Abstract
The intralaminar screw construct has been recently introduced in C6–C7 fixation. The aim of the study is to compare the stability afforded by three different C7 posterior fixation techniques using a three-dimensional finite element model of a C6–C7 cervical spine motion segment. Finite element models representing three different cervical anchor types (C7 intralaminar screw, C7 lateral mass screw, and C7 pedicle screw) were developed. Range of motion (ROM) and maximum von Mises stresses in the vertebra for the three screw techniques were compared under pure moments in flexion, extension, lateral bending, and axial rotation. ROM for pedicle screw construct was less than the lateral mass screw construct and intralaminar screw construct in the three principal directions. The maximum von Misses stress was observed in the C7 vertebra around the pedicle in all the three screw constructs. Maximum von Mises stress in pedicle screw construct was less than the lateral mass screw construct and intralaminar screw construct in all loading modes. This study demonstrated that the pedicle screw fixation is the strongest instrumentation method for C6–C7 fixation. Pedicle screw fixation resulted in least stresses around the C7 pedicle-vertebral body complex. However, if pedicle fixation is not favorable, the laminar screw can be a better option compared to the lateral mass screw because the stress around the pedicle-vertebral body complex and ROM predicted for laminar screw construct was smaller than those of lateral mass screw construct.
Keywords: cervical spine, pedicle screw, laminar screw, lateral mass screw, finite element method, biomechanics
Introduction
Posterior cervical screw instrumentation has been broadly used for cervical spine instability and spinal deformity in place of posterior wiring because it has been reported to induce higher fusion rates and obviates the need for rigid external mobilization.1,2) Although lateral mass screws are relatively safe and easy constructs to insert, lateral mass screw fixation at C7 can be problematic.3,4) Screw loosening or avulsion has been documented as a failure mechanism for lateral mass screws, particularly in the lower cervical spine where decreasing size of the lateral mass results in a decreased amount of the minimal pullout strength required.5,6)
Screw fixation into the cervical pedicle has been proposed as an alternative to overcome these limitations.7,8) Pedicle screw fixation is known to be the most biomechanically stable when performed through a posterior-only approach.7) However, their use in the cervical spine region can be technically difficult and potentially dangerous, as the cervical pedicle is small and is immediately surrounded by delicate structures: laterally by the vertebral artery (VA), medially by the spinal cord, and vertically by adjacent nerve roots.9,10) Anatomic variations in pedicle trajectory and morphology make pedicle screw placement using standard bony landmarks potentially dangerous.11,12) The shoulder girdle can hinder the use of conventional fluoroscopy for patients with short necks or who are obese and image quality can be suboptimal, especially in obese or osteopenic patients.13–15) Moreover, as up to 5% of patients have a VA in the C7 transverse foramen (TF), pedicle fixation at this level is anatomically dangerous.16,17) Thus, some authors recommend using a navigation system or laminoforaminotomy technique to aid in cervical pedicle screw placement.18,19) However, even under direct visualization in a cadaveric study or in experienced surgical hands, pedicle breaches have been reported up to 23% of the time.20,21) Computer-assisted navigation systems are also inconvenient as they increase surgical time in the operating room.18,22)
Due to these issues with C7 pedicle screw fixation and the potential for high biomechanical demands during posterior cervicothoracic fixation, we sought alternative methods of posterior instrumentation that could not only provide the required support but also avoid the potential risks seen with the use of cervical pedicle screws. Recently, intralaminar screws have been used as a potentially safer alternative to traditional fusion constructs involving fixation of C2 and the cervicothoracic junction.23–25) The intralaminar screw method is useful for avoiding vascular injuries, especially when the VA tracks in the C7 TF. Also, it maintains a high degree of stability in the subaxial cervical spine.14,26,27) This technique has two key advantages over the currently used surgical options: first, it is simpler and does not require the use of any navigational instruments, and second, it is not limited by the position of known vascular structures.25) Therefore, the potential patient population that could benefit from this procedure is large. However, to date, biomechanical comparisons of the C7 intralaminar screw technique with lateral mass screw or pedicle screw technique was rather scanty.14,26) Moreover biomechanical study using cadaveric specimen could be suboptimal to evaluate several different operative scenario due to the destructive nature of surgery and it is not possible to directly measure internal responses such as stress and strain in cadaveric model even though cadaveric model has quantified the external angular rotation biomechanical response to wide variety of external loading.
