Abstract
The outcomes and complications of posterior-only lumbar instrumented long fusions exceeding three segments with selective segmental transforaminal lumbar interbody fusion for the treatment of degenerative lumbar scoliosis, kyphosis, or both combined with spondylolisthesis were analyzed to investigate risk factors associated with surgical instrumentation failure. Fifteen consecutive patients with degenerative lumbar scoliosis, kyphosis, or both combined with spondylolisthesis were studied retrospectively. There were 5 male and 10 female patients, with a mean age of 71.8 years. All the patients were followed for a mean duration of 19.4 months postoperatively. Radiographic evaluation included coronal Cobb angle, lumbar lordosis (LL) angle, pelvic incidence (PI), and pelvic tilt (PT). The clinical outcomes were assessed by means of Japanese Orthopedic Association (JOA) score. Patients were divided into two groups: group 1—7 patients with surgical complications; group 2—8 patients without complications. The preoperative and postoperative coronal Cobb's angle were not significantly different between groups 1 and 2. The LL highly correlated with developing surgical complications. There were statistically significant differences in preoperative and postoperative LL and the mean difference between PI and the LL (PI–LL) between groups 1 and 2. Linear correlation and regression analysis showed that there was no correlation between JOA score and the coronal Cobb angle in degenerative scoliosis patients. However, we found a positive correlation between JOA and LL. Our series of long lumbar fusions had a high complication and instrumentation failure. Creating adequate LL angle in harmony with PI was a key to prevent surgical complications and attain neurological improvement.
Keywords: lumbar scoliosis, lumbar kyphosis, transforaminal lumbar interbody fusion, lumbar lordosis angle, pelvic incidence
Introduction
Long lumbar instrumented fusions have been described for various conditions, including degenerative lumbar scoliosis, adolescent idiopathic scoliosis, lumbar kyphosis, degenerative spondylolisthesis, and revision cases such as pseudarthoses.1–7) Spinal stabilization is often indicated in these circumstances as means of alleviating pain, preventing spinal instability, and avoiding progression of the deformity.8–10) The superiority of lumbar fusions with pedicle screw fixation in biomechanical properties, fusion rate, early mobilization, and versatility have been shown conclusively.11) However, the increasing number of patients treated with long lumbar fusions present to the surgeons with surgical failures.3,5,6) Such failures include proximal segment degeneration, screw failure in the upper or lower instrumented vertebra, vertebral compression fractures, and adjacent vertebral subluxations, as well as severe disc degeneration leading to junctional kyphosis.2,4,5) Many theories have been used to explain these high rates of failures. Fused lumbar segments may increase stress and motion at the adjacent unfused segments accelerating degeneration of these segments and/or inducing instrumentation failure.12,13) The importance of extending instrumentation adjacent to stable segments with normal alignment has been stressed.5,14) Other factors contributing to failures include increased age.1,11) osteopenia,1,11) preoperative comorbidites,12) thoracoplasty,15) male sex,15) preoperative kyphosis adjacent to the instrumented vertebra,15) rigid implant systems,16,17) preoperative hyperkyphotic thoracic alignment,12) postoperative sagittal imbalance,12) sagittal imbalance associated with hip and knee degeneration,1) acute corrections of sagittal malalignment,15) and technical problems of screw insertion.17)
We performed a retrospective analysis of the outcomes and instrumentation-related complications of long lumbar fusions with pedicle screw fixation exceeding three levels, which were performed for lumbar degenerative scoliosis, kyphosis, or both combined with spondylolisthesis. All cases were operated on by the same surgeon using a posterior-only approach with selective segmental transforaminal lumbar interbody fusion (TLIF). The aim of this study was to assess the outcomes and surgical complications of long lumbar fusions and to investigate risk factors associated with complications.
