Abstract
Background:
Suction blister epidermal grafting (SBEG) is one of the most commonly performed types of vitiligo surgery for stable vitiligo. The advantages of SBEG include cost-effectiveness and a relatively easier learning curve for the surgeon.
Aims:
To evaluate the outcome in terms of both recipient and donor site changes, on long-term follow-up of the patients who underwent SBEG in our center.
Methods:
Thirty patients, 21 females and 9 males ages ranging from 9 to 55 years, all having either stable vitiligo not responding to medical line of treatment, were included in the study done which involved a variable follow-up period ranging from 2 to 62 months (mean 23.6, standard deviation 17.79). SBEG was done as day care procedure. The patients were reviewed after 1-week and thereafter followed-up in the subsequent months and years. The results of the procedures were graded as poor (0–24%), fair (24–64%), good (64–94) and excellent (95–100%) depending on the patient satisfaction. Donor site changes were also analyzed.
Results:
The face and lips showed an excellent result and color match and persistent pigment retention. The larger areas, especially the lesions on the limbs showed comparatively less response. Of the total, 6.7% showed poor, 13.3% fair, 30% good and 50% excellent response to treatment. Patient satisfaction wise, 53.3% of the patients were very happy, 26.7% were happy, 10% satisfied and 10% unhappy. Significant positive correlation between patient satisfaction and physician observation was seen (Spearman's rho 0.866).
Conclusions:
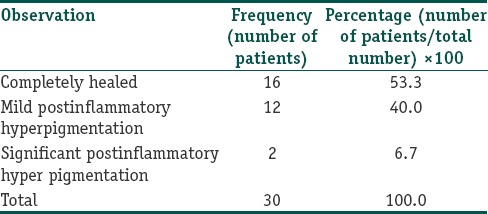
In spite of recent advances in surgical modalities like cellular grafting, SBEG continues to be a good, cost-effective, surgical method of treating vitiligo especially on the face and lip. The donor site also tends to show good healing tendency with minimal scarring and postinflammatory pigmentation.
Keywords: Segmental vitiligo, suction blister epidermal grafting, suction blister roof grafting, vitiligo surgery
What was known?
Suction blister epidermal grafting is a good surgical method of treating vitiligo especially on the face and lip. With less demand for technical expertise and laboratory investments, this method is still a cheap and effective choice of vitiligo surgery in indicated cases with excellent cosmetic results and patient satisfaction.
Introduction
There are very few studies in Indian literature that have assessed long-term follow-up of both recipient and donor sites after suction blister epidermal grafting (SBEG). This study was conducted to evaluate the outcome in long-term follow of the patients who underwent SBEG for various types of surgically indicated cases of vitiligo across all age groups who presented to our dermatology outpatient for treatment and also to evaluate the status of the donor site on long-term follow-up after surgery.
Methods
All the patients who underwent SBEG in our department during the period from January 2008 to December 2013 were included in the study. The maximum time on follow-up was 62 months and the least on follow-up was 2 months (mean 23.6, standard deviation 17.79). SBEG was performed in the standard method. Blisters were created using a 10 cc syringe connected to three-way stop cannula at the nozzle end and application of negative pressure using a 50 cc syringe.[1] [Figure 1]. Thirty patients (21 females and 9 males) with stable or segmental vitiligo were inducted into the study. The age of the patients ranged from 9 to 55 years. The donor area was the outer aspect of the thigh in 22 patients and inner aspect of the arm in 8 patients.
Figure 1.
