Abstract
In a cross-sectional survey conducted in 45 districts of India, we assessed 1) use of any rapid point-of-care (POC) tests by primary health care providers, and 2) their willingness to use POC tests for tuberculosis (TB) in future. A total of 767 primary health care providers, including private and public sector practitioners, health workers and chemists, were interviewed. A quarter of the primary health care providers reported using POC tests, with pregnancy tests being the most common. Nearly half of the respondents expressed willingness to use POC tests for TB, provided the test was available free or at low cost (<US$ 2.00).
Keywords: POC tests, India, primary care
Abstract
Dans une enquête transversale réalisée dans 45 districts d'Inde, nous avons évalué 1) l'utilisation d'un quelconque test rapide, effectué sur les lieux de soins (tests POC) par les prestataires de soins de santé primaires, et 2) leur volonté à utiliser les tests POC pour la tuberculose à l'avenir. Un total de 767 prestataires de soins de santé primaires, praticiens du secteur privé et public, travailleurs de santé et pharmaciens ont été interviewés. Un quart des prestataires de soins de santé primaires ont affirmé qu'ils recouraient aux tests POC, les plus utilisés étant les tests de grossesse. Près de la moitié des répondants a exprimé sa volonté d'utiliser un test POC pour la tuberculose à condition que le test soit disponible gratuitement ou à faible coût (<2$US).
Abstract
En un estudio transversal realizado en 45 distritos de la India, se examinó el uso de alguna prueba diagnóstica rápida en el lugar de atención por parte de los profesionales de salud y la inclinación que estos referían a usarlas en el diagnóstico de la tuberculosis en el futuro. Se administraron entrevistas a 767 profesionales de atención primaria del sector público y el sector privado, quienes pertenecían al personal médico y otros profesionales sanitarios y farmacéuticos. Un cuarto de los profesionales declaró estar usando las pruebas diagnósticas en el lugar de atención y las más utilizadas fueron las pruebas de embarazo. Cerca de la mitad de las personas que respondieron expresó su buena disposición a aplicar las pruebas diagnósticas de la tuberculosis en el lugar de atención, siempre y cuando se ofrecieran al paciente sin costo alguno o a un bajo costo (menos de 2 USD).
Apoint-of-care (POC) test is a diagnostic test used at or near the site where clinical care is provided.1,2 An ideal POC test provides rapid results that enable health care providers to make clinical decisions at the same clinical encounter.3 Testing and treating at the same visit should improve patient outcomes and reduce the transmission of infectious diseases.4
POC tests are available for a variety of conditions, such as pregnancy, anaemia, diabetes mellitus, malaria and the human immunodeficiency virus (HIV).5 They are minimally invasive, relatively inexpensive, require limited skill/training and give reasonably accurate results. In principle, these characteristics make them attractive and suitable for use by primary health care providers (PHCPs).6 However, limited data are available on whether PHCPs in resource-limited settings actually use POC tests in routine practice.
Tuberculosis (TB) is a major public health problem in many low- and middle-income countries, including India.7 Incorrect diagnosis and/or delays in diagnosis by the PHCPs are responsible for considerable morbidity, mortality and transmission. The development of POC testing technologies for TB has thus been ranked as high priority by several stakeholders.8–11
In this study, we assessed the use of any rapid POC tests by PHCPs at community level in India, and asked whether they would be willing to use a POC test for TB, if available, and at what price.
METHODS
Setting
This study, conducted in 45 districts of India between November 2012 and April 2013, was nested in a larger knowledge, attitude and practice (KAP) survey conducted under Project Axshya, funded by The Global Fund Round 9 India TB grant. A complete report of the survey is available elsewhere.12
Selection of study sites
The survey used a multistage cluster sampling methodology. The country was first divided into four zones (north, south, east and west). In each of these zones, 11–12 districts were selected by population proportionate to estimated size sampling (PPES) methodology. Each selected district was sub-divided into primary sampling units of ~250 households (separately for urban and rural areas) based on the population data from the Registrar General of India (http://www.censusindia.gov.in/). Ten primary sampling units were randomly selected in each district; the ratio of urban to rural primary sampling units was in proportion to the urban to rural population of the district.
Study population
PHCPs were defined as the health care personnel available within the primary sampling units identified by the community as their first point of contact for any medical care. In India, these providers include qualified public or private practitioners (allopathic or alternative systems of medicine), unqualified practitioners (informal providers), chemists (who often provide medications without prescriptions), nurses and health workers such as auxiliary nurse midwives (ANM), anganwadi workers and accredited social health activists (ASHA) involved in public health programmes.
