Abstract
Background:
A precise impression is mandatory to obtain passive fit in implant-supported prostheses. The aim of this study was to compare the accuracy of three impression materials in both parallel and nonparallel implant positions.
Materials and Methods:
In this experimental study, two partial dentate maxillary acrylic models with four implant analogues in canines and lateral incisors areas were used. One model was simulating the parallel condition and the other nonparallel one, in which implants were tilted 30° bucally and 20° in either mesial or distal directions. Thirty stone casts were made from each model using polyether (Impregum), additional silicone (Monopren) and vinyl siloxanether (Identium), with open tray technique. The distortion values in three-dimensions (X, Y and Z-axis) were measured by coordinate measuring machine. Two-way analysis of variance (ANOVA), one-way ANOVA and Tukey tests were used for data analysis (α = 0.05).
Results:
Under parallel condition, all the materials showed comparable, accurate casts (P = 0.74). In the presence of angulated implants, while Monopren showed more accurate results compared to Impregum (P = 0.01), Identium yielded almost similar results to those produced by Impregum (P = 0.27) and Monopren (P = 0.26).
Conclusion:
Within the limitations of this study, in parallel conditions, the type of impression material cannot affect the accuracy of the implant impressions; however, in nonparallel conditions, polyvinyl siloxane is shown to be a better choice, followed by vinyl siloxanether and polyether respectively.
Keywords: Dental implants, dental impression materials, dental impression techniques, polyvinyls
INTRODUCTION
As the dental implants are not supported by a periodontal ligament to compensate for a certain degree of inaccuracy in fixed dental prostheses, passive fit is the primary objective in fabricating a successful superstructure for osseointegrated endosseous implants.[1,2] Implant-prosthesis set shows only a minimal mobility caused by the elasticity of bone.[3]
A nonpassive framework results in the accumulation of stresses in the implant-prosthesis set, leading to certain biological and mechanical complications such as screw loosening, screw fracture, occlusal discrepancies,[4,5] loss of osseointegration, plaque accumulation, soft and hard tissue problems, and bone loss.[1,6]
There is tremendous uncertainty concerning the amount of stress that may be clinically tolerable about the long-term serviceability of the restorations. Although in practice, it is impossible to attain complete passive fit,[7] the clinicians must strive to overcome the variables influencing the clinical acceptable fit. The precise transfer of spatial relationships of implants to the master cast during making the impression is the first and critical step to ensure a strain-free superstructure.[8]
Numerous researchers have investigated the factors that affect the accuracy of impressions, such as impression techniques,[9,10,11,12] different impression materials,[13,14,15] implant angulations,[1,11] splinting or nonsplinting,[16,17,18,19,20] the impression copings modifications,[2,21,22,23] type of impression tray,[24] depth of implant,[6,13] connection length,[2,3] fixture or abutment level impression,[25,26,27] the time between impression making and pouring,[28] and implant system tolerance.[10,20,29]
Among the impression materials so far used for implant impression, polyether and additional silicone (A-silicon) are mostly suggested.[3,25,28,30,31,32,33,34]
While Wee,[34] Seyedan et al.[16] and Lee and Cho[18] found no difference between polyether and polyvinyl siloxane (PVS), Lee et al.[8] demonstrated that, in subgingival situations, PVS leads to better accuracy compared to polyether. In another study carried out by Wenz and Hertrampf,[12] the performance of polyether was shown to be superior to PVS.