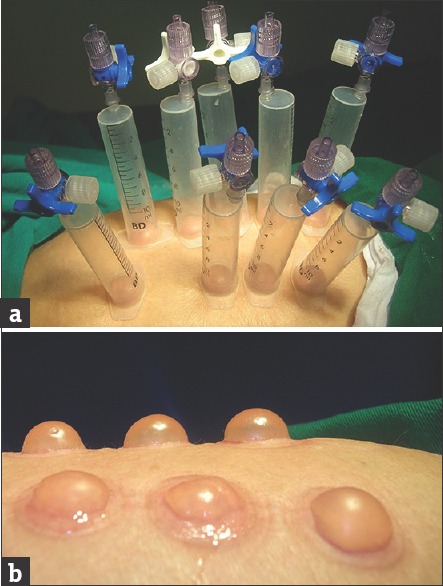
(a) 10 CC syringes in places with the three-way cannula as the suction blister raising mechanism. (b) Formed blisters ready for roof harvesting
The procedure was done under local anesthesia in a day care setting, and there were no untoward events during the immediate postoperative period. All the patients were reviewed after 1-week and thereafter in the subsequent months and years. Photographic documentation of the donor and recipient site were done for every patient visit to the hospital. The patients were not advised specifically to take phototherapy after the procedure. In the month of December 2013 (the observation time of the study), all the patients were contacted by telephone, letter or E-mail and asked to review in the dermatology outpatient department. Twenty-six patients responded to the request. In those who did not respond (4 patients), the finding on their last visit as per the medical records and photographs available with us were taken into consideration.
Patients were interviewed, examined and evaluated based on the questionnaire and doctor observation for re-pigmentation was graded as excellent with 95–100% pigmentation, good with 65–94%, fair with 25–64% and poor with 0–24% of the treated area.[2] Patient satisfaction was graded as “very happy,” “happy,” “satisfactory” and “unhappy.” Donor area was examined for pigmentary change (hyper or hypopigmentation) and also keloidal changes or hypertrophic scars.
Results
Observations
The mean age was 24.17. The face and lips showed an excellent result, color match and persistent pigment retention [Figures 2 and 3]. The larger areas, especially the lesions on the limbs showed comparatively less response. Of the total, 6.7% showed poor, 13.3% fair, 30% good and 50% excellent response to treatment [Table 1]. Patient satisfaction wise, 53.3% of the patients were very happy, 26.7% were happy, 10% satisfied and 10% unhappy [Table 2]. Donor area showed complete healing in 53.3%, mild postinflammatory hyperpigmentation in 40% and significant postinflammatory hyperpigmentation in 6.7%. There were no keloids or hypertrophic scars in any of the patients [Figure 4 and Table 3].
Figure 2.
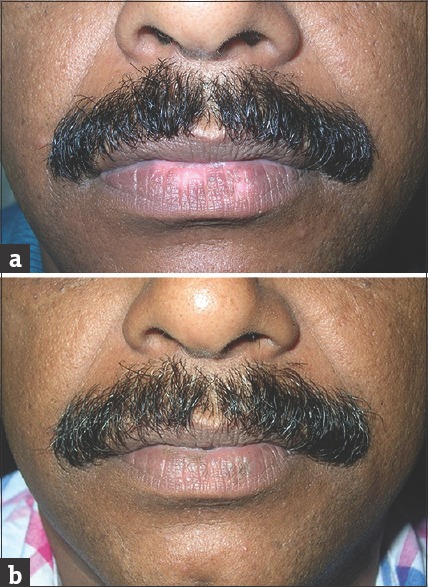
Vitiligo of the lower lip (a) before surgery (b) fully repigmented and normalized after surgery
Figure 3.
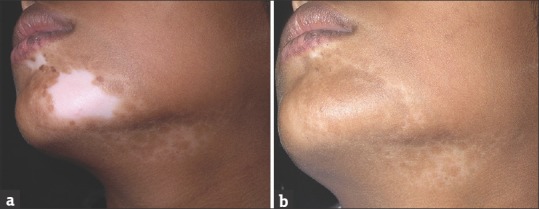
Segmental vitiligo of the face. A near total re-pigmentation with excellent color match
Table 1.
Doctors observation
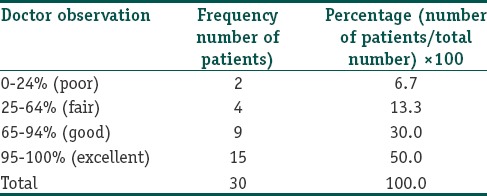
Table 2.
