Abstract
A 71-year-old woman with active rheumatoid arthritis (RA) was referred to our department because of multiple intracranial nodules. On admission, the RA disease activity was very high even after the treatment of methotrexate in other hospital. She underwent open biopsy to confirm a histopathological diagnosis of the intracranial lesions. Surgical specimen mainly consisted of necrosis surrounded by epithelioid cells. The masses were reduced spontaneously in size without additional treatment. Eleven month later, the lesions were relapsed. She underwent treatment with corticosteroid, and the lesions were remarkably regressed. The clinical course and histological examination were compatible with rheumatoid nodule (RN). Intracranial RN is extremely rare and its clinical course is not completely understood. In active RA patients, RNs should be considered, and histological diagnosis is inevitable for following suitable treatment.
Keywords: intracranial granulation, choroid plexus, corticosteroid, long term follow-up, rheumatoid nodule
Introduction
Rheumatoid arthritis (RA) is a systemic disease that affects nearly every organ. Nodule formation is observed in 20% of the patients with RA.1) It usually develops subcutaneously, but is rarely seen in various organs such as pleura, lung, and pharynx. On the other hand, central nervous system involvements such as vasculitis, hypertrophic pachymenigitis, or leptomeningitis rarely occur. It is often difficult to diagnose.2) Therefore, intracranial rheumatoid nodule (RN) has been rarely identified, and its clinical course and optimal treatment are not determined. We, here, present a case of intracranial multiple RNs that have been successfully treated with corticosteroid. We describe the clinical course, discuss the pathogenesis, and treatment of the intracranial RN.
Case Report
A 71-year-old woman had suffered from RA since August 2005. She started to take 4 mg of methotrexate (MTX) per week in November 2005. Because the arthritis was uncontrolled, MTX was increased up to 8 mg/week and the symptoms were gradually improved. However, the dose of MTX had to be decreased because of liver dysfunction. Alternatively, she was treated with decreased dose of MTX and other conventional therapy for RA such as salazosulfapyridine or bucillamine, which were neither effective. Therefore, she was referred to our University Hospital for further treatment in December 2006. On admission, rheumatoid factor was negative, but the 28-joint disease activity score (DAS-28) was 6.55. She underwent whole body examination by computed tomography (CT) for screening before the introduction of a newly developed therapeutic agent. Computed tomograms disclosed a mass with calcification in the posterior fossa, but not extra-cranial lesions. Magnetic resonance (MR) imaging showed multiple intracranial masses and they were strongly enhanced with contrast medium (Fig. 1a–d). The intracranial masses were located in the right cerebello-pontine angle, in the floor and posterior part of third ventricle, around bilateral foramens of Lushka, around bilateral Meckel's caves, and superior to left hippocampus. Some of them were attached to the dura mater and others were located adjacent to the choroid plexus. Abnormal high intensity area on T2-weighted image was seen in the brain parenchyma around the masses. The lesions strongly suggested dissemination of primary or metastatic brain tumor. Induction of new drug for RA was abandoned, and she was transferred to the neurosurgical department to confirm the histological diagnosis.
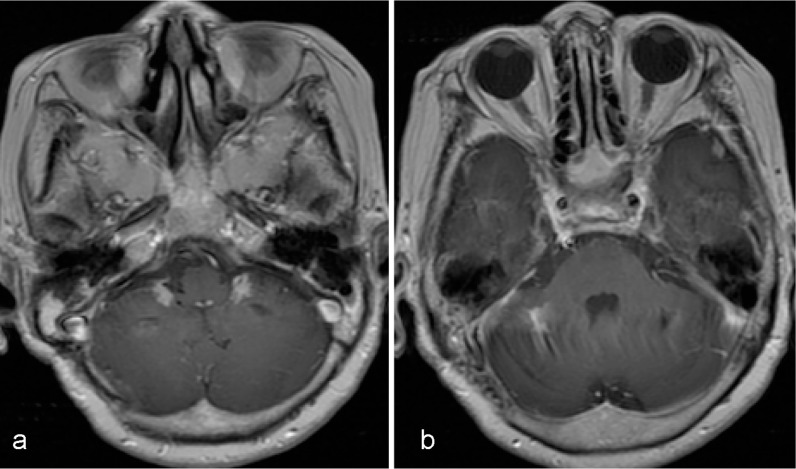
Fig. 1.
a: Initial T1-weighted magnetic resonance imaging with gadolinium. Well-enhanced nodules at bilateral foramen Lushka. b: The largest calcified mass in cerebello-pontine cistern showing mass effect. c: Coronal view showing enhanced lesions in the floor of third ventricle and adjacent to the left hippocampus. d: Sagittal section showing abnormal enhancement in the floor and posterior wall of third ventricle.