Vinyl siloxanether, composed of polyether and additional PVS, is a new impression material which is claimed[35] to have all the theoretical advantages of polyether[36] and PVS such as excellent flow ability, remarkable hydrophilicity, easy handling and optimized elastomeric properties. In addition to achieving its high final hardness immediately after the setting, vinyl siloxanether guarantees the precision of the impression. Furthermore, although it has different consistencies (heavy, medium, medium soft and light), the medium one is recommended for implant impression.[37]
A lack of parallelism among the implants, and that between the implants and the teeth is a common finding in clinic, which is due to anatomical limitations or the esthetic considerations. This may lead to undesirable path of impression withdrawal which is considered as a cause of impression distortion. Whereas most of the previous in vitro investigations have evaluated the impression accuracy under the ideal condition with parallel implants,[12,20] fewer studies have assessed the influence of nonparallel implants especially with four or more implants.[13,30,38] Moreover, previous studies failed to arrive at a clear consensus over impression materials and angulations. Some studies showed that when two or three implants are required, angulation of the implant has no adverse effect on the accuracy of impression.[1,11,39] Assuncao et al.[30] reported better results for the parallel situations compared to the 10, 15 and 25° angulations.
The aim of the present study was to evaluate the effect of impression materials and implant angulations on the accuracy of impressions in parallel and nonparallel implants.
The null hypothesis was that there would be no significant difference in the accuracy of the impressions between the parallel and angulated implants with different impression materials.
MATERIALS AND METHODS
Master models fabrication
Two heat-polymerized acrylic resin (Lucitone Clear; Dentsply International, York, PA, USA) master models of a maxillary arch with four internal connection implant analogues (3.5 mm × 10 mm) (130527P4, Dio Co., Busan, South Korea) were made. They were fabricated by duplicating a dentiform (D51DP-TRM.444, Nissin Dental Products Inc., Kyoto, Japan). The anatomic crown portions of premolars, canines and incisors of the dentiform were ground flat to simulate a residual ridge. On the lateral incisors and canines areas, four holes were prepared. The two models had different orientations of the implant replicas. In the master model 1, the longitudinal axes of analogues were parallel to each other and at right angle to the horizontal plane [Figure 1]. The four implant analogues (130527P4: Dio Co., Busan, South Korea) were sequentially numbered 1-4 from left to right. In master model 2, the implant analogues were positioned at 30° buccally in relation to their long axes. They were also positioned at 20° distally (implants No. 1, 4) and or mesially (implants No. 2, 3) in relation to horizontal the surface of the master model [Figure 2].
Figure 1.

Master model 1 (parallel situation).
Figure 2.

Master model 2 (angulated situation).
Implant analogues were fixed within the arranged holes using an auto-polymerizing clear acrylic resin (Orthojet; Lang Dental Manufacturing Co., Wheeling, IL, USA).
Impression tray design
Four open tray impression copings (Narrow, Pick Up, Sip3907N, Dio. co., Busan, South Korea) were hand-tightened to implant analogues. For fabricating special trays, two layers of base plate wax (Modeling wax; Dentsply Ltd., Weybridge, UK) were placed on the master models. Four stops were made by using a milling machine (Kavo EWL-K9, Leutkirch, Germany) to standardize the path of insertion and removal. Three of the stops had a rectangle shape with the area size of 2 mm × 4 mm and were placed in the landing area of the master model (two stops in the posterior part and one in the anterior part of the model). The last stop was in the midpalate in form of a 4 mm × 4 mm. To ensure uniform thickness of the impression material in all trays, both master models were duplicated by using A-Silicone (Monopren, Kettenbach, Eschenberg, Germany) and the impressions were poured using a type IV die stone (Herostone, Vigodent, Rio de Janeiro, Brazil) to obtain two casts on which all trays were made. A total of 30 custom open trays for each model (60 trays in total) were made using auto-polymerized acrylic resin (Jet; Artigos Odontologicos Classico Ltd., Sao Paulo, Brazil). The trays were stored at room temperature for 24 h before making the impression.
Impression procedure
In this study, there were six experimental groups (due to the three impression materials evaluated in two situations of implant angulations) as well as two control groups required for the two master models. A sample size of 10 was used in the experimental groups. Polyether (Impregum, 3M ESPE, Seefeld, Germany), A-silicon (Monopren, Iso4823, Kettenbach Gm BH & co. KG, Im, Heerfeld, Eschenburg, Germany) and vinyl siloxanether (Identium, Medium Kettenbach Gm BH & co. KG, Im, Heerfeld, Eschenburg, Germany) impression materials, all with medium consistency, were selected for this experiment. Appropriate adhesive was applied to the custom trays 1 h before impression making.
