Abstract
OBJECTIVE:
Maternal depression is a risk factor for adolescent depression; however, the effect of childhood exposure to maternal depression on adolescent engagement in health risk behaviors (eg, substance use, delinquency) is unclear.
METHODS:
We examined the relationship between maternal depressive symptoms (child’s age 4–15) and engagement in health risk behaviors at age 16 to 17 by using data from 2910 mother–youth pairs in a nationally representative prospective Canadian cohort. Maternal depressive trajectories were estimated through finite mixture modeling, and multiple regression analyses examined the relationship between maternal depressive symptoms and engagement in various health risk behaviors (linear regression) and age of debut of various behaviors (Cox regression).
RESULTS:
Five trajectories of maternal depressive symptoms were found: recurrent maternal symptoms, midchildhood exposure to maternal symptoms, adolescent exposure to maternal symptoms, mild maternal symptoms, and low symptoms. Adolescents exposed to maternal depressive symptoms during middle childhood were more likely to use common substances (alcohol, cigarettes, marijuana), engage in violent and nonviolent delinquent behavior, and have an earlier debut ages of cigarette, alcohol, marijuana, and hallucinogen use.
CONCLUSIONS:
The results of this study suggest that exposure to maternal depressive symptoms, particularly in middle childhood, is associated with greater and earlier engagement in health risk behaviors.
Keywords: depression, maternal welfare, adolescent, risk-taking, adolescent psychology
What’s Known on This Subject:
Maternal depression has been associated with adolescent engagement in risky behaviors such as substance use. However, there is a lack of longitudinal research examining timing-specific effects in this relationship.
What This Study Adds:
The results of this study indicate that youth exposed to increasing levels of maternal depressive symptoms in middle childhood are more likely to engage in substance use and delinquent behaviors and have an earlier debut age of these behaviors.
Adolescence is a developmental period characterized by multiple physiologic, behavioral, and emotional changes, including an increase in health risk behaviors, such as sexual intercourse, substance use, and delinquency.1 Substance behavior patterns tend to emerge during adolescence.2 In 2011, according to a report by the Centers for Disease Control and Prevention, 38.7% of high school students had used alcohol in the 30 days before the survey, 18% had smoked cigarettes, and 33% had been in a physical fight.3 Youth engagement in health risk behaviors has been associated with parenting factors during adolescence such as the quality of the parent–child relationship and parental engagement in health risk behaviors4,5; however, longitudinal research on earlier childhood factors may better explain the etiology of health risk behavior development.
Much of the previous research has been cross-sectional and therefore overlooks the potential contributions of childhood factors, such as exposure to parental mental illness. Maternal depression is a well-known risk factor for problematic adjustment, particularly depression, influencing youth outcomes through many pathways (eg, genetic vulnerability, parenting behaviors). Outcomes associated with exposure to maternal depression have a demonstrated relationship with engagement in health risk behaviors, such as increased stress response, childhood externalizing problems, and maladaptive affect regulation strategies.6–8 Furthermore, correlates of maternal depression, such as hostile parenting, are involved in the development of childhood aggression,9 and children of depressed mothers have demonstrated more childhood externalizing behavior.10,11 Those who do not learn to regulate aggression during childhood are the most likely to continue the use of aggressive behavior during adolescence,7 and exposure to maternal depression during middle childhood affects the development of emotional self-regulation strategies.12 However, the effect of childhood exposure to maternal depression on youth health risk behaviors is an emerging field of research.
Previous longitudinal research on maternal depression has demonstrated timing-specific effects on the offspring. For example, 1 study reported a sensitive window for exposure; youth initially exposed to maternal depression at ages 2 to 5 years had higher odds of experiencing emotional disorder.13 Another article, examining exposure during early childhood, concluded that maternal depression has differential effects on child problem behavior depending on its course.14 The first study that modeled trajectories of maternal depression that were prospectively assessed throughout childhood found chronic depression to be associated with adolescent adjustment difficulties.15 These findings underscore the importance of accounting for different patterns of maternal depression to illustrate any timing- or pattern-specific effects. The primary objective of this prospective cohort study was to investigate the effects of varying exposure to maternal depressive symptoms throughout childhood (age 4–15) on adolescent health risk behavior engagement at age 16 to 17. We hypothesized that youth exposed to high levels of maternal depression throughout childhood would engage in more health risk behavior than youth exposed to low levels of maternal depressive symptoms.
Methods
This research was approved by the Health Research Ethics Board at the University of Alberta.
