Abstract
Setting: Antiretroviral treatment (ART) Centre in Tumkur district of Karnataka State, India. There is no published information about pre-ART loss to follow-up from India.
Objective: To assess the proportion lost to follow-up (defined as not visiting the ART Centre within 1 year of registration) and associated socio-demographic and immunological variables.
Design: Retrospective cohort study involving a review of medical records of adult HIV-infected persons (aged ⩾15 years) registered in pre-ART care during January 2010–June 2012.
Results: Of 3238 patients registered, 2519 (78%) were eligible for ART, while 719 (22%) were not. Four of the latter were transferred out; the remaining 715 individuals were enrolled in pre-ART care, of whom 290 (41%) were lost to follow-up. Factors associated with loss to follow-up on multivariate analysis included age group ⩾45 years, low educational level, not being married, World Health Organization Stage III or IV and rural residence.
Conclusion: About four in 10 individuals in pre-ART care were lost to follow-up within 1 year of registration. This needs urgent attention. Routine cohort analysis in the national programme should include those in pre-ART care to enable improved review, monitoring and supervision. Further qualitative research to ascertain reasons for loss to follow-up is required to design future interventions.
Keywords: pre-ART, loss to follow-up, NACP, ART centre, operational research, India
Abstract
Contexte : Centre de traitement antirétroviral (ART) du district de Tumkur dans l'état de Karnataka, Inde. Il n'y a pas de document publié sur les perdus de vue avant le traitement ART en Inde.
Objectif : Evaluer la proportion de perdus de vue (définis comme l'absence de visite au centre d'ART dans l'année suivant l'enregistrement) et les variables sociodémographiques et immunologiques qui y sont associées.
Schéma : Etude rétrospective de cohorte impliquant une revue des dossiers médicaux des patients adultes infectés par le VIH (âge ⩾15 ans) enregistrés en soins pré-ART entre janvier 2010 et juin 2012.
Résultats : Sur 3238 patients enregistrés, 2519 (78%) étaient éligibles pour le traitement ART tandis que 719 (22%) ne l'étaient pas. Quatre de ces derniers ont été transférés. Parmi les 715 individus enrôlés en soin pré-ART, 290 (41%) ont été perdus de vue. Les facteurs associés avec le fait d'être perdus de vue en analyse multivariée incluaient la tranche d'âge ⩾45 ans, un niveau d'instruction faible, le célibat, le stade 3 ou 4 de l'OMS et la résidence en milieu rural.
Conclusion : Près de quatre individus sur 10 en soins pre-ART ont été perdus de vue dans l'année suivant leur enregistrement. Ceci requiert une attention urgente. L'analyse de cohorte en routine du programme national devrait inclure les patients en soins pré-ART afin d'améliorer la revue des cas, leur suivi et leur supervision. Une recherche qualitative ultérieure afin de cerner les raisons des pertes de vue est nécessaire pour concevoir les interventions futures.
Abstract
Marco de referencia: El centro de tratamiento antirretrovírico (ART) en el distrito de Tumkur del estado de Karnataka en la India. Hasta el momento no existen publicaciones sobre la pérdida de vista de los pacientes seropositivos durante el seguimiento antes de comenzar el ART en la India.
Objetivo: Se buscó definir la proporción de pacientes perdidos de vista durante el seguimiento (definidos como los pacientes que no habían acudido al centro de ART hasta un año después de haberse registrado) y evaluar las variables socioeconómicas e inmunitarias que se asociaban con esta situación.
Método: Se llevó a cabo un estudio retrospectivo de cohortes a partir del examen de las historias clínicas de los adultos (⩾15 años de edad) infectados por el virus de la inmunodeficiencia humana (VIH), que se inscribieron a la atención clínica previa al ART de enero del 2010 a junio del 2012.
