Abstract
Objectives
This paper reviews organizational and social issues (OSIs) in health information technology (HIT).
Methods
A review and synthesis of the literature on OSIs in HIT was conducted.
Results
Five overarching themes with respect to OSIs in HIT were identified and discussed: scope and frameworks for defining OSIs in HIT, context matters, process immaturity and complexity, trade-offs will happen and need to be discussed openly, and means of studying OSIs in HIT.
Conclusions
There is a wide body of literature that provides insight into OSIs in HIT, even if many of the studies are not explicitly labelled as such. The two biggest research needs are more explicit and theoretical studies of OSI in HITs and more research on integrating micro and macro perspectives of HIT use in organizations.
Keywords: Organizations, Social Norms, Health Information Technology, Process Assessment (Health Care), Collaboration
I. Introduction
Over the past two decades, there have been numerous calls worldwide to reform and innovate healthcare delivery to meet objectives, such as the provision of collaborative, safe, patient centered care [1,2]. Heath information technology (HIT) will play a key role in facilitating healthcare delivery to meet these objectives [3,4,5,6]. Studies have described positive outcomes from HIT, including support for the management of chronic diseases, facilitation of communication as part of care transitions, and improvements in patient safety by providing necessary information to all providers [7,8]. There is also a wide body of research that describes numerous challenges to implementing HIT in organizations, including workflow, communication and cognitive issues, and medical errors that are mitigated by the use of HIT [9,10,11,12]. Further, studies have reported that HIT adoption has had minimal impact on the quality of care, measured by patient mortality, adverse drug events, and readmission rates [13].
Yet, despite the implementation issues, governments continue to spend large amounts of money on the adoption of HIT [14]. Organizational and social issues (OSIs) contribute to HIT implementation issues [10,11,15,16]. While some studies have explicitly studied or discussed OSIs in HIT [15,16,17,18,19], much of the research on OSIs has been imbedded in studies of post-implementation issues, such as unintended consequences and adverse events [9,10,11,12]. One essential point that needs to be made is that even if the HIT in question adequately automates the task it was designed for (e.g., order entry), unintended consequences may still occur due to conflicts between the HIT and the context of how and where the system is used [9,10].
Overall, there is a need for better understanding of the organizational issues surrounding HIT implementation [16]. One of the biggest challenges in studying OSIs is what can be referred to as 'bounding'. Such a wide range of studies have reported on OSIs that it becomes challenging to identify what elements should be studied and how studies should be conducted. Healthcare systems continue to focus on goals such as patient safety, collaborative care delivery, and patient centered care, yet an often overlooked fact is that these goals are bound within the organizational and social web that exists in healthcare settings. There is a need for a paper that reviews the wide body of literature on OSIs in HIT to provide some bounding for how to think about and study these issues. This paper addresses that need by reviewing the literature on OSIs in HIT to identify themes that can be used to provide bounding for future research.
II. Methodology
This paper presents a non-systematic literature review of OSIs in HIT. The papers reviewed included explicit studies about OSIs in HIT (e.g., review articles) as well as papers that referred to OSIs in HIT in the context of other studies (e.g., unintended consequences, medical errors, collaborative care delivery). In reviewing the papers, five overarching themes around OSIs in HIT were identified: scope and frameworks for defining OSIs in HIT, context matters, process immaturity and complexity, trade-offs will happen and need to be openly discussed, and means of studying OSIs in HIT. To provide some framing for the discussion, each theme is discussed from the perspective of micro and macro aspects of OSIs. Macro aspects include organizational structure, leadership, incentives, training, and organizational structure (e.g., facility size, IT spending). Micro aspects include front-line care delivery issues, such as communication, collaboration or training for HIT usage. Each theme is discussed in the next section.
III. Results
1. Theme One - Scope and Frameworks for Defining OSIs in HIT
As stated in the introduction, a significant challenge in studying OSIs in HIT is defining them, given the range of studies that have reported on OSIs. On one hand, OSIs have been studied using broad approaches or frameworks, such as those from classic studies of information technology in organizations [20]. An interpretive review by Cresswell and Sheikh [16] points out the range of models used to study OSIs in HIT, such as the technology adoption model (TAM) [21], the diffusion of innovation model [22], and organizational psychology models [23]. Other models from the information systems literature that have been used to evaluate HIT include the DeLone and McLean information system success model [24,25]. A literature review by Lluch [15] identified and classified organizational barriers and HIT under five main headings: structure of healthcare organizations, tasks, people policies, incentives, and information and decision processes. It was proposed that the five categories be used as a starting point for policy interventions.
