Abstract
Marfan syndrome can demonstrate tortuous and elongated intracranial arteries. However, these arteries rarely cause neurovascular compression resulting in hemifacial spasm or trigeminal neuralgia. The authors report a 33-year-old woman who was diagnosed as Marfan syndrome, suffered from trigeminal neuralgia. Magnetic resonance (MR) angiography showed tortuous and elongated left vertebral artery (VA). The coronal section of three dimensional (3D) MR cisternography with contrast enhancement showed that the left trigeminal nerve was compressed from underneath by the tortuous and elongated left VA. After successful surgery of microvascular decompression, the patient’s symptom resolved and no recurrence was encountered. Neurosurgeons should not only be aware of hemifacial spasm but also of trigeminal neuralgia caused by elongated vessels in a patient with Marfan syndrome, although it is an extremely rare condition. In addition, offending vessel is not atherosclerotic in younger patients unlike usual cases of trigeminal neuralgia. Thus, microvascular decompression can be easier than usual cases. Care should be taken to prevent arterial dissection during transposition by using some technical tips.
Keywords: Marfan syndrome, trigeminal neuralgia, vertebral artery, microvascular decompression
Introduction
Marfan syndrome is a multisystem connective tissue disorder usually associated with mutation in fibrillin, and occasionally with mutation in transforming growth factor-beta receptor (TGFBR) 1 or 2.1) Its signs and symptoms are mainly skeletal and joint abnormalities, ocular signs, and symptoms such as ectopia lentis and cardiovascular system abnormalities.2) In addition, patients with Marfan syndrome can demonstrate tortuous and elongated intracranial arteries which may be related to dissection of the internal carotid artery3) or to intracranial giant aneurysms.4,5) Although these tortuous and elongated intracranial vessels can theoretically cause neurovascular compression resulting in hemifacial spasm or trigeminal neuralgia, only two cases of hemifacial spasm,5,6) and no case of trigeminal neuralgia have been reported so far. Here we report the first case of trigeminal neuralgia associated with a Marfan syndrome.
Case Report
A 33-year-old woman, who was diagnosed as Marfan syndrome at the age of three, had bilateral lens subluxation since she was 3 years old and aortic dissection since 18 years old. Further, she had mild dilation of aortic valve and mild aortic regurgitation, which were conservatively observed. In June 2010, she complained neuralgic pain on her left back teeth and cheek during meal, teeth brushing, and talking. Temporarily, her symptoms diminished in 1 month with medication of 400 mg/day of carbamazepine. However, her symptoms did not improve further even with medication of maximal dose of carbamazepine. In 4 months, she complained of numbness and pain in her left lip. She was diagnosed as having trigeminal neuralgia and was referred to our department for treatment.
Physical examination revealed visual disturbance due to lens dislocation and neuralgia in the left V2 area leading to left lip numbness. Three dimensionally reconstructed (3D) MR angiography showed tortuous and elongated left vertebral artery (VA) (Fig. 1). The coronal section of 3D-T2-driven equilibrium radio frequency reset pulse (DRIVE), axial, and coronal 3D-MR cisternography with contrast enhancement showed that the left trigeminal nerve was compressed from underneath by the tortuous and elongated left VA (Figs. 2, 3A, B).
Fig. 1.
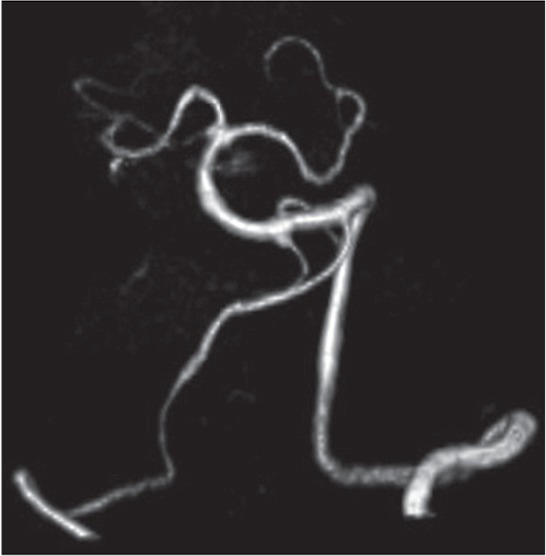
Three-dimensional reconstructed magnetic resonance (MR) angiography showing the tortuous and elongated left vertebral artery.