Sample
This study used data from the National Longitudinal Survey of Children and Youth (NLSCY), a nationally representative population-based cohort of 16 903 Canadian children studied every 2 years beginning in 1994 to 1995 and ending in 2008 to 2009. This study examined children aged 2 to 5 during 1994 to 1995 (N = 2910) and followed them longitudinally until they reached the age of 16 to 17 (2008–2009). During data collection, the mothers of the children completed various questionnaires, used to collect general health information about themselves and their spouses or partners and information on the children’s social environment, such as maternal mental health, social support, and family functioning. Once the children reached the age of 10 to 11, they were asked to confidentially complete their own questionnaires.16
Materials
Maternal Depression
A shortened form of the Center for Epidemiologic Studies Depression Scale (CES-D), including 12 questions pertaining to the experience of certain feelings during the past week (eg, “I felt that I could not shake off the blues even with help from my family or friends,” “I felt depressed,” “I felt hopeful about the future”), was used to assess maternal depression symptoms.17 There were 4 response categories, ranging from “rarely or none of the time (<1 day)” to “most or all of the time (5–7 days).” A summative score, from 0 to 36, was calculated for each mother every 2-year survey cycle, with higher scores indicating greater depressive symptoms. Cronbach’s α for the cycle-specific CES-D scores ranged from .91 to .97, indicating excellent internal consistency, and the mean scores for the sample ranged from 3.98 to 4.81. Across the cycles, ∼10% to 17% of the sample reached the clinical cutoff score of 12, indicating the presence of depression.
Health Risk Behaviors
Adolescents were asked questions about their engagement in various health risk behaviors over the past year (eg, use of various substances, delinquent behaviors such as carrying a weapon or running away). The questions were adapted by the NLSCY Project Team from the National Longitudinal Survey of Youth at Ohio State University; the Western Australia Child Health Survey; the Youth Smoking Survey; the World Health Organization Survey on Health Behaviors in School Children; and the Northwest Territories Health Attitudes, Knowledge and Behaviors Study and included additional questions provided by Dr Richard Tremblay from the University of Montreal.18 There were 4 possible responses per item, ranging from never to 5 times or more. Questions about the age of first engagement, beginning at age 12, were asked for alcohol and drug use (cigarettes, marijuana, hallucinogens, prescription drugs, and other drugs) and sexual intercourse.
Covariates
Additional covariates were controlled for in the regression analyses because of their association with maternal depression and health risk behaviors: baseline household socioeconomic status (SES) and adolescent gender. Five standardized variables, with a mean of 0 and an SD of 1, were used by Statistics Canada to derive the SES score for the NLSCY: the level of education of the mother, the level of education of the spouse or partner, the prestige of the mother’s occupation, the prestige of the spouse or partner’s occupation, and household income. Furthermore, because the NLSCY established cohorts at 2-year intervals, included in the age range of 2 to 5 years in 1994 to 1995 are the subcohorts of 2- to 3-year-olds and 4- to 5-year-olds; therefore, we controlled for any potential cohort effects.
Statistical Analysis
We modeled trajectories of maternal depression during adolescents’ age 4 to 15 by using latent class growth analysis.19 This approach uses a finite mixture model procedure to estimate multiple subgroups within the sample; it is designed to describe the trajectory over time in the variable and model unobserved heterogeneity in the population. We implemented this procedure in SAS (SAS Institute, Inc, Cary, NC) by using PROC TRAJ, which is capable of modeling up to fourth-order polynomial relationships between age and the observed behavior.19 We assessed model fit by comparing the Bayesian information criterion (BIC) values between models and by examining the average posterior probabilities of group membership, which approximate internal reliability.19–21 The strength of the evidence favoring the more complex model (ie, greater number of trajectories) is defined as follows: Values of ≥10 for 2(∆BIC) are considered very strong evidence, values between 6 and 10 are strong evidence, values between 2 and 6 are considered positive evidence, and values between 0 and 2 are weak evidence for the alternative model.19 Generally, average posterior probabilities >0.7 are considered to indicate that the trajectory groups include individuals who follow a similar pattern and discriminate between patterns of change that are dissimilar.21 Maternal depression (CES-D) scores, measured every 2 years between child’s age 4 to 5 and 14 to 15, were the dependent variable in the mixture model, and corresponding child’s age was the independent variable.
Principal components analysis (PCA) was conducted on the frequency-based (ie, “During the past 12 months how many times have you . . .”) health risk behavior questions, assessed at age 16 to 17 to describe the empirical structure of such behaviors and simplify the items for the main analyses. Factors with eigenvalues >1 were retained, a decision that was confirmed through graphic examination of a scree plot. Because health risk behaviors tend to co-occur and cannot be assumed to be uncorrelated, oblique rotation methods were used. Factor scores were calculated for each determined factor.
To determine the relationship between trajectories of maternal depressive symptoms during childhood and engagement in patterns of health risk behavior at age 16 to 17, multiple linear regression models were used, including maternal depressive trajectory group as the main predictor variable and the factor scores for health risk behaviors as the outcome. Bivariate associations were initially tested, and subsequently the models were adjusted for the effects of gender, SES, and age cohort.