Data collection
All identified PHCPs were interviewed by trained field investigators from a research agency (GfK India) using a semi-structured questionnaire. The respondents were shown photographs of commonly available POC tests, such as pregnancy test kits and glucometer devices, to ensure that they understood what the survey staff meant by POC tests.
Data management and analysis
The data were double entered in CSPro (US Census Bureau, Washington, DC, and ICF International, Fairfax, VA, USA, version 5.0.2), and analysed using EpiData version V2.2.2.182 (EpiData Association, Odense, Denmark). The data are summarised using simple proportions and confidence intervals.
Ethics
The study was approved by the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, and the Independent Ethics Committee of the Resource Group for Education and Advocacy for Community Health (REACH), Chennai, India.
RESULTS
A total of 767 PHCPs were identified. Table 1 provides a breakdown of the types of providers interviewed. Of the 767 providers, 186 (24%, 95% confidence interval 21–27) reported using any form of rapid POC test. POC testing was most commonly used for pregnancy, followed by malaria and blood glucose. Public sector providers reported greater use of rapid tests for malaria than private providers ((39% vs. 20%, P < 0.05) (Figure). POC tests were also used for other conditions, such as typhoid, TB, HIV, hepatitis, syphilis, influenza and dengue.
TABLE 1.
Types of primary health care providers and their use of POC tests
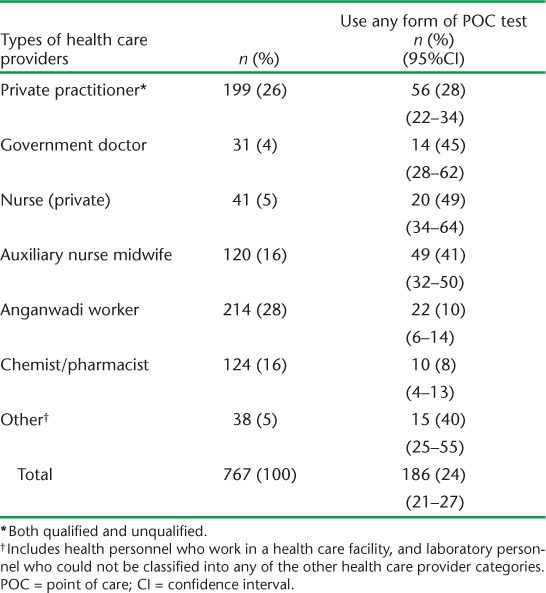
FIGURE.
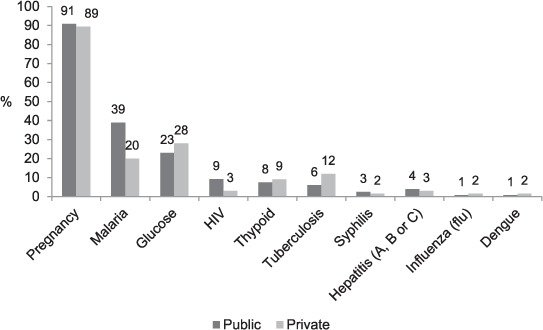
Conditions for which point-of-care tests were used by public (n = 120) and private (n = 66) primary health care providers. HIV = human immunodeficiency virus.
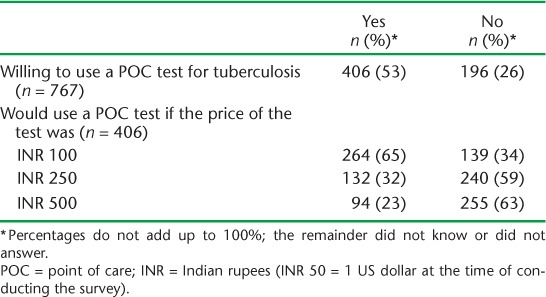
When asked about the need for a POC test for TB, 53% said they would use it if it was available free of charge. Of these, 65% reported they would still use it if it were priced at about INR 100 (~US$ 2.00), 32% if it were priced at around INR 250 and 23% if it were priced at INR 500 (INR 50~US$ 1.00) (Table 2).
TABLE 2.
Willingness of primary health care providers to use a POC test for tuberculosis
DISCUSSION
This is one of the first community-based surveys to assess the use of POC tests by PHCPs in India, and the data suggest one in four have used them in the past. A major limitation is that the information is based on self-reporting by the respondents, which we could not cross-verify with any records or observations.