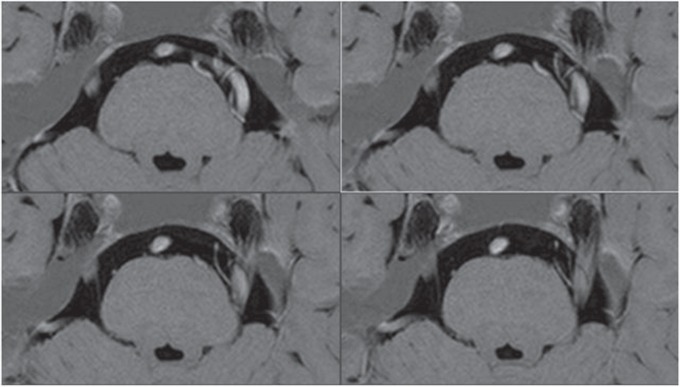
Fig. 2.
Axial three dimensionally reconstructed magnetic resonance (3D-MR) cisternography with contrast enhancement shows that the left trigeminal nerve was compressed from underneath by the tortuous and elongated left vertebral artery.
Fig. 3.
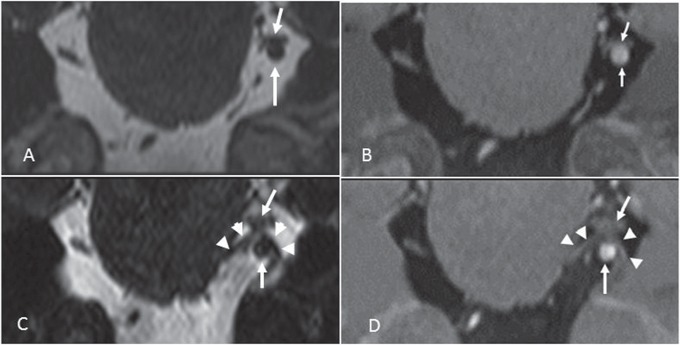
The pre- (A) and postoperative (C) coronal section of 3D-T2-driven equilibrium radio frequency reset pulse (DRIVE) and pre- (B) and postoperative (D) coronal section of 3D-MR cisternography with contrast enhancement show the successful transposition of the left vertebral artery away from the left trigeminal nerve. Upper arrow: left trigeminal nerve, lower arrow: left vertebral artery, arrow head: Teflon® sheet (Fluoro-Plastics, Inc., Philadelphia, Pennsylvania, USA).
A microvascular decompression was performed following a left retrosigmoid craniotomy. At first, the petrosal fissure was sharply opened to obtain wide operative view and working space. The trigeminal nerve was directly compressed by the left tortuous VA (Fig. 4A). The left VA was exposed and completely dissected from the left trigeminal nerve. Based on the intraoperative findings, wall of the left VA was rather soft and not arteriosclerotic, thus, VA was able to be moved easily with a suction or microdissection (Fig. 4B). Prior to the transposition of the VA, a small piece of Teflon sheet was inserted between VA and pons proximal to the vessel-nerve conflict site, so that the entire left VA was moved away from the trigeminal nerve; it is an useful technique to diverse the pressure from VA to the prosthesis and to prevent the rebound of the tortuous VA (Fig. 4C, D). Then the VA was transposed to the caudal side with a wider Teflon sling covering cranial side of the artery. In this procedure, we used a wide Teflon sling, which enabled to diverse the pressure to the arterial wall during the transposition preventing arterial dissection (Fig. 4E). Then the Teflon sling was fixed to the petrous bone and pons with fibrin glue (Fig. 4F). Postoperative course was uneventful, and her trigeminal neuralgia disappeared soon after the operation. MR images at 3 months after the operation showed that the left VA was separated from the trigeminal nerve (Fig. 3C, D). Up to a 2-year follow-up period, no recurrence was encountered.
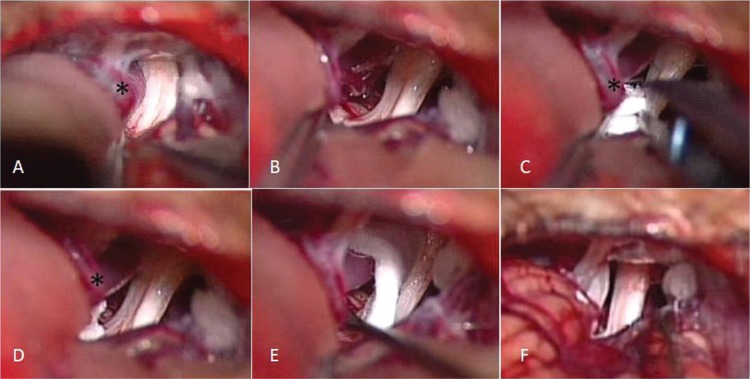
Fig. 4.
