Abstract
Malpositioning of cervical screws risks neurovascular injury. A cervical screw fixation system can provide proper rigidity, alignment correction, and high rates of fusion afforded by high pullout biomechanical strength. The objective is to assess the dimensions and axis of the C3–C7 cervical pedicles. A 1-mm slice thickness computed tomography (CT) scan of the cervical spine of 30 patients (15 males, 15 females) were analyzed and reconstructed in three-dimensions using Mimics® 10.01 software. We measured pedicle axis length (PAL), pedicle and lateral mass length (PL-LM), pedicle length (PL), outer pedicle width (OPW), and pedicle transverse angle (PTA) from the axial image and outer pedicle height (OPH) and pedicle sagittal angle (PSA) from the sagittal image. The OPH and OPW at all subaxial cervical spines were suitable for insertion of 3.5 mm cervical pedicle screws. PSA was directed cranially at C3 to C5 (13.84, 7.09, and 2.71) and directed caudally at C6 and C7 (–4.55, –6.94). PTA was greatest at C5 and smallest at C7. The respective difference between the left and right side for nearly all parameters was not statistically significant (except for C6 PL and C7 OPH). Females had a significantly smaller OPH and OPW than males at nearly all levels. The PTA was not significantly different between the sexes. Cervical pedicle screw fixation in the Thai population can be safely performed and guidelines for insertion at each vertebra documented. Appropriate preoperative planning is necessary to achieve safe and accurate placement of the screws.
Keywords: cervical pedicle, subaxial cervical pedicle, pedicle morphology, three-dimensional computed tomography reconstruction
Introduction
Subaxial pedicle screw fixation was recently considered an alternative to lateral mass (LM) screw fixation for posterior cervical spine stabilization. Abumi et al.1) and Jeanneret et al.2) were the first to introduce this system in the lower cervical spine to treat subaxial fractures and dislocations. The pedicle screw system provided the most stiffness (fixation) for flexion, extension, torsion, and compression in the posterior column and for three-column instabilities.3,4) As compared to bicortical LM screw fixation, pedicle screws have 4 times the pull-out strength3,5) and thus have a lower risk of loosening during cyclic loading.6)
Although pedicle screws provide excellent biomechanical features, the insertion technique is perceived as technically demanding because of the narrow and large anatomical variations of the pedicle in the cervical spine.7–10) Furthermore, there is a limitation of this technique because of its complications—such as nerve root injury by misplaced screws, vertebral artery injury or obstruction by laterally-misplaced screws, and injury to the spinal cord or dural sac by medially-misplaced screws.7,11–14) Several techniques were introduced to improve the accuracy of screw placement and to reduce the rate of screw-related complications, which vary with (a) the identification of intra-operative topographic landmarks, (b) the lateral fluoroscopy guidance insertion technique, and (c) the use of modern computer navigation-assisted insertion.15–21)
A quantitative understanding of three-dimensional (3D) pedicle morphology is crucial for determining the most appropriate pedicle screw insertion point and pedicle screw axis.22–26) The details of cervical pedicle morphology have been reported. Some studies measured dry bone cadaveric specimens and some using computed tomography (CT) imaging. Most studies, notwithstanding the method, reported significant variability in the range of pedicle dimension data.27) A review by Liu et al.27) reported no statistically significant difference between the two measurement methods (i.e., direct measurement from dry cadaveric bone vs. measurements using CT imaging). Liu et al. also reported that sex, race, and geographical occurrence play a significant role in cervical pedicle anatomy. To wit, Asians trend to be smaller than Europeans and Americans vis-àvis the dimensions of pedicles. Moreover, females have smaller pedicles than males. There have been relatively few morphological studies done in Asian countries. One such study reported their subjects’ pedicle dimension were not large or sturdy enough for safe and feasible insertion of cervical pedicle screws.10)
In Thailand, there has been no study to date on subaxial cervical pedicle morphology. Thus, our objective was to perform a morphological study of the subaxial cervical pedicle from CT imaging in various crucial parameters to provide morphometric data for determination of safe and accurate placement of subaxial cervical pedicle screws. In order to improve the accuracy in measurement, we decided to use Mimics® 10.01 software (Materialise, Leuven, Belgium) to generate a 3D reconstruction image of the CT scan data. Lu et al.28) likewise used Mimics® 10.01 software to generate a 3D reconstruction image to produce a virtual navigational template for cervical pedicle screw insertion. These results led us to use this software to measure the cervical pedicle morphology for this study.
Materials and Methods
CT scans (from 15 males and 15 females) with normal cervical spines were included in this study. Age ranged between 22 years and 60 years (three 20–30-year-olds, seven 30–40-year-olds, five 40–50-year-olds, fifteen 50–60-year-olds). Height ranged between 146 and 176 cm. Mean body mass index (BMI) was 22.28 among males and 22.85 among females. All cervical spines were good in bone macroarchitecture in 3D CT reconstruction images. The subjects with cervical spine trauma, infection, tumor, inflammatory diseases, deformity, or congenital abnormalities were excluded. The study was reviewed then approved by our institutional ethics committee.
The data for cervical spine CT scans (Brilliance iCT SP-128; Philips, Andover, Massachusetts, USA) were obtained in DICOM format file and transferred to Mimics® 10.01 software for generation of a 3D reconstruction model of C3–C7 vertebrae. Each cervical vertebra was evaluated for pedicle morphologic parameters.
On the axial image, the parameters were measured as shown in Fig. 1. Pedicle axis length (PAL) was the distance from the posterior cortex of the pedicle axis projection on the LM to the anterior margin of the vertebral body. Pedicle length and lateral mass (PL-LM) was the distance from the posterior cortex of the pedicle axis projection on the LM to the junction of the vertebral body and pedicle. Pedicle length (PL) was the distance between the vertebral body-pedicle junction and the LM. Outer pedicle width (OPW) was the outermost medial-lateral diameter of the pedicle isthmus (narrowest point). Pedicle transverse angle (PTA) was the angle between the pedicle axis projection and the vertebral midline.