We conducted Cox regressions to compare the rates of debut engagement in behavior across the subgroups in bivariate and adjusted analyses, using the NLSCY questions pertaining to age of first engagement in the different domains of health risk behaviors (ie, “How old were you when you tried the following drugs for the first time?”). The adjusted models controlled for the effects of gender, cohort, and baseline SES. The study end date was defined as September 2009, when the data collection for Cycle 8 had been completed, and the origin was defined as the child’s birth date. The proportional hazard assumption of Cox regression models was not violated in any models. Hazard ratios were calculated to compare the age of onset of behaviors between the trajectories of maternal depressive symptoms subgroups. Finally, because the sampling variance of the NLSCY is difficult to calculate because of the complex sample design, nonresponse adjustments, and post-stratification,22 bootstrap weights provided by Statistics Canada were used in all regression analyses.
Results
Prevalence of health risk behavior engagement in this sample of 2910 youth is provided in Table 1. By age 16 to 17, prevalence of health risk behaviors ranged from rare events such as attempting suicide (1.7%) and fighting to the point of injuring someone (6.7%) to highly prevalent behaviors such as drinking alcohol (58%).
TABLE 1.
Past-Year Prevalence of Health Risk Behaviors at Age 16 to 17
| Behavior | Prevalence (%)a |
|---|---|
| Staying out all night without permission | 27.0 |
| Being questioned by police by something they suspect involvement in | 20.3 |
| Stealing something from a store or school | 19.8 |
| Intentionally damaging or destroying something | 25.7 |
| Fought someone to the point where they needed care for their injuries | 6.7 |
| Attacking someone with the intention of causing serious harm | 7.8 |
| Sold drugs | 7.9 |
| Passenger in vehicle driven under the influence | 29.3 |
| Driving a vehicle under the influence | 11.6 |
| Cigarette use | |
| Some engagement | 26.2 |
| Once or more per week | 17.8 |
| Alcohol use | |
| Some engagement | 58.0 |
| Once or more per week | 16.4 |
| Using alcohol to the point of intoxication | |
| Some engagement | 55.8 |
| Once or more per week | 11.1 |
| Marijuana use | |
| Some engagement | 35.9 |
| Once or more per week | 10.8 |
| Hallucinogen use | 8.9 |
| Other drug use | 9.1 |
| Considered suicide | 7.2 |
| Attempted suicide | 1.7 |
| Sexual intercourse | 40.8 |
Prevalence was estimated based on any engagement versus no engagement. Where possible, for certain substance use variables, prevalence of weekly use was also estimated.
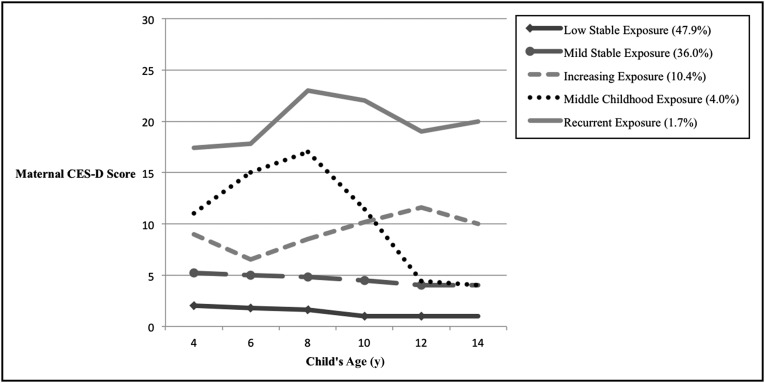
Identifying Trajectories of Maternal Depression Symptoms
There was strong evidence favoring a 5-trajectory model, 2(∆BIC) = 194.38 (Supplemental Table 5). Figure 1 displays the final model: group 1, the low stable exposure reference group (quadratic order; 47.9% of the sample); group 2, the mild stable exposure group (linear order; 36.0% of the sample); group 3, the increasing exposure group (cubic order; 10.4% of the sample); group 4, the high decreasing exposure group (cubic order; 4.0% of the sample); and finally, group 5, the high stable exposure group (quadratic order; 1.7% of the sample). The average posterior probabilities ranged from .75 (group 2) to .95 (group 5), indicating good model fit in terms of group membership.
FIGURE 1.
Five-group trajectory model of maternal CES-D scores by child’s age.
Compared with adolescents in the low stable exposure group, adolescents in all other trajectory groups had significantly lower SES scores at baseline (all P values < .004). There were no differences across trajectory groups with respect to child’s gender and cohort membership.
PCA of Adolescents’ Health Risk Behaviors
The PCA yielded 5 factors of adolescents’ health risk behaviors that had eigenvalues >1, explaining 56% of the variance in these behaviors (Table 2). Factor 1 (common substances) contained commonly used substances (cigarettes, alcohol, and marijuana) and both operating and being a passenger in a vehicle driven under the influence of substances. Factor 2 (nonviolent delinquency) contained nonviolent, delinquent behaviors: stealing, destruction of property, running away, and being out all night. Items exhibiting high loadings on Factor 3 (illicit substances) included less commonly used drugs such as hallucinogens and other drugs (eg, crack/cocaine) and selling drugs. Factor 4 (violent delinquency) contained violent, delinquent behaviors: fighting someone to the point they had to care for their injuries, attacking someone with the intent of seriously hurting them, being questioned by police over something they thought you did, and carrying a weapon. Factor 5 contained both the sexual assault and inhalant use variables.