The impression protocol was standardized as follows:
A 1.5 kg metal block exerted a standardized pressure on each tray during the polymerization.
The impression copings were secured with flat head screw on the implant analogues using dedicated torque wrench calibrated at 10 Ncm. The copings were coated with the appropriate adhesive of the impression material.
Impression-master model complex was placed in distilled water at 37°C during the polymerization time.
A-silicon was auto mix and polyether was hand-mixed according to the manufacturer's instructions.
After unscrewing impression copings, all the impressions were removed in the right angle to occlusal plan and checked for accuracy. If any inaccuracy, such as bubble, drag, or nonhomogeneous mix of materials was detected, the impression would be repeated. Then, implant analogues were screwed to the impression copings in the impression.
After 24 h, the impressions were poured using an type IV die stone (Herostone, Vigodent, Rio de Janeiro, Brazil), in accordance with manufacturer's instructions. To minimize the alteration of the setting expansion of the die stone, all the impressions were poured using a single prefabricated mold. All casts were stored at room temperature (23°C) and 50% relative humidity for a minimum of 24 h prior to measurements. All clinical and laboratory procedures were performed by the same operator.
Measurements
A coordinate measuring machine (CMM) (Mitutoyo Corp, Aurora, Ill, USA) was used to evaluate the positional accuracy of the samples. The machine probe moved within its limit in the space and measured the relative distances of the objects [Figure 3]. The measurement accuracy of the instrument was 0.001 mm for X, Y and Z-axis; all the measurements were made by the one operator.
Figure 3.

The coordinate measuring machine probe measuring the relative distances of analogues.
The following measuring protocol was used throughout the study: the analogues were denoted by 1-4 from left to right [Figure 4]. The center of the analogue 1 was determined as a reference point. The planar surface from this point was regarded as XY. An imaginary XZ line was considered between the centers of the analogue 1 and 4. The XZ plane was perpendicular to XY plane. Therefore the center of analogue 1 was laid on the origin (0, 0, 0) and the center of analogue 4 was laid on the XZ plane (X, 0, Z) For each analogue in the master models as well as the definitive casts, CMM measured the Cartesian coordinates (X, Y and Z) of each analogue with respect to the determined reference axis. In order to find the euclidean distance between each pair of analogues, the difference between their coordinate values in each dimension was computed (denoted as Δx, Δy and Δz). Thus, six distance values (d =  ) were measured on the master models as well as the experimental samples (denoted as d1 to d6), as shown in Figure 4. In all dimensions, measurements were repeated 3 times and the mean was used for the analysis. Having computed the difference values between the master model distance values and those of the cast, six distortion values were obtained for each cast, (denoted as Δd1 to Δd 6). The total three-dimensional distortion value for a sample cast was then obtained from the summation of Δd 1 to Δd 6. The data were transferred to SPSS software (SPSS Inc., Chicago, IL, USA) for the purpose of analysis. Two-way analysis of variance (ANOVA), one-way ANOVA and Tukey tests were used for data analysis (α = 0.05).
) were measured on the master models as well as the experimental samples (denoted as d1 to d6), as shown in Figure 4. In all dimensions, measurements were repeated 3 times and the mean was used for the analysis. Having computed the difference values between the master model distance values and those of the cast, six distortion values were obtained for each cast, (denoted as Δd1 to Δd 6). The total three-dimensional distortion value for a sample cast was then obtained from the summation of Δd 1 to Δd 6. The data were transferred to SPSS software (SPSS Inc., Chicago, IL, USA) for the purpose of analysis. Two-way analysis of variance (ANOVA), one-way ANOVA and Tukey tests were used for data analysis (α = 0.05).
Figure 4.
