Abstract
Background:
The second processing cycle for adding the artificial teeth to heat-polymerized acrylic resin denture bases may result in dimensional changes of the denture bases. The aim of this study was to evaluate the dimensional changes of the heat-polymerized acrylic resin denture bases with one and two-cycle processing methods.
Materials and Methods:
A metal edentulous maxillary arch was used for making 40 stone casts. Maxillary complete dentures were made with heat-polymerized acrylic resins (Meliodent and Acropars) with one and two stage processing methods (n = 10 for each group). Linear dimensional changes in anteroposterior and mediolateral distances and vertical changes in the first molar region were measured following each processing cycle, using a digital caliper. Mean percentage of the dimensional changes were subjected to two-way analysis of variance and Tukey honest significant difference tests (α = 0.05).
Results:
Postpolymerization contraction occurred in both anteroposterior and mediolateral directions in all studied groups; however, the vertical dimension was increased. Acropars acrylic resin showed the highest dimensional changes and the second processing cycle significantly affected the measured distances (P < 0.05). Meliodent acrylic resin was not significantly influenced by the processing method.
Conclusion:
Reheating of the acrylic resin denture bases for the addition of denture teeth result in linear dimensional changes, which can be clinically significant based on the acrylic resin used.
Keywords: Acrylic resins, denture bases, polymers
INTRODUCTION
A successful complete denture must provide esthetic, function, and health of supporting and surrounding tissues. Well-fitted dentures promote chewing efficiency, patient's comfort, and prevent the hyperplastic lesions. Polymethyl methacrylate is the material of choice for denture bases. However, the dimensional changes of acrylic resins are inevitable, which is caused by processing shrinkage and expansion upon water sorption.[1] Complete denture adaptation may be affected by impression, the type of acrylic resin, the processing cycle, cooling procedure, and water sorption.[2]
One of the important stages in the fabrication of complete denture is jaw relation records which affect esthetic, function, and patient's comfort. A precise determination of jaw relation records needs well-fitted bases. Ideal record bases should have requirements such as same border form and adaptation of the final denture base, sufficient rigidity, dimensional stability, ease of fabrication, low cost, desirable color, and ease of artificial teeth addition.[3] Different materials are used for making record bases such as wax, shellac, auto-polymerized, and heat-polymerized acrylic resins. Auto-polymerized acrylic resins are usually used for establishing the jaw relations. The heat-polymerized acrylic resin record bases have several advantages. They provide more retention and stability, which result in more accurate jaw relation records and final occlusion.[3] In addition, any problem in the denture base fit can be detected early and can be corrected before final finishing of the complete denture.[4] The disadvantages of heat-polymerized acrylic resin bases include extra cost and time for laboratory procedures, teeth arrangement difficulty in limited interarch space, and bonding between denture base and acrylic resin, which attaches the artificial teeth to the base. In addition, two stage processing may have an adverse effect on denture base dimensional accuracy and fit.[5] Denture processing may result in occlusal interferences, which may induce tissue injury, loss of comfort, masticatory inefficacy, and adverse effect on the complete denture function.
It has been reported that the second curing cycle (above 75°C)[6] results in stress release in the acrylic denture base and dimensional changes.[7] It was recommended to use lower temperatures of 66°C or 59°C for 12 h for the second heat curing cycle to minimize the dimensional changes of denture base. However, it was reported that the second cure at 74°C, 67°C, and 60°C results in small shrinkage of denture base, which would be clinically significant.[8] Yeung et al.[3] reported 1% total linear shrinkage of denture base as a result of the second curing cycle. Similarly, a subjective analysis showed an insignificant reduction of maxillary denture retention after second processing cycle.[9] The dimensional changes of mandibular denture base after second heat curing was also insignificant.[10]
The aim of this study was to evaluate the dimensional stability of acrylic resin denture bases with one and two stage processing cycle. The null hypothesis was that the dimensional stability of the maxillary denture base would not be affected by the second curing cycle.