Her general status was good and no neurological deficits were observed. The specimen was taken from the biggest mass located in the right cerebello-pontine angle. The lesion was grayish-white, avascular, and amorphous. The surgical specimens histologically consisted of coagulative necrosis surrounded by epithelioid cell granulomas with a few multinucleated giant cells including Langhans-type (Fig. 2a, b). Gram-stain did not show any microorganisms and it was diagnosed as a sort of granulation. It was strongly speculated that the lesions were associated with RA, but treatments targeting on the lesions were not performed because the exact etiology was not determined. She continued the treatment for RA with 8 mg/week of MTX. MR imaging taken 1 month after surgery disclosed that all the masses got reduced in size and she was followed up at the outpatient clinic. The masses continued to shrink for the next 6 months (Fig. 3a, b) as observed under MR imaging.
Fig. 2.
Photomicrograph showing necrosis surrounded by epithelioid cells (a) with few multinucleated giant cells (b). Hematoxylin and eosin stain.
Fig. 3.
T1-weighted magnetic resonance imaging with gadolinium enhancement taken one month after the biopsy. All the masses remarkably reducing in size (a, b).
Three months later, she became lethargic, and neurological examination showed right hearing disturbance and mild limb ataxia. MR imaging showed regrowth of the masses (Fig. 4a–d). RA at that moment was not active. Therefore, RA itself did not require further treatment. She was treated with predonisolone since the lesions were inflammatory granulomas. She gradually got better and became active. Limb ataxia disappeared, though gait disturbance was not completely improved. MR imaging taken 2 weeks after the induction of predonisolone, showed remarkable shrinkage of all masses. The lesions kept shrinking and the granulomas almost disappeared except calcification in 3 years (Fig. 5a–c). Consequently, we diagnosed the lesions as the RN. Predonisolone was tapered off over a period of 30 months and her general condition was stable after discontinuation of predonisolone.
Fig. 4.
Magnetic resonance (MR) imaging taken 9 months after the biopsy showing the recurrence of the masses. T2-weighted MR imaging showing remarkable high intensity in bilateral peduncle and thalamus (a, b). T1-weighted MR imaging showing regrowth of the pre-existed masses (c, d).
Fig. 5.
Final magnetic resonance (MR) imaging after steroid therapy. a: T1-weighted MR imaging with gadolinium enhancement showing minimal enhancement of the choroid plexus and b, c: disappearance of abnormal enhancement of the cerebellopontine angle and third ventricle.
Discussion
RNs are the most common extra-articular lesions that occur in 20% of RA patients.1) Most commonly RNs occur subcutaneously, and also develop in various organs in the body such as lungs, pleura, and larynx.3)
Intracranial RNs are very rare and the clinical course is not well understood. According to our survey of literature,1,2,4–13) most of the cases were reported more than 20 years ago, and the prognoses of the patients were poor. Most RNs were situated adjacent to dura mater, and choroid plexus were involved in some cases.6)
Our case showed intracranial multiple nodules associated with RA, which was successfully treated with corticosteroid. There is no report of RN with high resolutional MR imaging followed up for more than 3 years.
Histopathologically, RN is characterized by fibrinoid necrosis surrounded by nuclear palisading. Infiltration of inflammatory cells including plasma cells, lymphocytes, and eosinophills are in its peripheral.4) It is generally believed that RN is one of the consequences of rheumatoid vasculitis.8) According to the previous report, histopatho-logical examination disclosed that various intracranial lesions such as rheumatoid encephalopathy, meningitis, or nodule could appear at the same time.9) Therefore, all those lesions may occur through the same mechanism. Immunohistochemical examination showed deposition of IgG or IgM in the affected cerebral vessel wall and choroid plexus. Immune complexes may be trapped by choroid plexus as a result of filtration mechanism.10) MR imaging of our case showed abnormal signal intensity in the brain parenchyma around the nodules, which may suggest the vasculitis or encephalopathy.
Steroid therapy for intracranial lesions in RA seems to be effective.13,14) In our case, the lesions were reduced without additional treatment at the initial manifestation. Such evidence has not been reported previously. At the recurrence, we decided to treat the patient with predonisolone because of manifestation of neurological deficits, and the steroid therapy was thought to be effective for inflammatory granuloma. Subsequently, we concluded that the lesions were associated with RA since the clinical course and histological findings were compatible for RN. In this case, RN formation was not associated with activity of RA, but it was probably important for the onset of the nodules.
Most of intracranial RN cases were reported before 1990. MTX was approved for RA treatment in the late 1980s and control of RA became dramatically improved with MTX. It is speculated that incidence of intracranial RN was diminished due to the MTX treatment. Further reduction of the incidence will be expected with the newly developed treatment for RA such as rituximab.