Computational models provide an ideal method for the study of biomechanics following surgical intervention. Once a model has been developed and validated, a test can be repeated ad infinitum with alteration of only a single variable, allowing for the application of the scientific method to the study of the biomechanics of surgical interventions. A finite element model (FEM) of cervical spine was employed to investigate the biomechanical characteristics of three different posterior fixation techniques. With this method, we investigated the biomechanical results on the FEM and the cadaver model and the internal responses of C7 vertebrae as well in each different C7 screw construct to compare posterior cervical construct stability afforded by this novel C7 intralaminar screw technique with that of the more commonly used lateral mass technique and transpedicular screw fixation method.
Materials and Methods
A previously validated three-dimensional (3D) poro-elastic finite element model of an intact C6–C7 cervical spine segment was employed for this study. Detailed modeling and validation information has already been published and a brief description follows.28) The model was developed using serial axial computed tomography (CT) scans of a 38-year-old normal female subject. The CT scan was imported into the 3D medical imaging software, Mimics (Materialise N.V., Ann Arbor, Michigan, USA). The vertebral surface models were translated into solid models using another computer aided design software, Pro/Engineer (Parametric Technology Corporation, Needham, Massachusetts, USA). The vertebral solid models were then meshed in the FE software, ADINA (ADINA R & D Inc., Watertown, Massachusetts, USA) for the simulation. The disc was modeled with an elliptical shape by connecting the surfaces of inferior C6 endplate and superior C7 endplate. The anterior and posterior disc heights agreed with the anthropometric literature values.29) The major and minor diameters of the elliptical disc and NP were taken from the literature, and the NP was positioned in the center of the disc.30–33) The vertebrae, endplates, and the intervertebral disc were modeled as 3D solid element with free-form meshing. The facets were modeled as 3D solid moving contact surface element with free-form meshing between the superior and the inferior surfaces. Five ligaments: anterior longitudinal ligament, posterior longitudinal ligament, interspinous ligament, ligamentum flavum, and capsular ligaments were modeled. Ligament insertion points and area were closely matched with published data.34,35) The cortical bone, cancellous bone, posterior elements, endplates, annulus fibrosus, nucleus pulposus, and articular facets were assumed to be linear elastic, homogeneous, and isotropic. The five spinal ligaments were assumed to be non-linear elastic. Material properties for different structures of the motion segment were adopted from the literature (Table 1).36–40)
Table 1.
Material properties of the spinal components
| Description | Young's modulus, E, (MPa) | Poisson's ratio | Density, ρ, (1.00E–06 kg/mm3) |
|---|---|---|---|
| Cortical bone | 10000.00 | 0.29 | 1.83 |
| Cancellous bone | 100.00 | 0.29 | 1.00 |
| Posterior elements | 3500.00 | 0.29 | 1.83 |
| Endplate | 5.00 | 0.40 | 1.83 |
| Annulus fibrosus | 2.50 | 0.40 | 1.20 |
| Nucleus pulposus | 1.50 | 0.49 | 1.36 |
| Facets | 10.40 | 0.40 | 1.83 |
| Anterior longitudinal Ligament | 15 (ε < 12%) 30 (ε > 12%) |
– | – |
| Posterior longitudinal ligament | 10 (ε < 12%) 20 (ε > 12%) |
– | – |
| Interspinous ligament | 2 (ε < 40%) 8 (ε > 40%) |
– | – |
| Ligamentum flavum | 5 (ε < 25%) 10 (ε >25%) |
– | – |
| Capsular ligaments | 7 (ε < 12%) 30 (ε > 12%) |
– | – |
Three additional models were created by modifying the intact model to simulate three different types of C7 posterior screw fixation methods: lateral mass screw, intralaminar screw, and pedicle screw in C6–C7 segment. A 3.5φ × 14 mm screw was simulated to insert into the lateral mass of C6 vertebra. For C7 instrumentation, 3.5φ × 24 mm length screw was used for intralaminar screw fixation technique, C7 lateral mass screws (3.5φ × 12 mm) inserted into the lateral mass, and C7 pedicle screws (measuring 3.5φ × 24 mm) inserted into the C7 pedicle (Fig. 1).
Fig. 1.
