Abstract
Background:
Although various therapies used for the treatment of psoriasis are able to produce remission, yet relapses, a common problem, remains frequent. It was observed that treatment with intermittent high dose (IHD) and continuous low dose (CLD) azathioprine can produce prolonged and durable remission in psoriasis.
Aims:
To see the long term effect of azathioprine pulse therapy (APT) in psoriasis.
Methods:
Ten patients with psoriasis who has completed more than 5 years in remission with azathioprine pulse therapy are being taken in the study. They were given IHD azathioprine (500 mg on 3 consecutive days which is repeated every month) with CLD azathioprine (100 mg orally) daily in between IHD. The entire treatment schedule was divided into four phases. During phase I, treatment with IHD and CLD azathioprine was started and continued till complete clearance of lesions after which, patients proceeded to Phase II. In phase II, they continued to get treatment with IHD and CLD. After continued remission for a period of nine months, they entered into phase III, when the treatment with IHD was stopped, but CLD continued. If there was no recurrence after nine months of phase III treatment, CLD was also withdrawn, and patients were followed-up without any treatment (Phase IV).
Results:
All 10 patients completed treatment and are in remission for more than five years without any treatment.
Conclusions:
Out of 60 patients in phase IV, 10 patients were in continuous remission for more than five years, after all treatment had been stopped. Thus, azathioprine pulse therapy regimen produces prolonged remission in psoriasis.
Keywords: Azathioprine pulse therapy, continuous low dose azathioprine, intermittent high dose azathioprine, methotrexate, prolong remission, psoriasis
What was known?
Relapses in psoriasis are a frequent problem.
Introduction
Therapies[1,2,3] and therapeutic regimens[4,5,6] used for the treatment of psoriasis, cleared the lesions but were unable to prevent relapses. Our personal experience with psoriasis has been the same.[7] Psoriasis is caused by activated T lymphocyte cells, which produce cytokines. Cytokines lead to the proliferation of keratinocytes responsible for development of psoriasis.[8] Azathioprine is known to suppress activated T lymphocyte cells, which in turn stop production of cytokines that ultimately stop the proliferation of keratinocytes responsible for development of psoriasis. To achieve fast clearance of the lesions as well as prolong period of remission, in 2003, the author had started using an arbitrarily designed regimen of azathioprine which uses an intermittent high dose (IHD) azathioprine (500 mg on 3 consecutive days, repeated every month) in combination with continuous low dose (CLD) azathioprine (100 mg orally daily) given in between IHD.
The entire treatment was divided into four phases.[9] During phase I, treatment with IHD and CLD azathioprine was continued until the clearance of lesions. Once the lesions cleared completely [Figure 1], patient would proceed to Phase II, while continuing IHD and CLD azathioprine. After the patient had remained lesions free for a period of 9 months, treatment with IHD azathioprine was stopped, but CLD azathioprine continued (Phase III). Subsequently, after 9 months of phase III treatment with no recurrence, CLD azathioprine was also withdrawn, and patients were followed up without any treatment (Phase IV). This process is known as Azathioprine Pulse Therapy (APT) regimen.
Figure 1.

Psoriasis leg after treatment
Out of 60 patients of psoriasis who have completed the treatment with APT regimen and are in phase IV, 10 patients who have been in continuous clinical remission for the last 7 to 10 years and without any treatment for the last 5.5-8.25 years are being reported. The rest have not yet crossed the five years after treatment was stopped.
Purpose of this communication is to report long term effect of APT in psoriasis which is very important before claiming that a regimen is available,[10] which is able to put psoriasis, a universally recurrent disease into prolonged or permanent remission.