Resultados: De los 3238 pacientes registrados, 2519 cumplían con los requisitos para iniciar el ART (78%) y 719 de ellos no eran aptos (22%); cuatro pacientes de este último grupo se remitieron a otro centro. De las 715 personas restantes, inscritas en la atención previa al ART, 290 se perdieron de vista durante el seguimiento (41%). El análisis multifactorial puso en evidencia que los factores asociados con la pérdida de vista de los pacientes fueron el grupo de edad de ⩾45 años, una baja escolaridad, el hecho de ser solteros, el estado 3 o 4 de la enfermedad según la clasificación de la Organización Mundial de la Salud y la residencia en zona rural.
Conclusión: Cerca de cuatro de cada diez pacientes inscritos en la atención clínica previa al ART se perdieron de vista durante el seguimiento en el primer año después de haberse registrado. Esta situación exige una atención urgente. Es importante que los análisis sistemáticos de cohortes del programa nacional incluyan a las personas infectadas que reciben atención antes de comenzar el ART, a fin de mejorar la evaluación, el seguimiento y la supervisión de los pacientes. Es preciso fomentar la realización de nuevas investigaciones cualitativas que determinen las razones de la pérdida de vista durante el seguimiento y contribuyan a la planificación de las intervenciones futuras.
‘Pre-antiretroviral treatment (pre-ART) care’ in the Indian context refers to all services provided to individuals with human immunodeficiency virus (HIV) infection between registering at an ART centre and receiving the first dose of ART medication.1 Pre-ART ‘retention’ is an important programme indicator, and is defined as the capacity of the health system to maintain patients on active follow-up before ART initiation. Maintaining HIV-infected persons in pre-ART care is important to provide effective management of opportunistic infections, to ensure ART initiation at the optimal time, and to promote prevention of HIV transmission in the community.2,3 Delays in ART initiation result in increased morbidity and mortality, which impact negatively on programme performance.
India is currently facing a concentrated HIV epidemic, with an estimated 1.7–2.5 million people living with HIV.4 Of these, over 65% are considered eligible for ART,5 implying that about 35% should be retained in pre-ART care.6 Such individuals are required to be registered and maintained on follow-up care at ART centres countrywide. A systematic review by Rosen et al. showed that only a third of patients testing HIV-positive in sub-Saharan Africa are retained in care.7 India, like other ART programmes around the world, confines routine programme reporting to ‘on-treatment analysis’, which means that what happens before ART initiation is unknown. A previous study from Karnataka State, India, by Shastri et al. reported a 29% loss to follow-up between HIV testing, registration at ART centres and ART initiation among eligible individuals.8 However, retention among individuals who were not yet eligible for ART (pre-ART) was not assessed. Knowing the level of retention among pre-ART clients could have important programmatic and public health implications.
In a cohort of HIV-infected persons who were registered in pre-ART care at an ART centre in the Tumkur district of Karnataka State, India, we aimed to 1) report on the proportion lost to follow-up within 1 year of registration and 2) determine socio-demographic and immunological variables associated with loss to follow-up.
METHODS
Study design
This was a retrospective cohort study using routine programme data.
Study site, setting and population
The study was conducted at the ART Centre, located in the Tumkur District Hospital of Karnataka State, India. Karnataka is one of the four largest states in South India, with a relatively high HIV prevalence of 0.52%.4 Tumkur, with a population of 2.7 million, is one of the high HIV prevalence districts. Karnataka State has a total of 55 ART centres, with two located in the Tumkur district. All ART centres cater for patients in the pre-ART stage as well as those on ART.
The study was conducted between March and November 2013 and included a cohort of HIV-infected persons (aged ⩾15 years) registered in pre-ART care from January 2010 to June 2012.
