Abstract
AIM: To investigate the safety and efficacy of peroral endoscopic myotomy (POEM) for achalasia in patients aged ≥ 65 years.
METHODS: From November 2011 to August 2014, 15 consecutive patients (aged ≥ 65 years) diagnosed with achalasia were prospectively recruited and all underwent POEM at our institution. Eckardt score, lower esophageal sphincter (LES) pressure, esophageal diameter, SF-36 questionnaire, and procedure-related complications were used to evaluate the outcomes.
RESULTS: All 15 patients were treated successfully by POEM, with a median operation time of 55 min. Median myotomy length was 10 cm. Three patients underwent circular myotomy and 12 full-thickness myotomies. Symptoms remitted in all cases during post-POEM follow-up of 6-39 mo. Eckardt score reduced significantly (pre-operation vs post-operation: 8.0 vs 1.0, P < 0.05). Median LES pressure decreased from 27.4 to 9.6 mmHg (P < 0.05). Median diameter of the esophagus was significantly decreased (pre-operation vs post-operation: 51.0 mm vs 30.0 mm, P < 0.05). Only one patient had reflux, which was resolved with oral proton pump inhibitors. No serious complications related to POEM were found. The quality of life of the 15 patients improved significantly after POEM.
CONCLUSION: POEM is a safe and effective technique for treatment of achalasia in patients aged ≥ 65 years, with improvement in symptoms and quality of life.
Keywords: Achalasia, Peroral endoscopic myotomy, Elderly, Efficacy, Quality of life
Core tip: Peroral endoscopic myotomy (POEM) is a novel technique for treatment of achalasia, and has shown exciting results in clinical studies. However, little is known about its efficacy in elderly patients. In the present study, 15 achalasia patients aged ≥ 65 years received POEM. Eckardt score, lower esophageal sphincter pressure, esophageal diameter, SF-36 questionnaire, and procedure-related complications were used to evaluate the outcomes. Our study showed that POEM is a safe and effective therapy for achalasia in elderly patients, with improvement in symptoms and quality of life.
INTRODUCTION
Achalasia is an esophageal motility disorder characterized by aperistalsis of the esophageal body and impaired lower esophageal sphincter (LES) relaxation[1]. Although it occurs only rarely, with an estimated annual incidence between 0.3 and 1.5 per 100000 population and a prevalence of 1/10000, the disease is more common in older people, and the highest incidence appears in the seventh decade of life[2,3]. Clinical symptoms of achalasia include dysphagia, chest pain, and regurgitation. The disease course is usually chronic, with progressive dysphagia and weight loss over several months to years, which severely impairs quality of life, even resulting in aspiration pneumonia. Thus, proper treatment is of vital importance. Current treatment modalities for achalasia in elderly patients include medical treatment, endoscopy and surgery. Laparoscopic Heller myotomy (LHM) is the most definitive and successful treatment of choice. However, its safety and efficacy in elderly patients remain controversial, and some gastroenterologists recommend balloon dilatation as the primary therapy[4,5], whereas others prefer botulinum toxin injection[6].
Peroral endoscopic myotomy (POEM) is a novel technique for treatment of achalasia, and has shown exciting results in clinical studies[7-9]. However, the relative risk of POEM in patients aged ≥ 65 years has yet to be determined. It is also unclear whether POEM in these patients is as effective as it is in younger patients. Our aim was to evaluate the safety and efficacy of POEM in patients aged ≥ 65 years and report our preliminary experience in this pilot study.
MATERIALS AND METHODS
Patients
This study was approved by the Ethics Committee of the Second Xiangya Hospital of Central South University, Changsha, China. The enrollment criteria were as follows: (1) patients diagnosed with achalasia by established methods of esophagogastroduodenoscopy (EGD), esophageal manometry and barium esophagography on the basis of symptoms; (2) patients aged ≥ 65 years; and (3) patients who consented to receive POEM. Patients who could not tolerate anesthesia and those with severe cardiopulmonary disease or blood coagulation disorders were excluded. For patients diagnosed with severe achalasia (Eckardt score ≥ 6, esophageal diameter ≥ 6 cm, or sigmoid-type esophagus), full-thickness myotomy was recommended, while others underwent circular myotomy.