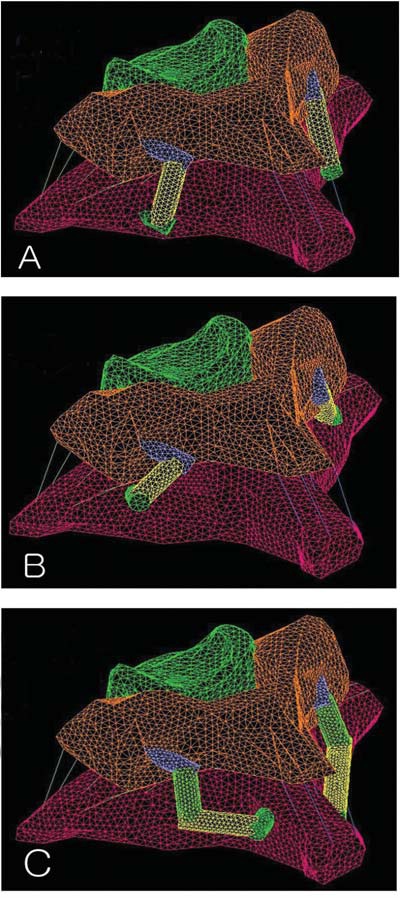
Illustration shows the three different C7 fixation methods. Lateral mass screws (A), pedicle screw (B), and intralaminar screws (C) are inserted.
Screws and the connecting rods were modeled as 3D solid elements with free-form meshing. Screws were approximated as cylinders with a Young's modulus of 100 GPa and were rigidly connected to the vertebrae. The connecting rod was also modeled as a cylinder and was rigidly connected to C6 and C7 screws. Elastic modulus of the connecting rod was adjusted to 300 MPa to allow for the motion of the connecting rod at the screw-connecting rod joint in the real scenario.
The inferior face of the C7 vertebra was constrained in translation along the three principal planes. Moments were simulated by the application of two equal and opposite point loads on the superior surface of the C6 vertebra. A 1.5 Nm flexion moment, 1.5 Nm extension moment, ± 1.5 Nm lateral bending moment, and ± 2.0 Nm axial rotation moment was applied to the C6–C7 segment.
Model validation
The intact finite element model was validated by comparing the range of motion (ROM) results against the cadaver study results.14) The cadaver study method is explained briefly below.
Ten fresh frozen human cadaver spines spanning from C5 to T1 were obtained. Donor criteria excluded subjects with history of spine trauma, osteoporosis, or any other bony diseases or radiation to the spine area. Any attached soft tissue not needed in the test was removed, carefully preserving the joint capsules and ligaments. C5 and T1 vertebral bodies were potted in a polymethylmethacrylate fixture in a manner that maintained the physiological motion from C6 to C7 and neutral and sagittal balance. The specimens were stored wrapped in saline-soaked gauze at −20°C until the day before testing, when they were allowed to thaw overnight in a +4°C refrigerator for 24 hrs.
Each specimen was mounted on a custom-built test frame designed to apply pure moments to a loading arm attached to the potted fixture on top of the C6 vertebral body. Polyaxial cervical screws (Mountaineer, DePuy Spine, Raynham, Massachusetts, USA) 3.5φ × 14 mm were inserted into the lateral mass of C6. Instrumentation of C7 was randomly alternated between laminar screws (3.5φ × 24 mm length) using the intralaminar screw fixation technique described by Wright for C2 fixation or C7 lateral mass screws (3.5φ × 12 mm) inserted into the lateral mass or C7 pedicle screws (measuring 3.5φ × 24 mm) inserted into the C7 pedicle. Pure moments along flexion/extension (1.5 Nm), lateral bending (1.5 Nm), and axial rotation (2.0 Nm) were applied. All moments were applied as a continuous load in order to produce smooth motion data with the Motion Analysis camera system. Vertebral motion was measured with a motion capture system (Motion Analysis Corp., Santa Rosa, California, USA) by tracking a set of reflective markers attached to the C6 and C7 vertebral bodies. ROM and rigid-body kinematics were calculated using dedicated analysis software (EvaRT 4.2, Motion Analysis Corp.). Each specimen was tested in four modes: (1) intact, (2) bilateral C6–C7 lateral mass screw fixation, (3) bilateral C6 lateral mass–C7 pedicle screw fixation, and (4) bilateral C6 lateral mass–C7 intralaminar screw fixation. The sequence of fixation testing was randomized to eliminate the effect of test order.
The comparison of ROM results from the cadaver study with finite element study is shown in Fig. 1. The finite element model ROM under flexion/extension and axial rotation moment corresponded well and were within one standard deviation of the cadaver study results. Lateral bending result from finite element model was 10% lower than one standard deviation of the cadaver results.
Results
I. Changes in ROM
Each type of C7 instrumentation significantly reduced the ROM compared with the intact spine in flexion, extension, axial rotation, and lateral bending (Fig. 2A). Biomechanical comparison of the three different types of fixation was performed using percentage ROM (PROM) was defined as:
Fig. 2.