Materials and Methods
Following Research Ethics Board's approval, a retrospective review was performed on 15 consecutive patients who underwent long-segment lumbar instrumented fusions exceeding three levels from 2010 to 2012. All surgeries were performed by the senior author at our hospital or an affiliated hospital. Inclusion criteria consisted of patients who had a minimum of three lumbar segments of posterior lumbar instrumented fusions for adult degenerative scoliosis or lumbar degenerative kyphosis combined with spondylolis-thesis with proximal level of Th10 or distal, distal level of L5 or distal. Previous thoracic procedures proximal to the upper instrumented vertebra, prior lumbar or thoracic spine fusions, or spine trauma were excluded. Patients were included if they had undergone a decompressive lumbar procedure. All constructs were pedicle screw and rod systems that extended to or beyond the region of the main pathology. TLIF with a single interbody fusion cage at each level was carried out in the segments, which satisfied one or more of the following criteria: (1) segmental kyphosis, (2) significant vertebral translation in any orientation (> 5 mm), (3) segmental instability (sagittal translation > 3 mm or sagittal rotation > 15°) or intraoperative instability (bilateral facetectomy > 50% or unilateral total facetectomy), and (4) significant upper endplate obliquities of L3 or L4 on coronal plane (> 15°). TLIF with intervertebral cages was carried out in 4 segments in 4 cases, 3 segments in 7 cases, 2 segments in 3 cases, and 1 segment in 1 case. Multilevel Ponte osteotomies18) were used for reduction of kyphosis. Rod derotation technique and compression on the convex side with the rod carefully contoured to lordosis were carried out. Local bone autograft was used without using bone graft substitutes or extenders.
Clinical and radiographical data were collected by a spine surgeon who was not directly involved in the care or surgical treatment of the patients. Their age, sex, and body mass index (BMI) were measured. The number of previous spinal surgeries and total number of levels fused were also noted. A retrospective chart and radiographic review of all preoperative and postoperative imaging were performed by an independent reviewer who had nothing to do with either the initial surgery or aftercare of the patients. Patients were instructed to assume a free-standing posture, with elbows flexed and fingertips on the clavicles. Spinal measurements (Fig. 1) included coronal Cobb angle, lumbar lordosis (LL; saggital Cobb angle measured between the superior endplate of Th12 and the superior endplate of S1). Pelvic measurements (Fig. 2) included pelvic tilt (PT; angle between the vertical line and the line through the midpoint of the sacral plate to axis of femoral heads) and pelvic incidence (PI; angle between the perpendicular to the superior S1 endplate at its midpoint and the line connecting this point to the center of the femoral heads). The initial predischarge standing film was considered as the postoperative film. The clinical outcome was assessed using the Japanese Orthopedic Association (JOA) score. All patients were followed for a minimum of 16 months or until revision surgery.
Fig. 1.
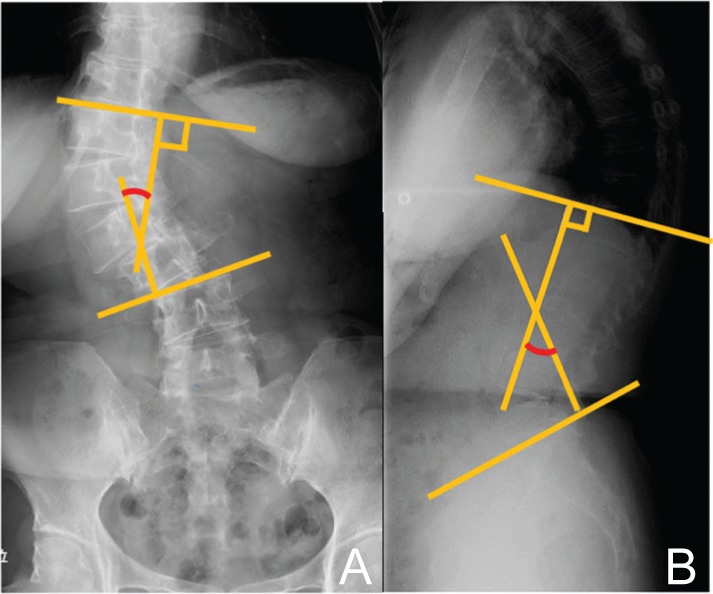
Diagram showing the measurement of coronal Cobb angle (A) and lumbar lordosis (LL) (B). LL was measured from Th12 to S1.
Fig. 2.