From November 2011 to August 2014, 15 consecutive patients were enrolled. There were six men and nine women with a median age of 67 years (range, 65-84 years) (Table 1). Written informed consent was obtained from all the patients before the procedure. All of them were informed of possible adverse events and other possible treatment options.
Table 1.
Demographics, clinical and operative data in elderly patients treated with peroral endoscopic myotomy
| Patient characteristics | |
| Sex, female/male, n | 9/6 |
| Age, median (range), yr | 67 (65-84) |
| Duration of symptoms, yr | 17 (4-40) |
| Primary procedure, n | |
| Heller surgical myotomy | 1 |
| Pneumatic dilatation | 4 |
| Self-expanding metallic stent | 1 |
| Interval between primary procedure and POEM, median (range), yr | 8.0 (2-20) |
| Procedure-related parameters | |
| Operating time, median (range), min | 55 (40-110) |
| Mode of myotomy | |
| Circular myotomy | 3 |
| Full-thickness | 12 |
| Submucosal tunnel length, cm | 13 (13-15) |
| Myotomy length, median (range), cm | |
| Total | 10 (9-13) |
| Esophageal | 7 (6-11) |
| Gastric | 3 (2-3) |
| Eckardt score | |
| Pre-operation | 8 (5-10) |
| Post-operation | 1 (0-3) |
| LES pressure, mmHg | |
| Pre-operation | 27.4 (22.8-33.5) |
| Post-operation | 9.6 (7.2-13.1) |
| Diameter of esophagus, mm | |
| Pre-operation | 51 (43-57) |
| Post-operation | 30 (24-35) |
| Complications, n | |
| Reflux esophagitis | 1 |
| Follow-up, median (range), mo | 18 (6-39) |
POEM: Peroral endoscopic myotomy.
POEM procedure
Prophylactic intravenous antibiotics and proton pump inhibitors (PPIs) were introduced before the procedure. POEM was performed under general anesthesia via tracheal intubation using a standard single-channel endoscope (GIF-Q260Z; Olympus, Tokyo, Japan) with a transparent cap (D-201-11802; Olympus) attached to the front. CO2 was used as the air supply from the endoscope. Other equipment and accessories included a high-frequency generator (ICC 200; Erbe, Tübingen, Germany), argon plasma coagulation unit (APC300; Erbe), injection needle (NM-4L-1; Olympus), hybrid knife (Erbe), dual knife (KD-650L; Olympus), and hemostatic clips (HX-600-135; Olympus).
The POEM procedure was performed as follows: (1) A submucosal injection (mixed solution of 100 mL saline + 2 mL indigo carmine + 1 mg epinephrine) was administered into the right posterior esophageal wall at 8-10 cm above the esophagogastric junction (EGJ); (2) To create the tunnel entry, a longitudinal mucosal incision of > 2 cm was made using a dual or hybrid knife, and submucosal dissection with the range of ≥ 0.5 cm was performed along both sides of the longitudinal incision; (3) A submucosal tunnel was created, passing over the EGJ, and 3 cm into the proximal stomach. The width of the submucosal tunnel was ≥ 3 cm; (4) Myotomy was started from 2-3 cm below the tunnel entry. Three patients underwent circular myotomy alone and nine received full-thickness myotomy within the range of 6 cm from the EGJ; and (5) After careful hemostasis, several metal clips were applied to close the mucosal entry (Figure 1).
Figure 1.