TABLE 2.
PCA: Factor Loadings for Health Risk Behaviors
| Health Risk Behavior | Common Substances (Factor 1) | Nonviolent Delinquency (Factor 2) | Illicit Substances (Factor 3) | Violent Delinquency (Factor 4) | Sexual Assault and Inhalants (Factor 5) |
|---|---|---|---|---|---|
| Staying out all night without permission | 0.16 | 0.62 | −0.01 | −0.04 | −0.02 |
| Running away from home | −0.26 | 0.80 | 0.13 | −0.18 | −0.07 |
| Being questioned by police about something they suspect involvement in | 0.21 | 0.24 | −0.01 | 0.43 | −0.04 |
| Stealing something from a store or school | −0.01 | 0.67 | 0.04 | 0.04 | −0.01 |
| Intentionally damaging or destroying something | −0.04 | 0.69 | −0.10 | 0.23 | −0.05 |
| Fought someone to the point where they needed care for their injuries | −0.02 | −0.05 | 0.05 | 0.86 | −0.05 |
| Attacking someone with the intention of causing serious harm | 0.02 | −0.07 | −0.03 | 0.81 | 0.07 |
| Sold drugs | 0.06 | 0.15 | 0.39 | 0.19 | 0.11 |
| Attempting to touch anyone in a sexual way without consent | −0.07 | −0.04 | −0.12 | 0.06 | 0.81 |
| Passenger in vehicle driven under the influence of alcohol or other drugs | 0.52 | 0.23 | 0.06 | −0.19 | 0.23 |
| Driving a vehicle under the influence of alcohol or drugs | 0.41 | 0.20 | −0.16 | −0.09 | 0.39 |
| Cigarette use | 0.54 | 0.07 | 0.27 | 0.04 | −0.11 |
| Alcohol use | 0.92 | −0.16 | −0.09 | 0.01 | −0.04 |
| Using alcohol to the point of intoxication | 0.89 | 0.10 | −0.02 | 0.04 | −0.06 |
| Marijuana use | 0.59 | 0.01 | 0.36 | 0.01 | −0.08 |
| Hallucinogen use | 0.07 | −0.04 | 0.80 | 0.03 | −0.02 |
| Glue or other inhalant use | −0.12 | 0.18 | 0.32 | −0.03 | 0.59 |
| Illicit use of prescription drugs | −0.08 | −0.01 | 0.72 | 0.01 | 0.03 |
| Other drug (eg, crack, heroin) use | 0.01 | 0.07 | 0.85 | −0.03 | −0.05 |
| Eigenvalue (% of variance) | 4.19 (21%) | 4.07 (20%) | 3.91 (20%) | 3.19 (16%) | 1.92 (10%) |
Maternal Depressive Trajectories and Adolescent Health Risk Behaviors
Compared with adolescents in the low stable group (trajectory group 1), only the middle childhood exposure group (trajectory group 4) had higher scores for common substance use (P = .005; Table 3). Adolescents exposed to high symptoms during middle childhood but decreasing symptoms by adolescence (trajectory group 4) and recurrent maternal depressive symptoms (trajectory group 5) had significantly higher factor scores for nonviolent delinquent behaviors than adolescents exposed to very low levels of maternal depressive symptoms (P = .03, and .01, respectively). Adolescents exposed during middle childhood (trajectory group 4) had significantly higher illicit substance scores than adolescents in the low stable group; however, this was only found in the unadjusted analysis (P = .05). These adolescents also had significantly higher violent delinquent behavior scores than adolescents exposed to very few maternal depressive symptoms in both the crude (P = .01) and adjusted (P = .02) models.
TABLE 3.