Intraoperative images. A: The trigeminal nerve was directly compressed by the left tortuous vertebral artery (VA). B: The VA was able to be easily moved with a suction because the wall of the left VA was rather soft and not arteriosclerotic. C, D: Prior to the transposition of the VA, a small piece of Teflon sheet were inserted between VA and pons proximal to the vessel-nerve conflict site, so that the entire left VA is moved away from the trigeminal nerve to diverse the pressure from VA to the prosthesis and to prevent the rebound of the tortuous VA. The VA was transposed to the caudal side with Teflon sling covering cranial side of the artery. E: In this procedure, we used a wide Teflon sling, which enable to diverse the pressure to the arterial wall during the transposition. The Teflon sling was fixed to the petrous bone and pons with fibrin glue. F: The trigeminal nerve is free from the Teflon sling and vertebral artery. asterisk: left vertebral artery.
Discussion
Marfan syndrome is a variable, autosomal-dominant disorder of connective tissue whose cardinal features affect the cardiovascular system, eyes, and skeleton.1) The estimated incidence of Marfan syndrome ranges from 1 in 5000 to 1 in 10,000 persons.6) The defect itself has been isolated to the fibrillin (FBN) 1 gene on chromosome 15, which codes for fibrillin, a glycoprotein that is a major structural component of microfibrils. Microfibrils are important components of elastic tissues, including the walls of arteries.7)
Clinically, the most prominent abnormalities are found in the skeleton, the eye, and the cardiovascular system. The typical clinical picture is easily recognized in patients with long, thin extremities, arachnodactyly, hyperextensible joints, chest deformity, dislocated lenses, and evidence of aortic dilatation.8) This syndrome is most often diagnosed clinically, but chromosome analysis is used in less clinically apparent cases. In addition to aortic dissection, other vascular problems including VA dissections3) and pulmonary artery aneurysms9) have been described in Marfan syndrome.6) Further, a link between Marfan syndrome and a cerebral aneurysm is well documented,6,10) and a case of elongation and tortuosity of the basilar artery and the VA has been described.2) To date, two cases of hemifacial spasm associated with Marfan syndrome have been reported, but no case of trigeminal neuralgia with Marfan syndrome is reported. Three cases of neurovascular syndrome with Marfan syndrome are listed in Table 1.5,6) All three patients were young. In all the patients, cerebral angiography or MR angiography showed tortuous and ectatic VA, which caused the neurovascular compression. All patients were successfully treated with microvascular decompression. Trigeminal neuralgia is usually caused by demyelination of trigeminal sensory fibers within either the nerve root or the brainstem. In most cases, the trigeminal nerve root demyelination involves the proximal, central nervous system (CNS) part of the root and results from compression by an overlying artery or vein.11) In the present case, numbness emerged possibly due to severe compression of the trigeminal nerve by the left VA; similar mechanism of the symptoms are seen in some cases of meningiomas or vestibular schwannomas.12,13) In terms of offending vessel(s) of trigeminal neuralgia, a superior cerebellar artery or in association with other vessel(s) was found in 88% of 560 patients, an anterior–inferior cerebellar artery (alone or in association) in 25.1%, a vein embedded in the nerve (alone or in association) in 27.6%, and the basilar artery (alone or in association) in 3.5%.14) On the other hand, VA rarely elicited trigeminal neuralgia; the incidence reported to be only from 0.3% (4 of 1404 cases)15) to 2% (19 of 1204 cases).16) Yang et al. reported 6 cases of trigeminal neuralgia caused by ectatic VA and in association with other vessels.17) According to their report, the patient’s ages were 67, 77, 57, 58, 70, and 47 and the ectasia of VA seemed to be the consequence of arteriosclerosis, unlike our present case. During microvascular decompression surgery, they recommended several technical tips to prevent the rebound of the ectatic vertebrobasilar artery; one of the tips is separating the entire vertebrobasilar artery from pons by inserting Teflon sheets; this technique is useful for this difficult situation, and we also used this technique in the present case. In addition, we used wider Teflon sling as usual to diverse the pressure to the wall of the VA, so that we could prevent a dissection of the vessel wall of the VA.
Table 1.
Reported cases of vascular compression syndrome associated with Marfan syndrome
| Authors/year | Age (yrs)/sex | Symptoms | Offending artery | Treatment | Complication | Outcome | Recurrence |
|---|---|---|---|---|---|---|---|
| Nagatani et al. (1998)5) | 24, F | HFS | AICA and VA | MVD | No | Symptom resolved | No |
| Braca et al. (2005)6) | 39, M | HFS | PICA and VA | MVD | Minor pulmonary embolism | Symptom resolved | No |
| Present case | 33, F | TN | VA | MVD | No | Symptom resolved | No |
AICA: anterior inferior cerebellar artery, F: female, HFS: hemifacial spasm; M: male, MVD: microvascular decompression, PICA: posterior inferior cerebellar artery, TN: trigeminal neuralgia, VA: vertebral artery.