Registration, eligibility for ART and management of patients at the ART centre
All HIV-infected persons presenting at ART centres are registered in a pre-ART register, and are given a unique pre-ART registration number and a treatment card. They are then assessed for ART eligibility according to national guidelines (Figure 1).6 Those found eligible are initiated on ART, while those not eligible (individuals with a CD4 count >350 cells/mm3 or in World Health Organization [WHO] Clinical Stage I and II) are registered and followed up in pre-ART care. Clients in pre-ART care undergo 6-monthly clinical and immunological assessments, including CD4 counts. A decision to start ART or to continue in pre-ART is made accordingly. Individuals who are found not to be eligible for ART are given a follow-up visit date. Those with a borderline CD4 count are monitored at more frequent intervals (those with CD4 counts of 350–400 and 400–500 cells/mm3 are monitored monthly and quarterly, respectively).6 In the event of intercurrent illness, individuals are advised to visit any of the nearest health facilities or the ART centre.
FIGURE 1.
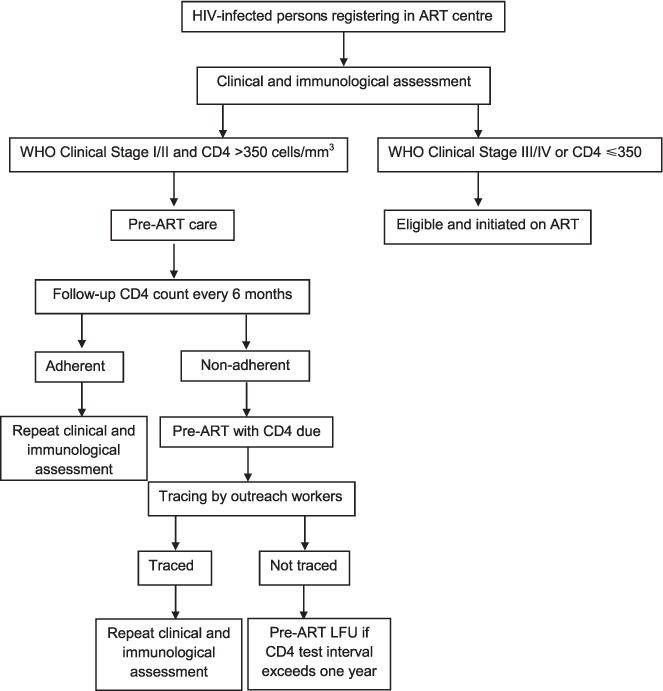
Management of HIV-infected persons in ART centres according to Indian ART operational guidelines, 2012. HIV = human immunodeficiency virus; ART = antiretroviral treatment; WHO = World Health Organization; LFU = lost to follow-up.
If a person registered under pre-ART care does not visit the ART centre as scheduled, he/she is listed as a ‘pre-ART patient with CD4 due’. Measures to trace the patient are initiated, and lists of these patients are shared with the community care centres (CCCs), community-based organisations (CBOs), non-governmental organisations (NGOs), integrated counselling and testing centres (ICTCs) and the district AIDS (acquired immune-deficiency syndrome) prevention and control unit (DAPCU) during routine monthly review meetings. If the patient does not attend for follow-up for a further 6 months (meaning that there has not been a single visit within a year of registration), this person is termed as ‘pre-ART lost to follow-up’.
If a patient declared lost to follow-up from pre-ART turns up anytime afterwards, he/she is counselled, continued with the previous pre-ART registration number and recorded as ‘re-entered (return after loss to follow-up)’.
Data and statistical analysis
Data related to the study objectives were sourced from National AIDS Control Programme (NACP) treatment cards maintained at the ART centre and cross-verified against the pre-ART register. Data were double entered in a structured data entry format prepared in EpiData entry software (Version 3.1, EpiData Association, Odense, Denmark) by two independent investigators, and validated. Data were summarised as means or medians (for continuous variables) and proportions (for categorical variables). The χ2 test was used to compare proportions. The primary outcome of interest was loss to follow-up, and the exposures assessed for association were age, sex, education, occupation, marital status, WHO clinical staging and CD4 count. The magnitude of associations was assessed using relative risks and adjusted using a multivariate log-binomial regression model to control for confounding;9 95% confidence intervals were used and a P value ⩽ 0.05 was considered statistically significant. EpiData analysis (version 2.2.2.182) and Stata version 12.1 (Stata Corporation, College Station, TX, USA) were used for analysis.