MATERIALS AND METHODS
A metal edentulous maxillary model with four reference points at incisive papilla (A), midpalatal area in front of posterior palatal seal area (B), left and right tuberosities (C and D) was used [Figure 1]. The metal model was duplicated using polyvinyl siloxane (Silastic E; Dow Corning, Midland, Mich, USA) to prepare 40 casts with type III dental stone (Moldano; Heraeus Kulzer, Dormager, Germany). A 2 mm thickness of the base plate wax (Dentsply, Surrey, UK) was adopted on the metal model and two wax sprues with 10 mm diameter were attached on the back of tuberosities. The second silicone mold (Silastic E; Dow Corning) was prepared from this metal model with covering base plate wax. This silicone mold was placed on 20 stone casts and molten base plate wax was poured through the sprues to prepare similar wax bases for fabricating of heat-polymerizing bases for two stage processing technique. These casts with wax bases were invested into flasks. After removing the wax with boiling water and separating medium application, the heat-polymerized resins including Meliodent (Heraeus Kulzer) and Acropars (Marlic Medical Instruments CO, Tehran, Iran) were prepared, poured and processed at 70°C for 2 h with a terminal boiling of 30 min. Then, the flasks were left in the water bath to cool completely. After deflasking, the excess resins and beads in the intaglio surfaces of denture bases were removed.
Figure 1.
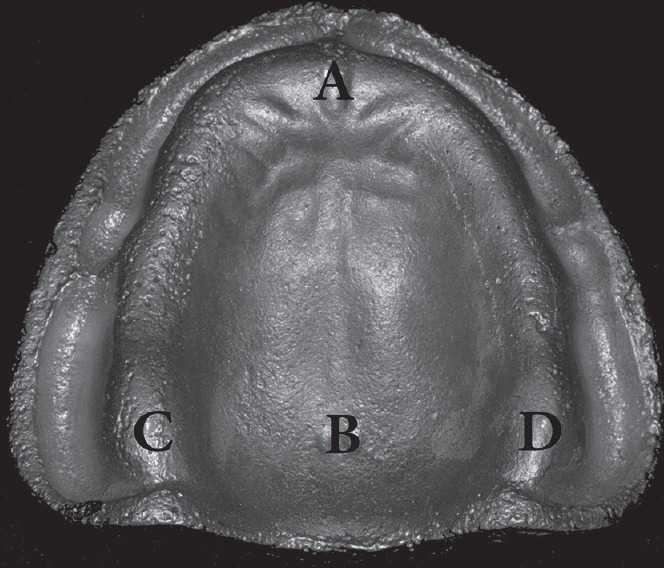
The reference points used for measuring the linear dimensions.
The artificial teeth (Marjan; Ideal Makoo, Urmia, Iran) were arranged on one of the base plate waxes and the third silicone mold (Silastic E; Dow Corning) was made from the arranged teeth and wax base including sprues. The third mold was used for making similar maxillary dentures for both one and two stage processing methods. For one stage processing technique, the artificial teeth with the same size and mold were placed in the third silicone mold and transferred to the remaining 20 casts and filled with molten base plate wax. The other steps of flasking, pouring and processing were same as making the acrylic resin bases. Thus, 20 identical maxillary dentures were made with one stage processing using the both acrylic resins (n = 10).
In the two-stage processing, after placing the teeth in the silicone mold, it was transferred to acrylic resin bases which were placed on the metal model. The next stages were repeated in a similar way as described previously. The dentures were processed in a cycle of 6 h at 70°C with a terminal boil of 1 h. Then, the flasks were left in the water bath to cool completely.
The studied groups
The complete dentures were divided into four groups; groups 1 and 2 were made with Meliodent acrylic resin and one or two stage processing techniques were used for denture processing respectively. In groups 3 and 4 dentures were made with Acropars acrylic resin and one or two stage processing techniques were used for denture processing respectively.
Measurement of the reference points
The AB (anteroposterior) and CD (mediolateral) dimensions were measured on the stone casts and the intaglio surface of the acrylic resin bases after first and second processing cycles for two-stage method and after single processing cycle of one stage method [Figure 2a and b], using digital caliper with 10 μm accuracy. Each measurement was repeated three times and the mean was calculated. Vertical changes were determined with measuring the distance between mesiobuccal cusp tip of maxillary right first molar to a depression which was created in the landing area of the model.
Figure 2.