While the above reviews and models are good at identifying the broader structural or macro aspects of HIT in OSIs, they do not provide as much insight into the behavioral or micro aspects of OSIs, yet behavioral issues are a major cause of HIT issues and often span across individual, group, and organizational levels [26]. A significant amount of research has looked at micro-level intricacies between HIT and the organizations where they are used [10,12,27,28,29]. While studies may not be explicitly labeled as studies on OSIs in HIT, many of their findings refer to aspects of OSIs. A seminal work by Ash et al. [9] identified the presence and significance of unintended consequence post-HIT implementation. The plethora of studies on the unintended consequences of HIT implementation emphasizes that even a well-designed system can be influenced by organizational culture and issues, such as power struggles. Research drawing upon socio-technical theory has been used to study HIT for some time and has provided valuable insight on HIT in OSIs [30,31]. A sociotechnical framework was developed by Sittig and Singh [32] that articulates eight dimensions for studying the safety and effectiveness of HIT, including organizational policies and procedures. Others have suggested that while organizational structure and leadership are important for HIT success, it is equally important that culture, workflow, and productivity be studied [33]. Some models have made explicit attempts to provide insights into organizational aspects and HIT. For example, Ancker et al. [34] developed the 'triangle evaluation model', which incorporates the organizational structure, processes pertaining to organizational implementation of technology, and organizational policies affecting providers.
2. Theme Two - Context Matters
Macro-level solutions are impacted by the micro-level context where they are implemented. A systematic review of HIT implementation identified better reporting of context as the biggest need in HIT evaluation [35]. Novak et al. [36] provide a good perspective on the importance of context by differentiating the ideal or abstract description (the ostensive dimension) of how HIT should be used and how it is actually used in real clinical settings (the performance dimension). The performance dimension is defined by context, and failure to account for the ostensive-performance gap can lead to unintended consequences, such as communication, coordination, and patient safety issues [14,37]. A key part of understanding the performance dimension is understanding the intersection of organizational routines and technology [36]. While evaluation approaches, such as usability testing, can identify individual variations or contexts, it is equally important to understand organizational contexts, such as leadership, culture, and workflow, as they can impact HIT usage [38].
There are several types of organizational contexts that need to be considered. One context is the type of organization, as HIT implementation can vary according to the size and type of organization where HIT is being implemented [39,40]. Another context is training. While training on the specific features of the HIT being used is obviously important, it is equally important that organizations invest in training on technical skill sets (e.g., information management skills, such as data entry and retrieval) that are necessary for effective interaction with HIT [41,42]. Another context is the care delivery setting where the HIT will be used. Collaborative or team settings require different HIT design considerations than designing for individual providers [43,44].
A shortcoming of many of the IT adoption frameworks described in the previous section, such as TAM, is that they focus on behavior related to the technology and not the organizational or clinical context where the technology is used [45]. To address this shortcoming, models of HIT implementation have been developed that attempt to incorporate the macro (organizational) and micro (clinical) context. One such model is the contextual implementation model (CIM), which looks at HIT usage from organizational, clinical unit, and individual contexts [45].
3. Theme Three - Process Immaturity and Complexity
HIT implementation is often compared to other industries, such as finance, aviation, or manufacturing. While IT has been able to improve supply chain efficiency in companies like Wal-Mart [46], and it has enabled courier companies to develop online customer package tracking systems, a key difference between these domains and healthcare is that supply chain management and parcel delivery are mature processes; therefore, the technology was used to automate well-defined processes.
A major challenge is that many of the healthcare organizational processes we are trying to automate lack maturity. For example, while numerous interventions have been proposed to improve team-based care delivery, including training and the use of technologies such as Electronic Health Records [44,47], these macro-level interventions have not resulted in improved outcomes. It has been stated that if a care team lacks team characteristics (e.g., shared objectives and processes) than they exist as teamwork in name only [48]. Poorly defined teams provide less than ideal team-based care delivery, leading to adverse events, such as communication issues and medical errors [49,50]. While there have been mixed reports about the ability of HIT to support teamwork [43,51], HIT on its own will not enhance team-based care delivery; rather, we need a better definition of the rules of engagement and the relationship between teamwork and individual provider work routines [52,53]. Handovers are another example of processes that can be classified as evolving [54,55]. A lack of standardized handover processes has been cited as a reason for errors and other quality issues related to handovers [56]. Essential elements for handoffs, such as common ground amongst providers, are still a work in progress [57]. Poorly defined handover processes and measures make it challenging to develop HIT to support handovers.