Ethics approval
Ethics approval was obtained from the Ethics Committee of the National AIDS Control Organisation (NACO), New Delhi, India, and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France. As the study did not involve direct patient interaction, the need for informed consent was waived by the ethics committees.
RESULTS
Of 3238 patients registered, 2519 (78%) were found to be eligible for ART at baseline, while 719 (22%) were not. Four of the latter were transferred out. Of the remaining 715 individuals enrolled in pre-ART care, 64% were females, and the mean (standard deviation) age was 33 (±11.2) years. At one year after registration, 425 (59%) were retained in pre-ART care and 290 (41%) had been lost to follow-up (Figure 2). Of those retained in care, 83 (20%) became eligible and were started on ART at their first follow-up visit after registration.
FIGURE 2.
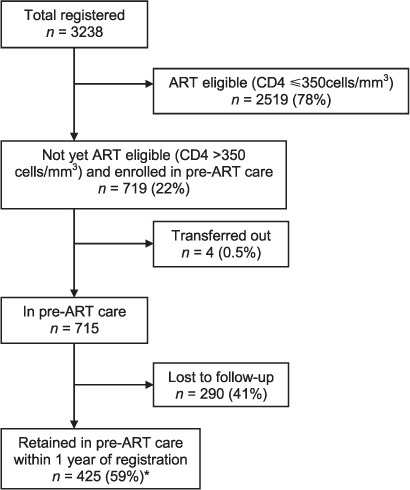
Retention of HIV-infected persons in pre-ART care in Tumkur district ART centre, Karnataka, India, January 2010–June 2012. * Among the 425 (59%) who were retained in care, 83 (20%) were initiated on ART as they were found to be eligible. HIV = human immunodeficiency virus; ART = antiretroviral treatment; WHO = World Health Organization.
The demographic and clinical characteristics of patients lost to follow-up and those retained in care are compared in Table 1. The two groups differed significantly with respect to age, education and residence. Patients in WHO Clinical Stage III or IV represented those co-infected with pulmonary tuberculosis (TB).
TABLE 1.
Demographic and clinical characteristics of patients lost to follow-up and retained in pre-ART care in Tumkur district, Karnataka, India, January 2010–June 2012
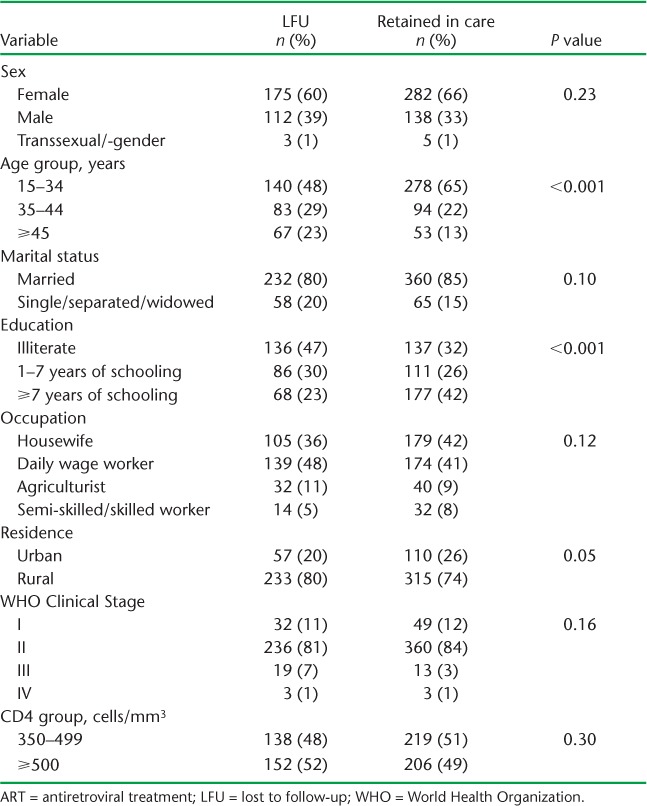
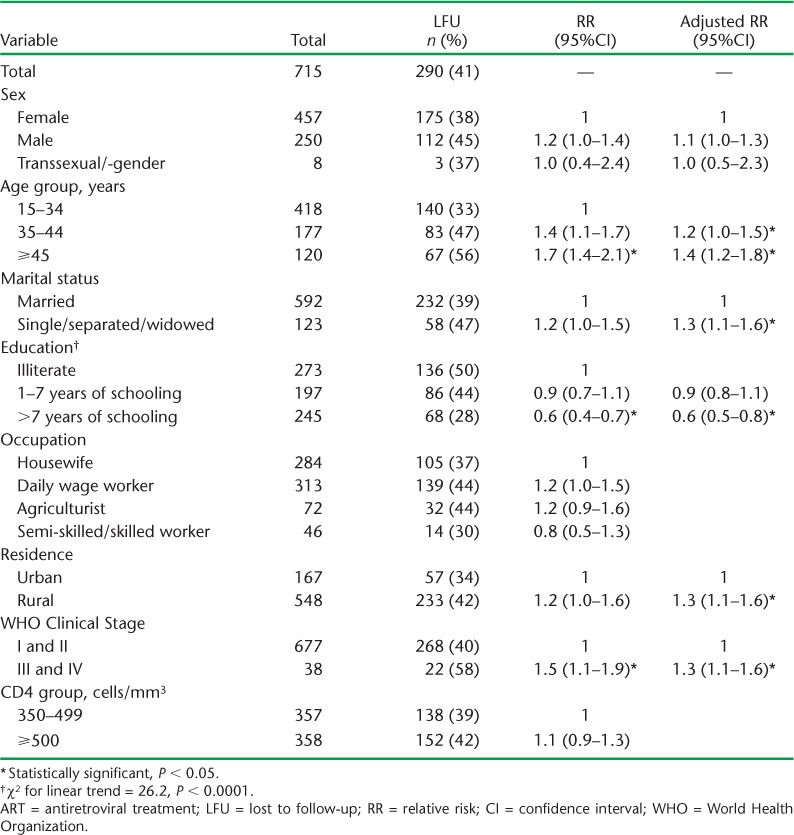