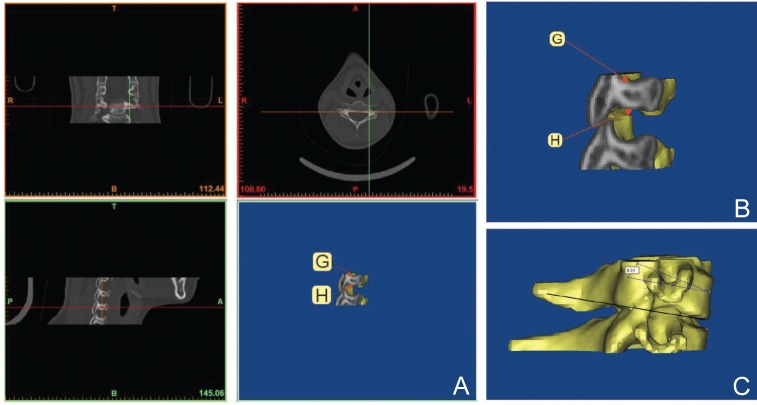
Fig. 1.
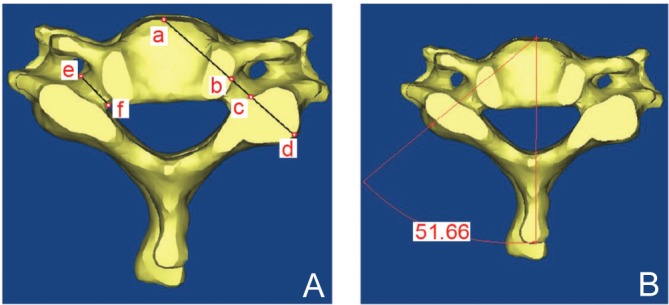
A: Showing pedicle morphological parameters measurement in axial three-dimensional image reconstructed from computed tomography (CT) imaging by Mimics® 10.01 software (Materialise, Leuven, Belgium). The line from E to F is the outer pedicle width, A to D the pedicle axis length, B to C the pedicle length, and B to D the pedicle length lateral mass. B: Demonstrating pedicle transverse angle measurement. a: anterior margin of the vertebral body in pedicle axis, b: junction between vertebral body and pedicle in pedicle axis, c: junction between pedicle and lateral mass in pedicle axis, d: posterior cortex of the pedicle axis, e: outermost lateral cortex of the pedicle isthmus, f: outermost medial cortex of the pedicle isthmus.
On the lateral image, the parameters were measured as shown in Fig. 2. Outer pedicle height (OPH) was the outermost supero-inferior diameter of the pedicle isthmus (narrowest point). Pedicle sagittal angle (PSA) was the angle between the pedicle axis line and the line parallel to inferior vertebral endplate. The value was recorded as positive if the pedicle axis angled cranially and negative if it angled caudally.
Fig. 2.
A: Showing outer pedicle height (OPH) determination and measurement. G–H distance is the OPH. B: Zooming in for OPH measurement. C: Demonstrating pedicle sagittal angle measurement by measuring the angle between the pedicle axis line and the line parallel to the inferior vertebral endplate. G: outermost superior cortex of the pedicle isthmus, H: outermost inferior cortex of the pedicle isthmus.
Two orthopedic surgeons (A and B with 4 and 8 years of experience, respectively) conducted the measurements independently. All parameters were determined a total of four times, that is, twice by both orthopedic surgeons A and B. The mean for each item was used as the data point. The intra-observer error was calculated from the first and second values determined by orthopedic surgeon A, and the inter-observer error from the values measured by both orthopedic surgeons A and B.
Statistical analysis
The mean and standard deviation were calculated for all parameters. The t test was used to determine if there were any significant differences (P < 0.05) in pedicle morphologic parameters according to sex, side, Asian population, and European/American population. SPSS® (SPSS Inc., Chicago, Illinois, USA) for Windows version 15.0 was used for the statistical analyses.
The intra- and inter-observer correlations were calculated using a two-way mixed effect model: the goal was to determine the intra-class correlation coefficients.
Results
We analyzed 150 3D reconstructions of subaxial cervical vertebrae from 30 subjects. Five linear and two angular parameters were measured for the 300 pedicles. The subjects’ demographic data are presented in Table 1.
Table 1.
Demographic data
| Males | Females | |
|---|---|---|
| Age (Mean ± SD) (years) | 47.8 ± 10.88 | 45.60 ± 12.05 |
| Height (Mean ± SD) (cm) | 163.73 ± 8.21 | 156 ± 6.58 |
| Weight (Mean ± SD) (kg) | 60.31 ± 9.39 | 55.05 ± 7.31 |
| BMI (Kg/m2) | 22.28 ± 2.32 | 22.85 ± 2.73 |
BMI: body mass index, SD: standard deviation.
The subaxial pedicle morphological data are presented in Table 2. Overall, the respective difference between the left and right side for each of the morphological parameters was not statistically significant. The exceptions were: (a) OPH at C4; (b) PL at C6; (c) PTA at C7; and (d) PSA at C5 (Tables 3 and 4). Females were significantly smaller than males for OPH (except C7), OPW (except C7 right side), and PAL (except C5 right side and C6 both sides) (Table 5). PL, there was a respective statistically significant difference between the sexes on both sides of C3 and C4 only. The PSA in females was significantly different than males on the right side of C5 and both sides of C4 and C6. Any difference in the PL-LM and PTA parameters was not statistically significant between the sexes.
Table 2.