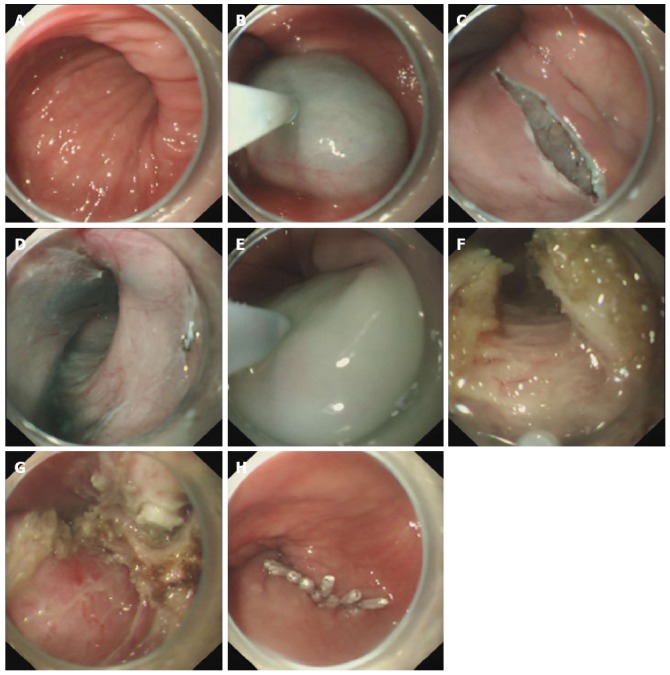
Case illustration of endoscopic full-thickness myotomy. A: A twisting esophagus was shown before POEM; B: Submucosal injection was made to provide a cushion; C: A longitudinal mucosal incision was made as the tunnel entry; D: Submucosal tunnel creation; E: Submucosal injection to the esophageal cavity to preset the tunnel route; F-G: Endoscopic full-thickness myotomy, peri-esophageal membrane could be seen; H: The mucosal entry was closed with several clips. POEM: Peroral endoscopic myotomy.
Postoperative management
Patients were kept nil by mouth for 24 h, a liquid diet for 3 d, and resumed gradually a normal diet within 2 wk. Intravenous PPI and antibiotics were used for 3 d. On postoperative day 2, thoracoabdominal X-ray was performed to check for the occurrence of emphysema, pneumothorax, pneumoperitoneum and pleural effusion.
Outcome and follow-up
Primary outcome was treatment success defined as a reduction in the Eckardt score to ≤ 3 during follow-up. Secondary outcomes included quality of life, esophageal diameter, LES pressure, and procedure-related parameters such as operation time, myotomy length, and rate of complications. Patients were scheduled for a follow-up visit at 1, 3, 6 and 12 mo after POEM, followed by EGD annually to observe the status of esophageal closure and check for any objective sign of reflux esophagitis. Esophageal manometry was also performed to determine LES pressure and barium esophagography was performed to measure esophageal diameter. Patients were contacted via telephone to obtain a current Eckardt score. SF-36 questionnaires were collected preoperatively, and at 1 and 6 mo after POEM.
Statistical analysis
Statistical analysis was performed using SPSS version 21.0 software (Chicago, IL, United States). As for the small sample, all the data were expressed as median and range, and analyzed by Wilcoxon rank sum test. P < 0.05 was considered statistically significant.
RESULTS
Clinical and operative data
Of the 15 patients, three had hypertension and the other 12 had no comorbidity. Five (33%) patients had received endoscopic therapy and one (7%) Heller myotomy, and the other nine patients had not received prior treatment for achalasia. Demographics, clinical and operative data are summarized in Table 1. The duration of symptoms ranged from 4 to 40 years with a median of 17 years. POEM was successfully completed in all 15 patients, with a median operation time of 55 min. The median length of the submucosal tunnel was 13.0 cm, and median myotomy length was 10.0 cm.
Comparison of clinical symptoms, LES pressure, esophageal diameters and SF-36 domain scores before and after POEM
Follow-up duration ranged from 6 to 39 mo with a median of 18 mo. The results were excellent in terms of symptomatic improvement in all the patients. Treatment success, as defined by a post-POEM Eckardt score ≤ 3, was achieved in all cases. Median post-treatment Eckardt score was 1, which was obviously decreased compared with 8 before treatment (P < 0.05). Median LES pressure decreased from 27.4 to 9.6 mmHg (P < 0.05). Median esophageal diameter was dramatically decreased from 51.0 to 30.0 mm (P < 0.05). SF-36 data were obtained at 1 and 6 mo after the operation. These results are described in Table 2 with medians and interquartile ranges and further depicted in Figure 2. Role Limitations due to Emotional Problems and Emotional Well-being domains did not demonstrate any significant differences in scores at any time point. However, Physical Functioning, Role Limitations due to Physical Problems, Energy/Fatigue, Social Functioning, Pain and General Health scores were all significantly higher at 1 and 6 mo (P < 0.05).