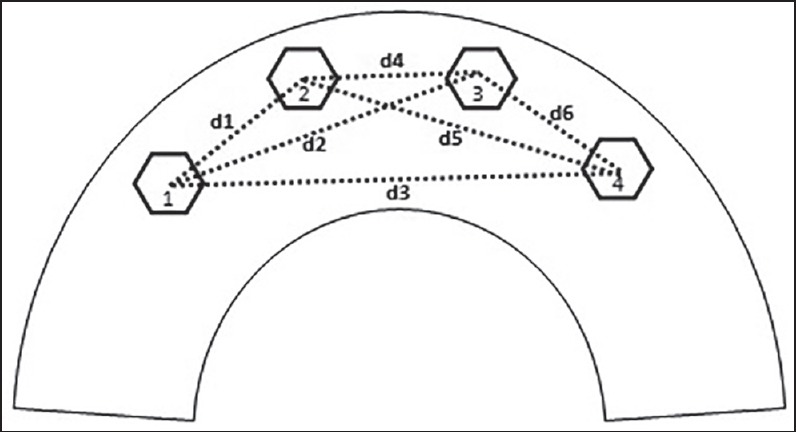
A schematic view of the reference points used to measure the distances.
RESULTS
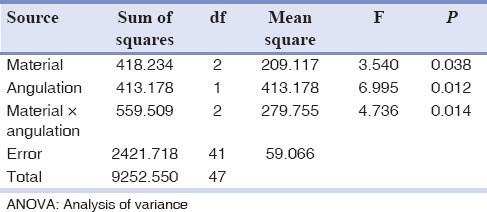
Table 1 presents the mean values and standard deviations of the studied groups. Two-way ANOVA showed that there were significant differences between the materials and angulations, as well as their interactions (P < 0.05) [Table 2]. One-way ANOVA showed that there was no significant difference between the three impression materials in the parallel condition (P = 0.74). However, there was a significant difference in the nonparallel condition (P = 0.01). Tukey test was performed for multiple comparisons. In the presence of angulated implants, Monopren showed more accurate results compared to Impregum (P = 0.01) but no significant difference was observed between Identium/Impregum (P = 0.27), and Identium/Monopren (P = 0.26)
Table 1.
Mean values and SDs of the measured distances of the studied groups (mm)
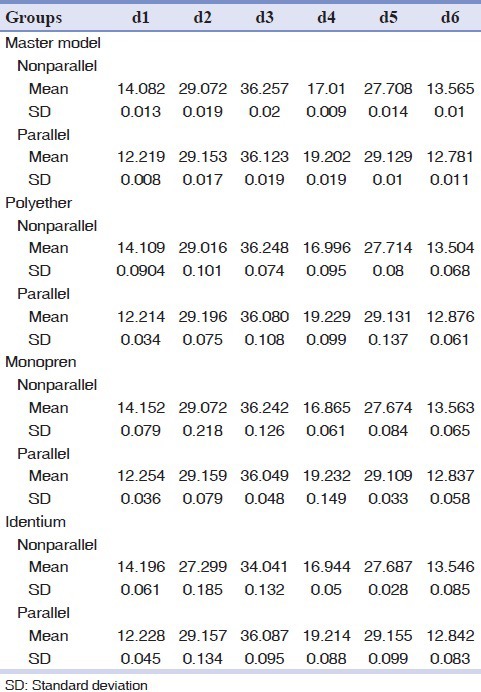
Table 2.
Two-way ANOVA
DISCUSSION
According to the recorded data, the null hypothesis was partially rejected because the accuracy of the impression materials was only different in non-parallel implants.
The impression material should be accurate (showing minimal distortion) with adequate rigidity (holding the impression coping tightly to prevent accidental displacement).[25,34,38,39] Some researchers investigated medium-body-consistency polyether and heavy-body-consistency PVS materials. Both materials were observed to meet the two previously mentioned requirements of impression materials.[25,31,32] Other studies assessed mechanical properties of heavy-body PVS and polyether and concluded that PVSs with greater modulus of elasticity would result in better accuracy in comparison to polyether.[33]
Moreover, the physical retention in the impression tray and also the application of appropriate adhesive play crucial roles in the dimensional stability of impression materials. Impression coping with physical retention probably has a significant effect on the reduction of minor movement of impression copings during clinical and laboratory procedures.
