Abstract
A novel cortical bone trajectory (CBT) screw technique provides an alternative fixation technique for lumbar spine. Trajectory of CBT screw creates a caudo-cephalad path in sagittal plane and a medio-lateral path in axial plane, and engages cortical bone in the pedicle. The theoretical advantage is that it provides enhanced screw grip and interface strength. Midline lumbar fusion (MIDLF) is composed of posterior mid-line approach, microsurgical laminectomy, and CBT screw fixation. We adopted the MIDLF technique for lumbar spondylolisthesis. Advantages of this technique include that decompression and fusion are available in the same field, and it minimizes approach-related damages. To determine whether MIDLF with CBT screw is as effective as traditional approach and it is minimum invasive technique, we studied the clinical and radiological outcomes of MIDLF. Our results indicate that MIDLF is effective and minimum invasive technique. Evidence of effectiveness of MIDLF is that patients had good recovery score, and that CBT screw technique was safety in clinical and stable in radiological. MIDLF with CBT screw provides the surgeon with additional options for fixation. This technique is most likely to be useful for treating lumbar spondylolisthesis in combination with midline decompression and insertion of an interbody graft, such as the transforaminal lumbar interbody fusion or posterior lumbar interbody fusion techniques.
Keywords: midline lumbar fusion, cortical bone trajectory, spondylolisthesis, osteoporosis, minimum invasive
Introduction
Lumbar arthrodesis for degenerative spine disease includes many techniques. Posterior decompression and pedicle screw fixation are two of the most standard techniques for lumbar unstable degenerative lesion. Although pedicle screw fixation is a common and reliable method, there are several disadvantages, which are invasive nature of traditional placement, potential risk for screw pullout, and additional approach to accomplish decompression and bone graft insertion.
Concerning invasive feature, minimally invasive techniques in spine surgery have evolved over the last decade,1) and less invasive pedicle screw instrumentations have been developed including an alternative percutaneous technique.2)
As for screw failure, stiffness of the standard trajectory screw depends on dorsal cortex and cancellous bone density at the pedicle and vertebral body.3) In case of osteoporotic bone condition, screw loosening was well-known complication.4) A novel cortical bone trajectory (CBT) screw fixation diminishes this complication.5) In the pedicle, trajectory of screw creates a caudo-cephalad path in sagittal plane and a medio-lateral path in axial plane, and CBT screw engages cortical bone (Fig. 1). The theoretical advantage associated with this technique is increased cortical bone contact, providing enhanced screw grip and interface strength independent of trabecular bone mineral density.
Fig. 1.
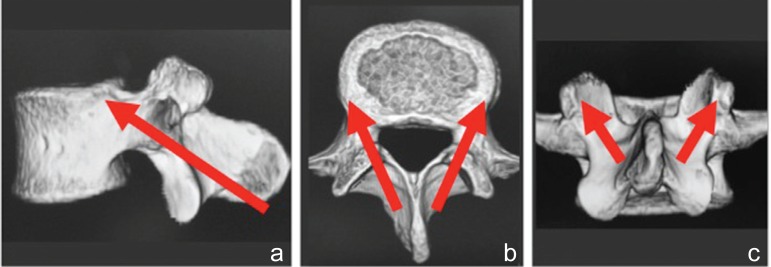
Trajectory of cortical bone screw. a: In sagittal plane, caudal to cranial direction of screw, b: medial to lateral trajection of screw in axial plane, c: CBT screw through the cortical bone of lamina and pedicle. CBT: cortical bone trajectory.
In addition, although percutaneous pedicle screw technique has been well known as minimum invasive method,6) it requires an additional approach for decompression and bone graft insertion. Therefore, we adopted the midline lumbar fusion (MIDLF) technique for degenerative pathologies. MIDLF is composed of posterior midline approach, microsurgical laminectomy, and CBT screw fixation. Advantages of this technique include that decompression and fusion is feasible in the same field, it minimizes approach-related damages, and it is suitable for osteoporotic patient.
To determine whether MIDLF with CBT screw is as effective as traditional approach and it is minimum invasive technique, we established a method to perform MIDLF and studied the clinical and radiological outcomes of MIDLF.