Another consideration is the manner in which organizational processes are connected. While HIT may be designed to automate a specific task, it will impact and be impacted by other organizational and clinical tasks [58]. A well acknowledged shortcoming in how we design HIT is a focus on "tidy use cases of predictable orderliness" which fail to describe the complex interrelated manner in which HIT is used [12]. Rather than considering HIT as isolated events or activities, we need to draw upon systems theory and consider HIT and the processes it supports as complex entities [59]. HIT is more likely to introduce unintended consequences if it designed to support specific tasks while ignoring other tasks or routines that interact with it [36,60]. Tenets of complexity theory, such as emergence, non-linearity, and self-organization can help us understand the inter-relatedness between HIT and the processes, policies, and other system components that interact with a HIT [59].
4. Theme Four - Trade-offs Will Happen and Need to Be Openly Discussed
HIT implementation often necessitates trade-offs between how people currently work and how their work routines change because of HIT [36,61,62]. However, providers may be unwilling to make trade-offs, or they may find trade-offs problematic to their work practices, and as a result develop workarounds to mitigate HIT-mediated changes [12,29]. A significant trade-off is the individual-collaborative interchange. While systems may be designed to support individual or organizational tasks, designing for groups is a different challenge [63]. Macro-level objectives, such as collaborative care delivery, necessitate trade-offs at the individual-collaborative interchange and across clinical units, change individual roles in the context of working in a team, and may require the development of awareness or rules of engagement for social or group dynamics [52,53,64].
While standardization of data and processes is required for interoperability to support inter- and intra-organizational care delivery, it can introduce several types of trade-offs. Standardized data may lead to increased charting for providers, which can require a workflow trade-off with respect to patient care delivery [65,66]. Tasks such as communication, information retrieval, or decision-making may become more challenging because of HIT [10]. At times, it may not be possible to perform tasks in the same manner with HIT, and providers may be forced to learn new variations on tasks [12].
In addition to the need to understand HIT mediated trade-offs, there is the need to effectively manage them. Some of the changes may be flexible and can be negotiated as part of HIT design, whereas others (e.g., data standards or organizational policy) are more permanent. Failure to discuss HIT-induced changes can result in adverse events and other unintended consequences because of individual variations on processes. The nature of trade-offs and/or losses to work practices from HIT need to be discussed and, if applicable, negotiated with providers [67,68].
5. Theme Five - Means of Studying OSIs in HIT
Several approaches have been used to study OSIs in HIT. Kaplan has advocated for methodological pluralism, emphasizing the need for broad approaches to HIT evaluation that study social, cultural, organizational, cognitive, and other contextual concerns [69]. Both qualitative and quantitative approaches have been used to study OSIs in HIT. Quantitative studies are helpful for providing the macro or structural perspective. Such studies have included the use of Markov models, simulation, and multi-agent models [70,71,72]. Quantitative studies can also be used to define structural aspects of work processes, such as communication flows or patterns, to model how things should work. For example, Grando et al. [73] developed patterns to understand collaborative practices.
While quantitative studies are helpful for providing bounding or structure regarding OSIs in HIT, a shortcoming of quantitative approaches is that they decontextualize situations and thus may not sufficiently explain why things happen [74]. As described above, a lack of rules of engagement for team-based care delivery may cause a seemingly ideal collaboration structure to work in unintended ways. Qualitative approaches, such as non-participant observations, interviews, and focus groups, have been valuable for studying and providing explanations about the organizational context of OSIs in HIT [75,76]. An advantage of qualitative studies is their ability to provide rich descriptions of situation, particularly the micro aspects regarding why things happen [10,77].
Although there has been a wide variety of approaches to studying HIT that have come directly from the medical informatics community, we need to remember that the broader discipline of information systems also offers many approaches and frameworks that can be used in studying OSIs in HIT [78]. Furthermore, fields peripheral to medical informatics, such as computer-supported cooperative work (CSCW), have also made significant contributions to our understanding of the relationship between OSIs in HIT [79,80].
Regardless of the type of approach used, an iterative approach that engages users will increase the chance of understanding OSIs as a precursor to successful HIT design and implementation. Methods such as design science and participatory design provide ways to engage users in the understanding of problems and the design of HIT solutions to these problems [81,82,83].