RN can occur during methotrexate therapy and it is called as MTX-induced accelerated nodulosis.7,15) It can be distinguished from spontaneous RN by the clinical course and immunohistochemical findings. Patients of RA develop RN rapidly after the induction or increasing of MTX and reduction of the dose induces rapid regression of RN.5) In some reports, it is positive for human leukocyte antigen (HLA)-DR4 though spontaneous RN did not.12) Difference may also be detected by expression of MMP-3, MMP-9, and Ki-67.11) Our case probably developed as spontaneous RNs because they resolved with continuation of MTX. In addition, there is no previous report of intracranial MTX-induced RN except for one suspected case.8) It is disputable if MTX should be continued or not when intracranial RN disclosed, because the definition and treatment of MTX-induced accelerated nodulosis are not clear.15)
In conclusion, RA can cause intracranial multiple nodules especially adjacent to dura mater and/or choroid plexus. Emergence of RN is not correlated with the activity of RA. Corticosteroid may be effective, but it can recur. Therefore long-term follow-up is necessary for the patient with intracranial RN. Treatment outcome might be more improved with newly developed therapeutic agents such as rituximab.
References
- 1). Kaye BR, Kaye RL, Bobrove A: Rheumatoid nodules. Review of the spectrum of associated conditions and proposal of a new classification, with a report of four seronegative cases. Am J Med 76: 279– 292, 1984. [DOI] [PubMed] [Google Scholar]
- 2). Koide R, Isoo A, Ishii K, Uruha A, Bandoh M: Rheumatoid leptomeningitis: rare complication of rheumatoid arthritis. Clin Rheumatol 28: 1117– 1119, 2009. [DOI] [PubMed] [Google Scholar]
- 3). Upile T, Jerjes W, Sipaul F, Singh S, Hopper C, Wright A, Sandison A: Rheumatoid nodule of the thyrohyoid membrane: a case report. J Med Case Rep 1: 123, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). Beck DO, Corbett JJ: Seizures due to central nervous system rheumatoid meningovasculitis. Neurology 33: 1058– 1061, 1983. [DOI] [PubMed] [Google Scholar]
- 5). Filosa G, Salaffi F, Bugatti L: Accelerated nodulosis during methotrexate therapy for refractory rheumatoid arthritis. A case report. Adv Exp Med Biol 455: 521– 524, 1999. [DOI] [PubMed] [Google Scholar]
- 6). Jackson CG, Chess RL, Ward JR: A case of rheumatoid nodule formation within the central nervous system and review of the literature. J Rheumatol 11: 237– 240, 1984. [PubMed] [Google Scholar]
- 7). Jang KA, Choi JH, Moon KC, Yoo B, Sung KJ, Koh JK: Methotrexate nodulosis. J Dermatol 27: 460– 464, 1999. [DOI] [PubMed] [Google Scholar]
- 8). Karam NE, Roger L, Hankins LL, Reveille JD: Rheumatoid nodulosis of the meninges. J Rheumatol 21: 1960– 1963, 1994. [PubMed] [Google Scholar]
- 9). Kim RC: Rheumatoid disease with encephalopathy. Ann Neurol 7: 86– 91, 1980. [DOI] [PubMed] [Google Scholar]
- 10). Kim RC, Collins GH, Parisi JE: Rheumatoid nodule formation within the choroid plexus. Report of a second case. Arch Pathol Lab Med 106: 83– 84, 1982. [PubMed] [Google Scholar]
- 11). Matsushita I, Uzuki M, Matsuno H, Sugiyama E, Kimura T: Rheumatoid nodulosis during methotrexate therapy in a patient with rheumatoid arthritis. Mod Rheumatol 16: 401– 403, 2006. [DOI] [PubMed] [Google Scholar]
- 12). Segal R, Caspi D, Tishler M, Fishel B, Yaron M: Accelerated nodulosis and vasculitis during methotrexate therapy for rheumatoid arthritis. Arthiritis Rheum 31: 1182– 1185, 1988. [DOI] [PubMed] [Google Scholar]
- 13). Tabuchi S, Tanabe M, Muraoka K, Hori T, Nakayasu H, Takahashi K, Ohama E: [A case of intracranial multiple nonspecific granulomas related to rheumatic disease: with special reference to magnetic resonance imaging]. No Shinkei Geka 20: 1025– 1030, 1992. (Japanese) [PubMed] [Google Scholar]
- 14). Matsushima M, Yaguchi H, Niino M, Akimoto-Tsuji S, Yabe I, Onishi K, Sasaki H: MRI and pathological findings of rheumatoid meningitis. J Clin Neurosci 17: 129– 132, 2010. [DOI] [PubMed] [Google Scholar]
- 15). Patatanian E, Thompson DF: A review of methotrexate-induced accelerated nodulosis. Pharmacotherapy 22: 1157– 1162, 2002. [DOI] [PubMed] [Google Scholar]