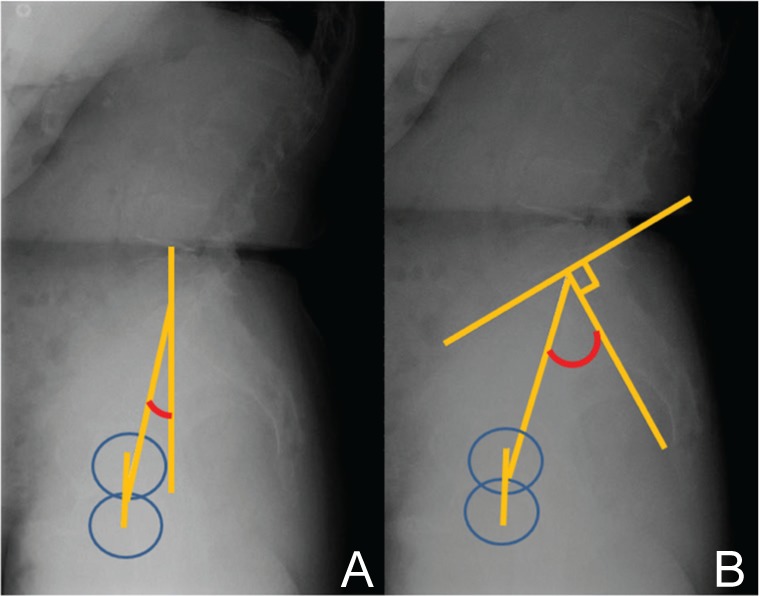
Diagram showing the measurement of pelvic tilt (PT) (A), and pelvic incidence (PI) (B). PT is defined as the angle subtended by a line drawn from the midpoint of the sacral endplate to the center of the bicoxofemoral axis and a vertical plumb line extended from the bicoxofemoral axis. PI is defined as the angle subtended by a line drawn between the center of the femoral head and the sacral endplate and a line drawn perpendicular to the center of the sacral endplate.
The patients were divided into two groups on the basis of outcome. Group 1 consisted of patients who sustained instrumentation-related complications postoperatively (Fig. 3). Group 2 consisted of patients who had no surgical complications (Fig. 4).
Fig. 3.
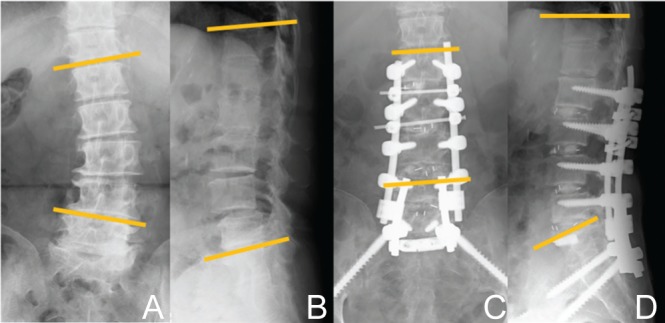
Radiographic studies obtained in a 74-year-old woman who complained of severe low back and radicular pain. A, B: Preoperative radiographs showing 21° of scoliosis (A) and 13° of LL (B) 30° of PT and 46° of PI. L2–S1 fusion was performed with transforaminal lumbar interbody fusion procedure of L2/3 to L5/S1. Nine months after surgery, the patient developed breakage of both S1 screws and underwent revision surgery for sacropelvic fixation using SAI screws and for removing broken S1 screws. C, D: Seven months after the second surgery, radiographs showing 2° of scoliosis (C) and 34° of LL angle and 18° of PT. The difference between PI and LL was improved from 33 to 12. LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SAI: sacral alar-iliac.
Fig. 4.
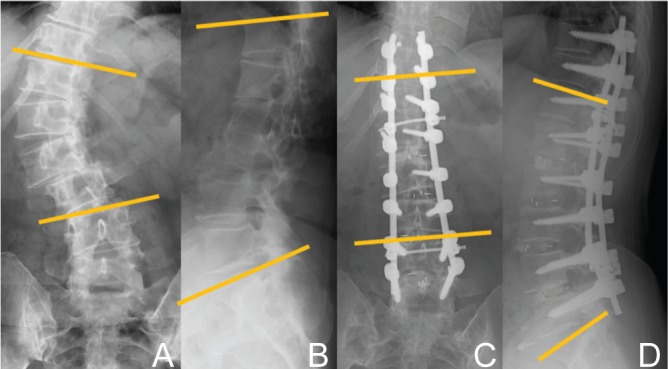
Radiographic studies obtained in a 65-year-old woman who complained of severe low back and radicular pain. A, B: Preoperative radiographs showing 49° of scoliosis (A), 26° of LL (B), 35° of PT, and 59° of PI. Th10–L5 fusion was performed with transforaminal lumbar interbody fusion procedure from L1/2 to L4/L5. C, D: Sixteen months postoperative radiographs showing 3° of scoliosis (C) and 49° of LL angle (D), and 21° of PT. The difference between PI and LL was improved from 33 to 10. LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt.
Statistical analysis
The statistical significance of observed differences was determined by t-tests and the relationship between the result of radiographic study and clinical outcome were analyzed with linear correlation and regression analysis (Stat View; SAS Institute, Cary, North Carolina, USA). All reported P-values are two-tailed; a value of P < 0.05 was considered statistically significant. Values are expressed as mean ± SE (standard error).
