Abstract
We describe a higher magnifying power operating microscope system to improve one method of high-quality microsurgical clipping for cerebral aneurysm in some cases. This higher magnification is achieved by a new lens design in the optical system, which makes the image of the object very clear at high magnifications (distinctiveness of 7 μm). This higher-resolution operating microscope system provides the surgeon with higher-magnified images (at the maximum of more than 30× magnifications as each working distance) in the operating field. The magnifications can be changed from low power (2.9×) to high power (62.0×) depending on the circumstances in a given procedure. We have used this operating microscope system on 11 patients with microsurgical clipping for cerebral aneurysms. Microsurgical treatment could be performed safely and precisely. All aneurysms were treated without any technical complications. We think that the use of this microscope would have potential benefits for microsurgical treatment for cerebral aneurysms because of better visualization.
Keywords: cerebral aneurysm, microsurgery, operating microscope, higher magnification
Introduction
Since the results of The International Subarachnoid Aneurysm Trial study were reported, endovascular procedure has been widely indicated to treat cerebral aneurysms.1,2) However, clipping surgery still occupies an important position to treat them. Especially, high-quality microsurgical procedures are more important to treat them with low surgical morbidity than before.3) Recent developments of microsurgical technology may support it. Thus, appropriate observations and precise manipulations under the operating microscope are of paramount importance in microsurgery. To achieve this purpose, we have recently developed a new surgical microscope with more than 30× magnifications and reported its extraordinary usefulness during microvascular anastomosis.4,5)
Here we described our experience of the use of the higher-magnification microscope system in treating cerebral aneurysms.
Patients and Methods
We treated totally 278 cerebral aneurysms at our hospital between November 2007 and August 2011. The treatment option used at our hospital was determined based on discussions by both microsurgical and endovascular neurosurgeons. As a result, 153 aneurysms were clipped through craniotomy. Of these, a higher-magnification operating microscope was employed to treat 11 (7.2%) aneurysms. There were five males and six females. Their mean age was 65.4 years, ranging from 57 to 71 years. Two were ruptured aneurysms and nine were nonruptured. The location of aneurysms included the middle cerebral artery (MCA) in seven cases, the internal carotid artery in one, the anterior communicating artery (AComA) in two, and the posterior inferior cerebellar artery in one. Their clinical characteristics are summarized in Table 1.
Table 1.
Clinical characteristics of 11 patients
| Case no. | Age (years) | Sex | Diagnosis | Approach | Complication |
|---|---|---|---|---|---|
| 1 | 68 | M | Rt MCA AN | Rt pterional | None |
| 2 | 65 | M | AComA AN | Interhemispheric | None |
| 3 | 70 | F | Rt distal PICA AN (SAH) | Midline suboccipital | None |
| 4 | 57 | F | Lt MCA AN | Lt pterional | None |
| 5 | 71 | F | Lt IC-PC AN | Lt pterional | None |
| 6 | 62 | M | Lt MCA AN | Lt pterional | None |
| 7 | 70 | M | Rt MCA AN | Rt pterional | None |
| 8 | 57 | F | Lt MCA AN | Lt pterional | None |
| 9 | 59 | F | Rt MCA AN (SAH) | Rt pterional | None |
| 10 | 70 | F | AComA AN | Lt pterional | None |
| 11 | 70 | M | Rt MCA AN | Rt pterional | None |
AComA: anterior communicating artery, AN: cerebral aneurysm, IC-PC: internal carotid artery–posterior communicating artery, Lt: left, MCA: middle cerebral artery, PICA: posterior inferior cerebellar artery, Rt: right, SAH: subarachnoid hemorrhage.