The overall subaxial pedicle morphological data
| C3 | C4 | C5 | C6 | C7 | ||
|---|---|---|---|---|---|---|
| OPH |  |
6.37 ± 1.09 | 6.52 ± 0.88 | 6.96 ± 0.85 | 6.96 ± 0.84 | 7.47 ± 0.80 |
| OPW | 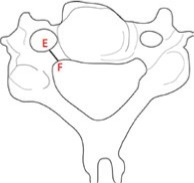 |
5.17 ± 0.79 | 5.46 ± 0.87 | 5.69 ± 0.69 | 5.89 ± 0.81 | 6.49 ± 0.73 |
| PAL | 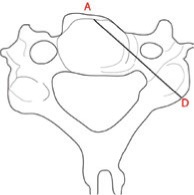 |
29.10 ± 2.49 | 30.48 ± 2.67 | 32.05 ± 2.39 | 33.40 ± 2.04 | 34.36 ± 1.75 |
| PL | 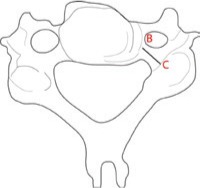 |
5.55 ± 0.76 | 5.76 ± 0.70 | 6.07 ± 0.70 | 6.13 ± 0.76 | 6.28 ± 0.79 |
| PL-LM | 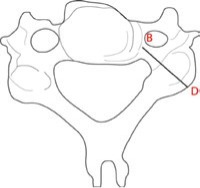 |
14.92 ± 1.43 | 14.84 ± 1.42 | 15.74 ± 1.85 | 15.76 ± 1.55 | 15.10 ± 1.60 |
| PSA | 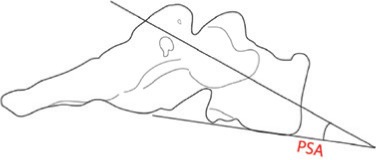 |
13.84° ± 1.46° | 7.09° ± 1.23° | 2.71° ± 1.17° | −4.55° ± 2.29° | −6.94° ± 1.28° |
| PTA | 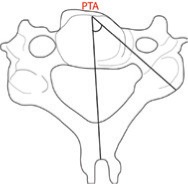 |
46.36° ± 3.03° | 48.5°2 ± 3.74° | 48.89° ± 2.93° | 44.30° ± 3.69° | 38.79° ± 4.64° |
Values are the mean and standard deviation. OPH: outer pedicle height, OPW: outer pedicle width, PAL: overall pedicle axis length, PL: pedicle length, PL-LM: pedicle length and lateral mass, PSA: pedicle sagittal angle of the subaxial cervical spines, PTA: pedicle transverse angle.
Table 3.
The difference between left and right side of the subaxial pedicles ( 1)
PAL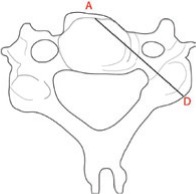
|
PL-LM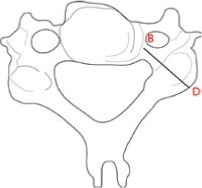
|
PL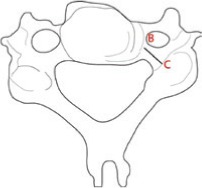
|
OPW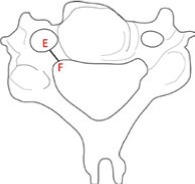
|
OPH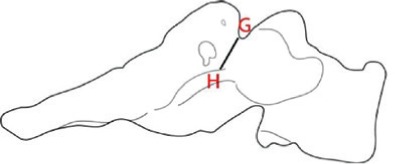
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left | Right | P value | Left | Right | P value | Left | Right | P value | Left | Right | P value | Left | Right | P value | |
| C3 | 29.28 ± 2.24 | 28.94 ± 3.00 | 0.3898 | 14.74 ± 1.35 | 15.11 ± 1.85 | 0.2818 | 5.49 ± 0.86 | 5.61 ± 0.75 | 0.2943 | 5.16 ± 0.84 | 5.19 ± 0.8 | 0.8157 | 6.27 ± 1.25 | 6.47 ± 0.98 | 0.0775 |
| C4 | 30.64 ± 2.58 | 30.33 ± 2.93 | 0.3232 | 14.78 ± 1.83 | 14.89 ± 1.47 | 0.7744 | 5.73 ± 0.72 | 5.77 ± 0.84 | 0.7685 | 5.45 ± 0.87 | 5.48 ± 0.92 | 0.7512 | 6.65 ± 0.9 | 6.39 ± 0.95 | 0.0444* |
| C5 | 32.4 ± 2.17 | 31.69 ± 3.09 | 0.2001 | 15.43 ± 1.96 | 16.06 ± 2.03 | 0.0802 | 5.97 ± 0.7 | 6.17 ± 0.82 | 0.1447 | 5.77 ± 0.73 | 5.61 ± 0.74 | 0.1557 | 6.98 ± 0.84 | 6.95 ± 0.94 | 0.8326 |
| C6 | 33.26 ± 1.91 | 33.55 ± 2.33 | 0.2939 | 15.47 ± 1.56 | 16.05 ± 1.86 | 0.0898 | 6.03 ± 0.76 | 6.24 ± 0.81 | 0.0133* | 5.95 ± 0.8 | 5.84 ± 0.85 | 0.2019 | 6.96 ± 0.93 | 6.98 ± 0.83 | 0.8614 |
| C7 | 34.57 ± 1.54 | 34.15 ± 2.14 | 0.1588 | 15.03 ± 1.72 | 15.17 ± 1.73 | 0.6286 | 6.23 ± 0.89 | 6.35 ± 0.80 | 0.3613 | 6.61 ± 0.83 | 6.38 ± 0.72 | 0.0551 | 7.49 ± 0.86 | 7.45 ± 0.85 | 0.7980 |
Values are the mean and standard deviation in mm.