Table 2 shows the results of bivariate and multivariate analysis examining factors associated with loss to follow-up. On bivariate analysis, age, education and WHO staging were found to be statistically significant. All variables except occupation and CD4 count were included in the multivariate analysis to rule out the possibility of negative confounding due to any variable. Occupation (with subcategory ‘housewife’) and CD4 count were not included in the final model, due to collinearity with the variables sex (with the subcategory female) and WHO clinical staging, respectively. Significant factors associated with greater risk of loss to follow-up on multivariate analysis included age group ⩾45 years, low educational level, being unmarried, rural residence and WHO Stage III or IV (Table 2). A significant linear trend in loss to follow-up was associated with the level of education.
TABLE 2.
Factors associated with loss to follow-up during pre-ART care in Tumkur district, Karnataka, India, January 2010–June 2012
DISCUSSION
This is the first study from India to assess pre-ART retention at a district-level ART centre in Karnataka state, showing that only about six in 10 individuals remained in care 1 year after registration. These findings are not encouraging, although marginally better than in a similar district-level study from Malawi, which showed a low retention of 4% at 6 months,10 a study from South Africa with a pre-ART retention of 43%,11 and findings of a systematic review from sub-Saharan Africa, where only a third of patients were retained.7 Few recent studies from sub-Saharan Africa have reported similar12 or better13 retention rates after accounting for the real reasons for loss to follow-up. We feel nevertheless that a loss to follow-up rate of 41% is high, and more effort is warranted to improve the situation. In India an estimated 500 000 individuals are in pre-ART care, and if the proportion of loss to follow-up seen in our study is reflective of the general situation, it would crudely extrapolate to 205 000 individuals countrywide. Loss to follow-up serves as a proxy for challenges in pre-ART management, and overcoming these would directly benefit patients and the community at large.