Materials and Methods
Diagnosis of psoriasis was made clinically [Figure 2]; histopathology [Figure 3] was done in some patients only. Laboratory evaluation included hemoglobin, total and differential leukocyte counts, platelet counts, erythrocyte sedimentation rate, blood urea, creatinine, SGOT, SGPT and alkaline phosphatase. These investigations were done in all patients before starting treatment and regularly before giving IHD. Psoriasis Area Severity Index (PASI) was charted in each patient. Thiopurine S-methyltransferase (TPMT) enzyme screening was done before starting the treatment. X-ray was taken in patients having pain in the joints. Patient with active systemic disease like hepatitis, cirrhosis of liver, acute and chronic nephritis etc., malignancy, pregnant women, lactating mother and children were excluded from the study. Informed written consent was taken from each patient. Ethical approval was obtained from the Institution Ethics Committee of Prayatna.
Figure 2.

Psoriasis leg before treatment
Figure 3.
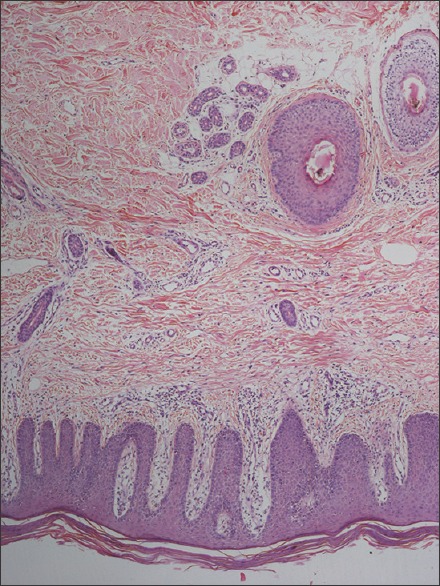
Histopathology of psoriasis lesion (H and E, ×10)
Initially to clear the lesion fast and in pustular psoriasis, erythrodermic psoriasis and extensive plaque psoriasis methotrexate (MTX) 15 mg per week[3] and topical coal tar 6%[1] was also used in phase I as azathioprine takes few weeks to start acting.
All previous treatments were stopped four weeks before starting APT.
Results
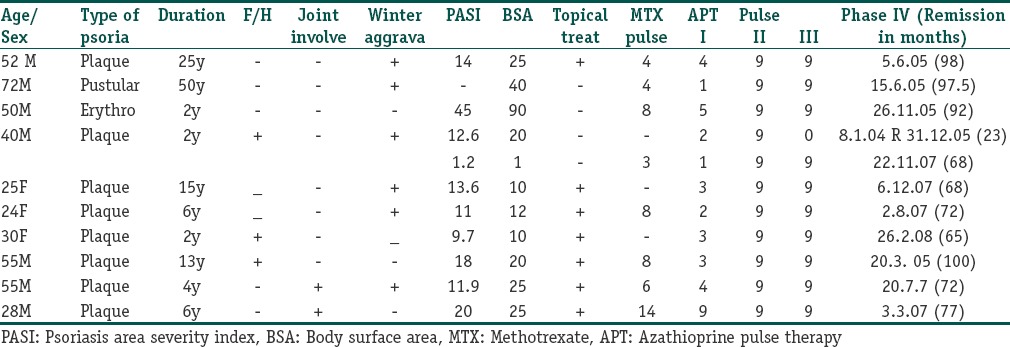
Salient features of all the ten patients are shown in Table 1. Before coming to us, they were given MTX, coal tar and PUVA with relapses at variable interval. In addition to APT, seven patients also received topical coal tar 6% ointment and eight patients were given oral MTX 15 mg per week, for 3-12 courses during Phase I, which varies from 1-4 months. This helps the patient clearing the lesions fast. One patient showed sclerosis in articular and subarticular portion of interphalyngial joint consistent with psoriatic arthritis of right ring finger on X-ray which was cleared with APT regimen in seven months duration. Two patients had onycholysis of few fingernails. This cleared in three months with APT. The duration of continuous remission in all patients is more than five years (maximum eight years) after stopping the APT regimen.
Table 1.
Details of psoriasis patients treated with azathioprine pulse therapy
Relapse
One patient relapsed (case no. 4) after being in phase IV for 23 months. He was restarted with APT and is in phase IV since 64 months.