Methods
I. Patient population
From March 2012 to March 2014, 12 patients (mean age 68.3 years, range 47–80 years; 7 males, 5 females) underwent MIDLF procedures for the treatment of single level lumbar spondylolisthesis. Follow-up period averaged 15 months (range 3–26 months). Ten (83.3%) of 12 patients had more than 6 months of follow-up. The retrospective review was performed by two of the authors (M. Mizuno and K. Kuraishi).
II. Clinical evaluation
All patients were selected for surgery from the outpatient clinic. Evaluation of the lumbar spondylolisthesis was performed by X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scan. CT myelography was performed in patients when the lesions appeared multiple or scoliotic. A neurological examination was performed in all patients by an attending board-certified neurosurgeon at preoperative and postoperative visits. Patient's symptoms were classified according to the Japanese Orthopedic Association (JOA) score (range from −3 points to 29 points). Inflammatory markers including serum creatine kinase (CK, normal limit; 12–170), CK-ratio (postoperative day 1 CK/postoperative day 7 CK), C-reactive protein (CRP, 0–0.30), and white blood cell (WBC, 4,300–6,900) count were measured in 9 cases out of 12 preoperatively and 7 days later postoperatively. Postoperative MRI and/or CT imaging was obtained in all patients to confirm decompression and fusion. The radiographs were examined for evidence of hardware failure, detection of radiolucent zone, loosening of the construct, or signs of spinal instability. Bony fusion was estimated that motion angle was below 2 degree on flexion-extension lateral X-rays, and continuous bony bridge at the interbody space was identified by CT scan image.
III. Surgical indication
Specifically, this study was used to confirm the presence of any of the following: dural theca and/or cauda equina compression, nerve root impingement, or hypertrophic facets with canal encroachment. All patients displayed both low back and sciatic pain, with or without claudication. Indication for inter-body fusion were over 4 mm olisthesis and over 10 degree angular motion on flexion-extension lateral radiographs.7) Secondary inclusion criteria for this study encompassed but did not require the following: degenerative spondylolisthesis up to Meyerding Grade II, isthmic spondylolisthesis, and advanced facet arthrosis. Mimicking pathologies were excluded from this study, including unilateral foraminal stenosis, spondylitis, or sacroiliac joint dysfunction.
Bony fusion method, that is posterior lumbar interbody fusion (PLIF) or transforaminal lumbar interbody fusion (TLIF), was selected by pathogenesis, degree of spondylolisthesis, and presence of vertebral body deformity. In patients with isthmic spondylolisthesis, MIDLF with PILF was considered for surgical treatment (Fig. 2).
Fig. 2.
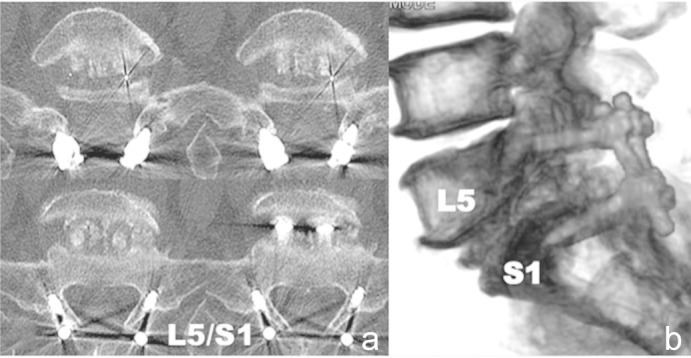
Cortical bone trajectory (CBT) screw and posterior lumbar interbody fusion (PLIF). a: Postoperative computed tomography (CT) scan showing L5/S1 CBT screw fixation and interbody cages with bone graft. b: 3-dimensional reconstruction CT showing interbody fusion of L5/S1 and CBT screw fixation.
IV. Surgical approach of MIDLF
The sequence of MIDLF procedure was as follows: midline posterior approach, spinous process splitting, making of screw trajectory, microsurgical trumpet laminectomy, PLIF or TLIF for bony union, and CBT screw fixation.
Midline skin incision is made at the level of affected spinous process (Fig. 3a). The spinous process splitting is able to achieve the appropriate angulation for CBT screw trajectory. Since the microsurgical trumpet laminectomy approach has been well known,8) we describe the process of CBT screw insertion in this part.
Fig. 3.