IV. Discussion
Although HIT continues to play a vital role in healthcare delivery, successful implementation of HIT remains a challenge. This paper reviewed OSIs in HIT and identified five themes to help us better understand and study OSIs in HIT. One overall finding is that, while organizations frequently have strategies for macro-level objectives, such as patient safety, systems integration, collaborative care delivery, and chronic disease management, these efforts need to be studied and integrated with the underlying micro processes that operationalize the objectives. Even a well-designed HIT may not function as intended because of OSIs. One of the key issues identified in this paper is the need to account for immature or evolving processes. While HIT introduces a sudden and often substantial change to how work is done, the processes being automated by HIT may not evolve as quickly. As a result, unintended consequences occur because of the gap between the level of automation and the people and processes using the automation. Defining rules of engagement for tasks such as collaborative care delivery, or handovers, needs to be done prior to automation of these tasks.
While we need to continue research on macro-level OSIs, such as leadership, funding, and organizational structure, these studies need to be complemented by research on OSIs at the micro level. Organizational strategy and policy may define the framework of healthcare delivery, but it is the social and behavioral aspects at the micro level that will define the activities within the framework. We also need to move away from studies that look broadly at OSIs; rather, we need to focus our research efforts on specific contexts of OSIs. For example, Dorr et al. [43] pointed out that HIT is often not designed to explicitly support collaboration. Therefore, there is a specific research need to define the collaborative behaviors and rules of engagement that HIT needs to support. Another context is the organizational setting or type. As more healthcare delivery, and subsequently more HIT, occurs outside traditional healthcare settings (e.g., in patient homes, long-term care centers) we need better evidence on how to design and evaluate HIT to support care delivery in these contexts.
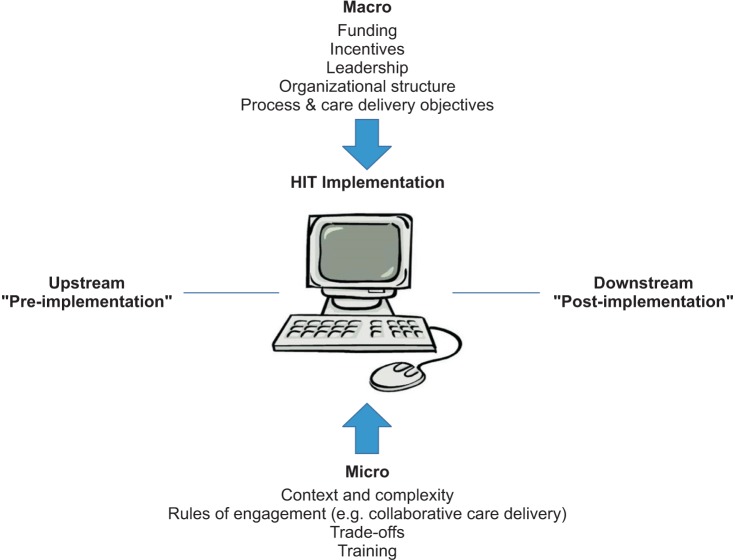
Figure 1 summarizes the findings of this paper. It shows how OSIs need to be studied from micro and macro perspectives, both upstream and downstream, as part of HIT implementation. Macro considerations include the funding, incentives, leadership, organizational structure, and process or care delivery objectives. Micro considerations include the context and complexity of HIT usage, rules of engagement, and training and trade-offs. 'Upstream' refers to HIT design and development prior to the actual implementation of HIT. 'Downstream' refers to the operations and maintenance that take place after HIT is implemented. It is essential that both micro and macro perspectives are studied upstream (i.e., pre-implementation) as well as downstream (i.e., post-implementation) because of the dynamic and evolving nature of healthcare processes. Further, HIT users need to be involved as much as possible to enable to them to understand the nature of HIT-induced changes and how it will impact their work routines.
Figure 1. Model for upstream and downstream study of micro and macro aspects of OSIs as part of HIT implementation. OSI: organizational and social issue, HIT: health information technology.
One of the other conclusions from this work is that OSIs cannot be studied from the perspective of linear modeling of ideal scenarios; rather, they must be studied from the perspective of the messy and complex reality in which HIT is situated. In that context the toolbox for studying OSIs may be richer than people realize. In addition to the frameworks and methods from medical informatics, insights may be gained through a wide array of approaches from the information systems discipline, such as Peter Checkland's Soft Systems Methodology [84] and the technological frames approach of Orlikowski and Gash [85], and approaches from the social sciences, such as Activity Theory and Actor Network Theory [86,87].