Associations Between Maternal Depression Trajectory Group and Health Risk Behavior Factor 1–5 Scores
| Outcome | Mild Maternal Depressive Symptoms (Trajectory Group 2) | Maternal Depressive Symptoms During Adolescence (Trajectory Group 3) | Maternal Depressive Symptoms During Midchildhood (Trajectory Group 4) | Recurrent Maternal Depressive Symptoms (Trajectory Group 5) | |
|---|---|---|---|---|---|
| Common substance (Factor 1) scores, (95% CI) | Crude | 0.02 (−0.16 to 0.20) | 0.19 (−0.16 to 0.57) | 0.48** (0.17 to 0.80) | 0.16 (−0.42 to 0.74) |
| Regressiona | |||||
| Adjustedb | −0.002 (−0.21 to 0.20) | 0.14 (−0.30 to 0.57) | 0.44** (0.14 to 0.75) | 0.04 (−0.57 to 0.65) | |
| Regression | |||||
| Nonviolent delinquent (Factor 2) scores, (95% CI) | Crude | 0.16 (−0.04 to 0.36) | 0.24 (−0.08 to 0.56) | 0.45* (0.08 to 0.82) | 1.05* (0.22 to 1.89) |
| Adjusteda | 0.12 (−0.09 to 0.33) | 0.26 (−0.10 to 0.62) | 0.41* (0.03 to 0.79) | 1.01* (0.20 to 1.81) | |
| Illicit substance (Factor 3) scores, (95% CI) | Crude | 0.09 (−0.07 to 0.25) | 0.17 (−0.10 to 0.46) | 0.49* (−0.01 to 0.99) | 0.15 (−0.24 to 0.54) |
| Adjusteda | 0.07 (−0.10 to 0.24) | 0.10 (−0.21 to 0.40) | 0.45 (−0.09 to 0.99) | 0.06 (−0.34 to 0.47) | |
| Violent delinquent (Factor 4) scores, (95% CI) | Crude | 0.24 (−0.01 to 0.48) | −0.04 (−0.29 to 0.21) | 0.64* (0.16 to 1.13) | 0.48 (−0.14 to 1.09) |
| Adjusteda | 0.22 (−0.06 to 0.49) | −0.001 (−0.25 to 0.25) | 0.55* (0.09 to 1.00) | 0.44 (−0.13 to 1.01) | |
| Sexual assault (Factor 5) scores, (95% CI) | Crude | 0.12 (−0.01 to 0.25) | 0.07 (−0.15 to 0.28) | −0.014 (−0.39 to 0.36) | −0.003 (−0.30 to 0.29) |
| Adjusteda | 0.10 (−0.05 to 0.24) | 0.03 (−0.21 to 0.26) | −0.05 (−0.45 to 0.34) | −0.04 (−0.37 to 0.29) | |
P < .05. **P < .005.
Results from multiple linear regression models with 5 factor scores as dependent variables, respectively, and regression coefficients indicate the average differences in the scores between trajectory groups 2, 3, 4, and 5 and group 1.
Adjusted for gender, SES, and cohort.
Maternal Depressive Trajectories and Debut Age of Health Risk Behaviors
Adolescents exposed to maternal depressive symptoms during middle childhood (trajectory group 4; hazard ratio [HR] 2.15; 95% confidence interval [CI], 1.48 to 3.13; P < .001) engaged in cigarette use earlier than adolescents exposed to very few maternal depressive symptoms (Table 4). A similar pattern was observed with respect to alcohol use (HR = 1.43), marijuana use (HR = 1.91), and hallucinogen use (HR = 3.51) compared with adolescents exposed to very few maternal depressive symptoms. Finally, although significant associations were found for the mild exposure group (trajectory group 2; HR 1.28; 95% CI, 1.01 to 1.62; P = .04) and the recurrent group (trajectory group 5; HR 1.98; 95% CI, 1.04 to 3.79; P = .04) for sexual intercourse in the bivariate analysis, this significant effect was attenuated upon adjustment.
TABLE 4.
Cox Regression Model Associations Between Maternal Depression Trajectory Group and Time of Onset of Health Risk Behaviors
| Outcome | Mild Maternal Depressive Symptoms (Trajectory Group 2) | Maternal Depressive Symptoms During Adolescence (Trajectory Group 3) | Maternal Depressive Symptoms During Midchildhood (Trajectory Group 4) | Recurrent Maternal Depressive Symptoms (Trajectory Group 5) | |
|---|---|---|---|---|---|
| Cigarette use, (95% CI) | Crude | 1.27* (1.02 to 1.57) | 1.17 (0.77 to 1.77) | 2.18** (1.52 to 3.13) | 1.15 (0.80 to 1.67) |
| HRa | |||||
| Adjustedb | 1.25* (1.00 to 1.56) | 1.01 (0.63 to 1.62) | 2.15** (1.48 to 3.12) | 0.92 (0.44 to 1.92) | |
| HR | |||||
| Alcohol use, (95% CI) | Crude | 1.15* (1.02 to 1.31) | 0.96 (0.70 to 1.31) | 1.37* (1.05 to 1.80) | 1.16 (0.80 to 1.67) |
| Adjusteda | 1.14 (0.99 to 1.31) | 0.95 (0.68 to 1.34) | 1.43* (1.05 to 1.96) | 1.31 (0.87 to 1.98) | |
| Alcohol use to intoxication, (95% CI) | Crude | 1.12 (0.93 to 1.36) | 0.85 (0.57 to 1.26) | 1.14 (0.7 to 1.88) | 1.14 (0.67 to 1.94) |
| Adjusteda | 1.03 (0.89 to 1.20) | 0.90 (0.62 to 1.29) | 1.28 (0.82 to 2.01) | 1.04 (0.59 to 1.87) | |
| Marijuana use, (95% CI) | Crude | 1.28* (1.05 to 1.57) | 1.05 (0.72 to 1.53) | 1.78* (1.10 to 2.86) | 1.28 (0.71 to 2.32) |
| Adjusteda | 1.24* (1.01 to 1.51) | 0.99 (0.65 to 1.51) | 1.91* (1.15 to 3.16) | 1.33 (0.72 to 2.47) | |
| Hallucinogen use, (95% CI) | Crude | 1.48 (0.93 to 2.38) | 1.33 (0.70 to 2.53) | 3.52* (1.32 to 9.38) | 1.11 (0.01 to 238.74) |
| Adjusteda | 1.52 (0.91 to 2.53) | 1.04 (0.43 to 2.50) | 3.51* (1.26 to 9.77) | 1.12 (0.01 to 218.22) | |
| Other drugs (eg, crack/cocaine) use, (95% CI) | Crude | 1.95** (1.25 to 3.03) | 1.86 (0.94 to 3.69) | 1.59 (0.63 to 4.01) | 2.51 (0.09 to 69.53) |
| Adjusteda | 1.77* (1.13 to 2.77) | 1.23 (0.56 to 2.70) | 1.43 (0.59 to 3.50) | 1.59 (0.04 to 62.34) | |
| Sexual intercourse, (95% CI) | Crude | 1.28* (1.01 to 1.62) | 1.15 (0.78 to 1.69) | 1.20 (0.69 to 2.08) | 1.98* (1.04 to 3.79) |
| Adjusteda | 1.26 (0.98 to 1.62) | 1.00 (0.65 to 1.54) | 1.28 (0.74 to 2.24) | 1.86 (0.89 to 3.86) | |
P < .05. ** P < .005.