Statistically significant (P < 0.05). OPH: outer pedicle height of the subaxial cervical spines vis-à-vis side, OPW: outer pedicle width, PAL : pedicle axis length, PL: pedicle length, PL-LM: pedicle length and lateral mass.
Table 4.
The difference between left and right side of the subaxial pedicles (2)
PTA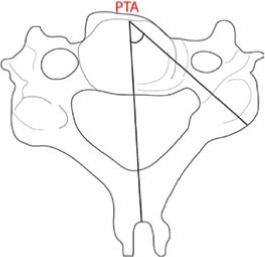
|
PSA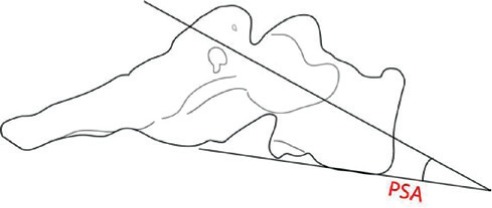
|
|||||
|---|---|---|---|---|---|---|
| Left | Right | P value | Left | Right | P value | |
| C3 | 46.13° ± 3.74° | 46.60° ± 3.11° | 0.5315 | 14.13° ± 1.67° | 13.56° ± 2.03° | 0.2814 |
| C4 | 48.16° ± 1.66° | 48.89° ± 3.85° | 0.4365 | 7.27° ± 1.56° | 6.92° ± 1.25° | 0.2647 |
| C5 | 49.29° ± 3.14° | 48.50° ± 3.51° | 0.2805 | 2.38° ± 1.19° | 3.04° ± 1.48° | 0.0364* |
| C6 | 43.93° ± 3.74° | 44.68° ± 4.20° | 0.2727 | −4.73° ± 2.72° | −4.37° ± 2.06° | 0.2862 |
| C7 | 37.98° ± 4.77° | 39.60° ± 4.78° | 0.0058* | −6.73° ± 1.36° | −7.16° ± 1.69° | 0.2736 |
Values are the mean and standard deviation in degrees.
Statistically significant (P < 0.05). PSA: pedicle sagittal angle of the subaxial cervical spines vis-à-vis side, PTA: pedicle transverse angle.
Table 5.
The difference between sex of the subaxial pedicles
| C3 | C4 | C5 | C6 | C7 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | P value | Male | Female | P value | Male | Female | P value | Male | Female | P value | Male | Female | P value | |
| OPH-Lt | 7.28 ± 0.80 | 5.26 ± 0.61 | < 0.0001* | 7.12 ± 0.74 | 6.19 ± 0.82 | 0.0162* | 7.43 ± 0.76 | 6.52 ± 0.68 | 0.0108* | 7.35 ± 0.91 | 6.57 ± 0.80 | 0.0575 | 7.78 ± 0.97 | 7.19 ± 0.63 | 0.1281 |
| OPH-Rt | 7.35 ± 0.41 | 5.60 ± 0.42 | < 0.0001* | 6.93 ± 0.88 | 5.85 ± 0.68 | 0.0066* | 7.57 ± 0.82 | 6.33 ± 0.58 | 0.0010* | 7.42 ± 0.77 | 6.53 ± 0.66 | 0.0129* | 7.77 ± 0.68 | 7.13 ± 0.91 | 0.0936 |
| OPW-Lt | 5.77 ± 0.35 | 4.55 ± 0.75 | 0.0002* | 6.05 ± 0.75 | 4.86 ± 0.55 | 0.0007* | 6.33 ± 0.55 | 5.21 ± 0.32 | < 0.0001* | 6.52 ± 0.39 | 5.37 ± 0.71 | 0.0003* | 7.07 ± 0.60 | 6.15 ± 0.79 | 0.0099* |
| OPW-Rt | 5.71 ± 0.33 | 4.66 ± 0.80 | 0.0013* | 5.93 ± 0.80 | 5.03 ± 0.82 | 0.0232* | 6.14 ± 0.60 | 5.08 ± 0.43 | 0.0003* | 6.43 ± 0.56 | 5.24 ± 0.63 | 0.0003* | 6.57 ± 0.72 | 6.18 ± 0.70 | 0.2311 |
| PAL-Lt | 30.58 ± 1.37 | 27.98 ± 2.23 | 0.0059* | 32.09 ± 1.85 | 29.19 ± 2.44 | 0.0079* | 33.73 ± 1.45 | 31.08 ± 1.99 | 0.0032* | 33.97 ± 2.16 | 32.55 ± 1.39 | 0.0974 | 35.47 ± 1.65 | 33.66 ± 0.66 | 0.0048* |
| PAL-Rt | 30.84 ± 1.58 | 27.03 ± 2.89 | 0.0019* | 31.92 ± 1.94 | 28.74 ± 2.96 | 0.0109* | 32.73 ± 3.26 | 30.66 ± 2.68 | 0.1374 | 34.46 ± 2.70 | 32.64 ± 1.50 | 0.0811 | 35.40 ± 2.06 | 32.89 ± 1.39 | 0.0052* |
| PL-Lt | 6.09 ± 0.61 | 4.88 ± 0.61 | 0.0003* | 6.16 ± 0.36 | 5.31 ± 0.75 | 0.0051* | 6.01 ± 0.86 | 5.93 ± 0.54 | 0.7754 | 6.14 ± 0.93 | 5.91 ± 0.56 | 0.5057 | 6.21 ± 0.66 | 6.24 ± 1.09 | 0.9536 |
| PL-Rt | 6.06 ± 0.54 | 5.17 ± 0.68 | 0.0045* | 6.36 ± 0.53 | 5.19 ± 0.68 | 0.0004* | 6.28 ± 0.80 | 6.07 ± 0.86 | 0.5712 | 6.32 ± 0.91 | 6.16 ± 0.73 | 0.6795 | 6.38 ± 0.6 | 6.32 ± 0.99 | 0.8681 |
| PL-LM-Lt | 15.21 ± 1.22 | 14.28 ± 1.37 | 0.1297 | 15.11 ± 2.13 | 14.45 ± 1.52 | 0.4333 | 15.46 ± 2.19 | 15.40 ± 1.82 | 0.9435 | 15.59 ± 1.69 | 15.34 ± 1.49 | 0.7316 | 15.29 ± 1.32 | 14.76 ± 2.09 | 0.5043 |
| PL-LM-Rt | 15.53 ± 1.78 | 14.69 ± 1.92 | 0.3235 | 15.30 ± 1.26 | 14.48 ± 1.61 | 0.2147 | 16.11 ± 2.05 | 16.0 ± 2.12 | 0.9101 | 16.76 ± 1.72 | 15.35 ± 1.80 | 0.0906 | 15.55 ± 1.68 | 14.79 ± 1.77 | 0.3373 |
