Abstract
A 50-year-old female presented with more than 20-year history of a large subcutaneous mass in the left parieto-occipital portion. Magnetic resonance (MR) imaging revealed the lipomatous mass to show a high signal intensity in both T1- and T2-weighted images. A part of the lipomatous lesion progressed into the underlying hyperostosis and skull. The preoperative diagnosis was skull invasion of a well-differentiated liposarcoma. The tumor was removed completely, including the underlying hyperostosis and skull. Microscopy confirmed a lipoma without any lipoblasts, which was firmly attached to the reactive hyperostosis, and islands of lipoma were involved in the underlying hyperostosis and skull cortex. A pathological diagnosis of parosteal lipoma with reactive hyperostosis was made. Long-term progression of parosteal lipoma may cause to involve the underlying hyperostosis and skull, and led to the diagnosis of invasion of a malignant tumor on MR imaging.
Keywords: parosteal lipoma, skull, hyperostosis, liposarcoma
Introduction
A parosteal lipoma is a benign fatty neoplasm showing an intimate relationship with the periosteum. Although the term “periosteal lipoma” has been used by most authors in the past, the term “parosteal lipoma” is thought to be more suitable since it indicates contiguity with bone rather than implying a definite origin from the periosteum.1) The most frequent site of the parosteal lipoma is the long bones of the extremities, whereas skull parosteal lipoma is extremely rare. We describe a case of skull parosteal lipoma with massive reactive hyperostosis mimicking tumor invasion in the skull cortex, which made it difficult to distinguish from intraosseous invasion of a liposarcoma.
Case Report
A 50-year-old female presented with more than 20-year history of a large subcutaneous mass in the left parieto-occipital portion. The mass was 5 by 8 cm, oval in shape, elastic-hard, and nontender. A computed tomography (CT) scan demonstrated a subcutaneous mass of fatty density, accompanied with cortical bone deformity and massive hyperostosis (Fig. 1). Magnetic resonance (MR) imaging revealed the mass to show a high signal intensity in both T1- and T2-weighted images, and its signal characteristics suggested a lipomatous tumor. The prominent area of low signal intensity in both T1- and T2-weighted images was closely attached to the skull, consistent with cortical hyperostosis as reactive bone. However, a part of the lipomatous lesion extended into the skull, suggesting bone invasion (Fig. 2). The mass was fed by the right occipital artery on a conventional angiogram. The preoperative diagnosis was invasion to the skull of a well-differentiated liposarcoma, because there has been no report of parosteal lipoma invading into the skull. The tumor was removed completely, including the underlying hyperostosis and skull by wide resection with a of 2 cm tumor margin. No invasion of the lesion was shown in the inner layer of the skull or the dura mater. When bisected, the cut surface showed a lipomatous yellowish lesion attached to the prominent hyperostosis (Fig. 3A). Microscopic finding was consistent with a lipoma because the tumor had no lipoblast. Tumor was firmly attached to the abnormal bone tissues. Those bone tissues were matured ones with reactive hyperostosis induced by parosteal lipoma (Fig. 3B, C). A diagnosis of a parosteal lipoma with reactive hyperostosis was made. A cranioplasty with titan mesh was performed two weeks after the operation.
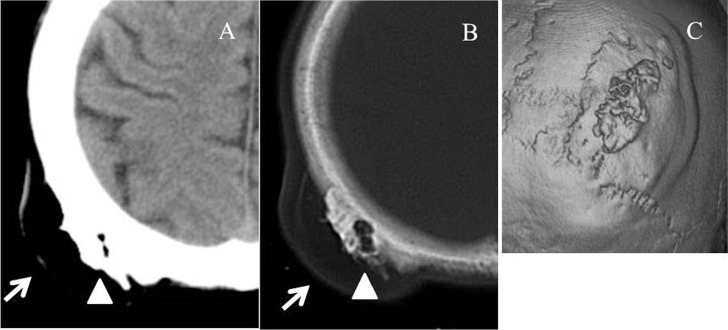
Fig. 1.