Results from Cox regression models with binary health risk behaviors and time of debut of these behaviors as outcomes, respectively. Hazard ratios compare trajectory groups 2, 3, 4, and 5 with group 1.
Adjusted for SES, gender, and cohort.
Discussion
The affective outcomes that may arise after childhood exposure to maternal depression are well documented, occurring throughout childhood into young adulthood,23,24 yet longitudinal behavioral outcomes warrant additional study. The results of this large population-based study are congruent with the hypothesis that childhood exposure to maternal depressive symptoms is associated with greater and earlier adolescent engagement in health risk behaviors. These behaviors are undoubtedly prevalent during adolescence; almost 20% of this sample reported weekly cigarette use, and almost 60% had consumed alcohol to the point of intoxication (10% were doing so weekly).
The results from this research indicate that those exposed to maternal depressive symptoms during middle childhood engaged in more health risk behaviors than those exposed to low symptoms, including violent and nonviolent delinquent behaviors, and substance use. Adolescents exposed to recurrent maternal symptoms throughout childhood engaged in more nonviolent delinquent behaviors than those exposed to low symptoms. However, those exposed to increasing depressive symptoms during early adolescence did not engage in more health risk behaviors.
These results may reflect early development of a lasting behavioral pattern, resulting from earlier exposure to maternal depression. Middle childhood is a period of increasing cognitive, social, and emotional development; children in this age group begin school, refine their linguistic skills, and increasingly engage in social peer relationships. Cognitive and socioemotional development may be particularly relevant to the development of both internalizing and externalizing behavioral patterns. During childhood, mothers are able to foster development through responsive parenting behaviors.25,26 Conversely, pathways through which maternal depression affects the child include exposure to maladaptive maternal affect and behaviors, as well as exposure to the stressful environmental context associated with maternal depression.23,24 Exposure to maternal depressive symptoms, and the associated negative parenting behaviors during middle childhood, as the child enters a stage of increased development may result in lasting developmental deficits, predisposing the child to future health risk behavior. Children may be more sensitive to the symptoms of maternal depression during this age window, resulting in lasting effects for adolescents.
Furthermore, our results indicated that exposure to maternal depressive symptoms during middle childhood was associated with earlier adolescent engagement in substance use, including cigarettes, alcohol, marijuana, and hallucinogens at an earlier age. Therefore, not only are adolescents exposed to high maternal depressive symptoms during childhood engaging in more health risk behaviors, they do so earlier than adolescents exposed to few maternal depressive symptoms. Again, this may suggest the early development of lasting behavioral patterns, because childhood externalizing behaviors not only have been associated with greater engagement in substance use, but are also linked to earlier engagement.27 This notion of behavioral continuity is supported by research that found that high levels of externalizing behaviors, including aggression, at earlier ages predicts the later engagement in problem behaviors, including substance use.27,28,30 It is a robust finding that debut age of drug use predicts later substance abuse and future engagement in additional health risk behaviors.31,32 Additional consequences of early substance use may be reflected in increased suicide risk,33 which itself represents a significant proportion of young adult and adolescent mortality.
Surprisingly, however, adolescents in the recurrent maternal depression group had only significantly higher nonviolent delinquency scores and did not have significantly higher factor scores on the remaining behaviors. It was also unexpected that these youth did not engage in substance use earlier. These findings were not anticipated, because there is an established association between adolescent psychopathology, including internalizing disorders such as depression, and an earlier onset of substance use.34 Although this finding may reflect inadequate power for the sample size in the recurrent depression group (1.64% of the sample fell into group 5), it may also reflect differences in adolescent outcomes associated with varied timing of exposure to or severity of maternal depressive symptoms. The children exposed to recurrent maternal depression were exposed to more severe depressive symptoms, which may have had effects different from those of midchildhood exposure followed by remittance.