| PSA-Lt | 14.09° ± 1.76° | 14.17° ± 1.66° | 0.9118 | 8.30° ± 0.83° | 6.24° ± 1.46° | 0.0011* | 2.88° ± 1.51° | 1.87° ± 0.33° | 0.0528 | −2.94° ± 1.86° | −6.53° ± 2.22° | 0.001* | −6.97° ± 1.19° | −6.49° ± 1.54° | 0.4397 |
| PSA-Rt | 14.43° ± 2.15° | 12.69° ± 1.54° | 0.0532 | 7.58° ± 1.24° | 6.25° ± 0.88° | 0.0130* | 3.96° ± 1.54° | 2.11° ± 0.56° | 0.0023* | −2.90° ± 1.24° | −5.83° ± 1.65° | 0.0003* | −6.87° ± 1.81° | −7.45° ± 1.60° | 0.4657 |
| PTA-Lt | 46.43° ± 3.72° | 45.83° ± 3.92° | 0.7273 | 49.35° ± 4.40° | 46.96° ± 4.84° | 0.2640 | 49.39° ± 3.69° | 49.18° ± 2.68° | 0.8850 | 44.14° ± 4.14° | 43.71° ± 3.51° | 0.8042 | 38.16° ± 5.61° | 37.79° ± 4.07° | 0.8693 |
| PTA-Rt | 47.11° ± 3.45° | 46.07° ± 2.81° | 0.4694 | 49.62° ± 2.46° | 48.16° ± 4.90° | 0.4103 | 48.57° ± 4.35° | 48.43° ± 2.65° | 0.9289 | 45.12° ± 5.19° | 44.23° ± 3.14° | 0.6468 | 39.90 ± 5.74° | 39.29 ± 3.88° | 0.7861 |
Values are the mean and standard deviation.
Statistical significant (P < 0.05). Lt: left, OPH: outer pedicle height, OPW: outer pedicle width, PAL : pedicle axis length, PL: pedicle length, PL-LM: pedicle length and lateral mass, PSA: pedicle sagittal angle of the subaxial cervical spines vis-à-vis sex, PTA: pedicle transverse angle, Rt: right.
The respective ICC and 95% confidence interval for inter- and intra-observer reproducibility was very good for all of the measured radiographic parameters (Table 6).
Table 6.
Inter- and intra-observer reproducibility using intra-class correlation coefficients in a two-way mixed effect model
| Measurement parameter | ICC | |||
|---|---|---|---|---|
| Inter-observer | 95% CI | Intra-observer | 95% CI | |
| PAL | 0.95 | 0.93–0.97 | 0.95 | 0.93–0.96 |
| PL-LM | 0.90 | 0.83–0.93 | 0.89 | 0.86–0.92 |
| PL | 0.89 | 0.84–0.93 | 0.94 | 0.92–0.95 |
| OPW | 0.94 | 0.91–0.96 | 0.94 | 0.93–096 |
| OPH | 0.89 | 0.83–0.92 | 0.95 | 0.93–0.96 |
| PTA | 0.94 | 0.91–0.96 | 0.95 | 0.94–0.97 |
| PSA | 0.89 | 0.83–0.93 | 0.97 | 0.96–0.98 |
CI: confidence interval, IC: intra-class correlation coefficient, OPH: outer pedicle height, OPW: outer pedicle width, PAL : pedicle axis length, PL: pedicle length, PL-LM: pedicle length and lateral mass, PSA: pedicle sagittal angle, PTA: pedicle transverse angle.
The difference in male vs. female PAL (range, 24.7 to 37.95 mm) was highly significant (males were longer than women), except on the right side of C5 and both sides of C6. The mean PAL at each level gradually increased from C3 to C7 (29.10 to 34.36 mm).
PL-LM (range, 11.79 to 19.56 mm) was not significantly dependent on either sex or side. The mean was shortest at C4 (14.84 mm) and longest at C6 (15.76 mm). The mean length for males was greater than for females.
At C3 and C4, PL (range, 3.68 to 17.94 mm) was significantly dependent on sex (males longer than females). At C5 to C7, however, length was not significantly different between the sexes. Vis-à-vis right and left side, length was significantly side dependent only at C6. The mean of the length at each level gradually increased from C3 to C7 (5.55 to 6.28 mm).
The mean OPW (range, 3.64 to 7.46 mm) at each level gradually increased from C3 to C7 (5.17 to 6.49 mm). Pedicle width in males was significantly greater than in females, at all spinal levels except at the C7 spinal level on the right side. The difference between sides vis-à-vis outer pedicle width was not statistically significant.
