutes incubation on ice with CD11c+ beads. The cellular suspensions were washed twice in MACS buffer and passed through a magnetic column, CD11c+ cells were isolated by positive selection, washed, resuspended in PBS. The subsets of CD11c+ enriched cells were then sorted on FACSAria (BD Biosciences, San Jose, CA) as CD11c+MHCII+CD11b+F4/80−CD64− and CD11c+MHCII+CD11b+F4/80+CD64+ cells.
Fluorescent antibodies used
We used the following murine antibodies, detailed in Supplementary table 3 to anti-CD3 (17A2), anti-CD4 (RM4-5), anti-CD8α (53–6.7), anti-CD103 (M290), anti-Ly6G (1A8), anti-CD64 (X54-5/7.1) from BD Biosciences (San Jose, CA); anti-CD11b (M1/70), anti-CD11c (N418), anti-CD45 (30-F11), anti-CD19 (6D5), anti-F4/80 (BM8), anti-Ly6C (HK1.4), anti-CD24 (M1/69), anti-TLR3 (11F8), anti-TCR Vα2 (B20.1), anti-CD14 (Sa14-2), anti-MMR/CD206 (C068C2) from Biolegend (San Diego, CA); anti-CD3e (145-2C11), anti-EpCAM (G8.8), anti-CD24 (M1/69), CD115 (AFS98), anti-MHCII (M5/114.15.2), anti-CD207 (L31), anti-CD317 (129c), anti-CD45R (RA3-6B2), anti-NK1.1 (PK136) from eBioscience (San Diego, CA). AQUA (L34957) was from Life technologies (Grand Island, NY) and CFSE was from Sigma-Aldrich (St. Louis, MO).
Flow Cytometric analyses and gating
Cells were isolated as described above. Prior to staining, cells were washed and resuspended in staining buffer containing 1x PBS, 2% BSA, 10 mM EDTA and 0.01% NaN3. To block non-specific staining, the 2.4G2 anti-CD16/32 antibody was added. Antibodies for cell surface markers were added and cells were incubated for 25 min at 4°C. Following the staining, the cells were washed twice and analyzed immediately or fixed in PBS containing 1% paraformaldehyde and 0.01% NaN3 and analyzed later on an LSR Fortessa (BD Biosciences, San Jose, CA) using multiparameter flow cytometry.
For intracellular staining, post surface staining, cells were resuspended in Fixation/Permeablization solution (BD Cytofix/Cytoperm kit- BD Biosciences, San Jose, CA), and intracellular cytokine staining was performed according to the manufacturer’s protocol. Flow cytometric data was analyzed with FlowJo software (Tree Star, Ashland, OR). Myeloid nasal DC cells were identified by forward and side scatter characteristics, dead cells were excluded using Live-dead fixable Aqua (Life technologies, Grand Island, NY) followed by sequential gating on CD45+, MHCII+, CD11c+, CD11b+ or CD103+ or CD11b+CD1103+ double positive populations.
B16-FLT3L-induced cell expansion in vivo
B16 melanoma cells (B16) and B16 melanoma cells expressing FLT3L (B16-FLT3L) were a provided by Dr. Andrew Sikora. Cells were cultured in DMEM containing 10% fetal calf serum and antibiotics. Mice were injected intradermally with 5–7 106 B16 or B16-FLT3L cells. The nasal DC subsets were analyzed 10–14 days later.