Side effects
Common side effects seen were nausea and vomiting in two patients, which was treated with prochlorperazine hydrochloride 5 mg thrice daily in 1-2 days; weakness and fatigue in two patients 2-5 days after IHD regimen, which last for 2-3 days; elevated liver function tests in one patient in phase I, leucopenia in one patient in phase I, which returned to normal in three weeks after stopping azathioprine.
Discussion
It is usually believed that complete and durable remission of psoriasis is extremely difficult to obtain. Our findings suggest that it may be possible to induce long term remission by using a regimen of intermittent high dose (IHD) and continuous low dose (CLD) azathioprine. Duration of post-treatment disease free period in our case has been more than five years (5-8 years) in all the 10 patients reported.
Systemic azathioprine has been extensively investigated for the treatment of psoriasis. In 1961 Kravetz and Balsam[11] for first time used azathioprine in psoriasis; they used 2 mg/kg daily in 12 patients, 1-4 courses with improvement. In majority of the patients, it relapsed within 1.5-6 months after the last dose. In 1970, Greaves and Dauber[12] used 2.5 mg/kg/day for 6 weeks in 10 patients with 25% clearance of the lesions in 5 patients within 2-6 weeks duration. Relapse was seen 1 month after stoppage of azathioprine. Fledges and Barnes[13] in 1974 used 2.5 mg/kg/day in 10 patients for 4 ½ months to 5 ½ years with almost complete clearance of skin lesions in 6 patients. Azathioprine was discontinued after remission lasting for 1 year. However, the lesions relapsed after stoppage of treatment. In 1974, Du Vivier et al.[14] used 100-300 mg azathioprine daily for 2-24 weeks with 75-100% clearance of psoriasis lesions with maintenance dose of 75-200 mg daily in 13 out of 29 patients. One patient who was free of the lesions developed relapse 6 months after complete stoppage of azathioprine. Lee et al.[15] used 200-300 mg azathioprine daily for 12-24 months in psoriatic arthritis with improvement with few transient side effects. In a recent review in 2008, Halverstam and Lebwohl[16] and Menter et al.[17] reported usefulness of azathioprine in psoriasis quoting all the above work.
Higher doses of azathioprine in pulse form (800 mg daily on 3 consecutive days repeated every month and 200 mg daily in between for 12-24 months) have recently been evaluated in limited patients with Wegner's granulomatosis and lupus nephritis[18,19] with very few side effects. The present study lies in using IHD and CLD azathioprine in aforementioned dosage schedule.
The duration of the initial treatment with IHD and CLD azathioprine (Phase I) in our experience was variable and did not seem to depend upon factors such as the initial severity or the extent of the disease. However, once the patient went into the remission phase (Phase II), the disease generally remained in remission. Only non-compliant patients continued to have relapses of their disease. Adverse events observed were generally minor and reversible but additional experience is necessary with particular emphasis on hematological and hepatic parameters.
Our choice of drugs, their dosage and duration of different phases of treatment, especially phase II and III, were arbitrary. There is ample scope for further modification to establish the most appropriate regimen.
A relapse after receiving complete and regular treatment or during treatment does not mean that APT therapy has failed completely. A second course of APT regimen in such cases usually achieves the desired result as happened to our fourth case, who developed relapse during phase IV and was subsequently treated with second course of APT regime.
In summary, treatment with IHD and CLD azathioprine regimen can induce durable clinical remission in patients with psoriasis with an acceptable safety profile as shown in this report.
What is new?