Results
I. Patient demographics
All patients underwent surgery for degenerative scoliosis, kyphosis, or both combined with spondylolisthesis (Table 1). In group 1 (Table 2), there were 4 patients with degenerative scoliosis, 3 with degenerative kyphosis with spondylisthesis. Surgical complications were detected on radio-graphic imaging 5.9 months after surgery on average (2–9 months). In group 2, there were 6 patients with degenerative scoliosis, 2 with degenerative kyphosis with spondylolisthesis. There were 4 men and 3 women in group 1 and 1 man and 6 women in group 2. There were no significant differences (P > 0.05) between the groups in mean age (71.4 years in group 1, 72.1 years in group 2), mean BMI (22.4 in group 1, 23.5 in group 2), levels fused [4.4 (3–6) in group 1, 4.3 (3–8) in group 2], the rate of levels with TLIF [71% (25–100) in group 1, 72% (50–100) in group 2] or number of previous spinal surgeries [0.4 (0–2) in group 1, 0.3 (0–1) in group 2]. The mean follow-up was calculated on the basis of the date of final follow-up or the date when patient underwent revision surgery. The mean length of follow-up was 16.9 (5–40) months for group 1 and 21.9 (14–33) months for group 2. All patients who were not revised had a minimum follow-up of 20 months in group 1 and 16 months in group 2. There were no systemic complications in both groups. All 7 patients in group 1 sustained screw cut-out (screw migration inside the vertebral body or out of the bone including screw back-out), screw loosening, or breakage of screws, vertebral compression fracture (Table 2).
Table 1.
Comparison of the clinical and radiological data between the study groups
| Complication (+) Group 1 n = 7 | Complication (−) Group 2 N = 8 | |
|---|---|---|
| Diagnosis | ||
| Degenerative scoliosis | 4 | 6 |
| Degenerative kyphosis | 3 | 2 |
| Age (yr), mean (range) | 71.4 (57–80) | 72.1 (65–77) |
| Sex | ||
| Male | 3 | 1 |
| Female | 4 | 7 |
| BMI-mean (range) | 22.4 (19.8–26.7) | 23.5 (20.7–30.2) |
| Number of previous spinal surgeries | 0.4 (0–2) | 0.3 (0–1) |
| Levels fused | 4.5 (3–6) | 4.3 (3–8) |
| Rate of number of levels with TLIF (%) | 71 (25–100) | 72 (50–100) |
| UIV | ||
| Th10 | 0 | 1 |
| Th11 | 0 | 1 |
| Th12 | 2 | 0 |
| L1 | 1 | 1 |
| L2 | 4 | 3 |
| L3 | 0 | 2 |
| LIV | ||
| L5 | 3 | 5 |
| S1 | 4 | 3 |
| Preoperative JOA, mean (range) | 13.1 (10–18) | 13.8 (10–19)† |
| Postoperative JOA, mean (range) | 13 (10–21)* | 20.6 (17–26)*,† |
| Revision surgery (post-index surgery) | n = 4 | n = 0 |
| Length of follow-up (mo)- mean (range) | 16.9 (5–40) | 21.6 (14–33) |
P < 0.05. BMI: body mass index, JOA: Japan Orthopedic Association, LIV: lower instrumented vertebra, TLIF: transforaminal lumbar interbody fusion, UIV: upper instrumented vertebra.
Table 2.
Cases with postoperative complications after thoracolumbar fusion for exceeding three levels
| Cases | Age | Sex | Pathology | Proximal fusion Levels | Distal fusion levels | Level fused | Number of segments with TLIF | Complications | Revision surgery |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 74 | F | DS | L2 | S1 | 4 | 4 (L2/3/4/5/S1) | Breakage of S1 screws | Pelvic fixation with SAI screws |
| Case 2 | 68 | M | DS | L2 | S1 | 4 | 4 (L2/3/4/5/S1) | Loosening of L2 Screws | Proximal extension up to Th10 and pelvic fixation |
| Case 3 | 57 | M | DS | Th12 | S1 | 6 | 3 (L2/3, L4/5/S1) | Loosening of S1 Screws | Pelvic fixation with SAI screws |
| Case 4 | 80 | F | DK with spondylolisthesis | Th12 | L5 | 6 | 3 (L1/2, 3/4/5) | Compression fracture of Th12 Body | (–) |
| Case 5 | 76 | M | DK with spondylolisthesis | L2 | S1 | 4 | 3 (L3/4/5/S1) | Loosening of L2 Screws | (–) |
| Case 6 | 73 | F | DS | L1 | L5 | 4 | 1 (L3/4) | Compression fracture of L1 Body | (–) |
| Case 7 | 72 | M | DK with spondylolisthesis | L2 | L5 | 3 | 3 (L2/3/4/5) | Loosening of L2 Screws | Proximal extension up to Th12 |
DK: degenerative kyphosis, DS: degenerative scoliosis, SAI: sacral alar-iliac, TLIF: transforaminal lumbar interbody fusion.