Nasal sample processing by mass cytometry
The entire nose from B16 or B16-FLT3L cells implanted mice were processed as described above and stained for CyTOF analysis. All CyTOF-associated reagents were purchased from Fluidigm Inc. (Sunnyvale, CA, formerly DVS Sciences). In brief, 5 million cells were stained with a panel of 20 metal-conjugated antibodies (Supplementary table 4) for 20 minutes on ice. All antibodies were either purchased pre-conjugated, or conjugated and validated in-house using MaxPar X8 conjugation kits according to the manufacturer’s protocols. The samples were then incubated for 5 minutes in cisplatin to identify dead cells, washed, and resuspended in fix/perm buffer containing Ir nucleic acid intercalator to label all nucleated cells. Immediately prior to analysis, the cells were washed in PBS and diH20 and resuspended in diH20 containing a 1:10 dilution of EQ 4 Element Calibration beads. After instrument tuning, the samples were acquired on a CyTOF2 Mass Cytometer (Fluidigm, Sunnyvale, CA) in sequential 10 minute acquisitions at a rate of <400 events/s. Following data acquisition, the FCS files were concatenated and normalized using a bead-based normalization algorithm within the CyTOF acquisition software and uploaded to Cytobank for analysis. The FCS files were manually pre-gated on Ir-193 DNA+CD45+ singlets excluding beads, doublets, DNA-negative cell debris and Pt-195 cisplatin+ dead cells. The gated population was clustered using spanning-tree progression analysis of density-normalized events (SPADE) (24). Cell populations on the SPADE trees were manually annotated on based on expression of key markers, while also preserving visualization of unidentified populations within the data set.
In vivo diphtheria toxin treatment
Diphtheria toxin (DT) purchased from Sigma–Aldrich (St. Louis, MO) was prepared in a sterile solution of PBS at a concentration of 1 mg/ml. DC depletion was effected in zDCDTR and MMDTR chimeras by a single i.p. injection of 500 ng DT. Additionally, WT bone marrow chimeras also received 500 ng DT per mouse. To analyze cell depletion, mice were euthanized 24 hr after DT injection.
In vitro DC: T cell co-cultures: Antigen presentation assays and MLR
The culture medium used for DC-T cell cultures was RPMI (Gibco, Grand Island, NY) supplemented with 10 % heat-inactivated FCS, 2 mM L-glutamine, 100 U/ml penicillin, 100 μg/ml streptomycin, and 5 mM β-mercaptoethanol (all from Sigma-Aldrich, St. Louis, MO). For antigen presentation assays, OT-II T cells (for the mixed leukocyte reaction, T cells from BALB/c spleen) were isolated from spleens of C57BL/6 mice by excluding B220+, F4/80+, CD49b+, and I-Ab+ cells with anti-rat IgG Dynabeads (Life technologies, Grand Island, NY) and labeled with 5 μM CFSE (Life technologies, Grand Island, NY) for 10 minutes at 37°C. CFSE-labeled T cells were added to round-bottom microtest wells at 5 x 104/well and mixed with isolated DCs at a DC:T cell ratio of 1:10, 1:30 and 1:100 in the presence of OVA (25 g/ml final) for antigen presentation assays. After 5 days, the proliferating T cells were evaluated by FACS.
Lipopolysaccharide administration and OVA-Alexa Fluor 488
Lipopolysaccharide (LPS) of Escherichia coli was purchased from Sigma-Aldrich (St. Louis, MO) and prepared in a sterile solution of PBS at a concentration of 1 mg/ml. OVA-Alexa Fluor 488 (Life Technologies, Grand Island, NY) was reconstituted at 15μg/μl with a sterile solution of PBS. 150 mg of OVA-Alexa Fluor 488 was co-administered with 1μg of LPS in a final volume of 11μl intranasally. Mice were sacrificed at 1h, 6h, 12h and 24h later and nasal tissues, cLN and mLN were examined for OVA+ cells.
Infection
For mCherry expressing Salmonella infection, mice were infected intranasally with 109 CFU per mouse. Where specified, 1μg pertussis toxin (List Biological Laboratories, Campbell, CA) per mouse was supplemented with Salmonella. Dr. Daniel Mucida kindly provided us with mCherry expressing Salmonella. Appearance of infected mice was monitored. Cells from the nose and cervical LNs were analyzed at 5min, 35min and 12 hrs post infection.
Statistical Analysis
Data were entered into a Microsoft Excel database and Prism 6 program (GraphPad Software, La Jolla, CA) was used for quantitative data and statistical analyses. Statistical significance was evaluated using a one-way ANOVA test followed by a post hoc Bonferroni’s test with a 95% confidence interval. Results are expressed as means ± SD. *P<0.05, ** P<0.01 or *** P<0.001 was considered to be statistically significant.