The strengths of the study are that the findings come from a routine setting and are likely to reflect the situation on the ground, and the cohort included all patients registered in pre-ART care. Further, we believe the data are robust, as cross-verification had been performed between treatment cards and registers, with data being double entered and validated. We also adhered to Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines,14 including ethics, in reporting this research.15
How can we improve current pre-ART retention rates in India?
Indian guidelines for cotrimoxazole prophylaxis therapy (CPT) for the prevention of opportunistic infections is restricted to those with WHO Clinical Stage III/IV and/or those with a CD4 count <250 cells/mm3. Isoniazid preventive therapy is also not offered, due to concerns about the feasibility of its implementation among national policy makers in India, although a pilot study is ongoing which is expected to inform future scale-up decisions. There is thus no real incentive or ‘offer’ to patients for return visits except for a CD4 count test. Current WHO guidelines recommend CPT for all individuals with CD4 count <500 cells/mm3 in areas where bacterial infections and malaria are common.16 The NACP could thus consider increasing the threshold for CPT initiation. The 2013 WHO ART guidelines also recommend initiating ART for all individuals with a CD4 count <500 cells/mm3.3 If these two recommendations had been followed, a considerable proportion of individuals who were in pre-ART care in this study and were subsequently lost to follow-up with a CD4 count 350–499 cells/mm3 (38%) would have started CPT and/or ART and might have been retained. About one fifth of the patients retained in care became eligible for ART even in accordance with current guidelines, and were initiated on ART.
Three unique registration numbers are currently being given to patients at the three levels of the patient care pathway: at the HIV testing site, at the pre-ART stage and while on ART. As India is moving towards an electronic online database system for HIV-infected persons, there is an excellent opportunity to move towards a unique patient identification number at all levels of the care pathway. The NACP could introduce monthly reporting on pre-ART, as is currently done for those on ART. This will enhance cohort monitoring and tracing of patients lost to follow-up.17
Individuals aged ⩾45 years and from rural areas have a significantly higher chance of being lost to follow-up. This may be due to socio-economic hardship, including the inability to pay for transport costs for a return visit. Karnataka state has already initiated a scheme that provides travel allowance to patients, but this is restricted to those on ART. It would now seem logical to also extend this laudable initiative to those in pre-ART care. There have also been recent initiatives to link HIV-infected people to existing social welfare schemes, although the impact of these on patient retention is yet to be evaluated. In addition, being unmarried was associated with a higher risk of loss to follow-up, suggesting the importance of family support in ensuring retention in care. Patients in WHO Stage III or IV had a higher risk of loss to follow-up and could represent unaccounted for deaths. These included patients co-infected with pulmonary TB but with a CD4 count of >350 cells/mm3 and thus ineligible for ART at the time of the study. The guidelines to start ART in all HIV-TB patients, irrespective of CD4 count, came into effect in March 2012. While most of these factors have already been identified by studies elsewhere, this is the first time there has been published information from India, and such local evidence is important for decision making.
There have been efforts to standardise the definition of loss to follow-up among patients started on ART, thus minimising misclassifications.18 Similar efforts are needed for patients in pre-ART care to ensure uniformity in reporting across the globe.