II. Effect of correction of coronal Cobb angle on surgical outcome
Lumbar coronal Cobb angle of degenerative scoliosis patients, 4 cases in group 1 and 6 cases in group 2, was compared before and after surgery (Tables 3, 4). The preoperative angle was approximately 22 ± 1.2° in group 1 and 30.5 ± 4.5° in group 2. The postoperative angle was 7.3 ± 2.6° in group 1 and 6.8 ± 1.7° in group 2. This difference was not significant between group 1 and group 2, both before (P = 0.17) and after (P = 0.30) surgery (Table 4), although in both groups, preoperative curve was significantly corrected after surgery (P < 0.05) (Table 3).
Table 3.
Comparison of measurements between preoperative and immediate postoperative values of coronal Cobb angle, LL, PI, PT, and PI–LL in each group
| Group 1 | |||||
| Coronal Cobb angle | LL | PI | PT | PI–LL | |
| Preoperative | 22 ± 1.2 | 19 ± 5.4 | 52.3 ± 4.9 | 30.1 ± 2.3 | 33.3 ± 2.7 |
| Postoperative | 7.3 ± 2.6* | 25.1 ± 3.8* | N.A. | 29.1 ± 4.3 | 27.1 ± 3.6* |
| Group 2 | |||||
| Coronal Cobb angle | LL | PI | PT | PI–LL | |
| Preoperative | 30.5 ± 4.5 | 34.3 ± 4.0 | 56.5 ± 2.1 | 26.3 ± 3.7 | 22.5 ± 4.0 |
| Postoperative | 6.8 ± 1.7* | 48.5 ± 3.0* | N.A. | 20.5 ± 2.9* | 9.8 ± 1.7* |
P < 0.05. LL: lumbar lordosis angle, N.A.: not applicable, PI: pelvic incidence, PT: pelvic tilt.
Table 4.
Comparison of measurements of coronal Cobb angle, LL, PI, PT, and PI–LL between group 1 and group 2 in preoperative and postoperative state
| Preoperative | |||||
| Coronal Cobb angle | LL | PI | PT | PI–LL | |
| Group 1 | 22 ± 1.2 | 19 ± 5.4 | 52.3 ± 4.9 | 30.1 ± 2.3 | 33.3 ± 2.7 |
| Group 2 | 30.5 ± 4.5 | 34.3 ± 4.0* | 56.5 ± 2.1 | 26.3 ± 3.7 | 22.5 ± 4.0* |
| Postoperative | |||||
| Coronal Cobb angle | LL | PI | PT | PI–LL | |
| Group 1 | 7.3 ± 2.6 | 25.1 ± 3.8 | N.A. | 29.1 ± 4.3 | 27.1 ± 3.6 |
| Group 2 | 6.8 ± 1.7 | 48.5 ± 3.0* | N.A. | 20.5 ± 2.9 | 9.8 ± 1.7* |
P < 0.05. LL: lumbar lordosis, N.A.: not applicable, PI: pelvic incidence, PT: pelvic tilt.
III. Effect of LL angle on surgical outcome
The LL highly correlated with developing surgical complications. Preoperative LL was 19 ± 5.4° in group 1, 34.3 ± 4.0° in group 2 and preoperative PT was 30.1 ± 2.3° in group 1, 26.3 ± 3.7° in group 2. The mean preoperative difference between the PI and the LL (PI–LL) was 33.3 ± 2.7° in group 1, 22.5 ± 4.0° in group 2. The postoperative LL was 25.1 ± 3.8° in group 1, 48.5 ± 3.0° in group 2. Postoperative PT was 29.1 ± 4.3° in group 1, 20.5 ± 2.9° in group 2. The postoperative PI–LL was 27.1 ± 3.6° in group 1, 9.8 ± 1.7° in group 2. There were statistically significant differences in preoperative and postoperative LL and PI–LL between group 1 and 2 (Table 4). There were no differences in preoperative and postoperative PT between two groups (Table 4). Coronal Cobb angle and LL were significantly corrected postoperatively in both groups 1 and 2 respectively (Table 3). PT in group 2 also significantly improved after surgery (Table 3).