The OPH (range, 4.18 to 6.17 mm) between the sexes nearly reached statistical significance (males trended to be larger than females) except at C6 on the left side and C7 on both sides. Vis-à-vis side, only the C4 spinal level had a statistically significant difference between left and right (left was greater than right). The mean height at each level increased from C3 to C7 (6.37 to 7.47 mm).
The mean PTA (range, 30.86° at C6 to 55.59° at C5) gradually increased from C3 to C5 (46.36° to 48.89°) then gradually decreased from C5 to C7 (48.89° to 38.79°). The mean was largest at the C5 spinal level and smallest at the C7 spinal level. A respective 67.5%, 80%, 85%, 37.5%, and 22.5% of all pedicles at C3, C4, C5, C6, and C7 had a transverse angle > 45°. There was no statistically significant difference in PTA between the sexes. Moreover, only the C7 spinal level had a statistically significant difference between the right and left side angle.
The range of the PSA (–10.92° to 18.86°) was significantly different between the sexes on both sides of C4 and C6, and on the right side of C5. The pedicle was oriented cranially at C3 (13.84°); the degree of which gradually decreased to C5 (2.71°). The pedicle was then oriented caudally at C6 (–4.55°) and C7 (–6.94°). Females had a more caudal trajectory of the pedicle than males; at almost all pedicles from C3 to C7. Only at the C5 spinal level was there any statistically significant difference between sides.
Discussion
Transpedicular screw fixation at the subaxial cervical spine is considered an alternative fixation for use in posterior cervical spine surgery, especially for posterior salvage surgery of the cervical spine. This system provides superior biomechanical strength compared to other posterior cervical fixation systems.3–5) This system, however, also has potential complications, such as nerve root injury, vertebral artery injury, and dural sac injury, that account for this system's being infrequently used. Morphologic studies on subaxial cervical pedicles—whether direct or CT measurement—are crucial for avoiding complications during surgeries implementing this system. There are not, however, many indexing studies on the cervical pedicle morphology of Asians over against those on Europeans or North Americans. This study was conducted to understand the morphology of subaxial cervical pedicles in various parameters in the Thai population and to understand the difference between our population and other populations in Asia, Europe, and America.
We found that the difference between males and females for almost all parameters of subaxial pedicle morphology were statistically significant. To reduce pedicle screw complications, it is therefore necessary for surgeons to be aware of these differences during pre-operative planning. The current study also showed that the pedicle height and width of subaxial cervical spines were suitable for insertion of 3.5 mm pedicle screws. Vis-à-vis angles, the PSA is directed cranially from C3 to C5 then caudally at C6 and C7. The PTA was greatest at C5 and smallest at C7.
Comparing our data (at all subaxial cervical spinal levels) with other Asian CT measurement studies8,10,25–29) (Table 7), differences in mean OPW, OPH, and PL-LM were not statistically significant (P > 0.05). Mean PAL at C4 to C7 in our population was significantly greater than in other Asian populations. Vis-à-vis the PSA, it was significantly different (albeit not exceeding 2°) at C3, C4, C6, and C7. The PTA, at the C3 and C4 spinal levels were significantly different but not exceeding 3° at each spinal level. The relative similarities to other Asian populations strongly suggests that the cervical pedicle screw can be performed in nearly the same way as it is done elsewhere in Asia.
Table 7.
Comparison of mean subaxial cervical pedicle morphological parameters between the present study and Asian, European, and American data
| This study | Asian | This study vs. Asian (P value) | European/American | This study vs. European (P value) | ||
|---|---|---|---|---|---|---|
| C3 | OPH | 6.37 | 6.70 | 0.1954 | 6.89 | 0.0479* |
| OPW | 5.17 | 5.26 | 0.6364 | 5.17 | 0.9801 | |
| PAL | 29.10 | 29.17 | 0.9110 | 33.34 | < 0.0001* | |
| PL | 5.55 | N/A | N/A | 5.25 | 0.0936 | |
| PL-LM | 14.92 | 15.48 | 0.1033 | N/A | N/A | |
| PSA | 13.84° | 13.10 | 0.0344* | 14.17 | 0.3309 | |
| PTA | 46.36° | 48.41 | 0.0070* | 47.06 | 0.3152 | |
| C4 | OPH | 6.52 | 6.78 | 0.2086 | 6.96 | 0.0392* |
| OPW | 5.46 | 5.468 | 0.4902 | 5.31 | 0.4304 | |
| PAL | 30.48 | 28.90 | 0.0159* | 32.81 | 0.0010* | |
| PL | 5.76 | N/A | N/A | 5.20 | 0.0038* | |
| PL-LM | 14.84 | 14.73 | 0.7421 | N/A | N/A | |
| PSA | 7.09° | 8.10 | 0.0017* | 7.46 | 0.2016 | |
| PTA | 48.52° | 50.58 | 0.0240* | 48.78 | 0.7633 | |
| C5 | OPH | 6.96 | 6.95 | 0.9436 | 6.74 | 0.2579 |
| OPW | 5.69 | 5.68 | 0.9416 | 5.66 | 0.8410 | |
| PAL | 32.05 | 30.82 | 0.0331* | 33.79 | 0.0042* | |
| PL | 6.07 | N/A | N/A | 5.60 | 0.0073* | |
| PL-LM | 15.74 | 15.48 | 0.5295 | N/A | N/A | |
| PSA | 2.71° | 2.90 | 0.4756 | −0.38 | < 0.0001 | |
| PTA | 48.89° | 48.95 | 0.9329 | 48.35 | 0.4176 | |
| C6 | OPH | 6.96 | 7.25 | 0.1526 | 6.71 | 0.1895 |
| OPW | 5.89 | 5.91 | 0.9151 | 5.99 | 0.5880 | |
| PAL | 33.40 | 31.67 | 0.0012* | 34.23 | 0.0859 | |
| PL | 6.13 | N/A | N/A | 5.80 | 0.0677 | |
| PL-LM | 15.76 | 15.50 | 0.4593 | N/A | N/A | |
| PSA | −4.55° | −4.10 | 0.4708 | −3.27 | 0.0023* | |
| PTA | 44.30° | 44.94 | 0.4507 | 44.24 | 0.9388 | |
| C7 | OPH | 7.47 | 7.63 | 0.3900 | 6.93 | 0.0071* |
| OPW | 6.49 | 6.63 | 0.4253 | 6.64 | 0.3923 | |
| PAL | 34.36 | 31.87 | < 0.0001* | 32.30 | < 0.0001* | |
| PL | 6.28 | N/A | N/A | 5.70 | 0.0039* | |
| PL-LM | 15.10 | 15.78 | 0.2296 | N/A | N/A | |
| PSA | −6.94° | −5.75 | 0.0010* | −1.89 | < 0.0001* | |
| PTA | 38.79° | 37.05 | 0.1096 | 38.68 | 0.9166 | |
Statistically significant (P < 0.05).