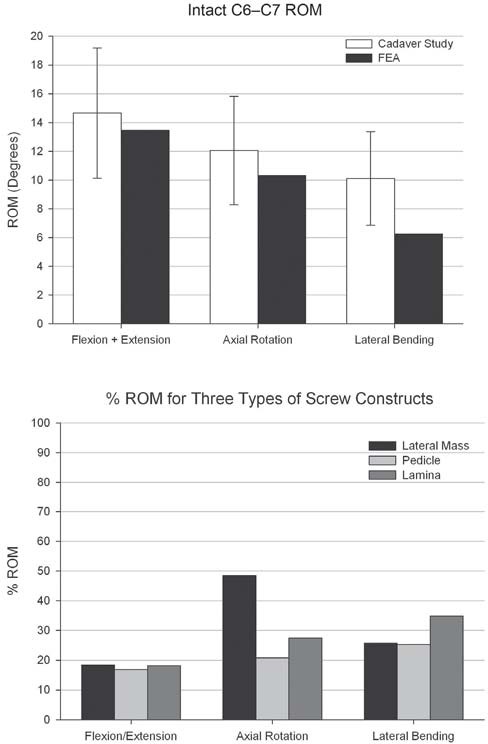
A: The range of motion (ROM) results from an intact finite element model compared very well against the cadaver study results. B: Biomechanical comparison of the three different types of fixation was done with the help of percentage ROM (PROM). All the three types of C7 instrumentation significantly reduced the ROM compared with the intact spine in flexion, extension, axial rotation, and lateral bending. FEA: finite element analysis.
The pedicle screw construct showed the least PROM in all loading modes. Intralaminar screw construct performed better than lateral mass screw construct under flexion/extension and axial rotation. PROM in flexion/extension for pedicle screw construct was found to be 16.9% as compared to 18.4% and 18.1% for lateral mass screw construct and intralaminar screw construct, respectively. PROM in axial rotation for pedicle screw construct was found to be 20.9% as compared to 48.5% and 27.5% for lateral mass screw construct and intralaminar screw construct, respectively. PROM in lateral bending for pedicle screw construct was found to be 25.3% as compared to 25.7% and 34.9% for lateral mass screw construct and intralaminar screw construct, respectively (Fig. 2B).
Figure 3 compares the results from the finite element study to the cadaver study PROM results in flexion/extension, axial rotation, and lateral bending for lateral mass screw construct, pedicle screw construct, and intralaminar screw construct, respectively. The finite element ROM results corresponded well with the cadaver study results for the three types of screw constructs in all loading modes. Largest range in PROM was found under axial rotation in all screw fixation systems in the cadaver study followed by change under flexion/extension and lateral bending. Finite element study showed that lateral mass screw permitted largest PROM in axial rotation, as opposed to pedicle screw and laminar screws permitted largest PROM in lateral bending. However, lateral bending produced only a small (5%) increase in PROM as compared to the effect due to axial rotation in these two screw systems.
Fig. 3.
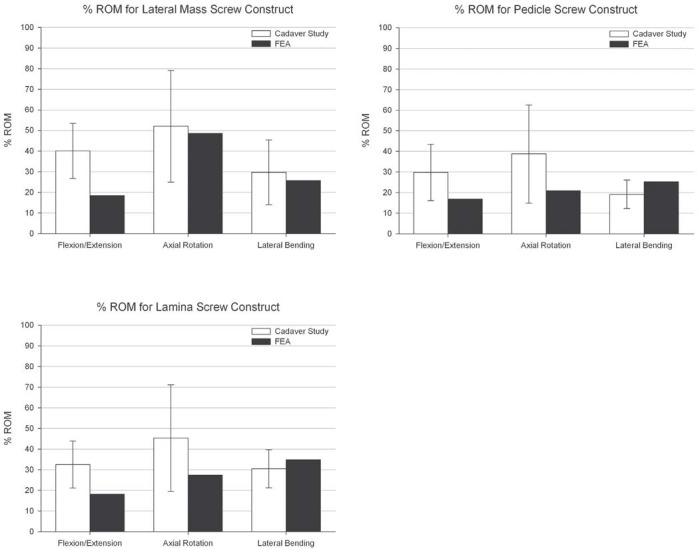
A: Comparison of the results from the finite element study to the cadaver study PROM results in flexion/extension, axial rotation and lateral bending for lateral mass screw construct. The finite element ROM results corresponded well with the cadaver study results in all loading modes. B: Comparison of the results from the finite element study to the cadaver study PROM results in flexion/extension, axial rotation, and lateral bending for pedicle screw construct. The finite element ROM results corresponded well with the cadaver study results in all loading modes. C: Comparison of the results from the finite element study to the cadaver study PROM results in flexion/extension, axial rotation, and lateral bending for lamina screw construct. The finite element ROM results corresponded well with the cadaver study results in all loading modes. FEA: finite element analysis, PROM: percentage range of motion, ROM: range of motion.