IV. Effect of choice of upper or lower instrumented level
Constructs with upper instrumented vertebra (UIV) of Th10, Th11, or Th12 developed proximal failures in 25% of cases (1 of 4) compared to 44% (5 of 11) of constructs with UIV of L1 or L2 or L3. The lower instrumented level was L5 in 8 patients, S1 in 7 patients. S1 screws loosening occurred in 2 cases, and no screw loosening was found in L5 screws.
V. Effect of TLIF
In this series, the number of levels with TLIF did not correlate with the onset of surgical complications. There was no significant difference between group 1 and 2 in terms of the number of TLIF. Furthermore, 4 out of 5 cases with screw loosening or breakage had undergone TLIF at the affected segments. Only 1 case with the top screws loosening had no TLIF at the affected level.
VI. Clinical outcome
The two groups were similar with regard to the mean preoperative JOA score (13.1 and 13.8 for groups 1 and 2, respectively). However, the difference of postoperative JOA score (13 and 20.6 for groups 1 and 2, respectively) was significant. The difference between the preoperative and postoperative JOA was significant in group 2. Linear correlation and regression analysis showed that there was no correlation between the increase of JOA score and the correction of the coronal Cobb angle (r = 0.381, P = 0.277) in degenerative scoliosis patients. However, across the whole study population, we found a positive correlation between the increase of JOA and correction of LL (r = 0.52, P < 0.05).
Discussion
In this study, we found that patients undergoing three or more levels of lumbar fusions with scoliosis and/or kyphosis combined with spondylolisthesis had an increased risk of surgical complications. These complications occurred after 5.9 months on average. We think that the LL is an important preoperative consideration in determining how much correction should be done and how many levels should be fused.
We identified the trend that the choice of UIV level influenced the overall rate of proximal failure in line with previous reports.1,13,19) Swank et al.13) observed that only 2 of 20 patients requiring revision surgery after receiving a long lumbar fusion to L1 or L2 had good or excellent clinical results. As well, Lewis et al.1) described lower proximal complications rate of 31% for fusions extending up to Th10–Th12 compared with proximal failure rate of 73% in fusions up to L1 or L2. They also emphasize that most proximal screws should be put on horizontally-oriented vertebra in sagittal section. Extension of fusions up to thoracic levels could provide more stable construct, however, all cases do not have to be fused up to thoracic levels. As claimed by Shufflebarger et al., we find it reasonable to choose the uppermost vertebra based on targeted LL and sagittal balance with fewest number of segments fused.5)
Lumbosacral pseudarthrosis is likely to come up as S1 screw loosening, as seen in this study.14,19,20) Weistroffer et al. suggest that a combination of both iliac fixation in addition to sacral fixation gives the most secure distal fixation.14) We suggest that sacral screws should be enhanced by using iliac fixation as well as L5/S1 TLIF since this study is showing two cases of S1 screw failures in spite of L5/S1 TLIF. However, iliac screws seem to be a problem of this implant sometimes becoming symptomatic. Instead, S2 sacral alar-iliac (SAI) screws, which have previously been reported as an interesting alternative to classic iliac wing screws, could be used in the initial surgery or as a salvage technique for lumbosacropelvic instability.20) According to the reported experience, this technique provides a biomechanically robust construct for definitive pelvic fixation during revision surgeries in the challenging scenarios of pseudarthrosis and instability of the lumbosacropelvic region.20)
We noted a high surgical complication rate of long fusion for degenerative scoliosis or kyphosis in our series of 46.7% (7 of 15), which were consistent with those reported in 2007 by Cho et al. (2008)19) (48.9%), by Weistroffer et al. (2012)14) (50%), by Lewis et al. (2012)1) (51.9%), and by Burneikiene et al. (2012)21) (66%). We attribute the high failure rate to a multitude of factors. The most important is related to sagittal balance as previously reported.22–25) First, patients in group 1 have more significant kyphotic deformity than group 2 preoperatively (LL; 19 ± 5.4° in group 1, 34.3 ± 4.0° in group 2). Second, we failed to create adequate LL in harmony with PI in group 1. PI is a morphological pelvic parameter that remains consistent during a patient's lifetime, with slight changes occurring during prepubertal development. Following puberty, PI is generally considered to be a fixed morphological parameter, reflecting the relationship of the sacrum to the pelvis.26) Numerous studies have led to the recognition that the pelvic morphology is an essential component of standing spinal alignment.25) Regional values are insufficient in assessing patient-specific harmonious alignment. Therefore, a ground rule of harmonious alignment consists of a LL proportional to PI. In light of this, each subject would require appropriate LL that measured within 10° of the measured PI.1,22,23,25,26) The PI–LL was well above this value in group 1 pre- and postoperatively, measuring 33.3 ± 2.7° and 27.1 ± 3.6° respectively. In contrast, group 2 had better balance pre- and postoperatively with a PI–LL of 22.5 ± 4.0° and 9.8 ± 1.7° respectively. This implicates the low LL relative to PI accounts for the high instrumentation failure rate in this series. Treatment goal should be adapted to a given individual on the basis of their respective realignment needs. The relationship between the result of radiographic study and clinical outcome was analyzed with linear correlation and regression analysis. This showed that there was a positive correlation between the increase in JOA score and the increase in the LL angle (r = 0.523, P < 0.05), which was consistent with earlier studies.25,26) However, no clear relationship between coronal Cobb angle and JOA scores (r = 0.381, P = 0.277) was detected. From these findings, the restoration of the LL angle should be much emphasized on in the surgical procedure.