N/A: not available, OPH: outer pedicle height, OPW: outer pedicle width, PAL : pedicle axis length, PL: pedicle length, PL-LM: pedicle length and lateral mass, PSA: pedicle sagittal angle, PTA: pedicle transverse angle.
Compared to European/American CT measurement studies,5,24,27,29–37) the respective C3 and C4 OPH in the current study was significantly smaller. By contrast, the C7 in our population was significantly taller. At all levels, differences in OPW were not statistically significant. PAL was significantly different at all levels except C6. The PL was significantly greater at C4, C5, and C7 than was found among Europeans and Americans. The PTA at all levels showed no significant difference, while the PSA was significantly different at C5 to C7; especially at C5, as our population's angle was directed cranially while the angle in European/American populations was directed caudally. Regarding C6 and C7, the respective sagittal angle in our population was directed more caudally than in Europeans and Americans. These results underscore that the use of European/American data for planning subaxial pedicle screw insertion in Asians could be risky, especially at the C5 level. Race specific data is needed.
The limitations of this study are: (1) our included subjects trended to be aged and old-age subjects might have some degree of degenerative process at the subaxial cervical spines; (2) some anatomical relationships may have changed when the position of the patient's head and neck was changed during intra-operative positioning; and (3) our data especially for screws insertion trajectory might be affected by points 1 and 2.
Conclusion
Better knowledge of the subaxial pedicle morphologies is the key to safe and successful insertion of 3.5 mm diameter screws in transpedicular screw fixation. According to the differences found between the sexes and sides of the cervical pedicle parameters, a pre-operative imaging study should be performed to know the orientation and size of the cervical pedicle. Armed with such knowledge, the surgeon uses (a) a virtual navigation template, (b) an intraoperative navigation system, or (c) an intraoperative imaging system to perform the transpedicular screw fixation in subaxial cervical spine surgery.
Acknowledgments
This study was granted by Faculty of Medicine, Khon Kaen University, Thailand (Grant number I 54115). The authors thank the patients for the participation, the Department of Orthopaedics and the Faculty of Medicine for support, and Mr. Bryan Roderick Hamman and Mrs. Janice Loewen-Hamman for assistance with the English-language presentation of the manuscript.
References
- 1). Abumi K, Itoh H, Taneichi H, Kaneda K: Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 7: 19– 28, 1994. [DOI] [PubMed] [Google Scholar]
- 2). Jeanneret B, Gebhard JS, Magerl F: Transpedicular screw fixation of articular mass fracture-separation: results of an anatomical study and operative technique. J Spinal Disord 7: 222– 229, 1994. [DOI] [PubMed] [Google Scholar]
- 3). Ito Z, Higashino K, Kato S, Kim SS, Wong E, Yoshioka K, Hutton WC: Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: a biomechanical study on strength of fixation. J Spinal Disord Tech 27: 80– 85, 2014. [DOI] [PubMed] [Google Scholar]
- 4). Kotani Y, Cunningham BW, Abumi K, McAfee PC: Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine (Phila Pa 1976) 19: 2529– 2539, 1994. [DOI] [PubMed] [Google Scholar]
- 5). Jones EL, Heller JG, Silcox DH, Hutton WC: Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 22: 977– 982, 1997. [DOI] [PubMed] [Google Scholar]
- 6). Kothe R, Rüther W, Schneider E, Linke B: Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976) 29: 1869– 1875, 2004. [DOI] [PubMed] [Google Scholar]
- 7). Abumi K, Ito M, Sudo H: Reconstruction of the subaxial cervical spine using pedicle screw instrumentation. Spine (Phila Pa 1976) 37: E349– E356, 2012. [DOI] [PubMed] [Google Scholar]
- 8). Chazono M, Soshi S, Inoue T, Kida Y, Ushiku C: Anatomical considerations for cervical pedicle screw insertion: the use of multiplanar computerized tomography reconstruction measurements. J Neurosurg Spine 4: 472– 477, 2006. [DOI] [PubMed] [Google Scholar]
- 9). Shin EK, Panjabi MM, Chen NC, Wang JL: The anatomic variability of human cervical pedicles: considerations for transpedicular screw fixation in the middle and lower cervical spine. Eur Spine J 9: 61– 66, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Yusof MI, Ming LK, Abdullah MS, Yusof AH: Computerized tomographic measurement of the cervical pedicles diameter in a Malaysian population and the feasibility for transpedicular fixation. Spine (Phila Pa 1976) 31: E221– E224, 2006. [DOI] [PubMed] [Google Scholar]
- 11). Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K: Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 25: 962– 969, 2000. [DOI] [PubMed] [Google Scholar]