CT scan showing radiolucency of the subcutaneous mass (arrow), accompanied by prominent hyper-ostosis (arrowheads) at the parietal bone (A, B). Hyperostosis is noted on a three-dimensional CT image (C). CT: computed tomography.
Fig. 2.
Magnetic resonance imaging demonstrating a subcutaneous mass displays predominantly high signal intensity on both T1- (A) and T2-weighted images (B). A part of the lipomatous lesion progressed into the underlying hyperostosis (arrow).
Fig. 3.
A: A gross photograph of the cut surface showed a lipomatous yellowish lesion attached to the prominent hyperostosis. Small foci of lipomatous lesions were macroscopically observed within the hyperostosis and the skull (arrows). B: A lipoma was firmly attached to the reactive hyperostosis. Islands of lipoma were involved in the hyperostosis and the skull (arrows) (H&E ×10). C: No lipoblasts were observed in a higher power view (H&E ×200).
Discussion
Parosteal lipomas arise almost exclusively as solitary entities adjacent to the long bones of the upper and lower extremities, especially the proximal radius and femur. Although parosteal lipomas of the mandible, clavicle, scapula, ribs, pelvis, and cervical vertebrae have been reported,1) skull parosteal lipoma is extremely rare. Cil et al. recently reported the case of a 20-year-old man who presented with frontal parosteal lipoma.2) Although a few cases of skull parosteal lipoma had been reported before 1962 according to the review of a parosteal lipoma by Fleming et al.,1) skull parosteal lipoma has been rarely reported recently, probably due to strict definition of the entity. Bony changes are associated with a parosteal lipoma, and, in particular, reactive hyperostosis of cortical bone is frequently observed.1,3) Miller et al. reported 14 cases of parosteal lipoma in the bone tumor resistry at the Armed Forces Institute of Pathology, presenting the classification into four variants of underlying ossification: type 1: no ossification, type 2: pedunculated exostosis, type 3: sessile exostosis, and type 4: patchy chondro-osseous modulation. They commented that no ossification type was present in their files.3) This case was evaluated as type 3 ossification. In this case, foci of a lipoma within underlying hyperostosis and skull cortex were macroscopically and microscopically observed, whereas there has been no report about a parosteal lipoma extending into underlying hyperostosis. We suggested that a lipoma would be surrounded by and involved in hyperostotic lesion while reactive bone tissue was growing over 20 years, and that a soft lipomatous tissue might extend into vacancy along irregular surface of hyperostosis. Therefore, it seemed that a part of the parosteal lipoma would be involved within the underlying hyperostosis and skull cortex on some pathological sections.
Radiologic diagnosis of a parosteal lipoma is facilitated by MR imaging. MR imaging showed the characteristic features of a lipoma, as well as hyperostotic areas that remained of low signal intensity in both T1- and T2-weighted sequences.4) In this case, we diagnosed as a malignant tumor, because it seemed that lipomatous lesion progressed into the skull cortex. We performed wide resection of the tumor, considering the lesion to be located in the low surgical risk site for wide resection. If a parosteal lipoma could be diagnosed on preoperative imaging, resection of the tumor along with shaving of the reactive ossification would be a sufficient management procedure.2) An open biopsy followed by resection of the tumor is recommended in cases of lesions at high surgical risk for wide resection.
References
- 1). Fleming RJ, Alpert M, Garcia A: Parosteal lipoma. Am J Roentgenol 87: 1075– 1084, 1962. [Google Scholar]
- 2). Cil Y, Kocer NE, Yapici AK: Frontal parosteal lipoma. J Craniofac Surg 19: 1122– 1125, 2008. [DOI] [PubMed] [Google Scholar]
- 3). Miller MD, Ragsdale BD, Sweet DE: Parosteal lipomas: a new perspective. Pathology 24: 132– 139, 1992. [DOI] [PubMed] [Google Scholar]
- 4). Laorr A, Greenspan A: Parosteal lipoma with hyperostosis: report of two pathologically proven cases evaluated by magnetic resonance imagin g. Can Assoc Radiol J 44: 285– 290, 1993. [PubMed] [Google Scholar]