Supplementary Material
Acknowledgments
This work was inspired by Dr. Ralph Steinman. We would like to thank Dr. Maggi Pack for her help with immunofluorescent staining Dr. Michelle Gaylord for her help with tissue processing and Dr. Chae Gyu Park for valuable discussion. This work was supported by grants from the American Gastroenterology Association Elsevier Award (S.M.), The Rockefeller University Clinical and Translation science award pilot project from NIH/NCRR (5UL1RR024143-05) National Institutes of Health (S.M. and G.B- grant #8 UL 1 TR000043), The Leona M. and Harry B. Helmsley Charitable Trust, (S.M and G.B) as well as the Crohn’s & Colitis Foundation of America (S.M.)
References
- 1.Kurono Y, Yamamoto M, Fujihashi K, Kodama S, Suzuki M, Mogi G, et al. Nasal immunization induces Haemophilus influenzae-specific Th1 and Th2 responses with mucosal IgA and systemic IgG antibodies for protective immunity. J Infect Dis. 1999;180(1):122–32. doi: 10.1086/314827. [DOI] [PubMed] [Google Scholar]
- 2.Yanagita M, Hiroi T, Kitagaki N, Hamada S, Ito HO, Shimauchi H, et al. Nasopharyngeal-associated lymphoreticular tissue (NALT) immunity: fimbriae-specific Th1 and Th2 cell-regulated IgA responses for the inhibition of bacterial attachment to epithelial cells and subsequent inflammatory cytokine production. J Immunol. 1999;162(6):3559–65. [PubMed] [Google Scholar]
- 3.Sandoval F, Terme M, Nizard M, Badoual C, Bureau MF, Freyburger L, et al. Mucosal imprinting of vaccine-induced CD8(+) T cells is crucial to inhibit the growth of mucosal tumors. Sci Transl Med. 2013;5(172):172ra20. doi: 10.1126/scitranslmed.3004888. Epub 2013/02/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Langermann S, Palaszynski S, Sadziene A, Stover CK, Koenig S. Systemic and mucosal immunity induced by BCG vector expressing outer-surface protein A of Borrelia burgdorferi. Nature. 1994;372(6506):552–5. doi: 10.1038/372552a0. [DOI] [PubMed] [Google Scholar]
- 5.Velge-Roussel F, Marcelo P, Lepage AC, Buzoni-Gatel D, Bout DT. Intranasal immunization with Toxoplasma gondii SAG1 induces protective cells into both NALT and GALT compartments. Infect Immun. 2000;68(2):969–72. doi: 10.1128/iai.68.2.969-972.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruane D, Brane L, Reis BS, Cheong C, Poles J, Do Y, et al. Lung dendritic cells induce migration of protective T cells to the gastrointestinal tract. The Journal of experimental medicine. 2013;210(9):1871–88. doi: 10.1084/jem.20122762. Epub 2013/08/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gautier EL, Shay T, Miller J, Greter M, Jakubzick C, Ivanov S, et al. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat Immunol. 2012;13(11):1118–28. doi: 10.1038/ni.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imaoka K, Miller CJ, Kubota M, McChesney MB, Lohman B, Yamamoto M, et al. Nasal immunization of nonhuman primates with simian immunodeficiency virus p55gag and cholera toxin adjuvant induces Th1/Th2 help for virus-specific immune responses in reproductive tissues. J Immunol. 1998;161(11):5952–8. [PubMed] [Google Scholar]
- 9.Hiroi T, Goto H, Someya K, Yanagita M, Honda M, Yamanaka N, et al. HIV mucosal vaccine: nasal immunization with rBCG-V3J1 induces a long term V3J1 peptide-specific neutralizing immunity in Th1- and Th2-deficient conditions. J Immunol. 2001;167(10):5862–7. doi: 10.4049/jimmunol.167.10.5862. [DOI] [PubMed] [Google Scholar]