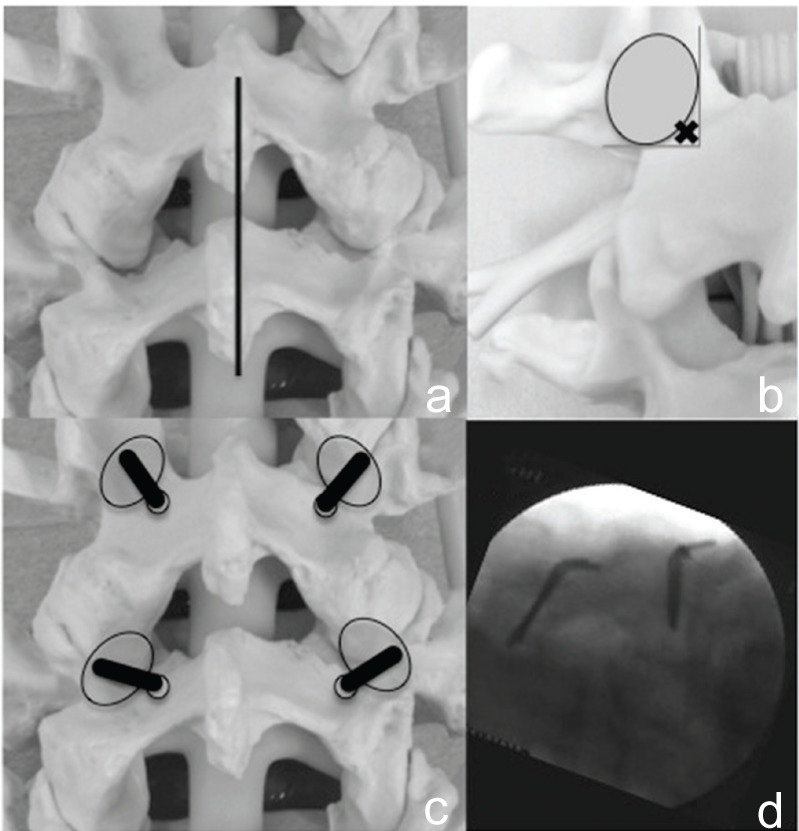
Surgical procedure of MIDLF part 1. a: Synthetic model showing midline surgical incision (black line). b: Starting point (x mark) exists at the intersection of medial and caudal aspect of pedicle. c: Synthetic model showing cortical bone trajectory of maker pins. d: Intraoperative lateral image demonstrated the proper position of maker pins. MIDLF: midline lumbar fusion.
For safe insertion of CBT screw, we recommend using fluoroscopy during all steps. Under anterior-posterior (AP) image, the initial starting point is identified at medial and caudal point of the pedicle (Fig. 3b). Using a 2 mm high-speed diamond drill, we make the initial hole and take care to prevent fracture of the pars.
The surgeon advances the cervical fine pedicle probe to medio-lateral and caudo-cranial direction using AP imaging, making sure not to breach the pedicle wall and using a sounder to check the lateral placement of the hole.
Following completion of the pedicle trajectory, it is indispensable for the surgeon to tap the hole as the size is the same as the planned screw. For example, the surgeon taps the hole to 4.5 mm if planning to use a 4.5 mm screw. Under-tapping can result in fracture of the pars when the surgeon attempts to insert a large screw into an undersized cortical bone hole. If a pars fracture occurs, we recommend making another fascial incision and placing a pedicle screw via a standard trajectory through the intermuscular approach.
The surgeon advances the guiding maker pin with the use of AP and lateral images to confirm its accurate placement (Fig. 3c, d).
After preparing the screw insertion, we perform laminectomy and decompress the neural structures (Fig. 4a), and then we can complete bony grafting into the disc space, and perform PLIF or TLIF.
Fig. 4.
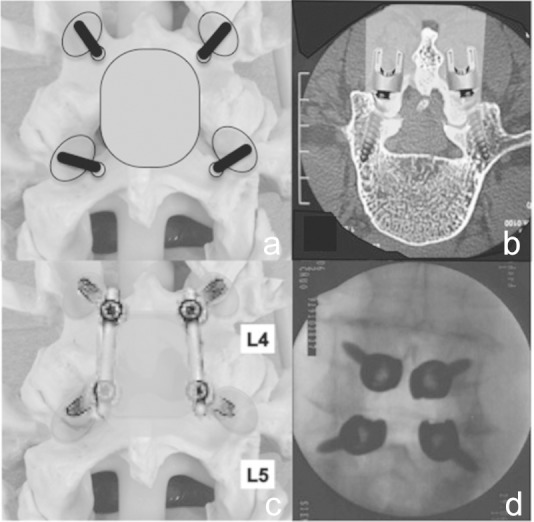
Surgical procedure of MIDLF part 2. a: Synthetic model showing laminectomy zone (gray oval area). b: Figure illustrated the minimum access route of MIDLF including microsurgical laminectomy and CBT screw fixation. c: Synthetic model showing accomplishment of the MIDLF with decompression and CBT fusion. d: Intraoperative AP image demonstrated the CBT screw insertion. CBT: cortical bone trajectory, MIDLF: midline lumbar fusion.