Patient satisfaction
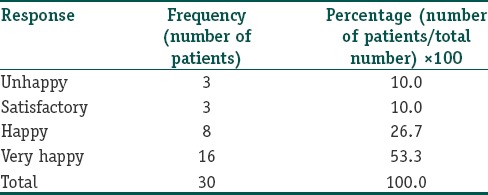
Figure 4.
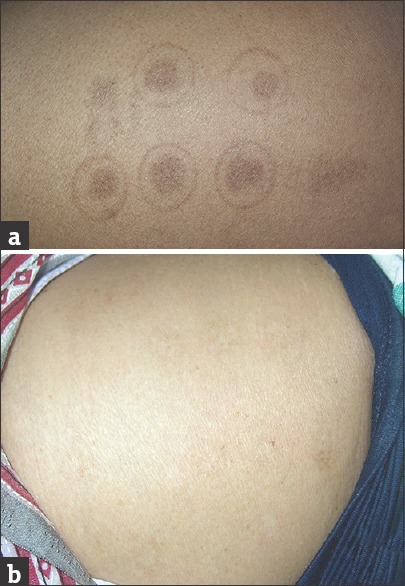
Donor site. Later aspect of the thigh. (a) Hyperpigmentation and (b) Normalized and unidentifiable
Table 3.
Donor area changes
A significantly positive correlation was seen between patients’ satisfaction and physician observation (Spearman's rho 0.866, P = 0.0001, significant at 5% level of significance). There was no significant correlation between age of the patient and doctor observation (Spearman's rho 0.008, the P = 0.892,) as well as age of the patient and patient satisfaction (Spearman's rho 0.118, P = 0.536).
A significant positive correlation was seen between site and donor area changes (Spearman's rho 0.482, P = −0.007, significant at 5% level of significance). There was no significant correlation between Age of the patient and donor area changes (Spearman's rho 0.104, P = 0.583 at 5% level of significance).
Discussion
Vitiligo is an autoimmune disorder that affects all ages and is prevalent in all skin types and age groups. The condition is highly refractory and with varied results outcome to treatment. When vitiligo becomes stable and also refractory to medical therapy, surgical therapies are indicated. The common indications for vitiligo surgery are patients with stable vitiligo not responding to medical treatment or causing severe psychosocial distress, patients with leukoderma due to burns, piebaldism, inactive discoid lupus erythematosus, and other stable disease states causing permanent depigmentation.[3,4]
Assessment of stability is usually done based on clinical criteria like: Lack of progression of old lesions within the past 2 years, no new lesions developing within the same period and absence of a recent Koebner phenomenon. Test grafting at various sites in different time intervals is another option to assess the stability factor. Analysis of cellular stability is yet another option that is cumbersome and needs expensive laboratory facilities and expertise.[5]
The different surgical modalities used for vitiligo have their own pros and cons. SBEG is one of the best surgical modalities of treating stable nonsegmental vitiligo and segmental vitiligo with the advantages that it is a “scar less” surgery as both recipient and donor sites heal without the slightest scarring and donor sites can repeated for several sessions. Being a purely epidermal graft, there is no “stuck-on” effect. Color and texture match with the surrounding skin is generally good.[6] The procedure involves induction of blister on the donor area (usually the outer thigh or the inner arms) using multiple syringes connected with three-way stop cannulas at their nozzle end and application of negative pressure using a larger syringe.[1] The recipient area can be abraded manually or with a motorized dermabrader and in addition recipient sites on mucosal sites can be prepared by inducing a phototoxic blister.[7] The patients can then be started on phototherapy to improve postgraft results.