Fixture-level impression allows a selection of the most proper abutments. Then, it is mostly helpful in situations where angulation of the abutments and the vertical space are difficult to be determined intraorally. Moreover, since fixture-level impression eliminates the need to cover the abutments with temporary restorations or protective caps, replacement of the healing caps will be facilitated.[1,3]
While the findings of most studies conducted so far showed no difference between the direct and indirect impression techniques, there were few investigations which reported the superiority of open tray technique. Carr[38] mentioned that in closed tray technique, using polyether in nonparallel situation, leads to deformation of the impression.
The accuracy of the implant level impression technique may be affected by the connection structure. Unlike the external-hexagon implant, which has a short hexagon, some implants with the internal connection have longer walls of relative parallelism which complicates the removal of impression.[3]
Vigolo et al.[2] reported that the splinted technique led to more accurate definitive casts when multiple internal-connection implants with an almost parallel configuration were to be restored. The inaccuracy of the impression would be exaggerated in internal connection implants with longer walls of relative parallelism.[3]
In such cases, it might be impossible to remove the rigid splinted internal-connection. Hence, this will necessitate the use of no splinted impression copings.[2]
To the best of our knowledge, the only study which has assessed vinyl siloxanether- a new material which is categorized between A-silicone and polyether material - was performed by Enkling et al.[35] They investigated the subjective and objective clinical fit of dental prosthesis made by using polyether (Impregum penta) and Identium. Both materials showed comparable results. However, Identium indicated superiority about subjective assessment of the dentist (handling, taste, precision detail of impression) and the dental technician (the ease of removing plaster model from the mold).[35]
In general, the results of the present study are in line with those of the previous studies,[38,39,40,41] showing no difference between PVS and polyether in multi-implant impression in the parallel situation.
Identium appears to be a good alternative for PVS and polyether in the parallel situations in partially edentulous arches.
Parallel placement of the implant may ease the removal of impressions. Therefore, it probably reduces the distortion of impressions in partially dentate arches. The angulations of the teeth, the relations of the teeth to implants and the amount of undercuts influence the ease of removal. The presence of teeth in partially dentate arches causes the anatomical undercuts which increase both the removal forces and the consequent impression distortion.
In brief, the results obtained in a parallel situation using three impression materials were all comparably satisfactory.
Some studies have indicated the superiority of polyether in the parallel conditions compared to angulated ones.[1,3] In the present study, polyether has shown a tendency toward the increase of mean distortion value with the implant angulations. The measurements of Identium demonstrated noninferiority of the Identium in the angulated situation in comparison with the PVS. Some scholars suggest polyether as the best choice for complete edentulous multi-implant impressions, due to its rigidity.[3] Nevertheless, in partially edentulous arches, this material makes the withdrawal of the impression more difficult. Thus, it probably increases permanent deformations.[38,39,40] On the other hand, PVS, due to its more favorable lower rigidity, is considered as a viable alternative. It can be used more safely in partially edentulous particularly in nonparallel situations.[40,41]
Lee et al.[8] concluded that, in subgingival implant placement, PVS showed greater accuracy than polyether; however, there was no effect of implant depth on the accuracy of PVS group.
The findings of this study support the use of PVS (Monopren) for partially edentulous multi-unit angulated implant impressions.
The implant system can influence the impression accuracy in different ways: The design and the length of impression copings, the connection length and the machining tolerance of the system (defined as the difference in rest positions between the components when they are connected by their screws). Ma et al.[29] concluded that connecting a component can induce as much displacement as that resulting only from an impression or cast fabrication. Given that, we did not measure this tolerance; hence, the results should be interpreted with caution. It must be assumed that this tolerance might have significantly affected the distortion beyond the inaccuracy of impression material itself in the present study.
The design of the present study involved a few limitations. The measured distortion values did not completely evaluate the axial rotations of the components. The present investigation was carried out using four implants; therefore, the results may not necessarily be generalized for impressions made using higher numbers of implants. The implant angulations performed throughout the experiments were all limited to 30°. Finally, in this study, only internal connection implants were used, and external connections were not considered at all.