II. Stress in the vertebrae
The maximum von Mises stress was observed to be around the pedicle in the C7 vertebra in the three types of constructs under all loading modes. The pedicle screw construct showed the least von Mises stress of the three screw constructs in all loading modes. Lateral mass screw construct showed higher von Mises stress than the intralaminar screw construct in all loading modes except under axial rotation. Maximum von Mises stress under extension for pedicle screw construct was found to be 30% and 22% smaller than those for lateral mass screw construct and intralaminar screw construct, respectively (Fig. 4). Maximum von Mises stress under flexion for pedicle screw construct was found to be 32% and 25% smaller than those for lateral mass screw construct and intralaminar screw construct, respectively. Maximum von Mises stress under lateral bending for pedicle screw construct was found to be 25% and 10% smaller than those for lateral mass screw construct and intralaminar screw construct, respectively. Maximum von Mises stress under axial rotation for pedicle screw construct was found to be 10% and 14% smaller than those for lateral mass screw construct and intralaminar screw construct, respectively.
Fig. 4.
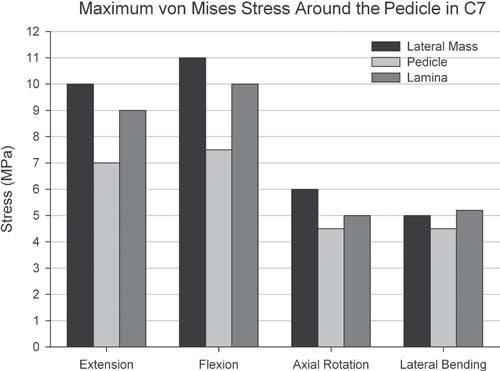
The maximum Von misses stress was observed to be around the pedicle in the C7 vertebra in the three types of constructs under all loading modes. The pedicle screw construct showed the least Von misses stress of the three screw constructs in all loading modes. Lateral mass screw construct showed higher Von misses stress than the intralaminar screw construct in all loading modes except under axial rotation.
Discussion
Pedicle screw fixation in the cervical spine can be technically difficult and potentially dangerous, where the margin for error is small, as important vascular structures and nerves abound in this region.41) In addition, complicated biomechanical forces are present at the cervicothoracic junction between the flexible cervical and rigid thoracic spines.4) Lateral mass screws, while easier and safer to insert, cannot always be placed into C7 and are known to exhibit lower pullout strengths.6)
Recently, authors described a novel technique of laminar screw fixation of the subaxial cervical spine and reported successful case series using this technique.5,23,42) One major advantage of this technique is to eliminate the risk of injury to neurovascular structures by screw placement as the translaminar screws remain in the posterior element. When the VA courses into the C7 TF, insertion of a C7 pedicle screw carries the risk of injuring either the adjacent VA or spinal cord. The use of laminar screws allows immobilization of the C7 without causing risk to the VA in these cases. Another important advantage of laminar screw fixation is the use of a navigation system is not longer necessary, because the screw can be placed under direct vision of the lamina and all relevant structures.25,43)
In spite of this, concern about the C7 laminar screw is the lack of the biomechanical study in the literature comparing construct stability and screw pullout strength of C7 intralaminar screws versus other type of C7 screws. Consequently, the objective of this study was to investigate and compare the posterior cervical construct stability afforded by this novel C7 intralaminar screw technique with that of the more commonly used lateral mass technique and transpedicular screw fixation method.
The current study employed a finite element model of a C6–C7 human spinal segment to compare the kinematics and the maximum stress in the vertebra for the three types of screw constructs. Validation study demonstrated excellent comparison with kinematics data from cadaver study. This study showed that all three fixation system adequately stabilize (better than intact spine) the C6–C7 segment in flexion, extension, lateral bending, and axial rotation.
To summarize the kinematics results, the C7 laminar screw was equivalent to a C7 pedicle screw fixation in flexion/extension, axial rotation but inferior in lateral bending. C7 lateral mass screw was equivalent to C7 pedicle screw fixation in flexion/extension, lateral bending but inferior in axial rotation.
Larger ROM was observed for the laminar construct under lateral bending than the other two fixation constructs considered. This is attributed to the orientation of the connecting rod between the C6 and C7 screws which allows for a larger motion under lateral bending.