V. Conclusion
As HIT is more widely implemented in healthcare settings, it is essential that we ensure HIT is a fit in the organizational setting where it will be used. This paper reviewed OSIs in HIT and identified five themes to provide guidance and bounding for future research. Echoing other studies [16], the findings from this paper suggest that there is a key need for more explicit and theoretical studies of OSIs in HIT. More research on integrating micro and macro perspectives of HIT use in organizations is also a priority need.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Institute of Medicine. Health IT and patient safety: building safer systems for better care. Washington (DC): National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press; 2001. [PubMed] [Google Scholar]
- 3.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526–2534. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 4.Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007;14(1):29–40. doi: 10.1197/jamia.M2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coiera E. Building a National Health IT System from the middle out. J Am Med Inform Assoc. 2009;16(3):271–273. doi: 10.1197/jamia.M3183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stead WW, Lin HS. Computational technology for effective health care: immediate steps and strategic directions. Washington (DC): National Academies Press; 2009. [PubMed] [Google Scholar]
- 7.Rao S, Brammer C, McKethan A, Buntin MB. Health information technology: transforming chronic disease management and care transitions. Prim Care. 2012;39(2):327–344. doi: 10.1016/j.pop.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 8.McKibbon KA, Lokker C, Handler SM, Dolovich LR, Holbrook AM, O'Reilly D, et al. The effectiveness of integrated health information technologies across the phases of medication management: a systematic review of randomized controlled trials. J Am Med Inform Assoc. 2012;19(1):22–30. doi: 10.1136/amiajnl-2011-000304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 2007;76(Suppl 1):S21–S27. doi: 10.1016/j.ijmedinf.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 10.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11(2):104–112. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borycki E. Trends in health information technology safety: from technology-induced errors to current approaches for ensuring technology safety. Healthc Inform Res. 2013;19(2):69–78. doi: 10.4258/hir.2013.19.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith SW, Koppel R. Healthcare information technology's relativity problems: a typology of how patients' physical reality, clinicians' mental models, and healthcare information technology differ. J Am Med Inform Assoc. 2014;21(1):117–131. doi: 10.1136/amiajnl-2012-001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agha L. The effects of health information technology on the costs and quality of medical care. J Health Econ. 2014;34:19–30. doi: 10.1016/j.jhealeco.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coiera E, Aarts J, Kulikowski C. The dangerous decade. J Am Med Inform Assoc. 2012;19(1):2–5. doi: 10.1136/amiajnl-2011-000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lluch M. Healthcare professionals' organisational barriers to health information technologies: a literature review. Int J Med Inform. 2011;80(12):849–862. doi: 10.1016/j.ijmedinf.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int J Med Inform. 2013;82(5):e73–e86. doi: 10.1016/j.ijmedinf.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Ash J. Organizational factors that influence information technology diffusion in academic health sciences centers. J Am Med Inform Assoc. 1997;4(2):102–111. doi: 10.1136/jamia.1997.0040102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lorenzi NM, Riley RT, Blyth AJ, Southon G, Dixon BJ. Antecedents of the people and organizational aspects of medical informatics: review of the literature. J Am Med Inform Assoc. 1997;4(2):79–93. doi: 10.1136/jamia.1997.0040079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplan B. Addressing organizational issues into the evaluation of medical systems. J Am Med Inform Assoc. 1997;4(2):94–101. doi: 10.1136/jamia.1997.0040094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chae YM. Management issues in healthcare information technology. Healthc Inform Res. 2012;18(2):85–87. doi: 10.4258/hir.2012.18.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yarbrough AK, Smith TB. Technology acceptance among physicians: a new take on TAM. Med Care Res Rev. 2007;64(6):650–672. doi: 10.1177/1077558707305942. [DOI] [PubMed] [Google Scholar]
- 22.Rogers EM. Diffusion of innovations. New York (NY): Free Press; 1983. [Google Scholar]