Many of our patients showed very good results post-SBEG even without postgraft phototherapy. Blister grafting has shown to given good results even without postgraft phototherapy in other studies too.[8] With the advent of newer and effective modalities of treatment for stable vitiligo, like autologous melanocyte transfer, the role of relatively older techniques like SBEG has become debatable. However, with our study we would like to reiterate the importance of SBEG as a very effective therapeutic modality for localized and stable vitiligo lesions, especially in the context of resource poor settings. Autologous melanocyte transfer (both cultured and noncultured) has a bigger learning curve, requires more resources – laminar flow, specific reagents and centrifuge etc., whereas SBEG can be done with very minimal resources. This indirectly also means that the cost transferred to the patient will also be less in the case of suction blister grafting.
The main issue would be whether the results of the two procedures are comparable. There are not many controlled studies available which answer this, but our study suggests that, in general, the results of suction blister technique are good to excellent from both the objective re-pigmentation viewpoint and the patient satisfaction viewpoint.
The main limitation of our study is the small sample size and the variable follow-up period. Further controlled studies are warranted in comparing the actual re-pigmentation (time and amount) between suction blister grafting and autologous melanocyte transfer techniques over a uniform and long period.
We conclude that for small and localized lesions especially on the face and lip, suction blister grafting should be considered as an equally viable option compared to autologous melanocyte transfer. The donor site also tends to heal well in general, and postinflammatory pigmentary changes and scarring tends to be minimal.
Suction blister grafting is an effective and simple method of surgical correction for localized, stable vitiligo, especially in resource poor settings.
What is new?
The study highlights that SBEG still has a role in the context of availability of newer surgical modalities like cellular grafting for vitiligo.
Acknowledgements
Mr. Girish Kumar, Assistant Professor. Department of Statistics, Government Arts and Science College, Meenchanda Kozhikode for the statistical analysis of the raw data
Mrs. Sreedevi and Ms. Rajeena, Nursing Staff, Department of Dermatology, KIMS Al Shifa Super Speciality Hospital for assistance during the surgeries and follow-up evaluation of the patients.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Gupta S, Ajith C, Kanwar AJ, Kumar B. Surgical pearl: Standardized suction syringe for epidermal grafting. J Am Acad Dermatol. 2005;52:348–50. doi: 10.1016/j.jaad.2004.06.041. [DOI] [PubMed] [Google Scholar]
- 2.Mulekar SV. Long-term follow-up study of 142 patients with vitiligo vulgaris treated by autologous, non-cultured melanocyte-keratinocyte cell transplantation. Int J Dermatol. 2005;44:841–5. doi: 10.1111/j.1365-4632.2005.02226.x. [DOI] [PubMed] [Google Scholar]
- 3.Falabella R. Surgical approaches for stable vitiligo. Dermatol Surg. 2005;31:1277–84. doi: 10.1111/j.1524-4725.2005.31203. [DOI] [PubMed] [Google Scholar]
- 4.Khunger N, Kathuria SD, Ramesh V. Tissue grafts in vitiligo surgery – Past, present, and future. Indian J Dermatol. 2009;54:150–8. doi: 10.4103/0019-5154.53196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lahiri K, Malakar S. The concept of stability of vitiligo: A reappraisal. Indian J Dermatol. 2012;57:83–9. doi: 10.4103/0019-5154.94271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta S, Goel A. Suction blister epidermal grafting. In: Gupta S, editor. Surgical Management of Vitiligo. 1st ed. New Delhi: Wiley India; 2007. pp. 96–107. [Google Scholar]
- 7.Shenoi SD, Srinivas CR, Pai S. Treatment of stable vitiligo with autologous epidermal grafting and PUVA. J Am Acad Dermatol. 1997;36:802–3. doi: 10.1016/s0190-9622(97)80358-1. [DOI] [PubMed] [Google Scholar]
- 8.Maleki M, Banihashemi M, Sanjari V. Efficacy of suction blister epidermal graft without phototherapy for locally stable and resistant vitiligo. Indian J Dermatol. 2012;57:282–4. doi: 10.4103/0019-5154.97669. [DOI] [PMC free article] [PubMed] [Google Scholar]