Table 2.
SF-36 domain scores before operation and at 1 and 6 mo after operation
| Preoperative | 1 mo after operation | P value | 6 mo after operation | P value | |
| Physical functioning | 85 (75-90) | 90 (85-90) | 0.005 | 90 (85-95) | 0.001 |
| Role limitations due to physical problems | 100 (50-100) | 100 (81-100) | 0.007 | 100 (100-100) | 0.009 |
| Role limitations due to emotional problems | 100 (67-100) | 100 (100-100) | 0.110 | 100 (100-100) | 0.055 |
| Energy/fatigue | 80 (50-80) | 85 (80-85) | 0.002 | 85 (80-85) | 0.002 |
| Emotional well-being | 80 (72-88) | 84 (80-88) | 0.084 | 84 (80-84) | 0.079 |
| Social functioning | 100 (67-100) | 100 (78-100) | 0.013 | 100 (100-100) | 0.010 |
| Pain | 68 (52-100) | 84 (72-100) | 0.009 | 92 (84-100) | 0.005 |
| General health | 52 (35-77) | 77 (57-77) | 0.000 | 87 (72-97) | 0.000 |
All scores expressed as median with interquartile range.
Figure 2.
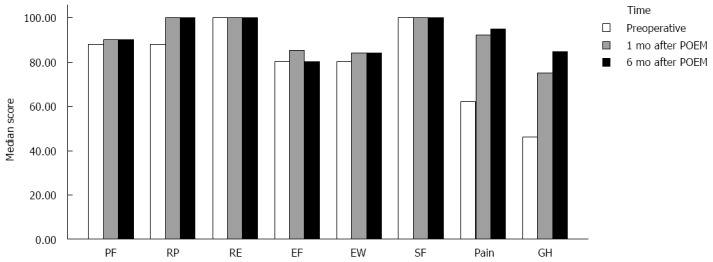
Quality of life outcomes (SF-36 domain).
Complications
Complications occurred in only one case. The patient experienced reflux symptom 2 mo after POEM, and EGD revealed esophagitis, which was relieved after oral PPI therapy. No complications occurred in the rest of the patients during the operation and follow-up.
DISCUSSION
All treatments for achalasia aim to reduce LES pressure with three goals of relieving symptoms, improving esophageal emptying, and preventing development of mega-esophagus[10]. Current treatments for achalasia include pharmacological and endoscopic therapy (injection of botulinum toxin, pneumatic balloon dilation, and POEM) and surgical myotomy[10]. Medical treatment with nitrates or calcium antagonists has been largely abandoned due to its poor efficacy and significant side effects. LHM is the most definitive and successful treatment for elderly patients with no contraindications for the surgical procedure[11]. Nevertheless, it is still an invasive procedure, and it often leads to complications such as perforation, esophageal reflux, and stricture. Therefore, endoscopic treatment is recommended as the first-line option due to poly-morbidity (hypertension, cardiac diseases and diabetes) in elderly patients. Endoscopic dilation and botulinum toxin injection are safe and effective in aged patients, but the effect tends to attenuate over time, and repeated treatment is thus needed. POEM is a novel endoscopic treatment for achalasia and has shown exciting results[7-9,12]. Compared with Heller myotomy, POEM bears the advantages of shorter duration of operation and hospitalization, lower complication rate, and a similar short-term efficacy[13]. However, the safety and efficacy of POEM in elderly patients has yet to be well documented. Six centers have reported POEM for only a total of 14 achalasia patients aged 84-97 years[14]. In our pilot study, a total of 15 achalasia patients aged 65-84 years underwent POEM at our hospital. Symptoms remitted in all cases, and no serious complications or recurrence were noted during follow-up of 6-39 mo. SF-36 questionnaires demonstrated a significant improvement in quality of life. This indicates that POEM is an effective and safe technique for achalasia in elderly patients.