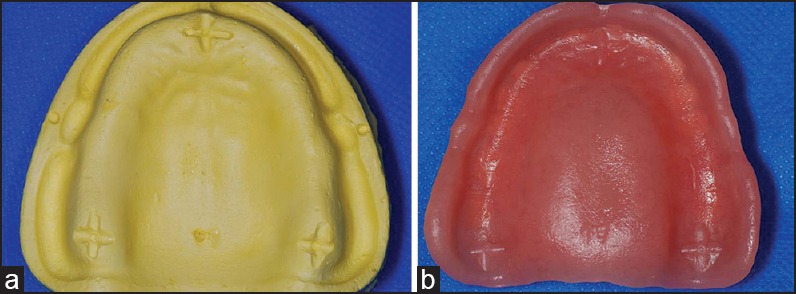
(a-b)The dimensions were measured on the stone casts and the intaglio surface of the acrylic resin bases.
The percentage of dimensional changes was calculated using the following formula:
Percentage of linear changes = (Dimensions in the denture base-dimensions on the casts/Dimensions on the casts) × 100.
The percentages of linear and vertical changes were analyzed using two-way analysis of variance (ANOVA) and Tukey honest significant difference (HSD) (α = 0.05).
RESULTS
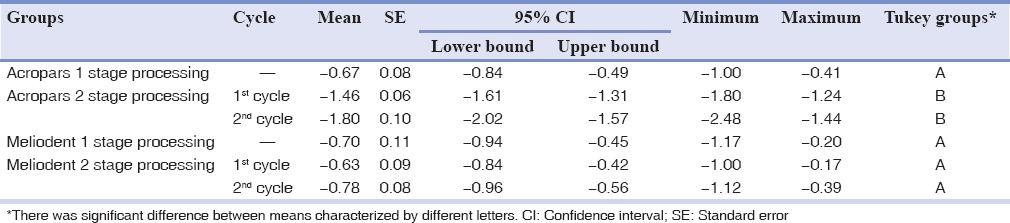
Tables 1–3 present the mean percentages of linear and vertical changes of the studied groups. Postpolymerization contraction occurred in both anteroposterior and mediolateral distances, but the vertical dimension was increased. Acropars acrylic resin, which was processed with two stage processing cycle, had the highest changes in all dimensions. Two-way ANOVA showed that the type of processing cycle of acrylic resins significantly affected both the anteroposterior and mediolateral dimensions (P < 0.05). The type of resin and its interaction with processing method were statistically effective only in mediolateral dimension (P < 0.05) [Table 4].
Table 1.
Mean percentage of anteroposterior linear changes of the studied groups
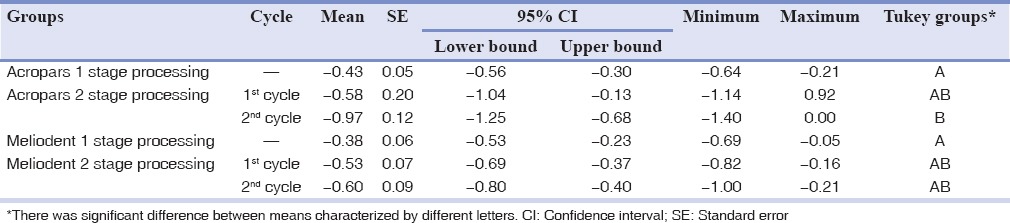
Table 3.
Mean percentage of vertical dimension changes of the studied groups
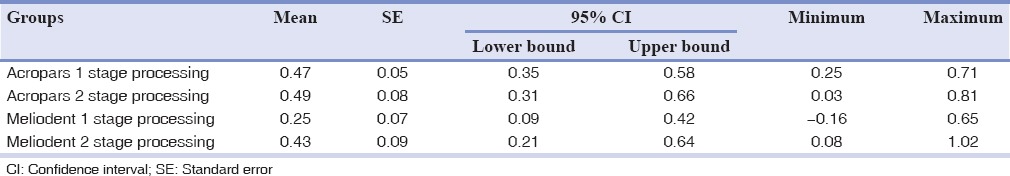
Table 4.