- 10.Kuper CF, Hameleers DM, Bruijntjes JP, van der Ven I, Biewenga J, Sminia T. Lymphoid and non-lymphoid cells in nasal-associated lymphoid tissue (NALT) in the rat. An immuno- and enzyme-histochemical study. Cell Tissue Res. 1990;259(2):371–7. doi: 10.1007/BF00318460. [DOI] [PubMed] [Google Scholar]
- 11.Kuper CF, Koornstra PJ, Hameleers DM, Biewenga J, Spit BJ, Duijvestijn AM, et al. The role of nasopharyngeal lymphoid tissue. Immunol Today. 1992;13(6):219–24. doi: 10.1016/0167-5699(92)90158-4. [DOI] [PubMed] [Google Scholar]
- 12.Yao Q, Vuong V, Li M, Compans RW. Intranasal immunization with SIV virus-like particles (VLPs) elicits systemic and mucosal immunity. Vaccine. 2002;20(19–20):2537–45. doi: 10.1016/s0264-410x(02)00160-3. [DOI] [PubMed] [Google Scholar]
- 13.Fukuyama S, Hiroi T, Yokota Y, Rennert PD, Yanagita M, Kinoshita N, et al. Initiation of NALT organogenesis is independent of the IL-7R, LTbetaR, and NIK signaling pathways but requires the Id2 gene and CD3(−)CD4(+)CD45(+) cells. Immunity. 2002;17(1):31–40. doi: 10.1016/s1074-7613(02)00339-4. [DOI] [PubMed] [Google Scholar]
- 14.Lindquist RL, Shakhar G, Dudziak D, Wardemann H, Eisenreich T, Dustin ML, et al. Visualizing dendritic cell networks in vivo. Nat Immunol. 2004;5(12):1243–50. doi: 10.1038/ni1139. [DOI] [PubMed] [Google Scholar]
- 15.Wu Y, Wang X, Csencsits KL, Haddad A, Walters N, Pascual DW. M cell-targeted DNA vaccination. Proc Natl Acad Sci U S A. 2001;98(16):9318–23. doi: 10.1073/pnas.161204098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong KI, Suzuki H, Nakayama H, Doi K. Ultrastructural study on the follicle-associated epithelium of nasal-associated lymphoid tissue in specific pathogen-free (SPF) and conventional environment-adapted (SPF-CV) rats. J Anat. 2000;196 (Pt 3):443–51. doi: 10.1046/j.1469-7580.2000.19630443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spit BJ, Hendriksen EG, Bruijntjes JP, Kuper CF. Nasal lymphoid tissue in the rat. Cell Tissue Res. 1989;255(1):193–8. doi: 10.1007/BF00229081. [DOI] [PubMed] [Google Scholar]
- 18.Nagatake T, Fukuyama S, Kim DY, Goda K, Igarashi O, Sato S, et al. Id2-, RORgammat-, and LTbetaR-independent initiation of lymphoid organogenesis in ocular immunity. J Exp Med. 2009;206(11):2351–64. doi: 10.1084/jem.20091436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sosa GA, Roux ME. Development of T lymphocytes in the nasal-associated lymphoid tissue (NALT) from growing Wistar rats. Clin Dev Immunol. 2004;11(1):29–34. doi: 10.1080/10446670410001670463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costalonga M, Cleary PP, Fischer LA, Zhao Z. Intranasal bacteria induce Th1 but not Treg or Th2. Mucosal Immunol. 2009;2(1):85–95. doi: 10.1038/mi.2008.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiyono H, Fukuyama S. NALT- versus Peyer’s-patch-mediated mucosal immunity. Nature reviews Immunology. 2004;4(9):699–710. doi: 10.1038/nri1439. Epub 2004/09/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartmann E, Graefe H, Hopert A, Pries R, Rothenfusser S, Poeck H, et al. Analysis of plasmacytoid and myeloid dendritic cells in nasal epithelium. Clin Vaccine Immunol. 2006;13(11):1278–86. doi: 10.1128/CVI.00172-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heritage PL, Underdown BJ, Arsenault AL, Snider DP, McDermott MR. Comparison of murine nasal-associated lymphoid tissue and Peyer’s patches. Am J Respir Crit Care Med. 1997;156(4 Pt 1):1256–62. doi: 10.1164/ajrccm.156.4.97-03017. [DOI] [PubMed] [Google Scholar]