Further clinical investigations would be necessary to confirm the results of the present in vitro study. Even though we tried to simulate the clinical situations closely, further in vivo studies would be essential to yield more clinically applicable findings. The comprehensive characteristic of vinyl siloxanether ought to be more clarified through further investigations.
CONCLUSION
Within the limitations of this study, the following conclusions can be drawn:
The presence of undercuts and the implant angulation both negatively affected the precision of the impressions.
In the presence of nonparallel implants, the use of additional silicones resulted in more accurate casts than polyether.
In the presence of parallel implants, there were no significant differences among all the three materials.
ACKNOWLEGMENTS
The authors thank the Vice-Chancellory of Shiraz University of Medical Sciences for supporting this research. This article is based on the thesis by Dr. Elham Ansarifard. The authors also thank Dr. M. Vossugh of the Dental Research Development Center, School of Dentistry for the statistical analysis and Dr. Sh. Hamedani for English editing of the manuscript.
This project was also financially supported by Dio Implant System Co., and Kettenbach GmbH and Co., KG for which authors would like to thankfully acknowledge.
Footnotes
Source of Support: Nil.
Conflicts of Interest: The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- Choi JH, Lim YJ, Yim SH, Kim CW. Evaluation of the accuracy of implant-level impression techniques for internal-connection implant prostheses in parallel and divergent models. Int J Oral Maxillofac Implants. 2007;22:761–8. [PubMed] [Google Scholar]
- 2.Vigolo P, Fonzi F, Majzoub Z, Cordioli G. An evaluation of impression techniques for multiple internal connection implant prostheses. J Prosthet Dent. 2004;92:470–6. doi: 10.1016/j.prosdent.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Sorrentino R, Gherlone EF, Calesini G, Zarone F. Effect of implant angulation, connection length, and impression material on the dimensional accuracy of implant impressions: An in vitro comparative study. Clin Implant Dent Relat Res. 2010;12(Suppl 1):e63–76. doi: 10.1111/j.1708-8208.2009.00167.x. [DOI] [PubMed] [Google Scholar]
- 4.Walton JN, MacEntee MI. Problems with prostheses on implants: A retrospective study. J Prosthet Dent. 1994;71:283–8. doi: 10.1016/0022-3913(94)90468-5. [DOI] [PubMed] [Google Scholar]
- 5.Brunski JB. Biomechanical factors affecting the bone-dental implant interface. Clin Mater. 1992;10:153–201. doi: 10.1016/0267-6605(92)90049-y. [DOI] [PubMed] [Google Scholar]
- 6.Brunski JB. Biomechanics of oral implants: Future research directions. J Dent Educ. 1988;52:775–87. [PubMed] [Google Scholar]
- 7.Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent. 1999;81:7–13. doi: 10.1016/s0022-3913(99)70229-5. [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Ercoli C, Funkenbusch PD, Feng C. Effect of subgingival depth of implant placement on the dimensional accuracy of the implant impression: An in vitro study. J Prosthet Dent. 2008;99:107–13. doi: 10.1016/S0022-3913(08)60026-8. [DOI] [PubMed] [Google Scholar]
- 9.Cabral LM, Guedes CG. Comparative analysis of 4 impression techniques for implants. Implant Dent. 2007;16:187–94. doi: 10.1097/ID.0b013e3180587b3f. [DOI] [PubMed] [Google Scholar]