Two-way ANOVA of the dimensional changes
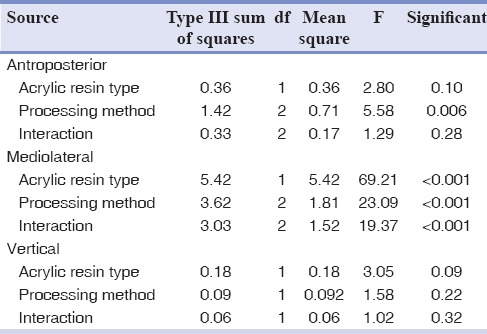
Table 2.
Mean percentage of mediolateral linear changes of the studied groups
The vertical dimension was increased in all specimens, but the difference was not statistically significant.
Tukey HSD showed that the anteroposterior and mediolateral dimensions of Acropars acrylic resin were significantly different in one cycle processing compared to two cycle processing (P = 0.02 and P < 0.001, respectively). However, it was not significantly different in Meliodent specimens (P = 1.00).
DISCUSSION
Despite development of different denture base materials, acrylic resins are still the material of choice. The dimensional changes of heat-polymerized acrylic resins occur due to thermal expansion on heating, contraction on cooling, polymerization shrinkage, and expansion as a result of water sorption.[11,12]
In this study, the one cycle processing of acrylic resin lead to less shrinkage than two stage processing in both anteroposterior (AB) and mediolateral (CD) distances, which was significant for Acropars acrylic resin; thus, the null hypothesis was partially rejected. The percentage of linear shrinkage of the denture bases was <1% in all dimensions of the two studied acrylic resins except mediolateral distance of Acropars specimens in two stage processing which was 1.80%.
The properties of acrylic resins were affected by polymerization process, which involves chemical, mechanical, dimensional and thermal changes. Density of the monomer is less than the density of the polymer, which causes dimensional contraction of the acrylic resins during the polymerization process. The amount of polymerization shrinkage depends on the degree of conversion, type of monomer, volume and size of the filler, the nature of resin, flow of resin, the polymerization rate and water sorption.[13,14,15,16,17] A higher amount and smaller size of monomer molecules result in more shrinkage due to a higher proportion of the monomer to polymer.[16,18] The polymer to monomer ratio of Acropars is 2:1 by volume as recommended by the manufacturer. This ratio for Meliodent resin is 3:1, which is accepted for polymer/monomer ratio.[19] This can imply more shrinkage of Acropars compared to Meliodent acrylic resin.
Studies have shown that two stage processing results in slight dimensional changes, which is not considered clinically significant, and is comparable to one stage processing.[3,8,9,10] Yeung et al.[3] showed that only 0.2% of 1% total linear shrinkage of the denture bases occurred during the second processing cycle. Other studies reported significant greater distortion of the denture bases due to recurring[20] or as great as the first cycle.[5] High distortion of the denture bases has been reported when more than 72°C have been used for processing.[21] The rapid heating of the resin during the polymerization cycle results in boiling of monomer and porosity.[5] The porosity causes internal stress, distortion and warpage of the denture, and reduces the mechanical properties of acrylic resins.[22,23,24]
The dimensional changes in anteroposterior distance were less than mediolateral posterior distances. It has been shown that in the maxillary dentures, maximum dimensional changes occur around the posterior segment.[21,25,26]
During the processing of heat-polymerized resins, the temperature is raised above the glass transition temperature. Cooling of the resin from the maximum temperature to the glass transition temperature produces small stress because the resin is soft. Below the glass transition temperature, resin becomes more rigid and different contraction rate of resin and stone induces stresses as it cools toward room temperature.[27] The reheating of the denture base during second curing cycle results in the release of the inherent stress in the first curing.[3,7]
It has been shown that the addition of denture teeth induces more distortion of the denture base due to the laboratory procedures (such as wax removing with hot water), which results in additional stress releasing.[28] When the volume of the resin for addition of denture teeth increases, more shrinkage will occur. In addition, increased volume of the resin can increase the exothermic heat of reaction, which cause temperature rise exceeding glass transition temperature.[8] The resulting warpage of denture base can also be due to additional polymerization and rearrangement and closer packing of the long-chain molecules.[3,5] However, it was suggested that the shrinkage decreased with each reheating of the denture base.[3]
The linear dimensional changes of the denture bases especially in mediolateral direction results in increased vertical dimension. In spite of the lack of statistical significant increase of the vertical dimension in the first molar region in present study, it can be concluded that the linear dimensional changes of the acrylic resin denture bases due to second processing cycle can be clinically significant.