- 24.Qiu P, Simonds EF, Bendall SC, Gibbs KD, Jr, Bruggner RV, Linderman MD, et al. Extracting a cellular hierarchy from high-dimensional cytometry data with SPADE. Nat Biotechnol. 2011;29(10):886–91. doi: 10.1038/nbt.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307(5707):254–8. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- 26.Jakubzick C, Gautier EL, Gibbings SL, Sojka DK, Schlitzer A, Johnson TE, et al. Minimal differentiation of classical monocytes as they survey steady-state tissues and transport antigen to lymph nodes. Immunity. 2013;39(3):599–610. doi: 10.1016/j.immuni.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392(6673):245–52. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 28.Liu YJ, Kanzler H, Soumelis V, Gilliet M. Dendritic cell lineage, plasticity and cross-regulation. Nat Immunol. 2001;2(7):585–9. doi: 10.1038/89726. [DOI] [PubMed] [Google Scholar]
- 29.Kataoka K, Fujihashi K, Oma K, Fukuyama Y, Hollingshead SK, Sekine S, et al. The nasal dendritic cell-targeting Flt3 ligand as a safe adjuvant elicits effective protection against fatal pneumococcal pneumonia. Infect Immun. 2011;79(7):2819–28. doi: 10.1128/IAI.01360-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nacer A, Carapau D, Mitchell R, Meltzer A, Shaw A, Frevert U, et al. Imaging murine NALT following intranasal immunization with flagellin-modified circumsporozoite protein malaria vaccines. Mucosal Immunol. 2014;7(2):304–14. doi: 10.1038/mi.2013.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tamoutounour S, Guilliams M, Montanana Sanchis F, Liu H, Terhorst D, Malosse C, et al. Origins and functional specialization of macrophages and of conventional and monocyte-derived dendritic cells in mouse skin. Immunity. 2013;39(5):925–38. doi: 10.1016/j.immuni.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 32.Schlitzer A, McGovern N, Teo P, Zelante T, Atarashi K, Low D, et al. IRF4 transcription factor-dependent CD11b+ dendritic cells in human and mouse control mucosal IL-17 cytokine responses. Immunity. 2013;38(5):970–83. doi: 10.1016/j.immuni.2013.04.011. Epub 2013/05/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kataoka K, McGhee JR, Kobayashi R, Fujihashi K, Shizukuishi S, Fujihashi K. Nasal Flt3 ligand cDNA elicits CD11c+CD8+ dendritic cells for enhanced mucosal immunity. J Immunol. 2004;172(6):3612–9. doi: 10.4049/jimmunol.172.6.3612. [DOI] [PubMed] [Google Scholar]
- 34.Jakubzick C, Helft J, Kaplan TJ, Randolph GJ. Optimization of methods to study pulmonary dendritic cell migration reveals distinct capacities of DC subsets to acquire soluble versus particulate antigen. J Immunol Methods. 2008;337(2):121–31. doi: 10.1016/j.jim.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maraskovsky E, Brasel K, Teepe M, Roux ER, Lyman SD, Shortman K, et al. Dramatic increase in the numbers of functionally mature dendritic cells in Flt3 ligand-treated mice: multiple dendritic cell subpopulations identified. J Exp Med. 1996;184(5):1953–62. doi: 10.1084/jem.184.5.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fukuiwa T, Sekine S, Kobayashi R, Suzuki H, Kataoka K, Gilbert RS, et al. A combination of Flt3 ligand cDNA and CpG ODN as nasal adjuvant elicits NALT dendritic cells for prolonged mucosal immunity. Vaccine. 2008;26(37):4849–59. doi: 10.1016/j.vaccine.2008.06.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Varmus H, Klausner R, Zerhouni E, Acharya T, Daar AS, Singer PA. Public health. Grand Challenges in Global Health. Science. 