- 10.Del’Acqua MA, Arioli-Filho JN, Compagnoni MA, Mollo Fde A., Jr Accuracy of impression and pouring techniques for an implant-supported prosthesis. Int J Oral Maxillofac Implants. 2008;23:226–36. [PubMed] [Google Scholar]
- 11.Conrad HJ, Pesun IJ, DeLong R, Hodges JS. Accuracy of two impression techniques with angulated implants. J Prosthet Dent. 2007;97:349–56. doi: 10.1016/S0022-3913(07)60023-7. [DOI] [PubMed] [Google Scholar]
- 12.Wenz HJ, Hertrampf K. Accuracy of impressions and casts using different implant impression techniques in a multi-implant system with an internal hex connection. Int J Oral Maxillofac Implants. 2008;23:39–47. [PubMed] [Google Scholar]
- 13.Lee H, So JS, Hochstedler JL, Ercoli C. The accuracy of implant impressions: A systematic review. J Prosthet Dent. 2008;100:285–91. doi: 10.1016/S0022-3913(08)60208-5. [DOI] [PubMed] [Google Scholar]
- 14.Lorenzoni M, Pertl C, Penkner K, Polansky R, Sedaj B, Wegscheider WA. Comparison of the transfer precision of three different impression materials in combination with transfer caps for the Frialit-2 system. J Oral Rehabil. 2000;27:629–38. doi: 10.1046/j.1365-2842.2000.00594.x. [DOI] [PubMed] [Google Scholar]
- 15.Jannesar S, Siadat H, Alikhasi M. A dual impression technique for implant overdentures. J Prosthodont. 2007;16:327–9. doi: 10.1111/j.1532-849X.2007.00193.x. [DOI] [PubMed] [Google Scholar]
- 16.Seyedan K, Sazgara H, Kalalipour M, Alavi K. Dimensional accuracy of polyether and poly vinyl siloxane materials for different implant impression technique. Res J Appl Sci. 2008;3:257–63. [Google Scholar]
- 17.Filho HG, Mazaro JV, Vedovatto E, Assunção WG, dos Santos PH. Accuracy of impression techniques for implants. Part 2 - Comparison of splinting techniques. J Prosthodont. 2009;18:172–6. doi: 10.1111/j.1532-849X.2008.00325.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee SJ, Cho SB. Accuracy of five implant impression technique: Effect of splinting materials and methods. J Adv Prosthodont. 2011;3:177–85. doi: 10.4047/jap.2011.3.4.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burawi G, Houston F, Byrne D, Claffey N. A comparison of the dimensional accuracy of the splinted and unsplinted impression techniques for the Bone-Lock implant system. J Prosthet Dent. 1997;77:68–75. doi: 10.1016/s0022-3913(97)70209-9. [DOI] [PubMed] [Google Scholar]
- 20.Kim S, Nicholls JI, Han CH, Lee KW. Displacement of implant components from impressions to definitive casts. Int J Oral Maxillofac Implants. 2006;21:747–55. [PubMed] [Google Scholar]
- 21.Assunção WG, Cardoso A, Gomes EA, Tabata LF, dos Santos PH. Accuracy of impression techniques for implants. Part 1 – Influence of transfer copings surface abrasion. J Prosthodont. 2008;17:641–7. doi: 10.1111/j.1532-849X.2008.00308.x. [DOI] [PubMed] [Google Scholar]
- 22.Vigolo P, Majzoub Z, Cordioli G. Evaluation of the accuracy of three techniques used for multiple implant abutment impressions. J Prosthet Dent. 2003;89:186–92. doi: 10.1067/mpr.2003.15. [DOI] [PubMed] [Google Scholar]
- 23.Rashidan N, Alikhasi M, Samadizadeh S, Beyabanaki E, Kharazifard MJ. Accuracy of implant impressions with different impression coping types and shapes. Clin Implant Dent Relat Res. 2012;14:218–25. doi: 10.1111/j.1708-8208.2009.00241.x. [DOI] [PubMed] [Google Scholar]
- 24.Burns J, Palmer R, Howe L, Wilson R. Accuracy of open tray implant impressions: An in vitro comparison of stock versus custom trays. J Prosthet Dent. 2003;89:250–5. doi: 10.1067/mpr.2003.38. [DOI] [PubMed] [Google Scholar]