Other factors contributing to the high failure rate are involving surgical technique, which include inadequate osteotomy, use of single TLIF cage at each level, high reliance on local bone graft. The great outcome of extreme lateral interbody fusion (XLIF) with low complication rate (21%)27) indicates importance of robust anterior support, adequate anterior release, and significant restoration of disc height. Given these facts, posterior-only approach would require the following techniques to achieve solid fusion and appropriate restoration of LL leading to low complication rate: (1) more aggressive osteotomy with thorough release of the posterior and anterior structure should be adopted because hyperplasia of the articular process and osteophyte bridging neighboring vertebral body could prevent the adequate restoration of LL,28) (2) for those patients with severe segmental kyphosis, multisegmental TLIF technique should be applied with two interbody cages put in the anterior part of the intervertebral disc space. The lordosis angle of the TLIF segment could be increased by 5°,29) (3) the placement of wedge-shaped cages could produce better lordosis than cylinder-shaped cages,30) and (4) more amount of bone graft than harvested as local bone has to be placed.
Like other studies, this series is limited by the small numbers. Nevertheless, we think that our conclusions related to fusion levels, sagittal imbalance, and surgical procedures are significant findings. A multicenter setting based on this study results may help further validate these findings and other findings in this study to provide surgeons with a better understanding in choosing appropriate surgical strategies for their patients with degenerative lumbar conditions.
Conclusion
Our series of long lumbar fusions had a high surgical complications and revision rate. Under correction of the sagittal balance in this series may have contributed to most of the poor outcomes and we may have to extend the fusion until thoracic level to attain the satisfactory lordosis. This study also showed that there was a positive correlation between the increase in JOA score and the increase in the LL angle, which was consistent with earlier studies. On the basis of the findings of this study, we recommend that long lumbar fusion should be performed long enough to achieve an adequate LL properly proportional to PI.
References
- 1). Lewis SJ, Abbas H, Chua S, Bacon S, Bronstein Y, Goldstein S, Magana S, Sullivan K, Dold AP, Bodrogi A: Upper instrumented vertebral fractures in long lumbar fusions: what are the associated risk factors? Spine 37: 1407– 1414, 2012. [DOI] [PubMed] [Google Scholar]
- 2). Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M: Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine 35: 138– 145, 2010. [DOI] [PubMed] [Google Scholar]
- 3). Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW: Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine 32: 2653– 2661, 2007. [DOI] [PubMed] [Google Scholar]
- 4). Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C: Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine 30: 1643– 1649, 2005. [DOI] [PubMed] [Google Scholar]
- 5). Shufflebarger H, Suk SI, Mardjetko S: Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine 31: S185– S194, 2006. [DOI] [PubMed] [Google Scholar]
- 6). Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G: An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine 31: 2343– 2352, 2006. [DOI] [PubMed] [Google Scholar]
- 7). Helgeson MD, Shah SA, Newton PO, Clements DH, Betz RR, Marks MC, Bastrom T, Harms Study Group : evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 35: 177– 181, 2010. [DOI] [PubMed] [Google Scholar]
- 8). Frazier DD, Lipson SJ, Fossel AH, Katz JN: Associations between spinal deformity and outcomes after decompression for spinal stenosis. Spine 22: 2025– 2029, 1997. [DOI] [PubMed] [Google Scholar]
- 9). Katz JN, Lipson SJ, Lew RA, Grobler LJ, Weinstein JN, Brick GW, Fossel AH, Liang MH: Lumbar laminectomy alone or with instrumented or noninstrumented arthrodesis in degenerative lumbar spinal stenosis. Patient selection, costs, and surgical outcomes. Spine 22: 1123– 1131, 1997. [DOI] [PubMed] [Google Scholar]