However, efficacy of the fixation construct cannot be judged based on the ROM only. Stress distribution in the motion segment under different loading modes is an important consideration in assessing the mechanical characteristics of the fixation technique. It is not possible to obtain stress distribution in the cadaver testing. That is why authors found it necessary to perform finite element analyses in addition to the experimental testing.
There was not so much difference in maximum effective stress around the C6 lateral mass screw between three different constructs. However, maximum effective stress data around the C7 screw shows there was vivid difference between each type of constructs. Stress around the C7 pedicle screw was highest, and that around C7 lateral mass screw was lowest. All three constructs showed higher stress around the C7 pedicle compared to the intact spine model. And also, maximum effective stress on the C7 pedicle was highest in lateral mass construct and lowest in pedicle screw construct, which suggest that pedicle screw, intralaminar screw, and lateral mass screw, in that order, has higher load sharing capability for C7 fixation.
Finite element models predicted higher stresses in the C7 vertebra for lateral mass fixation construct as compared with the other two fixation techniques. Higher stresses in the vertebra represent the greater risk of failure of the fixation construct due to vertebra fracture. Thus, the finite element analyses pinpoints lateral mass fixation construct as the weakest technique susceptible to greater risk of failure. Also the maximum stress in the vertebra under flexion (11 MPa) and extension (10 MPa) were considerably higher than that under axial rotation (6 MPa) and lateral bending (5.2 MPa). Although ROM under flexion/extension were very similar for the three fixation constructs (Fig. 2), the stresses for lateral mass construct (Flexion: 11 MPa, Extension: 10 MPa) were considerably higher than lamina construct (Flexion: 10 MPa, Extension: 9 MPa), and pedicle construct (Flexion: 7.5 MPa, Extension: 7 MPa). This observation provides a good reason for conducting finite element analyses in addition to the cadaver experiment.
These results suggest that pedicle screws provide the strongest fixation in C7, as expected. But in cases where the pedicle screw is not favorable or when pedicle screw should fail, the use of C7 laminar screws seems to be a stronger and more reproducible fixation than employing lateral mass screws.
It is important that this result is kept within the context of its limitations. For example, the forces exerted by muscle and tendons in the physiological situation cannot be modeled in the laboratory. Furthermore, the relationship between stability and its effect on the bone fusion has not quantified yet in the cervical spine. And also, the computation model does not take into account the anatomical parameter variations of pedicle, lamina, and lateral mass of each patient. Future research will involve the development of a model that will incorporate changes in muscle force and their mechanical influence on various surgical techniques.
In finite element models, screws were assumed to be rigidly connected to the vertebrae. However in cadaver experimental testing, screws were inserted in the vertebrae without any cement, thus some relative motion between the screws and vertebrae was expected. Due to the assumption of rigid connection between the screws and the bone, smaller ROM was predicted by finite element models as compared to the cadaver testing. This phenomenon was more pronounced under flexion/extension than under axial rotation and lateral bending. Another drawback of finite element model testing is that this data cannot guarantee long-term stability. Future studies on fatigue tests and clinical data will throw more light on long-term stability and fusion rates.
Conclusion
The current study demonstrated that C7 pedicle screw provides most stable construct for C6–C7 posterior fixation. If C7 pedicle fixation is not possible, C7 laminar screw can be an alternative fixation point with similar limitation of motion except in lateral bending and higher load sharing capability compared to lateral mass screw.