However, we should pay attention to the following points during POEM for achalasia in elderly patients. First, elderly patients usually complain of long-term symptoms and some may have a dilated or distorted esophagus, even with sigmoid-type esophagus. In these cases, creating a straight submucosal tunnel is technically difficult because of the “tunnel maze”. Second, some elderly patients have undergone endoscopic or surgical treatments prior to POEM. Although a few studies have shown that POEM is safe and effective for achalasia patients in the setting of prior interventions[15,16], POEM may be technically difficult due to the presence of fibrosis of varying degrees and altered intramural planes resulting from prior procedures. In our experience, submucosal injection into the esophageal cavity with a mixed solution containing indigo can be used to preset tunnel routes to ensure a straight tunnel into the proximal stomach. Moreover, we can avoid the most fibrotic site by the same method. When encountering fibrotic submucosa near the LES during initial tunnel dissection, caution should be used to avoid thermal injury to the mucosa. In case of difficulty in making a safe submucosal passage when traversing the LES, we can start myotomy prematurely in order to gain access to the distal esophagus and proximal gastric wall. In the present study, one patient had sigmoid-type esophagus and six had undergone prior treatments, and all of them underwent POEM uneventfully. Six of them gained sustained symptomatic improvement. One patient experienced reflux symptoms 2 mo after POEM, and EGD revealed esophagitis, which was relieved after oral PPI therapy.
During POEM, a selective circular myotomy preserving the longitudinal outer esophageal muscular layer is designed to avoid entering the pleural space and reduce morbidity[17]. However, completeness of myotomy is the prerequisite of sufficient and long-term reduction of LES pressure, and is the basis for the excellent results of conventional surgical myotomy[1,18]. Two clinical studies have demonstrated that full-thickness myotomy may be superior for rapid esophagogastric emptying and reducing operation time, without increasing procedure-related adverse events and clinical reflux complications[12,19]. Given the fact that full-thickness myotomy theoretically results in long-term symptom remission, we performed full-thickness myotomy in 12 patients. Although 15 patients may not be sufficient for a comparative study of circular and full-thickness myotomy, only one patient had reflux esophagitis in the full-thickness myotomy group, which was relieved after oral PPI therapy. However, because the follow-up period was short, whether full-thickness myotomy has better long-term efficacy than circular myotomy needs further study.
In conclusion, POEM is safe and effective in elderly patients with achalasia. It is a less-invasive endoscopic procedure for achalasia, and shows good results without causing serious complications. Although the sample size was small and duration of follow-up was short, this new method showed satisfactory initial results. A large randomized controlled study is needed to evaluate the long-term efficacy of POEM compared with other treatments for achalasia in elderly patients.
COMMENTS
Background
Current treatment modalities for achalasia in elderly patients include medical treatment, endoscopy, and surgery. Medical treatment has been largely abandoned due to its poor efficacy and significant side effects. Laparoscopic Heller myotomy is now the most definitive and successful treatment of choice. Nevertheless, it is still an invasive procedure, and often yields complications such as perforation, esophageal reflux and stricture. Conventional endoscopic treatment such as endoscopic dilation, stent insertion and botulinum toxin injection has been shown to be safe and effective in aged patients, but the effect tends to attenuate over time and repeated treatment is often needed.
Research frontiers
Peroral endoscopic myotomy (POEM) is a novel technique for treatment of achalasia. The current research hotspot is how to perform it successfully while simultaneously reducing the procedure-related complications.
Innovations and breakthroughs
This is the first study to investigate the safety and efficacy of POEM for the treatment of achalasia in elderly patients. The authors shared some useful experience in POEM for end-stage achalasia.
Applications
The study results suggest that POEM is safe and effective in elderly patients with achalasia. It is a less-invasive endoscopic procedure, and shows good results without causing serious complications.