One of the limitations of this study was that the three-dimensional changes of the denture bases were not measured. Moreover, in the current study, the water absorption and its effect on dimensional changes were not investigated. The results of this in vitro study may be different from clinical conditions.
CONCLUSION
Within the limitations of this study the following conclusions were drawn:
Two stage processing cycle can influence the dimensional stability of Acropars heat-polymerizing acrylic resin.
Meliodent heat-polymerizing acrylic resin can be processed by one or two stage processing method with insignificant dimensional changes.
Vertical dimension of dentures increased with one and two stage processing methods with no significant difference.
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences Research Grant #83406.
Footnotes
Source of Support: This study was supported by Isfahan University of Medical Sciences Research Grant #83406.
Conflicts of Interest: The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- Skinner EW, Cooper EN. Physical properties of denture resin. Part I: Curing shrinkage and water sorption. J AM Dent Assoc. 1943;30:1845–52. [Google Scholar]
- 2.Ganzarolli SM, Rached RN, Garcia RC, Del Bel Cury AA. Effect of cooling procedure on final denture base adaptation. J Oral Rehabil. 2002;29:787–90. doi: 10.1046/j.1365-2842.2002.00886.x. [DOI] [PubMed] [Google Scholar]
- 3.Yeung KC, Chow TW, Clark RK. Temperature and dimensional changes in the two-stage processing technique for complete dentures. J Dent. 1995;23:245–53. doi: 10.1016/0300-5712(95)91190-x. [DOI] [PubMed] [Google Scholar]
- 4.Bailey L. Permanent-type bases for transferring records to an articulator. Dent Clin North Am. 1964;8:623. [Google Scholar]
- 5.Tuckfield AM, Worner HK, Guerin BD. Acrylic resins in dentistry part II: Their use for denture construction. Aust J Dent. 1943;47:1–26. [Google Scholar]
- 6.Cooper EN, Skinner EW. Dimensional stability of denture resins. J Dent Res. 1943;22 abstr. 203. [Google Scholar]
- 7.Woelfel JB, Paffenbarger GC. Dimensional changes occuring in artificial denture. Int Dent J. 1959;9:451–60. [Google Scholar]
- 8.Polukoshko KM, Brudvik JS, Nicholls JI, Smith DE. Evaluation of heat-cured resin bases following the addition of denture teeth using a second heat cure. J Prosthet Dent. 1992;67:556–62. doi: 10.1016/0022-3913(92)90090-w. [DOI] [PubMed] [Google Scholar]
- 9.Ellis JS, Read GE, Thomason JM. A subjective study of dimensional stability of permanent acrylic resin complete denture bases after a second curing cycle. Eur J Prosthodont Restor Dent. 2004;12:105–8. [PubMed] [Google Scholar]
- 10.Fenlon MR, Juszczyk AS, Rodriguez JM, Curtis RV. Dimensional stability of complete denture permanent acrylic resin denture bases; A comparison of dimensions before and after a second curing cycle. Eur J Prosthodont Restor Dent. 2010;18:33–8. [PubMed] [Google Scholar]
- 11.Keenan PL, Radford DR, Clark RK. Dimensional change in complete dentures fabricated by injection molding and microwave processing. J Prosthet Dent. 2003;89:37–44. doi: 10.1067/mpr.2003.3. [DOI] [PubMed] [Google Scholar]
- 12.Wong DM, Cheng LY, Chow TW, Clark RK. Effect of processing method on the dimensional accuracy and water sorption of acrylic resin dentures. J Prosthet Dent. 1999;81:300–4. doi: 10.1016/s0022-3913(99)70273-8. [DOI] [PubMed] [Google Scholar]
- 13.Puckett AD, Smith R. Method to measure the polymerization shrinkage of light-cured composites. J Prosthet Dent. 1992;68:56–8. doi: 10.1016/0022-3913(92)90285-i. [DOI] [PubMed] [Google Scholar]