Finally, we insert CBT screws (Fig. 4b–d). A standard screw diameter for a CBT pedicle screw is 4.5 mm to 5.5 mm, with a length of 25–30 mm. We use screws of Medtronic (Memphis, Tennessee, USA), the Stryker Japan, Tokyo, and CMI, Tokyo. The position of the tulip of the screw determines rod placement. When tulips lie in a close position, rod placement may be complicated. However, with the use of poly-axial screws, it should not be too difficult.
We recommend a postoperative CT to check that the CBT screw is within the confines of the pedicle.
Results
I. Clinical features
Seven males and five females underwent MIDLF with CBT + PLIF/TLIF (Fig. 5). The ages of the patients ranged from 47 years to 80 years (mean, 68.3 years, Table 1).
Fig. 5.
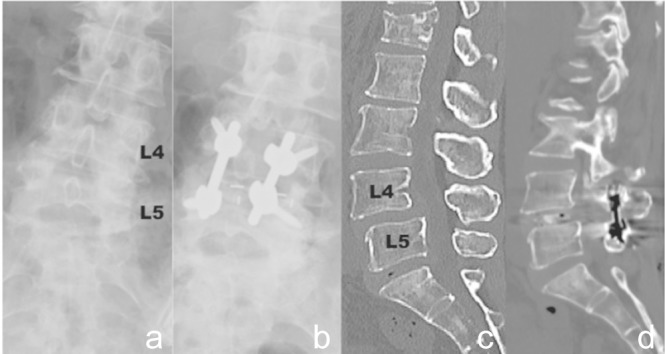
CBT screw and posterior lumbar interbody fusion (PLIF). a: Preoperative AP X-ray. b: Postoperative AP X-ray showing interbody fusion cages of L4/5 and CBT screw fixation. c: Preoperative reconstruction sagittal CT demonstrating L4/5 spondylolisthesis. d: Postoperative reconstruction sagittal CT demonstrating L4/5 interbody fusion and mild reduction of spondylolisthesis. AP: anterior-posterior, CBT: cortical bone trajectory, CT: computed tomography.
Table 1.
Results of MIDLF
| Case | Age | Gender | Level | Patho. | Fusion | Follow-up (MOS) | Preop. JOA score | Postop. JOA score | RR (%) | Labo data | Complication | Postop. Imaging |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 67 | M | L5/S1 | IS | PLIF | 26 | 23 | 27 | 67 | + | − | Fusion |
| 2 | 67 | M | L5/S1 | IS | PLIF | 24 | 13 | 25 | 75 | + | − | Fusion |
| 3 | 60 | M | L5/S1 | IS | PLIF | 22 | 11 | 18 | 39 | − | − | Fusion |
| 4 | 80 | F | L5/S1 | DS | TLIF | 26 | 14 | 22 | 53 | + | − | |
| 5 | 72 | M | L5/S1 | IS | PLIF | 20 | 4 | 24 | 80 | − | − | Fusion |
| 6 | 47 | M | L5/S1 | IS | PLIF | 20 | 16 | 27 | 85 | − | − | Fusion |
| 7 | 78 | F | L4/5 | DS | TLIF | 15 | 4 | 19 | 60 | + | − | |
| 8 | 61 | F | L4/5 | IS | PLIF | 12 | 6 | 26 | 87 | + | − | Perforation |
| 9 | 70 | F | L4/5 | DS | TLIF | 8 | 8 | 15 | 33 | + | Fracture | |
| 10 | 72 | F | L4/5 | DS | TLIF | 7 | 11 | 22 | 61 | + | − | Perforation x2 |
| 11 | 74 | M | L4/5 | DS | TLIF | 4 | 16 | 23 | 54 | + | − | |
| 12 | 71 | M | L4/5 | IS | PLIF | 3 | 24 | 29 | 100 | + | − | Perforation |
DS: degenerative spondylolisthesis, F: female, IS: isthmic spondylolisthesis, JOA: Japanese Orthopedic Association, M: male, MIDLF: midline lumbar fusion, perforation: cortical perforation of cortical bone trajectory screw, PLIF: posterior lumbar interbody fusion, RR: recovery rate of JOA score, TLIF: transforaminal lumbar interbody fusion.