Limitations
There are methodological considerations to note for this study. The main outcome measure, health risk behavior, was self-reported by the youth and is therefore subject to potential biases such as social desirability bias; however, it is likely that these behaviors are underreported rather than overreported. Additionally, the weighted estimate of attrition in this sample was 37.47%; attrition may have affected the results, because those with higher depressive scores, higher number of stressful life events and alcohol use, and lower SES dropped out from the study, and the adolescent engagement in health risk behavior for this higher-risk group was not assessed. Finally, this research was limited to maternal depressive symptoms, because in cycle 1 of the NLSCY, 91.3% of the children’s main parental survey respondents were mothers. Research suggests that paternal depression similarly affects children,35 but this potential association was beyond the methodological scope of the present study.
Despite these limitations, this research had notable methodological strengths over some past research. These strengths include the use of a nationally representative cohort with a large sample size and bootstrap weighting; the longitudinal nature of the data, which allows stronger temporal inference; and the prospective collection of maternal depressive symptoms (as opposed to retrospective data collection). Although the assessment of depressive symptoms over the past 2 weeks may be prone to some recall bias, depressive scores were systematically collected every 2 years during the participants’ lifetimes, as opposed to retrospective assessment, which also allowed trajectory modeling.
It is important to note that although using trajectory modeling as a categorical variable is useful in describing longitudinal data, allowing clusters of individuals who follow similar behavioral trajectories over time to be identified, and used in additional statistical inference,19 these discrete trajectories may not fully represent real-world phenomena, and caution must be taken in interpreting the findings with respect to membership in distinct maternal depression groups. The use of trajectories with respect to childhood exposure to maternal depressive symptoms allows group membership to be inferred from the longitudinal CES-D scores. Although the group size for the recurrent maternal depression group was small, the trajectory model selected best represented the observed data on maternal depressive symptoms, thereby improving estimates of patterns of childhood exposure to maternal depression.
The results of this study suggest that exposure to maternal depressive symptoms in childhood is associated with greater, earlier engagement in health risk behaviors, and they suggest a sensitive period in midchildhood during which exposure to maternal depressive symptoms appears to have the strongest effects on adolescent engagement in delinquent and substance use behaviors. Engagement in risky behaviors, which are increasingly prevalent during the adolescent years, may be associated with severe immediate and future morbidity and mortality risks. Consequently, identification and treatment of depressed mothers during midchildhood years may have an impact in reducing the engagement in health risk behaviors in adolescence and associated long-term sequelae.
Supplementary Material
Acknowledgment
The authors thank Irene Wong of Statistics Canada for her assistance with data access and use. The research and analysis are based on data from Statistics Canada, and the opinions expressed do not represent the views of Statistics Canada.
Footnotes
Ms Wickham conceived and designed the study, designed the data analysis strategy, conducted the data analysis, and drafted the initial manuscript; Drs Senthilselvan, Wild, and Hoglund contributed to and refined the study design and analytic strategy, interpreted results, and critically reviewed and revised the manuscript; Dr Colman conceived and designed the study, designed the data analysis strategy, interpreted results, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by a grant from the SickKids Foundation and the Canadian Institutes of Health Research (grant SKF 116328). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program for I.C. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24(4):417–463 [DOI] [PubMed] [Google Scholar]
- 2.Bonomo YA, Bowes G, Coffey C, Carlin JB, Patton GC. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction. 2004;99(12):1520–1528 [DOI] [PubMed] [Google Scholar]
- 3.Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control and Prevention (CDC) . Youth risk behavior surveillance: United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162 [PubMed] [Google Scholar]
- 4.Hoeve M, Dubas JS, Gerris JR, van der Laan PH, Smeenk W. Maternal and paternal parenting styles: unique and combined links to adolescent and early adult delinquency. J Adolesc. 2011;34(5):813–827 [DOI] [PubMed] [Google Scholar]
- 5.Gault-Sherman M. It’s a two-way street: the bidirectional relationship between parenting and delinquency. J Youth Adolesc. 2012;41(2):121–145 [DOI] [PubMed] [Google Scholar]
- 6.Auerbach RP, Claro A, Abela JRZ, Zhu X, Yao S. Understanding risky behavior engagement amongst Chinese adolescents. Cognit Ther Res. 2010;34(2):159–167 [Google Scholar]