References
- 1). Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, Crawford NR: Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine 30: 915– 922, 2005. [DOI] [PubMed] [Google Scholar]
- 2). Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M: Effect of constrained posterior screw and rod systems for primary stability: biomechanical in vitro comparison of various instrumentations in a single-level corpectomy model. Eur Spine J 14: 372– 380, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Papagelopoulos PJ, Currier BL, Neale PG, Hokari Y, Berglund LJ, Larson DR, Fisher DR, An KN: Biomechanical evaluation of posterior screw fixation in cadaveric cervical spines. Clin Orthop Relat Res 13– 24, 2003. [DOI] [PubMed] [Google Scholar]
- 4). Rhee JM, Kraiwattanapong C, Hutton WC: A comparison of pedicle and lateral mass screw construct stiffnesses at the cervicothoracic junction: a biomechanical study. Spine 30: E636– 640, 2005. [DOI] [PubMed] [Google Scholar]
- 5). Hong JT, Sung JH, Son BC, Lee SW, Park CK: Significance of laminar screw fixation in the subaxial cervical spine. Spine 33: 1739– 1743, 2008. [DOI] [PubMed] [Google Scholar]
- 6). Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D: Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J 6: 667– 672, 2006. [DOI] [PubMed] [Google Scholar]
- 7). Kothe R, Rüther W, Schneider E, Linke B: Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine 29: 1869– 1875, 2004. [DOI] [PubMed] [Google Scholar]
- 8). Reinhold M, Magerl F, Rieger M, Blauth M: Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J 16: 47– 56, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Karaikovic EE, Yingsakmongkol W, Gaines RW: Accuracy of cervical pedicle screw placement using the funnel technique. Spine 26: 2456– 2462, 2001. [DOI] [PubMed] [Google Scholar]
- 10). Xu R, Kang A, Ebraheim NA, Yeasting RA: Anatomic relation between the cervical pedicle and the adjacent neural structures. Spine 24: 451– 454, 1999. [DOI] [PubMed] [Google Scholar]
- 11). Kim HS, Heller JG, Hudgins PA, Fountain JA: The accuracy of computed tomography in assessing cervical pedicle screw placement. Spine 28: 2441– 2446, 2003. [DOI] [PubMed] [Google Scholar]
- 12). Miller RM, Ebraheim NA, Xu R, Yeasting RA: Anatomic consideration of transpedicular screw placement in the cervical spine. An analysis of two approaches. Spine 21: 2317– 2322, 1996. [DOI] [PubMed] [Google Scholar]
- 13). Holly LT, Foley KT: Percutaneous placement of posterior cervical screws using three-dimensional fluoroscopy. Spine 31: 536– 540; discussion 541, 2006. [DOI] [PubMed] [Google Scholar]
- 14). Hong JT, Tomoyuki T, Udayakumar R, Espinoza Orías AA, Inoue N, An HS: Biomechanical comparison of three different types of C7 fixation techniques. Spine 36: 393– 398, 2011. [DOI] [PubMed] [Google Scholar]
- 15). Mazel C, Hoffmann E, Antonietti P, Grunenwald D, Henry M, Williams J: Posterior cervicothoracic instrumentation in spine tumors. Spine 29: 1246– 1253, 2004. [DOI] [PubMed] [Google Scholar]
- 16). Barrey C, Cotton F, Jund J, Mertens P, Perrin G: Transpedicular screwing of the seventh cervical vertebra: anatomical considerations and surgical technique. Surg Radiol Anat 25: 354– 360, 2003. [DOI] [PubMed] [Google Scholar]
- 17). Hong JT, Park DK, Lee MJ, Kim SW, An HS: Anatomical variations of the vertebral artery segment in the lower cervical spine: analysis by three-dimensional computed tomography angiography. Spine 33: 2422– 2426, 2008. [DOI] [PubMed] [Google Scholar]
- 18). Arand M, Kinzl L, Gebhard F: [Sources of error and risks in CT based navigation]. Orthopade 31: 378– 384, 2002. (German) [DOI] [PubMed] [Google Scholar]
- 19). Reinhold M, Bach C, Audigé L, Bale R, Attal R, Blauth M, Magerl F: Comparison of two novel fluoroscopy-based stereotactic methods for cervical pedicle screw placement and review of the literature. Eur Spine J 17: 564– 575, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Kamimura M, Ebara S, Itoh H, Tateiwa Y, Kinoshita T, Takaoka K: Cervical pedicle screw insertion: assessment of safety and accuracy with computer-assisted image guidance. J Spinal Disord 13: 218– 224, 2000. [DOI] [PubMed] [Google Scholar]
- 21). Rath SA, Moszko S, Schäffner PM, Cantone G, Braun V, Richter HP, Antoniadis G: Accuracy of pedicle screw insertion in the cervical spine for internal fixation using frameless stereotactic guidance. J Neurosurg Spine 8: 237– 245, 2008. [DOI] [PubMed] [Google Scholar]