In cases of MIDLF, preoperative JOA score was 12.5 points (range, 4–24 points) and postoperative score was 23.1 points (range, 18–29 points). Recovery rate was 66.1% (range, 39–100%, Table 1).
There was one case of intraoperative complication, which was cortical bone fracture at the screw compression. No patient had surgery-related spinal nerve injury or new neurological deficit. As for 48 screws in 12 patients, there was no screw related nerve injury.
In 9 patients out of 12, who completed pre- and postoperative inflammatory markers data, mean CK data was 108.8 IU/L preoperatively and 122.4 U/L, 7 days later postoperatively, mean CK-ratio was 3.4 points. Mean CRP data was 0.04 mg/dL and 1.37 mg/dL and mean WBC data was 6,540/μL and 5,840/μL.
II. Radiographic findings
No failures of hardware such as fracture of the screws or rods, angulations or disconnections could be detected. Five cases over 20 months’ follow-up period revealed bony fusion by postoperative radio-graphs and CT scan (Table 1). There were no findings of screw loosing or backout in all 48 screws. Four screws (8.3%) were judged to have perforated of the wall of pedicles and vertebral bodies. The protrusion was 5.0 mm length on average (range, 3.5 mm–7.0 mm), which showed in the case of isthmic spondylolisthesis and scoliosis. There was no nerve root injury of upper side at extraforaminal space by the perforated screws.
Discussion
In the present study, we established how to perform the MIDLF with CBT screw and investigated the outcome to determine whether this method is as effective as traditional approach. Our results indicate that MIDLF is valid and is a minimum invasive technique. Evidence of effectiveness of MIDLF is that patients had a good recovery score that is similar to previous study,9) and that CBT screw technique was safety in clinical and stable in radiological. Moreover the inflammatory markers data of CK and WBC recovered in a normal limit within a week, and the ratio of CK level was equivalent to the data of mini open PLIF in the literature.9)
CBT screw technique provides an alternative fixation technique advocated by Santoni et al. in 2009.5) The concept of MIDLF has appeared with CBT screw technique. Experimental10–12) and clinical13,14) studies of CBT screw support the effectiveness of MIDLF. The theoretical advantage associated with CBT technique involves maximizing the thread contact with the higher density bone surface.15) It was found to have similar biomechanical characteristics to the traditional trajectory despite using a screw that is shorter and smaller in diameter.5) Accordingly, this technique has a potential of rigid fixation for osteoporotic patient.16)
Furthermore, the MIDLF with CBT offers several advantages over the traditional pedicle screw trajectory. At first, since the screw trajectory makes medial to lateral and caudal to cephalad path, the direction away from the neural elements provides safety and a lower incidence of nerve injury.
A second advantage is that the screw insertion through a medial starting point enables less tissue dissection and retraction for reduced muscle damage. Following the second point, because of an affinity between microsurgical laminectomy and CBT at the point of posterior minimum approach, MIDLF can operate decompression and fusion through the same surgical corridor.
In addition, since we can select the trajectory freely as long as keeping the trajectory inside the pedicle, there are numerous starting points for CBT screw.13) These advantages may contribute to reduce the surgeon's stress in clinical practice.
In contrast, there are some drawbacks in CBT screw. First, like the percutaneous pedicle screw technique, CBT approach depends on intraoperative multiplanar fluoroscopy. The surgeon has the risk of radiation exposure. But nowadays, we can reduce the risk by the usage of navigation system.
Next, posterior midline approach and decompression is familiar for spinal surgeons. However, CBT screw is novel method and not familiar for us, so that it has barriers to be related to technical difficulties of procedure. To resolve this problem, it is important for surgeon to make the strategy preoperatively (e.g., initial point, screw size, screw angle, and decompression width). It makes the procedure safe to operate.