- 7.Tremblay RE, Nagin DS, Séguin JR, et al. Physical aggression during early childhood: trajectories and predictors. Pediatrics. 2004;114(1). Available at: www.pediatrics.org/cgi/content/full/114/1/e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baldwin JA, Brown BG, Wayment HA, Nez RA, Brelsford KM. Culture and context: buffering the relationship between stressful life events and risky behaviors in American Indian youth. Subst Use Misuse. 2011;46(11):1380–1394 [DOI] [PubMed] [Google Scholar]
- 9.Côté SM, Vaillancourt T, Barker ED, Nagin D, Tremblay RE. The joint development of physical and indirect aggression: predictors of continuity and change during childhood. Dev Psychopathol. 2007;19(1):37–55 [DOI] [PubMed] [Google Scholar]
- 10.Civic D, Holt VL. Maternal depressive symptoms and child behavior problems in a nationally representative normal birthweight sample. Matern Child Health J. 2000;4(4):215–221 [DOI] [PubMed] [Google Scholar]
- 11.Essex MJ, Klein MH, Cho E, Kraemer HC. Exposure to maternal depression and marital conflict: gender differences in children’s later mental health symptoms. J Am Acad Child Adolesc Psychiatry. 2003;42(6):728–737 [DOI] [PubMed] [Google Scholar]
- 12.Silk JS, Shaw DS, Skuban EM, Oland AA, Kovacs M. Emotion regulation strategies in offspring of childhood-onset depressed mothers. J Child Psychol Psychiatry. 2006;47(1):69–78 [DOI] [PubMed] [Google Scholar]
- 13.Naicker K, Wickham M, Colman I. Timing of first exposure to maternal depression and adolescent emotional disorder in a national Canadian cohort. PLoS ONE. 2012;7(3):e33422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cents RA, Diamantopoulou S, Hudziak JJ, et al. Trajectories of maternal depressive symptoms predict child problem behaviour: the Generation R study. Psychol Med. 2013;43(1):13–25 [DOI] [PubMed] [Google Scholar]
- 15.Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. J Abnorm Psychol. 2009;118(3):479–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Statistics Canada National Longitudinal Survey of Children and Youth: Overview of Survey Instruments for 1994–1995 Data Collection—Cycle 1. Ottawa, Ontario: Statistics Canada; 1995 [Google Scholar]
- 17.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401 [Google Scholar]
- 18.Human Resources Canada and Skills Development Canada National Longitudinal Survey of Children and Youth, Cycle 5. User Guide. Ottawa, ON: Statistics Canada; 2003 [Google Scholar]
- 19.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–393 [Google Scholar]
- 20.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138 [DOI] [PubMed] [Google Scholar]
- 21.Andruff H, Carraro N, Thompson A, Gaudreau P. Latent class growth modelling: a tutorial. Quant Methods Psychol. 2009;5(1):11–24 [Google Scholar]
- 22.Statistics Canada National Longitudinal Survey of Children and Youth: Microdata User Guide—Cycle 6. Ottawa, ON: Statistics Canada; 2005 [Google Scholar]
- 23.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106(3):458–490 [DOI] [PubMed] [Google Scholar]
- 24.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27 [DOI] [PubMed] [Google Scholar]
- 25.Landry SH, Smith KE, Miller-Loncar CL, Swank PR. Predicting cognitive-language and social growth curves from early maternal behaviors in children at varying degrees of biological risk. Dev Psychol. 1997;33(6):1040–1053 [DOI] [PubMed] [Google Scholar]
- 26.Smith KE, Landry SH, Swank PR. The role of early maternal responsiveness in supporting school-aged cognitive development for children who vary in birth status. Pediatrics. 2006;117(5):1608–1617 [DOI] [PubMed] [Google Scholar]
- 27.Thompson R, Tabone JK, Litrownik AJ, et al. Early adolescent risk behavior outcomes of childhood externalizing behavioral trajectories. J Early Adolesc. 2011;31(2):234–257 [Google Scholar]
- 28.Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol. 2002;14(1):179–207 [DOI] [PubMed] [Google Scholar]
- 29.Goodman A. Substance use and common child mental health problems: examining longitudinal associations in a British sample. Addiction. 2010;105(8):1484–1496 [DOI] [PubMed] [Google Scholar]
- 30.Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: a developmental cascade model. Dev Psychopathol. 2010;22(4):883–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mason WA, Hitch JE, Kosterman R, McCarty CA, Herrenkohl TI, Hawkins JD. Growth in adolescent delinquency and alcohol use in relation to young adult crime, alcohol use disorders, and risky sex: a comparison of youth from low- versus middle-income backgrounds. J Child Psychol Psychiatry. 2010;51(12):1377–1385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brook JS, Adams RE, Balka EB, Whiteman M, Zhang C, Sugerman R. Illicit drug use and risky sexual behavior among African American and Puerto Rican urban adolescents: the longitudinal links. J Genet Psychol. 2004;165(2):203–220 [PubMed] [Google Scholar]
- 33.Cho H, Hallfors DD, Iritani BJ. Early initiation of substance use and subsequent risk factors related to suicide among urban high school students. Addict Behav. 2007;32(8):1628–1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J Consult Clin Psychol. 2002;70(6):1224–1239 [DOI] [PubMed] [Google Scholar]
- 35.Ramchandani P, Stein A, Evans J, O’Connor TG, ALSPAC Study Team . Paternal depression in the postnatal period and child development: a prospective population study. Lancet. 2005;365(9478):2201–2205 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.