- 22). Abumi K, Ito M, Kaneda K: Surgical treatment of cervical destructive spondyloarthropathy (DSA). Spine 25: 2899– 2905, 2000. [DOI] [PubMed] [Google Scholar]
- 23). Hong JT, Yi JS, Kim JT, Ji C, Ryu KS, Park CK: Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation—review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg 73: 112– 118; discussion e15, 2010. [DOI] [PubMed] [Google Scholar]
- 24). Kretzer RM, Sciubba DM, Bagley CA, Wolinsky JP, Gokaslan ZL, Garonzik IM: Translaminar screw fixation in the upper thoracic spine. J Neurosurg Spine 5: 527– 533, 2006. [DOI] [PubMed] [Google Scholar]
- 25). Wright NM: Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 17: 158– 162, 2004. [DOI] [PubMed] [Google Scholar]
- 26). Cardoso MJ, Dmitriev AE, Helgeson MD, Stephens F, Campbell V, Lehman RA, Cooper P, Rosner MK: Using lamina screws as a salvage technique at C-7: computed tomography and biomechanical analysis using cadaveric vertebrae. Laboratory investigation. J Neurosurg Spine 11: 28– 33, 2009. [DOI] [PubMed] [Google Scholar]
- 27). Jea A, Johnson KK, Whitehead WE, Luerssen TG: Translaminar screw fixation in the subaxial pediatric cervical spine. J Neurosurg Pediatr 2: 386– 390, 2008. [DOI] [PubMed] [Google Scholar]
- 28). Hussain M, Natarajan RN, Chaudhary G, An HS, Andersson GB: Relative contributions of strain-dependent permeability and fixed charged density of proteoglycans in predicting cervical disc biomechanics: a poroelastic C5-C6 finite element model study. Med Eng Phys 33: 438– 445, 2011. [DOI] [PubMed] [Google Scholar]
- 29). Nissan M, Gilad I: The cervical and lumbar verte-brae—an anthropometric model. Eng Med 13: 111– 114, 1984. [DOI] [PubMed] [Google Scholar]
- 30). Kumaresan S, Yoganandan N, Pintar FA, Macias M, Cusick JF: Morphology of young and old cervical spine intervertebral disc tissues. Biomed Sci Instrum 36: 141– 146, 2000. [PubMed] [Google Scholar]
- 31). Panjabi MM, Duranceau J, Goel V, Oxland T, Takata K: Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine 16: 861– 869, 1991. [DOI] [PubMed] [Google Scholar]
- 32). Skrzypiec DM, Pollintine P, Przybyla A, Dolan P, Adams MA: The internal mechanical properties of cervical intervertebral discs as revealed by stress profilometry. Eur Spine J 16: 1701– 1709, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33). Vasavada AN, Danaraj J, Siegmund GP: Head and neck anthropometry, vertebral geometry and neck strength in height-matched men and women. J Biomech 41: 114– 121, 2008. [DOI] [PubMed] [Google Scholar]
- 34). Panjabi MM, Oxland TR, Parks EH: Quantitative anatomy of cervical spine ligaments. Part II. Middle and lower cervical spine. J Spinal Disord 4: 277– 285, 1991. [DOI] [PubMed] [Google Scholar]
- 35). Yoganandan N, Kumaresan S, Pintar FA: Geometric and mechanical properties of human cervical spine ligaments. J Biomech Eng 122: 623– 629, 2000. [DOI] [PubMed] [Google Scholar]
- 36). Argoubi M, Shirazi-Adl A: Poroelastic creep response analysis of a lumbar motion segment in compression. J Biomech 29: 1331– 1339, 1996. [DOI] [PubMed] [Google Scholar]
- 37). Clausen JD, Goel VK, Traynelis VC, Scifert J: Unci-nate processes and Luschka joints influence the biomechanics of the cervical spine: quantification using a finite element model of the C5-C6 segment. J Orthop Res 15: 342– 347, 1997. [DOI] [PubMed] [Google Scholar]
- 38). Kumaresan S, Yoganandan N, Pintar FA: Finite element modeling approaches of human cervical spine facet joint capsule. J Biomech 31: 371– 376, 1998. [DOI] [PubMed] [Google Scholar]
- 39). Lee CK, Kim YE, Lee CS, Hong YM, Jung JM, Goel VK: Impact response of the intervertebral disc in a finite-element model. Spine 25: 2431– 2439, 2000. [DOI] [PubMed] [Google Scholar]
- 40). Teo EC, Ng HW: Evaluation of the role of ligaments, facets and disc nucleus in lower cervical spine under compression and sagittal moments using finite element method. Med Eng Phys 23: 155– 164, 2001. [DOI] [PubMed] [Google Scholar]
- 41). Ebraheim NA, Tremains M, Xu R, Yeasting RA: Anatomic study of the cervicothoracic spinal nerves and their relation to the pedicles. Am J Orthop 29: 779– 781, 2000. [PubMed] [Google Scholar]
- 42). Jang SH, Hong JT, Kim IS, Yeo IS, Son BC, Lee SW: C7 posterior fixation using intralaminar screws : early clinical and radiographic outcome. J Korean Neurosurg Soc 48: 129– 133, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43). Wang MY: Cervical crossing laminar screws: early clinical results and complications. Neurosurgery 61: 311– 315; discussion 315–316, 2007. [DOI] [PubMed] [Google Scholar]