Finally, there are some potential risks during screw insertion such as the cortical bone fractures by immoderate screw diameter, the upper nerve root injury by improper penetration or direction of screw, and the lower nerve root injury by insufficient angle trajectory. Accordingly, an accurate understanding of the anatomy and the procedures are essential for decreasing the risks.
In conclusion, our study found that MIDLF with CBT screw is effective and minimum invasive technique. It provides the surgeon with additional options for fixation. We have used the technique for a variety of pathologies including trauma, spondylitis, and degenerative conditions. However, the technique is most likely to be useful for treating single-level degenerative pathologies in combination with midline insertion of an interbody graft, such as the TLIF or PLIF technique.
References
- 1). Kim CW, Siemionow K, Anderson DG, Phillips FM: The current state of minimally invasive spine surgery. J Bone Joint Surg Am 93: 582– 596, 2011. [PubMed] [Google Scholar]
- 2). Mobbs RJ, Sivabalan P, Li J: Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci 18: 741– 749, 2011. [DOI] [PubMed] [Google Scholar]
- 3). Karataglis D, Kapetanos G, Christodoulou A, Christoforides J, Pournaras J: The role of the dorsal vertebral cortex in the stability of transpedicular screws. J Bone Joint Surg Br 88: 692– 695, 2006. [DOI] [PubMed] [Google Scholar]
- 4). Cho W, Cho SK, Wu C: The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br 92: 1061– 1065, 2010. [DOI] [PubMed] [Google Scholar]
- 5). Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, Womack WJ, Puttlitz CM: Cortical bone trajectory for lumbar pedicle screws. Spine J 9: 366– 373, 2009. [DOI] [PubMed] [Google Scholar]
- 6). Mobbs RJ, Sivabalan P, Li J: Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci 19: 829– 835, 2012. [DOI] [PubMed] [Google Scholar]
- 7). Herkowitz HN, Kurz LT: Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 73: 802– 808, 1991. [PubMed] [Google Scholar]
- 8). Mizuno M, Kubo Y, Niwa S: [Microsurgical Trumpet Laminectomy, minimum invasive surgical techniques for lumbar canal stenosis]. Spine & Spinal Cord 18: 303– 309, 2005. (Japanese) [Google Scholar]
- 9). Tsutsumimoto T, Shimogata M, Ohta H, Misawa H: Mini-open versus conventional open posterior lumbar interbody fusion for the treatment of lumbar degenerative spondylolisthesis: comparison of paraspinal muscle damage and slip reduction. Spine 34: 1923– 1928, 2009. [DOI] [PubMed] [Google Scholar]
- 10). Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K: [In vivo analysis of insertion torque during pedicle screwing using cortical bone trajectory Technique]. Spine & Spinal Cord 26: 665– 671, 2013. (Japanese) [DOI] [PubMed] [Google Scholar]
- 11). Perez-Orribo L, Kalb S, Reyes PM, Chang SW, Crawford NR: Biomechanics of lumbar cortical screw-rod fixation versus pedicle screw-rod fixation with and without interbody support. Spine 38: 635– 641, 2013. [DOI] [PubMed] [Google Scholar]
- 12). Barber JW, Boden SD, Ganey T, Hutton WC: Biomechanical study of lumbar pedicle screws: does convergence affect axial pullout strength? J Spinal Disord 11: 215– 220, 1998. [PubMed] [Google Scholar]
- 13). Mobbs RJ: The “medio-latero-superior trajectory technique”: an alternative cortical trajectory for pedicle fixation. Orthop Surg 5: 56– 59, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Shiraishi T, Aoyama T, Yamane J, Ninomiya K, Ueda S, Kato K: [Muscle-preserving posterior lumbar inter-body fusion using cortical bone trajectory screws]. Seikei-saigai 56: 69– 75, 2013. (Japanese) [Google Scholar]
- 15). Matsukawa K, Yato Y, Nemoto O, Imabayashi H, Asazuma T, Nemoto K: Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech 26: E248– E253, 2013. [DOI] [PubMed] [Google Scholar]
- 16). Inceoğlu S, Montgomery WH, St Clair S, McLain RF: Pedicle screw insertion angle and pullout strength: comparison of 2 proposed strategies. J Neurosurg Spine 14: 670– 676, 2011. [DOI] [PubMed] [Google Scholar]