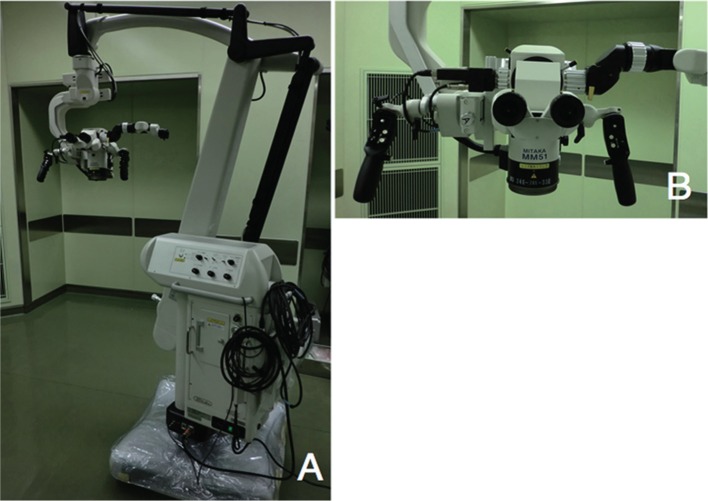
An operating microscope system with high magnification and high resolution (Mitaka Kohki Co., Ltd., Mitaka, Tokyo) was used in those procedures. This operating microscope has a single focal objective lens type (MM50/YOH) and modified varifocal objective lens type (MM51/YOH) (Fig. 1). The system is a standard zooming system and a newly developed high magnification system, with a magnification changer in the binocular tube system. This design permits high-resolution observation at a high magnification at suitable working distances. The zoom ratio of the microscope is 1:8. The spatial resolution and depth of focus for this new lens design is very high and good (distinctiveness of 7 μm and depth of about 1.0–2.0 mm at highest magnification). The eyepiece is 10×. The microscope stand has the ability to stop until three cycles against an external impact. The microscope has a novel illumination system of a 300-xenon light source and a foot pedal for hands-free operation.
Fig. 1.
Photographs of the operating microscope system with high magnification and high resolution with varifocal objective lens type. (A) A view of the operating microscope with the floor stand. (B) A closer view of the head of the microscope.
In the operating microscope with the single focal objective lens, the three fixed working distances are 200, 250, and 300 mm in neurosurgery. The combination of a 10× eyepiece and the 200-mm objective lens enabled a range of final magnification from 4.4× to 50.4×. The 250-mm objective lens enabled a range of final magnification from 3.5× to 40.3×. Then, the 300-mm objective lens enabled a range of final magnification from 2.9× to 33.6×. The objective lens had to be exchanged before an operation. In the operating microscope with the varifocal objective lens, the variable working distances range from 240 to 330 mm. The objective lens system did not have to be exchanged. The combination of a 10× eyepiece and the variable objective lens enabled a range of final magnification from 2.9× to 62.0×. The objective lens had a multifocal lens system that did not need to be exchanged.
The usual surgical procedures and instruments were employed in the microsurgical treatment. The magnifications were changed from low power to high power depending on the circumstances in a given procedure. Microsurgical procedures were performed at higher magnifications in certain situations.
Results
The magnifications could be altered to match the requirements as needed. In microsurgical procedures, higher magnifications were employed to observe and dissect the vessels that were tightly adhered to the aneurysms in the deep surgical fields. The images of the object were much clearer at higher magnifications than at regular ones. The working space, size of the field of vision, and illumination of the operative fields were also suitable to observe the small objects precisely. This equipment facilitated safe and precise observations and performance in various microsurgical situations. No intraoperative complications were encountered with the use of the novel microscope system. Postoperative angiograms revealed vascular reconstruction of the clip. No patients experienced perioperative complications.