Terminology
POEM represents a natural orifice endoscopic surgical technique for scarless Heller myotomy for the treatment of achalasia. It utilizes a submucosal tunnel approach that offsets the mucosal and muscular incisions and thus allows secure closure with a few clips on the mucosotomy site.
Peer-review
This is an interesting study that presents the outcome of POEM in 15 AC patients aged 65 years or older, recorded with lower esophageal sphincter-pressure esophageal diameter and QoL (SF 36) as endpoints.
Footnotes
Institutional review board statement: The study was approved by the Ethics Committee of the Second Xiangya Hospital of Central South University, Changsha, China.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: There was no potential conflict of interest related to this study.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 13, 2015
First decision: April 23, 2015
Article in press: June 10, 2015
P- Reviewer: Buanes TA, Tellez-Avila F S- Editor: Ma YJ L- Editor: Kerr C E- Editor: Ma S
References
- 1.Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, Ciovica R. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249:45–57. doi: 10.1097/SLA.0b013e31818e43ab. [DOI] [PubMed] [Google Scholar]
- 2.Sonnenberg A. Hospitalization for achalasia in the United States 1997-2006. Dig Dis Sci. 2009;54:1680–1685. doi: 10.1007/s10620-009-0863-8. [DOI] [PubMed] [Google Scholar]
- 3.Gennaro N, Portale G, Gallo C, Rocchietto S, Caruso V, Costantini M, Salvador R, Ruol A, Zaninotto G. Esophageal achalasia in the Veneto region: epidemiology and treatment. Epidemiology and treatment of achalasia. J Gastrointest Surg. 2011;15:423–428. doi: 10.1007/s11605-010-1392-7. [DOI] [PubMed] [Google Scholar]
- 4.Robertson CS, Fellows IW, Mayberry JF, Atkinson M. Choice of therapy for achalasia in relation to age. Digestion. 1988;40:244–250. doi: 10.1159/000199661. [DOI] [PubMed] [Google Scholar]
- 5.Boztas G, Mungan Z, Ozdil S, Akyüz F, Karaca C, Demir K, Kaymakoglu S, Besisik F, Cakaloglu Y, Okten A. Pneumatic balloon dilatation in primary achalasia: the long-term follow-up results. Hepatogastroenterology. 2005;52:475–480. [PubMed] [Google Scholar]
- 6.Bruley des Varannes S, Scarpignato C. Current trends in the management of achalasia. Dig Liver Dis. 2001;33:266–277. doi: 10.1016/s1590-8658(01)80718-0. [DOI] [PubMed] [Google Scholar]
- 7.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 8.Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309–11.e1-3. doi: 10.1053/j.gastro.2013.04.057. [DOI] [PubMed] [Google Scholar]
- 9.Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–667. doi: 10.1097/SLA.0b013e31826b5212. [DOI] [PubMed] [Google Scholar]
- 10.Richter JE. Achalasia - an update. J Neurogastroenterol Motil. 2010;16:232–242. doi: 10.5056/jnm.2010.16.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roll GR, Ma S, Gasper WJ, Patti M, Way LW, Carter J. Excellent outcomes of laparoscopic esophagomyotomy for achalasia in patients older than 60 years of age. Surg Endosc. 2010;24:2562–2566. doi: 10.1007/s00464-010-1003-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411–417. doi: 10.1038/ajg.2011.388. [DOI] [PubMed] [Google Scholar]
- 13.Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2014;259:1098–1103. doi: 10.1097/SLA.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 14.Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322–3338. doi: 10.1007/s00464-013-2913-8. [DOI] [PubMed] [Google Scholar]
- 15.Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg. 2013;17:1188–1192. doi: 10.1007/s11605-013-2193-6. [DOI] [PubMed] [Google Scholar]
- 16.Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598–605. doi: 10.1016/j.jamcollsurg.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 17.Inoue H, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Minami H, Kudo SE. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519–525. doi: 10.1016/j.thorsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A, Costantino M, Nicoletti L, Ancona E. Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg. 2002;235:186–192. doi: 10.1097/00000658-200202000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg. 2013;217:442–451. doi: 10.1016/j.jamcollsurg.2013.04.033. [DOI] [PubMed] [Google Scholar]