- 23.Karsten R, Schmidt D. Social psychology for IT professionals: a proposed model. Acad Inf Manag Sci. 2004;8(1):37. [Google Scholar]
- 24.Bossen C, Jensen LG, Udsen FW. Evaluation of a comprehensive EHR based on the DeLone and McLean model for IS success: approach, results, and success factors. Int J Med Inform. 2013;82(10):940–953. doi: 10.1016/j.ijmedinf.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Delone WH, McLean ER. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst. 2003;19(4):9–30. [Google Scholar]
- 26.Kukafka R, Johnson SB, Linfante A, Allegrante JP. Grounding a new information technology implementation framework in behavioral science: a systematic analysis of the literature on IT use. J Biomed Inform. 2003;36(3):218–227. doi: 10.1016/j.jbi.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 28.Balka E, Doyle-Waters M, Lecznarowicz D, FitzGerald JM. Technology, governance and patient safety: systems issues in technology and patient safety. Int J Med Inform. 2007;76(Suppl 1):S35–S47. doi: 10.1016/j.ijmedinf.2006.05.046. [DOI] [PubMed] [Google Scholar]
- 29.Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care: an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549. doi: 10.1197/jamia.M2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform. 2001;64(2-3):143–156. doi: 10.1016/s1386-5056(01)00200-3. [DOI] [PubMed] [Google Scholar]
- 31.Berg M, Aarts J, van der Lei J. ICT in health care: sociotechnical approaches. Methods Inf Med. 2003;42(4):297–301. [PubMed] [Google Scholar]
- 32.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(Suppl 3):i68–i74. doi: 10.1136/qshc.2010.042085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meeks DW, Takian A, Sittig DF, Singh H, Barber N. Exploring the sociotechnical intersection of patient safety and electronic health record implementation. J Am Med Inform Assoc. 2014;21(e1):e28–e34. doi: 10.1136/amiajnl-2013-001762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ancker JS, Kern LM, Abramson E, Kaushal R. The Triangle Model for evaluating the effect of health information technology on healthcare quality and safety. J Am Med Inform Assoc. 2012;19(1):61–65. doi: 10.1136/amiajnl-2011-000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karsh BT, Weinger MB, Abbott PA, Wears RL. Health information technology: fallacies and sober realities. J Am Med Inform Assoc. 2010;17(6):617–623. doi: 10.1136/jamia.2010.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Novak L, Brooks J, Gadd C, Anders S, Lorenzi N. Mediating the intersections of organizational routines during the introduction of a health IT system. Eur J Inf Syst. 2012;21(5):1–31. doi: 10.1057/ejis.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borycki EM, Kushniruk AW, Bellwood P, Brender J. Technology-induced errors: the current use of frameworks and models from the biomedical and life sciences literatures. Methods Inf Med. 2012;51(2):95–103. doi: 10.3414/ME11-02-0009. [DOI] [PubMed] [Google Scholar]
- 38.Doran D, Haynes BR, Estabrooks CA, Kushniruk A, Dubrowski A, Bajnok I, et al. The role of organizational context and individual nurse characteristics in explaining variation in use of information technologies in evidence based practice. Implement Sci. 2012;7:122. doi: 10.1186/1748-5908-7-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Furukawa MF, King J, Patel V, Hsiao CJ, Adler-Milstein J, Jha AK. Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood) 2014;33(9):1672–1679. doi: 10.1377/hlthaff.2014.0445. [DOI] [PubMed] [Google Scholar]
- 40.Pare G, Raymond L, de Guinea AO, Poba-Nzaou P, Trudel MC, Marsan J, et al. Barriers to organizational adoption of EMR systems in family physician practices: a mixed-methods study in Canada. Int J Med Inform. 2014;83(8):548–558. doi: 10.1016/j.ijmedinf.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 41.Villalba-Mora E, Casas I, Lupianez-Villanueva F, Maghiros I. Adoption of health information technologies by physicians for clinical practice: the Andalusian case. Int J Med Inform. 2015;84(7):477–485. doi: 10.1016/j.ijmedinf.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Gonen A, Sharon D, Offir A, Lev-Ari L. How to enhance nursing students' intention to use information technology: the first step before integrating it in nursing curriculum. Comput Inform Nurs. 2014;32(6):286–293. doi: 10.1097/CIN.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 43.Dorr D, Bonner LM, Cohen AN, Shoai RS, Perrin R, Chaney E, et al. Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc. 2007;14(2):156–163. doi: 10.1197/jamia.M2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Collins SA, Bakken S, Vawdrey DK, Coiera E, Currie L. Model development for EHR interdisciplinary information exchange of ICU common goals. Int J Med Inform. 2011;80(8):e141–e149. doi: 10.1016/j.ijmedinf.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Callen JL, Braithwaite J, Westbrook JI. Contextual implementation model: a framework for assisting clinical information system implementations. J Am Med Inform Assoc. 2008;15(2):255–262. doi: 10.1197/jamia.M2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nash K. Wal-Mart builds supply chain to meet e-commerce demands [Internet] New York (NY): The Wall Street Journal; c2015. [cited at 2015 Jul 10]. Available from: http://www.wsj.com/articles/wal-mart-builds-supply-chain-to-meet-e-commerce-demands-1431016708. [Google Scholar]