- 12). Kast E, Mohr K, Richter HP, Börm W: Complications of transpedicular screw fixation in the cervical spine. Eur Spine J 15: 327– 334, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Neo M, Sakamoto T, Fujibayashi S, Nakamura T: The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine (Phila Pa 1976) 30: 2800– 2805, 2005. [DOI] [PubMed] [Google Scholar]
- 14). Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T: Spinal reconstruction using a cervical pedicle screw system. Clin Orthop Relat Res 111– 119, 2005. [DOI] [PubMed] [Google Scholar]
- 15). Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S: Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine 13: 606– 611, 2010. [DOI] [PubMed] [Google Scholar]
- 16). Ito Y, Sugimoto Y, Tomioka M, Hasegawa Y, Nakago K, Yagata Y: Clinical accuracy of 3D fluoroscopy-assisted cervical pedicle screw insertion. J Neurosurg Spine 9: 450– 453, 2008. [DOI] [PubMed] [Google Scholar]
- 17). Ludwig SC, Kowalski JM, Edwards CC, Heller JG: Cervical pedicle screws: comparative accuracy of two insertion techniques. Spine (Phila Pa 1976) 25: 2675– 2681, 2000. [DOI] [PubMed] [Google Scholar]
- 18). Lu S, Xu YQ, Lu WW, Ni GX, Li YB, Shi JH, Li DP, Chen GP, Chen YB, Zhang YZ: A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila Pa 1976) 34: E959– E966, 2009. [DOI] [PubMed] [Google Scholar]
- 19). Miyamoto H, Uno K: Cervical pedicle screw insertion using a computed tomography cutout technique. J Neurosurg Spine 11: 681– 687, 2009. [DOI] [PubMed] [Google Scholar]
- 20). Rajasekaran S, Kanna PR, Shetty TA: Intra-operative computer navigation guided cervical pedicle screw insertion in thirty three complex cervical spine deformities. J Craniovertebr Junction Spine 1: 38– 43, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Richter M, Cakir B, Schmidt R: Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa 1976) 30: 2280– 2287, 2005. [DOI] [PubMed] [Google Scholar]
- 22). Kosmopoulos V, Schizas C: Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 32: E111– E120, 2007. [DOI] [PubMed] [Google Scholar]
- 23). Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ: Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res 77– 88, 1999. [DOI] [PubMed] [Google Scholar]
- 24). Rao RD, Marawar SV, Stemper BD, Yoganandan N, Shender BS: Computerized tomographic morpho-metric analysis of subaxial cervical spine pedicles in young asymptomatic volunteers. J Bone Joint Surg Am 90: 1914– 1921, 2008. [DOI] [PubMed] [Google Scholar]
- 25). Ruofu Z, Huilin Y, Xiaoyun H, Xishun H, Tiansi T, Liang C, Xigong L: CT evaluation of cervical pedicle in a Chinese population for surgical application of transpedicular screw placement. Surg Radiol Anat 30: 389– 396, 2008. [DOI] [PubMed] [Google Scholar]
- 26). Su P, Ma R, Li C, Liu S, Huang D: Pedicle screw fixation of the cervical spine: guidance by computed tomography. Clin Orthop Relat Res 462: 99– 104, 2007. [DOI] [PubMed] [Google Scholar]
- 27). Liu J, Napolitano JT, Ebraheim NA: Systematic review of cervical pedicle dimensions and projections. Spine (Phila Pa 1976) 35: E1373– E1380, 2010. [DOI] [PubMed] [Google Scholar]
- 28). Lu S, Xu YQ, Chen GP, Zhang YZ, Lu D, Chen YB, Shi JH, Xu XM: Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg 16: 240– 248, 2011. [DOI] [PubMed] [Google Scholar]
- 29). Sakamoto T, Neo M, Nakamura T: Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine (Phila Pa 1976) 29: 2510– 2514; discussion 2515; 2004. [DOI] [PubMed] [Google Scholar]
- 30). Barrey C, Cotton F, Jund J, Mertens P, Perrin G: Transpedicular screwing of the seventh cervical vertebra: anatomical considerations and surgical technique. Surg Radiol Anat 25: 354– 360, 2003. [DOI] [PubMed] [Google Scholar]
- 31). Howington JU, Kruse JJ, Awasti D: Surgical anatomy of the C-2 pedicle. J Neurosurg 95( Suppl 1): 88– 92, 2001. [DOI] [PubMed] [Google Scholar]
- 32). Karaikovic EE, Daubs MD, Madsen RW, Gaines RW: Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976) 22: 493– 500, 1997. [DOI] [PubMed] [Google Scholar]
- 33). Nogueira-Barbosa MH, Defino HL: Multiplanar reconstructions of helical computed tomography in planning of atlanto-axial transarticular fixation. Eur Spine J 14: 493– 500, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34). Reinhold M, Magerl F, Rieger M, Blauth M: Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morpho-metric data. Eur Spine J 16: 47– 56, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35). Rezcallah AT, Xu R, Ebraheim NA, Jackson T: Axial computed tomography of the pedicle in the lower cervical spine. Am J Orthop 30: 59– 61, 2001. [PubMed] [Google Scholar]
- 36). Bozbuga M, Ozturk A, Ari Z, Sahinoglu K, Bayraktar B, Cecen A: Morphometric evaluation of subaxial cervical vertebrae for surgical application of transpedicular screw fixation. Spine (Phila Pa 1976) 29: 1876– 1880, 2004. [DOI] [PubMed] [Google Scholar]
- 37). Koller H, Hempfing A, Acosta F, Fox M, Scheiter A, Tauber M, Holz U, Resch H, Hitzl W: Cervical anterior transpedicular screw fixation. Part I: Study on morphological feasibility, indications, and technical prerequisites. Eur Spine J 17: 523– 538, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]