Our definition of PHCPs included paramedical workers. Most of the public sector paramedical workers are primarily involved in delivering maternal and child-health related services, and rapid tests for pregnancy were therefore commonly used. Nearly 8% of the respondents reported that they used rapid POC tests for TB, most likely antibody-based serological tests that were banned by the Government of India in 2012, a few months before the survey began. The use of POC tests by private practitioners was surprisingly low (26%). This could be due to the preference of these providers to refer patients to local laboratories with whom they have established relations, including financial incentives.13
About half of the PHCPs were willing to use POC tests for TB if provided free of charge or at a low price (<US$ 2.00 per test). This information may be useful for product developers interested in the POC testing market in India. As the use of antibody-based serological tests is banned, there is a potential demand for an accurate POC test in the private sector. Although sputum smears are performed in about 13 000 microscopy centres located within health facilities, there are currently no options for TB testing at community level in the public health system, and a good POC test may be very helpful.
CONCLUSION
The use of POC tests by PHCPs in India is limited. However, providers did seem interested and willing to use a POC test for TB (when made available), provided the cost were low. Further research is necessary to understand the reasons for limited use, and to identify barriers to future POC testing for TB.
Acknowledgments
The survey was conducted as a part of the mid-project knowledge, attitude and practice survey conducted by Project Axshya, supported by the Global Fund. Additional funding for the point-of-care testing component was provided by the Bill and Melinda Gates Foundation (grant OPP1061487). SS is a recipient of a studentship award from the Canadian Thoracic Society, July 2014–June 2015. MP is a recipient of a salary award from the Fonds de Recherche du Québec – Santé.
Footnotes
Conflicts of interest: none declared.
References
- 1.Kost G J. Point-of-care testing. Encyclopedia of Analytical Chemistry. Chichester, West Sussex, UK: Wiley Online Library; 2006. [Google Scholar]
- 2.Nichols J H. Point of care testing. Clin Lab Med. 2007;27:893–908. doi: 10.1016/j.cll.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Kost G J. Guidelines for point-of-care testing. Improving patient outcomes. Am J Clin Pathol. 1995;104(Suppl):S111–S127. [PubMed] [Google Scholar]
- 4.Pai N P, Vadnais C, Denkinger C, Engel N, Pai M. Point-of-care testing for infectious diseases: diversity, complexity, and barriers in low- and middle-income countries. PLOS Med. 2012;9:e1001306. doi: 10.1371/journal.pmed.1001306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dooley J F. Point-of-care diagnostic testing markets. Point of Care. 2009;8:154–156. [Google Scholar]
- 6.Jones C H, Howick J, Roberts N W et al. Primary care clinicians' attitudes towards point-of-care blood testing: a systematic review of qualitative studies. BMC Fam Pract. 2013;14:1–9. doi: 10.1186/1471-2296-14-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Global Tuberculosis Report 2013. Geneva, Switzerland: WHO; 2013. WHO/HTM/TB/2013.11. http://www.who.int/tb/publications/global_report/en/ Accessed October 2014. [Google Scholar]
- 8.McNerney R, Daley P. Towards a point-of-care test for active tuberculosis: obstacles and opportunities. Nat Rev Microbiol. 2011;9:204–213. doi: 10.1038/nrmicro2521. [DOI] [PubMed] [Google Scholar]
- 9.Denkinger C M, Pai M. Point-of-care tuberculosis diagnosis: are we there yet? Lancet Infect Dis. 2012;12:169–170. doi: 10.1016/S1473-3099(11)70257-2. [DOI] [PubMed] [Google Scholar]
- 10.Peeling R, Mabey D. Point-of-care tests for diagnosing infections in the developing world. Clin Microbiol Infect. 2010;16:1062–1069. doi: 10.1111/j.1469-0691.2010.03279.x. [DOI] [PubMed] [Google Scholar]
- 11.Kik S V, Denkinger C M, Casenghi M, Vadnais C, Pai M. Tuberculosis diagnostics: which target product profiles should be prioritised? Eur Respir J. 2014;44:537–540. doi: 10.1183/09031936.00027714. [DOI] [PubMed] [Google Scholar]
- 12.Sagili K D. Knowledge, attitude and practice about tuberculosis in India. A midline survey, 2013. Project Axshya. New Delhi, India: International Union Against Tuberculosis and Lung Disease South East Asia Office; 2014. http://www.axshya-theunion.org/images/documents/kap-midline.pdf Accessed October 2014. [Google Scholar]
- 13.Jaroslawski S, Pai M. Why are inaccurate tuberculosis serological tests widely used in the Indian private healthcare sector? A root-cause analysis. J Epidemiol Glob Health. 2012;2:39–50. doi: 10.1016/j.jegh.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