- 47.O'Leary KJ, Sehgal NL, Terrell G, Williams MV High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2012;7(1):48–54. doi: 10.1002/jhm.970. [DOI] [PubMed] [Google Scholar]
- 48.West MA, Lyubovnikova J. Illusions of team working in health care. J Health Organ Manag. 2013;27(1):134–142. doi: 10.1108/14777261311311843. [DOI] [PubMed] [Google Scholar]
- 49.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(Suppl 1):i85–i90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kuziemsky CE, Varpio L. A model of awareness to enhance our understanding of interprofessional collaborative care delivery and health information system design to support it. Int J Med Inform. 2011;80(8):e150–e160. doi: 10.1016/j.ijmedinf.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 51.Reddy MC, Shabot MM, Bradner E. Evaluating collaborative features of critical care systems: a methodological study of information technology in surgical intensive care units. J Biomed Inform. 2008;41(3):479–487. doi: 10.1016/j.jbi.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 52.Reddy MC, Spence PR. Collaborative information seeking: a field study of a multidisciplinary patient care team. Inf Process Manag. 2008;44(1):242–255. [Google Scholar]
- 53.Kuziemsky CE, Bush P. Coordination considerations of healthcare information technology. Stud Health Technol Inform. 2013;194:133–138. [PubMed] [Google Scholar]
- 54.Abraham J, Kannampallil TG, Patel VL. Bridging gaps in handoffs: a continuity of care based approach. J Biomed Inform. 2012;45:240–254. doi: 10.1016/j.jbi.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 55.Wong MC, Turner P, Yee KC. Clinical handover improvement in context: exploring tensions between usercentred approaches and standardisation. Stud Health Technol Inform. 2013;194:48–53. [PubMed] [Google Scholar]
- 56.Abraham J, Kannampallil T, Patel VL. A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014;21(1):154–162. doi: 10.1136/amiajnl-2012-001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Collins SA, Mamykina L, Jordan D, Stein DM, Shine A, Reyfman P, et al. In search of common ground in hand-off documentation in an Intensive Care Unit. J Biomed Inform. 2012;45(2):307–315. doi: 10.1016/j.jbi.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Coiera E. Interaction design theory. Int J Med Inform. 2003;69(2-3):205–222. doi: 10.1016/s1386-5056(02)00106-5. [DOI] [PubMed] [Google Scholar]
- 59.Kannampallil TG, Schauer GF, Cohen T, Patel VL. Considering complexity in healthcare systems. J Biomed Inform. 2011;44(6):943–947. doi: 10.1016/j.jbi.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 60.Howard-Grenville JA. The persistence of flexible organizational routines: the role of agency and organizational context. Organ Sci. 2005;16(6):618–636. [Google Scholar]
- 61.Braithwaite J, Westbrook J, Iedema R. Restructuring as gratification. J R Soc Med. 2005;98(12):542–544. doi: 10.1258/jrsm.98.12.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bloomrosen M, Starren J, Lorenzi NM, Ash JS, Patel VL, Shortliffe EH. Anticipating and addressing the unintended consequences of health IT and policy: a report from the AMIA 2009 Health Policy Meeting. J Am Med Inform Assoc. 2011;18(1):82–90. doi: 10.1136/jamia.2010.007567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grudin J. Groupware and social dynamics: eight challenges for developers. Commun ACM. 1994;37(1):92–105. [Google Scholar]
- 64.Reddy MC, Paul SA, Abraham J, McNeese M, DeFlitch C, Yen J. Challenges to effective crisis management: using information and communication technologies to coordinate emergency medical services and emergency department teams. Int J Med Inform. 2009;78(4):259–269. doi: 10.1016/j.ijmedinf.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 65.Campion TR, Jr, Waitman LR, Lorenzi NM, May AK, Gadd CS. Barriers and facilitators to the use of computer-based intensive insulin therapy. Int J Med Inform. 2011;80(12):863–871. doi: 10.1016/j.ijmedinf.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vogelsmeier AA, Halbesleben JR, Scott-Cawiezell JR. Technology implementation and workarounds in the nursing home. J Am Med Inform Assoc. 2008;15(1):114–119. doi: 10.1197/jamia.M2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McAlearney AS, Hefner JL, Sieck CJ, Huerta TR. The journey through grief: insights from a qualitative study of electronic health record implementation. Health Serv Res. 2015;50(2):462–488. doi: 10.1111/1475-6773.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Popovici I, Morita PP, Doran D, Lapinsky S, Morra D, Shier A, et al. Technological aspects of hospital communication challenges: an observational study. Int J Qual Health Care. 2015;27(3):183–188. doi: 10.1093/intqhc/mzv016. [DOI] [PubMed] [Google Scholar]