Neurosurgeons should be aware of trigeminal neuralgia in a patient with Marfan syndrome. Although it is a rare condition, elongated and tortuous VA can cause not only hemifacial spasm but also trigeminal neuralgia. In addition, offending vessel is not atherosclerotic in younger patients unlike usual cases of trigeminal neuralgia, thus, microvascular decompression can be easier than usual cases. Care should be taken to prevent arterial dissection during transposition by using some technical tips as we showed.
Conclusion
We reported the first case of trigeminal neuralgia with Marfan syndrome. Elongated and tortuous VA in a patient with Marfan syndrome can cause not only hemifacial spasm but also trigeminal neuralgia. Microvascular decompression is an effective treatment of choice, and can be easier than usual cases due to the absence of arteriosclerosis. However, tortuous VA should be carefully dealt using some technical tips to avoid arterial dissection.
References
- 1). Dean JC: Marfan syndrome: clinical diagnosis and management. Eur J Hum Genet 15: 724– 733, 2007. [DOI] [PubMed] [Google Scholar]
- 2). Kondo M, Itoh S, Nagano K, Namba M, Kondo M, Imai T, Onishi S: A 10-year-old boy with Marfan syndrome exhibiting cerebrovascular abnormalities. Brain Dev 23: 251– 254, 2001. [DOI] [PubMed] [Google Scholar]
- 3). Maski KP, Sengupta S, Silvera M, Rivkin MJ: Intracranial artery dissection in an adolescent with Marfan syndrome. Pediatr Neurol 45: 39– 41, 2011. [DOI] [PubMed] [Google Scholar]
- 4). Hainsworth PJ, Mendelow AD: Giant intracranial aneurysm associated with Marfan's syndrome: a case report. J Neurol Neurosurg Psychiatry 54: 471– 472, 1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Nagatani T, Inao S, Yoshida J: Hemifacial spasm associated with Marfan's syndrome: a case report. Neurosurg Rev 21: 152– 154, 1998. [DOI] [PubMed] [Google Scholar]
- 6). Braca J, Hornyak M, Murali R: Hemifacial spasm in a patient with Marfan syndrome and Chiari I malformation. Case report. J Neurosurg 103: 552– 554, 2005. [DOI] [PubMed] [Google Scholar]
- 7). Collod-Béroud G, Boileau C: Marfan syndrome in the third millennium. Eur J Hum Genet 10: 673– 681, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Murdoch JL, Walker BA, Halpern BL, Kuzma JW, McKusick VA: Life expectancy and causes of death in the Marfan syndrome. N Engl J Med 286: 804– 808, 1972. [DOI] [PubMed] [Google Scholar]
- 9). Ting P, Jugdutt BI, Le Tan J: Large pulmonary artery aneurysm associated with Marfan syndrome. Int J Angiol 19: e48– 50, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). van den Berg JS, Limburg M, Hennekam RC: Is Marfan syndrome associated with symptomatic intracranial aneurysms? Stroke 27: 10– 12, 1996. [DOI] [PubMed] [Google Scholar]
- 11). Love S, Coakham HB: Trigeminal neuralgia: pathology and pathogenesis. Brain 124: 2347– 2360, 2001. [DOI] [PubMed] [Google Scholar]
- 12). Matthies C, Samii M: Management of 1000 vestibular schwannomas (acoustic neuromas): clinical presentation. Neurosurgery 40: 1– 9; discussion 9–10, 1997. [DOI] [PubMed] [Google Scholar]
- 13). Schaller B, Merlo A, Gratzl O, Probst R: Premeatal and retromeatal cerebellopontine angle meningioma. Two distinct clinical entities. Acta Neurochir (Wien) 141: 465– 471, 1999. [DOI] [PubMed] [Google Scholar]
- 14). Sindou M, Howeidy T, Acevedo G: Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict). Prospective study in a series of 579 patients. Acta Neurochir (Wien) 144: 1– 12; discussion 12–13, 2002. [DOI] [PubMed] [Google Scholar]
- 15). Linskey ME, Jho HD, Jannetta PJ: Microvascular decompression for trigeminal neuralgia caused by vertebrobasilar compression. J Neurosurg 81: 1– 9, 1994. [DOI] [PubMed] [Google Scholar]
- 16). Barker FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD: The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334: 1077– 1083, 1996. [DOI] [PubMed] [Google Scholar]
- 17). Yang XS, Li ST, Zhong J, Zhu J, Du Q, Zhou QM, Jiao W, Guan HX: Microvascular decompression on patients with trigeminal neuralgia caused by ectatic vertebrobasilar artery complex: technique notes. Acta Neurochir (Wien) 154: 793– 797; discussion 797, 2012. [DOI] [PubMed] [Google Scholar]