I. Illustrative Case 1
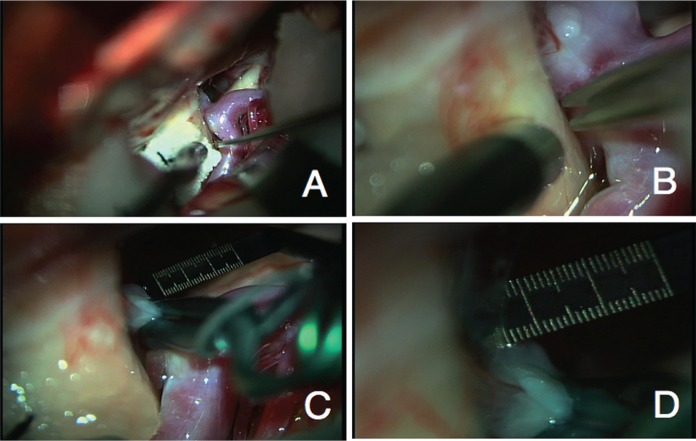
A 62-year-old male patient was incidentally discovered to have a left MCA aneurysm and underwent surgery because of a small aneurysm. A wide neck aneurysm was observed at standard magnifications via a left pterional approach (Fig. 2A). The dissection of the dome of an aneurysm and a temporal lobe was performed at higher magnifications safely (Fig. 2B, C). The aneurysm was clipped with a curved clip (Fig. 2D). The postoperative course was uneventful. Postoperative digital subtraction angiography documented complete obliteration of the aneurysm and normal filling of the surrounding vasculature.
Fig. 2.
Intraoperative photographs showing the left middle cerebral artery aneurysm at standard magnification (A) and dissecting the dome of the aneurysm from the temporal lobe at 40× magnification (B). After dissecting the aneurysm from the surrounding tissue (C), the neck of the aneurysm was clipped completely (D).
II. Illustrative Case 2
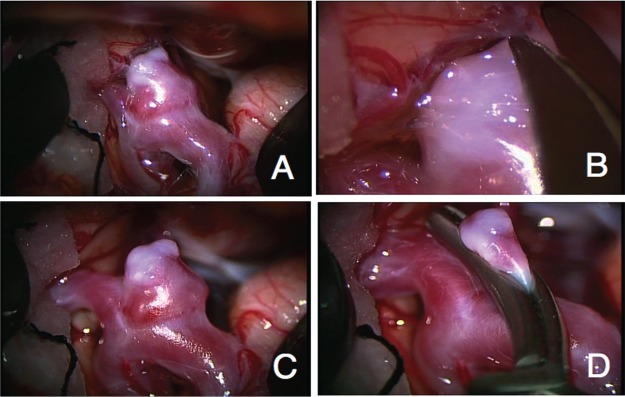
A 70-year-old female patient was incidentally discovered to have an AComA aneurysm and underwent surgery because of a small aneurysm. The dissection of the surrounding aneurysm and a left optic nerve was performed at higher magnifications for preservation of the nerve and perforating arteries via a left pterional approach (Fig. 3A, B). The aneurysm was clipped with a straight clip and observed to preserve the surrounding small vessels and the optic nerve (Fig. 3C, D). Postoperative digital subtraction angiography documented complete obliteration of the aneurysm. The patient had no complications and was discharged.
Fig. 3.
Intraoperative photographs demonstrating the anterior communicating artery aneurysm and the left optic nerve at standard magnification (A) and dissecting the neck of the aneurysm from the optic nerve at 62× magnification (B). The neck of the aneurysm was clipped at standard magnifications (C) and the small artery of the nerve (about 0.1 mm in diameter) in the dome was observed (D). One scale of the ruler was 0.1 mm.
Discussion
Recently, modern microscopes have been developed multiple modalities and visualization techniques intraoperatively.6) In literature, Zeiss OPMI 1 (the first operating microscope) with a single focal system had a working distance of 100–405 mm and final magnifications of 2.5–50× by Galilean step magnification changer.6,7) Yasargil described that it should adjust the degree of magnification according to the size of the object and also described that magnifications of 25–40× for a 0.5–1.0 mm of the object size should be selected.8) A 40× magnification, which was the combination of a 20× eyepiece and the 200-mm objective lens by this Zeiss OPMI 1, was the highest magnification for neurosurgery. However, this image at highest magnification would be magnified by the eyepiece, but would be unclear, dark, and with a short working distance. It means that the resolution (optical quality) was not increased. Optical quality of the intraoperative image is an important factor for microsurgical procedures.9) Moreover, standard operating microscopes in neurosurgery usually use a 10× or 12.5× eyepiece, objective lenses of focal lengths 200–350 mm and a range of final magnification from about 2× to 20× magnification in surface and deep surgical fields.10) These do not have a range of more than 30× magnifications.