- 69.Kaplan B. Evaluating informatics applications: some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inform. 2001;64(1):39–56. doi: 10.1016/s1386-5056(01)00184-8. [DOI] [PubMed] [Google Scholar]
- 70.Mohammadzadeh N, Safdari R, Rahimi A. Multi-agent system as a new approach to effective chronic heart failure management: key considerations. Healthc Inform Res. 2013;19(3):162–166. doi: 10.4258/hir.2013.19.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Michel-Verkerke MB, Spil TA. The USE IT-adoption-model to predict and evaluate adoption of information and communication technology in healthcare. Methods Inf Med. 2013;52(6):475–483. doi: 10.3414/ME12-01-0107. [DOI] [PubMed] [Google Scholar]
- 72.Zhou Y, Ancker JS, Upadhye M, McGeorge NM, Guarrera TK, Hegde S, et al. The impact of interoperability of electronic health records on ambulatory physician practices: a discrete-event simulation study. Inform Prim Care. 2013;21(1):21–29. doi: 10.14236/jhi.v21i1.36. [DOI] [PubMed] [Google Scholar]
- 73.Grando MA, Peleg M, Cuggia M, Glasspool D. Patterns for collaborative work in health care teams. Artif Intell Med. 2011;53(3):139–160. doi: 10.1016/j.artmed.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 74.Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess. 1998;2(16):iii–ix. 1–274. [PubMed] [Google Scholar]
- 75.Kaplan B, Maxwell JA. Qualitative research methods for evaluating computer information systems. In: Anderson JG, Aydin CE, editors. Evaluating the organizational impact of healthcare information systems. New York (NY): Springer; 2005. pp. 30–55. [Google Scholar]
- 76.Borycki EM, Househ M, Kushniruk AW, Kuziemsky C. Use of qualitative methods across the software development lifecycle in health informatics. Stud Health Technol Inform. 2011;164:293–297. [PubMed] [Google Scholar]
- 77.Strauss AL. Qualitative analysis for social scientists. Cambridge, UK: Cambridge University Press; 1987. [Google Scholar]
- 78.Chiasson M, Reddy M, Kaplan B, Davidson E. Expanding multi-disciplinary approaches to healthcare information technologies: what does information systems offer medical informatics? Int J Med Inform. 2007;76(Suppl 1):S89–S97. doi: 10.1016/j.ijmedinf.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 79.Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform. 2004;37(2):128–137. doi: 10.1016/j.jbi.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 80.Fitzpatrick G, Ellingsen G. A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas. Comput Support Coop Work. 2013;22(4-6):609–665. [Google Scholar]
- 81.Peffers K, Tuunanen T, Rothenberger MA, Chatterjee S. A design science research methodology for information systems research. J Manag Inf Syst. 2007;24(3):45–77. [Google Scholar]
- 82.Weng C, McDonald DW, Sparks D, McCoy J, Gennari JH. Participatory design of a collaborative clinical trial protocol writing system. Int J Med Inform. 2007;76(Suppl 1):S245–S251. doi: 10.1016/j.ijmedinf.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 83.Peyton L, Kuziemsky C, Langayan D. A case study in interoperable support for collaborative community health-care; Proceedings of the 4th International Workshop on Software Engineering in Health Care (SEHC); 2012 Jun 4-5; Zurich, Switzerland. pp. 8–14. [Google Scholar]
- 84.Filippi L, Spalanzani A. Using technology in an e-learning training course: the role of the student's personal environment. Int J Bus Inf Syst. 2012;11(1):41–68. [Google Scholar]
- 85.Orlikowski WJ, Gash DC. Technological frames: making sense of information technology in organizations. ACM Trans Manag Inf Syst. 1994;12(2):174–207. [Google Scholar]
- 86.Sadeghi P, Andreev P, Benyoucef M, Momtahan K, Kuziemsky C. Activity theory driven system analysis of complex healthcare processes; Proceedings of the 22nd European Conference on Information Systems (ECIS); 2014 Jun 9-11; Tel Aviv, Israel. pp. 1–14. [Google Scholar]
- 87.Ackerman SL, Tebb K, Stein JC, Frazee BW, Hendey GW, Schmidt LA, et al. Benefit or burden? A sociotechnical analysis of diagnostic computer kiosks in four California hospital emergency departments. Soc Sci Med. 2012;75(12):2378–2385. doi: 10.1016/j.socscimed.2012.09.013. [DOI] [PubMed] [Google Scholar]