Finally, reinforcing outreach tracing, improved counselling and peer support mechanisms at community level may enhance retention, as has been shown in sub-Saharan Africa.19,20
There are some study limitations. We used a 1-year cut-off period to declare a patient as lost to follow-up, but such patients may attend for follow-up after this time. Those retained may also be lost after the cut-off used in this study. This may influence the real retention rates in the long term. We assessed retention from the time of registration, but losses are also known to occur before this stage, between HIV testing and registration, and this was not captured in our study. The overall losses in pre-ART care may thus be higher.7,8 We also do not know the exact reasons why patients were lost to follow-up. Anecdotal evidence during informal interactions with outreach workers and patients suggested three main reasons: being clinically asymptomatic, migration or wrong address provided at the time of registration and death. While other studies have shown that ‘unaccounted transfers’, reflecting patients on care elsewhere (including those on care in the private health sector), have accounted for loss to follow-up, we feel that this represents a negligible proportion in our setting.13,21 Further qualitative research and a sampling-based approach to interview a random sample of patients lost to follow-up are required to confirm these, ascertain other reasons and guide future interventions.22,23 Finally, this study focused on one of the 55 nodal ART centres that currently exist in Karnataka state, thus limiting the generalisability of the findings. The indicator for pre-ART loss to follow-up is now part of routine reporting from all the ART centres, and this is expected to inform the state-wide situation. All of these aspects merit specific operational research.
CONCLUSION
Pre-ART retention at an ART centre in Karnataka State, India, was not encouraging, and further efforts are warranted to improve the situation for the benefit of patients and the community at large. Routine cohort analysis in the national programme should include patients in pre-ART care in addition to those on ART, to enable improved review, monitoring and supervision. Further qualitative research to ascertain reasons for loss to follow-up is required to design future interventions.
Acknowledgments
Thanks to the Karnataka State AIDS Prevention Society and the National AIDS Control Organisation, Department of AIDS Control, New Delhi, India, for all support and guidance throughout the study. This research was supported through an operational research course that was jointly developed and run by the International Union Against Tuberculosis and Lung Disease (The Union) South-East Asia Regional Office, New Delhi, India; the Centre for Operational Research, The Union, Paris, France; and the Operational Research Unit (LUXOR), Médecins Sans Frontières, Brussels Operational Centre, Luxembourg. This course is under the umbrella of the World Health Organization (WHO-TDR) SORT IT programme (Structured Operational Research and Training Initiative) for capacity building in low- and middle-income countries.
Funding for the course was from the Bloomberg Philanthropies and the Department for International Development, UK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: None declared.
References
- 1.Fox M P, Larson B, Rosen S. Defining retention and attrition in pre-antiretroviral HIV care: proposals based on experience in Africa. Trop Med Int Health. 2012;17:1235–1244. doi: 10.1111/j.1365-3156.2012.03055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen M S, Chen Y Q, McCauley M et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Consolidated guidelines for the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach. Geneva, Switzerland: WHO; 2013. http://www.who.int/hiv/pub/guidelines/arv2013/download/en/index.html Accessed October 2014. [PubMed] [Google Scholar]
- 4.National AIDS Control Organization, National Institute of Medical Statistics. Technical Report India HIV Estimates – 2012. Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India 2013. New Delhi, India: Ministry of Health; 2012. http://pib.nic.in/newsite/PrintRelease.aspx?relid=89785 Accessed October 2014. [Google Scholar]