- 10). Serhan HA, Varnavas G, Dooris AP, Patwadhan A, Tzermiadianos M: Biomechanics of the posterior lumbar articulating elements. Neurosurg Focus 22: E1, 2007. [DOI] [PubMed] [Google Scholar]
- 11). Heim SE: Transpedicle instrumentation in the degenerative spine. Clin Orthop Relat Res 97– 110, 1997. [DOI] [PubMed] [Google Scholar]
- 12). Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G: Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine 31: 2359– 2366, 2006. [DOI] [PubMed] [Google Scholar]
- 13). Swank S, Lonstein JE, Moe JH, Winter RB, Bradford DS: Surgical treatment of adult scoliosis. A review of two hundred and twenty-two cases. J Bone Joint Surg Am 63: 268– 287, 1981. [PubMed] [Google Scholar]
- 14). Weistroffer JK, Perra JH, Lonstein JE, Schwender JD, Garvey TA, Transfeldt EE, Ogilvie JW, Denis F, Winter RB, Wroblewski JM: Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine 33: 1478– 1483, 2008. [DOI] [PubMed] [Google Scholar]
- 15). Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J: Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine 32: 2731– 2738, 2007. [DOI] [PubMed] [Google Scholar]
- 16). Gaines RW: The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 82-A: 1458– 1476, 2000. [DOI] [PubMed] [Google Scholar]
- 17). Pihlajämaki H, Myllynen P, Böstman O: Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Joint Surg Br 79: 183– 189, 1997. [DOI] [PubMed] [Google Scholar]
- 18). Geck MJ, Macagno A, Ponte A, Shufflebarger HL: The Ponte procedure: posterior only treatment of Scheuermann's kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech 20: 586– 593, 2007. [DOI] [PubMed] [Google Scholar]
- 19). Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, Lee KY, Lee SR: Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine 32: 2232– 2237, 2007. [DOI] [PubMed] [Google Scholar]
- 20). Mattei TA, Fassett DR: Combined S-1 and S-2 sacral alar-iliac screws as a salvage technique for pelvic fixation after pseudarthrosis and lumbosacropelvic instability: combined S-1 and S-2 sacral alar-iliac screws as a salvage technique for pelvic fixation after pseudarthrosis and lumbosacropelvic instability: technical note. J Neurosurg Spine 19: 321– 330, 2013. [DOI] [PubMed] [Google Scholar]
- 21). Burneikiene S, Nelson EL, Mason A, Rajpal S, Serxner B, Villavicencio AT: Complications in patients undergoing combined transforaminal lumbar interbody fusion and posterior instrumentation with deformity correction for degenerative scoliosis and spinal stenosis. Surg Neurol Int 3: 25, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22). Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V: Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine 37: 1077– 1082, 2012. [DOI] [PubMed] [Google Scholar]
- 23). Schwab F, Patel A, Ungar B, Farcy JP, Lafage V: Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35: 2224– 2231, 2010. [DOI] [PubMed] [Google Scholar]
- 24). Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V, Lafage V, Schwab F, Shaffrey CI: Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine 16: 547– 564, 2012. [DOI] [PubMed] [Google Scholar]
- 25). Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR: Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30: 682– 688, 2005. [DOI] [PubMed] [Google Scholar]
- 26). Hasegawa K, Homma T: One-stage three-dimensional correction and fusion: a multilevel posterior lumbar interbody fusion procedure for degenerative lumbar kyphoscoliosis. Technical note. J Neurosurg 99: 125– 131, 2003. [DOI] [PubMed] [Google Scholar]
- 27). Phillips FM, Isaacs RE, Rodgers WB, Khajavi K, Tohmeh AG, Deviren V, Peterson MD, Hyde J, Kurd M: Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine 38: 1853– 1861, 2013. [DOI] [PubMed] [Google Scholar]
- 28). Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, Kostuik JP: Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: a radiographic analysis. Spine 32: 1551– 1554, 2007. [DOI] [PubMed] [Google Scholar]
- 29). Li F, Chen Q, Chen W, Xu K, Wu Q: Posterior-only approach with selective segmental TLIF for degenerative lumbar scoliosis. J Spinal Disord Tech 24: 308– 312, 2011. [DOI] [PubMed] [Google Scholar]
- 30). Goldstein JA, Macenski MJ, Griffith SL, McAfee PC: Lumbar sagittal alignment after fusion with a threaded interbody cage. Spine 26: 1137– 1142, 2001. [DOI] [PubMed] [Google Scholar]