Psoriasis can be put in prolong remission by APT pulse regimen.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Lebwohl M, Abel E, Zanolli M, Koo J, Drake L. Topical therapy for psoriasis. Internat J Dermatol. 1995;34:673–84. [PubMed] [Google Scholar]
- 2.Jain S, Sehgal VN. Psoriasis and calcipotriol: An overview. Int J Dermatol. 1997;36:255–8. doi: 10.1046/j.1365-4362.1997.00030.x. [DOI] [PubMed] [Google Scholar]
- 3.Roenigk HH, Jr, Auerbach R, Maibach HI, Weinstein GD. Methotrexate in psoriasis: Revised guidelines. J Am Acad Dermat. 1988;19:145–56. doi: 10.1016/s0190-9622(88)80237-8. [DOI] [PubMed] [Google Scholar]
- 4.Morison WL, Momtaz K, Parrish JA, Fitzpatrick TB. Combined methotrexate-PUVA therapy in the treatment of psoriasis. J Am Acad Dermatol. 1982;6:46–51. doi: 10.1016/s0190-9622(82)70005-2. [DOI] [PubMed] [Google Scholar]
- 5.Roenigk HH., Jr Acitretin combination therapy. J Am Acad Dermatol. 1999;41:S18–21. doi: 10.1016/s0190-9622(99)70361-0. [DOI] [PubMed] [Google Scholar]
- 6.Lebwohl M, Ellis C, Gottlieb A, Koo J, Krueger G, Linden K, et al. Cyclosporine consensus conference: With emphasis on the treatment of psoriasis. J Am Acad Dermatol. 1998;39:464–75. doi: 10.1016/s0190-9622(98)70325-1. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R, Gupta S. Methotrexate-betamethasone weekly oral pulse in psoriasis. J Dermatol Treat. 2007;18:291–4. doi: 10.1080/09546630701487643. [DOI] [PubMed] [Google Scholar]
- 8.Das RP, Jain AK, Ramesh V. Current concepts in the pathogenesis of psoriasis. Indian J Dermatol. 2009;54:7–12. doi: 10.4103/0019-5154.48977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta R. Can psoriasis be cured. Delhi Medical Asso. News Bull May. 2013;10:22. [Google Scholar]
- 10.Gupta R. Azathioprine pulse therapy in the treatment of psoriaisis. J Pakistan Asso Dermatologists. 2013;23:120–5. [Google Scholar]
- 11.Kravetz RE, Balsam T. Treatment of psoriasis with mercaptopurine. Arch Dermatol. 1961;84:597–600. doi: 10.1001/archderm.1961.01580160061008. [DOI] [PubMed] [Google Scholar]
- 12.Greaves MW, Dawber R. Azathioprine in psoriasis. Br Med J. 1970;2:237–8. doi: 10.1136/bmj.2.5703.237-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feldges DH, Barnes CG. Treatment of psoriatic arthropathy with either azathioprine or methotrexate. Rheumatol Rehabil. 1974;13:120–4. doi: 10.1093/rheumatology/13.3.120. [DOI] [PubMed] [Google Scholar]
- 14.Du Vivier A, Munro DD, Verbov J. Treatment of psoriasis with azathioprine. Br Med J. 1974;1:49–51. doi: 10.1136/bmj.1.5897.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JC, Gladman DD, Schentag CT, Cook RJ. The long-term use of azathioprine in patients with psoriatic arthritis. J Clin Rheumatol. 2001;7:160–5. doi: 10.1097/00124743-200106000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Halverstam CP, Lebwohl M. Nonstandard and off-label therapies for psoriasis. Clin Dermatol. 2008;26:546–53. doi: 10.1016/j.clindermatol.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 17.Menter A, Korman NJ, Elments CA, Feldman SR, Gelfand JM, Gordon KB, et al. Guidelines of care for the management and treatment of psoriasis with traditional systemic agents. J Am Acad Dermatol. 2009;61:451–85. doi: 10.1016/j.jaad.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 18.Benenson E, Fries JW, Heilig B, Pollok M, Rubbert A. High-dose azathioprine pulse therapy as a new treatment option in patients with active Wegener's granulomatosis and lupus nephritis refractory or intolerant to cyclophosphamide. Clin Rheumatol. 2005;24:251–7. doi: 10.1007/s10067-004-1002-8. [DOI] [PubMed] [Google Scholar]
- 19.Aries PM, Hellmich B, Reinhold-Keller E, Gross WL. High-dose intravenous azathioprine pulse treatment in refractory Wegener's granulomatosis. Rheumatology (Oxford) 2004;43:1307–8. doi: 10.1093/rheumatology/keh300. [DOI] [PubMed] [Google Scholar]