- 5.Shastri S, Boregowda P H, Rewari B B, Tanwar S, Shet A, Kumar A M. Scaling up antiretroviral treatment services in Karnataka, India: impact on CD4 counts of HIV-infected people. PLOS ONE. 2013;8:e72188. doi: 10.1371/journal.pone.0072188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National AIDS Control Organization. Antiretroviral therapy guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis, 2012. New Delhi, India: Ministry of Health and Family Welfare, Government of India; 2012. http://www.nacoonline.org/Quick_Links/Publication/Treatment_Care__Support/ Accessed October 2014. [Google Scholar]
- 7.Rosen S, Fox M P. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLOS Med. 2011;8:e1001056. doi: 10.1371/journal.pmed.1001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shastri S, Satyanarayana S, Nagaraja S B et al. The journey to antiretroviral therapy in Karnataka, India: who was lost on the road? J Int AIDS Soc. 2013;16:18502. doi: 10.7448/IAS.16.1.18502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNutt L A, Wu C, Xue X, Hafner J P. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 10.Tayler-Smith K, Zachariah R, Manzi M et al. Antiretroviral treatment uptake and attrition among HIV-positive patients with tuberculosis in Kibera, Kenya. Trop Med Int Health. 2011;16:1380–1383. doi: 10.1111/j.1365-3156.2011.02863.x. [DOI] [PubMed] [Google Scholar]
- 11.Clouse K, Pettifor A E, Maskew M et al. Patient retention from HIV diagnosis through one year on antiretroviral therapy at a primary health care clinic in Johannesburg, South Africa. J Acquir Immune Defic Syndr. 2013;62:e39–46. doi: 10.1097/QAI.0b013e318273ac48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pati R, Lahuerta M, Elul B et al. Factors associated with loss to clinic among HIV patients not yet known to be eligible for antiretroviral therapy (ART) in Mozambique. J Int AIDS Soc. 2013;16:18490. doi: 10.7448/IAS.16.1.18490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Namusobya J, Semitala F C, Amanyire G et al. High retention in care among HIV-infected patients entering care with CD4 levels >350 cells/μL under routine program conditions in Uganda. Clin Infect Dis. 2013;57:1343–1350. doi: 10.1093/cid/cit490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.von Elm E, Altman D G, Egger M, Pocock S J, Cøtzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 15.Edginton M, Enarson D, Zachariah R, Reid T, Satyanarayana S, Bissell K. Why ethics is indespensible for good-quality operational research. Public Health Action. 2012;2:21–22. doi: 10.5588/pha.12.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Guidelines on co-trimoxazole prophylaxis for HIV-related infections among children, adolescents and adults. Recommendations for a public health approach. Geneva, Switzerland: WHO; 2006. http://www.who.int/hiv/pub/guidelines/ctxguidelines.pdf Accessed October 2014. [PubMed] [Google Scholar]
- 17.Zachariah R, Tayler-Smith K, Manzi M et al. Retention and attrition during the preparation phase and after start of antiretroviral treatment in Thyolo, Malawi, and Kibera, Kenya: implications for programmes? Trans R Soc Trop Med Hyg. 2011;105:421–430. doi: 10.1016/j.trstmh.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 18.Chi B H, Yiannoutsos C T, Westfall A O et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLOS Med. 2011;8:e1001111. doi: 10.1371/journal.pmed.1001111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Decroo T, Rasschaert F, Telfer B, Remartinez D, Laga M, Ford N. Community-based antiretroviral therapy programs can overcome barriers to retention of patients and decongest health services in sub-Saharan Africa: a systematic review. Int Health. 2013;5:169–179. doi: 10.1093/inthealth/iht016. [DOI] [PubMed] [Google Scholar]
- 20.Decroo T, Van Damme W, Kegels G, Remartinez D, Rasschaert F. Are expert patients an untapped resource for ART provision in sub-Saharan Africa? AIDS Res Treat. 2012;2012:749718. doi: 10.1155/2012/749718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geng E H, Glidden D V, Emenyonu N et al. Tracking a sample of patients lost to follow-up has a major impact on understanding determinants of survival in HIV-infected patients on antiretroviral therapy in Africa. Trop Med Int Health. 2010;15(Suppl):63–69. doi: 10.1111/j.1365-3156.2010.02507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geng E H, Glidden D V, Bwana M B et al. Retention in care and connection to care among HIV-infected patients on antiretroviral therapy in Africa: estimation via a sampling-based approach. PLOS ONE. 2011;6:e21797. doi: 10.1371/journal.pone.0021797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geng E H, Nash D, Kambugu A et al. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7:234–244. doi: 10.1007/s11904-010-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