- 14.Yap AU, Ng SC, Siow KS. Soft-start polymerization: Influence on effectiveness of cure and post-gel shrinkage. Oper Dent. 2001;26:260–6. [PubMed] [Google Scholar]
- 15.Min SH, Ferracane J, Lee IB. Effect of shrinkage strain, modulus, and instrument compliance on polymerization shrinkage stress of light-cured composites during the initial curing stage. Dent Mater. 2010;26:1024–33. doi: 10.1016/j.dental.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Nejatidanesh F, Lotfi HR, Savabi O. Marginal accuracy of interim restorations fabricated from four interim autopolymerizing resins. J Prosthet Dent. 2006;95:364–7. doi: 10.1016/j.prosdent.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 17.Savabi O, Nejatidanesh F, Fathi MH, Navabi AA, Savabi G. Evaluation of hardness and wear resistance of interim restorative materials. Dent Res J (Isfahan) 2013;10:184–9. doi: 10.4103/1735-3327.113338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim SH, Watts DC. Polymerization shrinkage-strain kinetics of temporary crown and bridge materials. Dent Mater. 2004;20:88–95. doi: 10.1016/s0109-5641(03)00101-5. [DOI] [PubMed] [Google Scholar]
- 19.Anusavice KJ, Shen C, Rawls HR. 12th ed. St. Louis: Elsevier; 2013. Phillips’ Science of Dental Materials; pp. 478–9. [Google Scholar]
- 20.Jerolimov V, Jagger RG, Milward PJ. Effect of the curing cycle on acrylic denture base glass transition temperatures. J Dent. 1991;19:245–8. doi: 10.1016/0300-5712(91)90128-l. [DOI] [PubMed] [Google Scholar]
- 21.Pasam N, Hallikerimath RB, Arora A, Gilra S. Effect of different curing temperatures on the distortion at the posterior peripheral seal: An in vitro study. Indian J Dent Res. 2012;23:301–4. doi: 10.4103/0970-9290.102209. [DOI] [PubMed] [Google Scholar]
- 22.Honorez P, Catalan A, Angnes U, Grimonster J. The effect of three processing cycles on some physical and chemical properties of a heat-cured acrylic resin. J Prosthet Dent. 1989;61:510–7. doi: 10.1016/0022-3913(89)90025-5. [DOI] [PubMed] [Google Scholar]
- 23.Chee WW, Donovan TE, Daftary F, Siu TM. The effect of vacuum-mixed autopolymerizing acrylic resins on porosity and transverse strength. J Prosthet Dent. 1988;60:517–9. doi: 10.1016/0022-3913(88)90261-2. [DOI] [PubMed] [Google Scholar]
- 24.Firtell DN, Harman LL. Porosity in boilable acrylic resin. J Prosthet Dent. 1983;49:133–4. doi: 10.1016/0022-3913(83)90254-8. [DOI] [PubMed] [Google Scholar]
- 25.Consani RL, Domitti SS, Consani S. Effect of a new tension system, used in acrylic resin flasking, on the dimensional stability of denture bases. J Prosthet Dent. 2002;88:285–9. doi: 10.1067/mpr.2002.128447. [DOI] [PubMed] [Google Scholar]
- 26.Abby A, Kumar R, Shibu J, Chakravarthy R. Comparison of the linear dimensional accuracy of denture bases cured the by conventional method and by the new press technique. Indian J Dent Res. 2011;22:200–4. doi: 10.4103/0970-9290.84282. [DOI] [PubMed] [Google Scholar]
- 27.Pow EH, Chow TW, Clark RK. Linear dimensional change of heat-cured acrylic resin complete dentures after reline and rebase. J Prosthet Dent. 1998;80:238–45. doi: 10.1016/s0022-3913(98)70117-9. [DOI] [PubMed] [Google Scholar]
- 28.Barco MT, Jr, Moore BK, Swartz ML, Boone ME, Dykema RW, Phillips RW. The effect of relining on the accuracy and stability of maxillary complete dentures: An in vitro and in vivo study. J Prosthet Dent. 1979;42:17–22. doi: 10.1016/0022-3913(79)90324-x. [DOI] [PubMed] [Google Scholar]