This operating microscope system offers the image of the object clear at higher magnifications (more than 30× magnifications) because it has a newly designed lens system with a higher resolution. It means that the information of the visualization (optical quality) is increased. This operating microscope has a 10× eyepiece that is also optically adjustable. The range of the magnifications can also be altered to match the requirements for a particular situation. The disadvantage of high magnifications is that the increased magnification requires a darker operative field and a reduced depth of focus. In this microscope, visualization at high magnifications is achieved using a novel illumination system consisting of a xenon light source with a filter of reduced heat. The depth of focus in this microscope is about 1.0–2.0 mm at the highest magnification (62.0×), which is acceptable because the object is quite small. This microscope also has the ability to attach to the device of intraoperative videoangiography using indocyanine green.
In microsurgical work for cerebral aneurysms, the operative field must be arranged optimally. It is very important that the magnifications are of adequate ranges in various operative situations for each surgeon. We performed microsurgical observation and dissection around an aneurysm at higher magnifications. However, we applied to clip the neck of the aneurysm at appropriate magnifications and good depth of focus, because it was important to observe the profound of it. Use of the range of high magnifications may be limited to cerebral aneurysm operations. Furthermore, it would be needed for surgical skills at higher magnifications. However, we think that microsurgical observation and dissection of the object size of 0.5–1.0 mm would be needed regardless of large or small size of an aneurysm itself. It is obvious that practical final magnifications of more than 30× at each working distance would provide higher-magnified stereoscopic operative views. We think that the use of this microscope would have potential benefits for microsurgical treatment for cerebral aneurysms because of better visualization.
References
- 1). Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group : International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360: 1267– 1274, 2002. [DOI] [PubMed] [Google Scholar]
- 2). Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M, Rischmiller J, ISAT Collaborators : Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol 8: 427– 433, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, Albuquerque FC: The barrow ruptured aneurysm trial. J Neurosurg 116: 135– 144, 2012. [DOI] [PubMed] [Google Scholar]
- 4). Matsumura N, Shibata T, Umemura K, Nagao S, Horie Y: Extracranial-intracranial bypass surgery at high magnification using a new high-resolution operating microscope: technical note. Surg Neurol 72: 690– 694, 2009. [DOI] [PubMed] [Google Scholar]
- 5). Matsumura N, Hayashi N, Kamiyama H, Kubo M, Shibata T, Okamoto S, Horie Y, Hamada H, Endo S: Microvascular anastomosis at 30–50× magnifications (super-microvascular anastomosis) in neurosurgery. Surg Neurol Int 2: 6, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Uluç K, Kujoth GC, Başkaya MK: Operating microscope: past, present, and future. Neurosurg Focus 27: E4, 2009. [DOI] [PubMed] [Google Scholar]
- 7). Lang WH, Muchel F: ZEISS Microscopes for Microsurgery. Berlin, Springer-Verlag, 1981. [Google Scholar]
- 8). Yaşargil MG: The operating microscope, in Yaşargil MG. (ed): Microsurgery Applied to Neurosurgery. Stuttgart, Georg Thieme Verlag, 1969, pp 12– 32 [Google Scholar]
- 9). Hoerenz P: The operating microscope. I. Optical principles, illumination systems, and support systems. J Microsurg 1: 364– 369, 1980. [DOI] [PubMed] [Google Scholar]
- 10). Sekhar LN, Bucur SD, Fuentes G: General techniques and instrumentation for cranial microsurgery, in Sekhar LN, de Oliverira E. (eds): Cranial Micro-surgery: Approaches and Techniques. New York, Thieme, 1999, pp 1– 11 [Google Scholar]