- 25.Daoudi MF, Setchell DJ, Searson LJ. A laboratory investigation of the accuracy of two impression techniques for single-tooth implants. Int J Prosthodont. 2001;14:152–8. [PubMed] [Google Scholar]
- 26.Bartlett DW, Greenwood R, Howe L. The suitability of head-of-implant and conventional abutment impression techniques for implant-retained three unit bridges: An in vitro study. Eur J Prosthodont Restor Dent. 2002;10:163–6. [PubMed] [Google Scholar]
- 27.Alikhasi M, Siadat H, Monzavi A, Momen-Heravi F. Three-dimensional accuracy of implant and abutment level impression techniques: Effect on marginal discrepancy. J Oral Implantol. 2011;37:649–57. doi: 10.1563/AAID-JOI-D-09-00112.1. [DOI] [PubMed] [Google Scholar]
- 28.Holst S, Blatz MB, Bergler M, Goellner M, Wichmann M. Influence of impression material and time on the 3-dimensional accuracy of implant impressions. Quintessence Int. 2007;38:67–73. [PubMed] [Google Scholar]
- 29.Ma T, Nicholls JI, Rubenstein JE. Tolerance measurements of various implant components. Int J Oral Maxillofac Implants. 1997;12:371–5. [PubMed] [Google Scholar]
- 30.Assuncao WG, Filho HG, Zaniquelli O. Evaluation of transfer impressions for osseointegrated implants at various angulations. Implant Dent. 2004;13:358–66. doi: 10.1097/01.id.0000144509.58901.f7. [DOI] [PubMed] [Google Scholar]
- 31.Akça K, Cehreli MC. Accuracy of 2 impression techniques for ITI implants. Int J Oral Maxillofac Implants. 2004;19:517–23. [PubMed] [Google Scholar]
- 32.Cehreli MC, Akça K. Impression techniques and misfit-induced strains on implant-supported superstructures: An in vitro study. Int J Periodontics Restorative Dent. 2006;26:379–85. [PubMed] [Google Scholar]
- 33.Liou AD, Nicholls JI, Yuodelis RA, Brudvik JS. Accuracy of replacing three tapered transfer impression copings in two elastomeric impression materials. Int J Prosthodont. 1993;6:377–83. [PubMed] [Google Scholar]
- 34.Wee AG. Comparison of impression materials for direct multi-implant impressions. J Prosthet Dent. 2000;83:323–31. doi: 10.1016/s0022-3913(00)70136-3. [DOI] [PubMed] [Google Scholar]
- 35.Enkling N, Bayer S, Jöhren P, Mericske-Stern R. Vinylsiloxanether: A new impression material. Clinical study of implant impressions with vinylsiloxanether versus polyether materials. Clin Implant Dent Relat Res. 2012;14:144–51. doi: 10.1111/j.1708-8208.2009.00240.x. [DOI] [PubMed] [Google Scholar]
- 36.Shetty S, Kamat G, Shetty R. Wettability changes in polyether impression materials subjected to immersion disinfection. Dent Res J (Isfahan) 2013;10:539–44. [PMC free article] [PubMed] [Google Scholar]
- 37.Christopher JB. Obtaining a high-quality impression with a new elastomeric material. J Inside Dent. 2011;7:56–61. [Google Scholar]
- 38.Carr AB. Comparison of impression techniques for a five-implant mandibular model. Int J Oral Maxillofac Implants. 1991;6:448–55. [PubMed] [Google Scholar]
- 39.Carr AB. Comparison of impression techniques for a two-implant 15-degree divergent model. Int J Oral Maxillofac Implants. 1992;7:468–75. [PubMed] [Google Scholar]
- 40.Lu H, Nguyen B, Powers JM. Mechanical properties of 3 hydrophilic addition silicone and polyether elastomeric impression materials. J Prosthet Dent. 2004;92:151–4. doi: 10.1016/j.prosdent.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 41.Schneider RL, Wee AG. Fabricating low-fusing metal casts for more accurate implant prosthodontics. J Prosthodont. 1996;5:301–3. doi: 10.1111/j.1532-849x.1996.tb00515.x. [DOI] [PubMed] [Google Scholar]