2003;302(5644):398–9. doi: 10.1126/science.1091769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bendall SC, Simonds EF, Qiu P, Amir el AD, Krutzik PO, Finck R, et al. Single-cell mass cytometry of differential immune and drug responses across a human hematopoietic continuum. Science. 2011;332(6030):687–96. doi: 10.1126/science.1198704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meredith MM, Liu K, Darrasse-Jeze G, Kamphorst AO, Schreiber HA, Guermonprez P, et al. Expression of the zinc finger transcription factor zDC (Zbtb46, Btbd4) defines the classical dendritic cell lineage. J Exp Med. 2012;209(6):1153–65. doi: 10.1084/jem.20112675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Satpathy AT, Kc W, Albring JC, Edelson BT, Kretzer NM, Bhattacharya D, et al. Zbtb46 expression distinguishes classical dendritic cells and their committed progenitors from other immune lineages. J Exp Med. 2012;209(6):1135–52. doi: 10.1084/jem.20120030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schreiber HA, Loschko J, Karssemeijer RA, Escolano A, Meredith MM, Mucida D, et al. Intestinal monocytes and macrophages are required for T cell polarization in response to Citrobacter rodentium. J Exp Med. 2013;210(10):2025–39. doi: 10.1084/jem.20130903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Steinman RM, Witmer MD. Lymphoid dendritic cells are potent stimulators of the primary mixed leukocyte reaction in mice. Proc Natl Acad Sci U S A. 1978;75(10):5132–6. doi: 10.1073/pnas.75.10.5132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J Exp Med. 1973;137(5):1142–62. doi: 10.1084/jem.137.5.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jabbal-Gill I, Watts P, Smith A. Chitosan-based delivery systems for mucosal vaccines. Expert Opin Drug Deliv. 2012;9(9):1051–67. doi: 10.1517/17425247.2012.697455. [DOI] [PubMed] [Google Scholar]
- 45.Nochi T, Yuki Y, Takahashi H, Sawada S, Mejima M, Kohda T, et al. Nanogel antigenic protein-delivery system for adjuvant-free intranasal vaccines. Nat Mater. 2010;9(7):572–8. doi: 10.1038/nmat2784. [DOI] [PubMed] [Google Scholar]
- 46.Bogunovic M, Ginhoux F, Helft J, Shang L, Hashimoto D, Greter M, et al. Origin of the lamina propria dendritic cell network. Immunity. 2009;31(3):513–25. doi: 10.1016/j.immuni.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sekine S, Kataoka K, Fukuyama Y, Adachi Y, Davydova J, Yamamoto M, et al. A novel adenovirus expressing Flt3 ligand enhances mucosal immunity by inducing mature nasopharyngeal-associated lymphoreticular tissue dendritic cell migration. J Immunol. 2008;180(12):8126–34. doi: 10.4049/jimmunol.180.12.8126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jahnsen FL, Gran E, Haye R, Brandtzaeg P. Human nasal mucosa contains antigen-presenting cells of strikingly different functional phenotypes. Am J Respir Cell Mol Biol. 2004;30(1):31–7. doi: 10.1165/rcmb.2002-0230OC. Epub 2003/06/28. [DOI] [PubMed] [Google Scholar]
- 49.Takano K, Kojima T, Go M, Murata M, Ichimiya S, Himi T, et al. HLA-DR- and CD11c-positive dendritic cells penetrate beyond well-developed epithelial tight junctions in human nasal mucosa of allergic rhinitis. J Histochem Cytochem. 2005;53(5):611–9. doi: 10.1369/jhc.4A6539.2005. Epub 2005/05/06. [DOI] [PubMed] [Google Scholar]
- 50.Ing R, Segura M, Thawani N, Tam M, Stevenson MM. Interaction of mouse dendritic cells and malaria-infected erythrocytes: uptake, maturation, and antigen presentation. J Immunol. 2006;176(1):441–50. doi: 10.4049/jimmunol.176.1.441. Epub 2005/12/21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.