Abstract
Eyelash trichomegaly is increased length, curling, pigmentation or thickness of eyelashes. Various causes include congenital syndromes, acquired conditions and drugs. It can manifest at birth or present later in life. It can form a part of spectrum of manifestations of some congenital syndromes. Although it tends to have a benign course, it can lead to psychological disturbances and can result in corneal abrasions and visual disturbances, if trichiasis occurs. This article focuses on its etiology, pathogenesis and brief management.
Keywords: Trichomegaly, HIV, latanoprost
What was known?
Causes of trichomegaly.
Management of trichomegaly.
Introduction
Eyelash trichomegaly is defined as increase in length (12 mm or more), curling, pigmentation or thickness of eyelashes.[1,2] The term “trichomegaly” was first used by Gray in 1944. Various causes of trichomegaly include congenital, familial, acquired and drugs. Eyelash trichomegaly can be psychologically disturbing and may lead to corneal abrasions and visual disturbances, if trichiasis occurs.[3,4]
Eyelash growth
During embryological development, eyelashes are the first terminal hairs to appear. Their growth cycle lasts approximately 5-6 months, with a very short anagen phase (30 days) and a relatively long telogen phase (approximately 4-5 months).[1] Eyelashes and eyebrows have the lowest ratio of anagen to telogen hair follicles, with approximately 50% of eyelashes in the anagen phase compared with 85–90% of scalp hairs.
The epidermal growth factor receptor appears to play a crucial role in hair growth as evidenced by drugs that inhibit its function. In addition, prostaglandins have been shown to be able to convert the hair follicle from the telogen phase into the anagen phase.[5]
Congenital conditions associated with eyelash trichomegaly
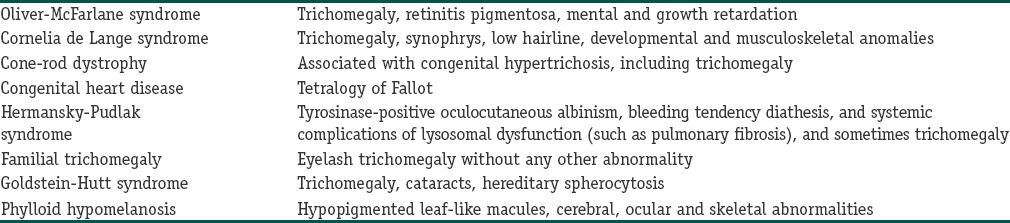
Among various congenital conditions associated with eyelash trichomegaly [Table 1], only two include it as a defining diagnostic feature: Oliver-McFarlane syndrome and Cornelia de Lange syndrome.
Table 1.
Congenital conditions associated with eyelash trichomegaly
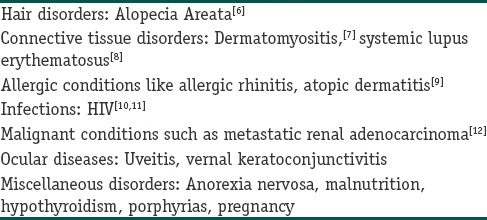
Acquired conditions associated with eyelash trichomegaly
In HIV trichomegaly has been observed to occur in association with late-stage disease. Eyelash length has been shown to normalize as patients respond to anti-retroviral therapy.[13] However, no association has been seen between the length of eyelashes and either the severity or prognosis of HIV infection. Acquired conditions associated with eyelash trichomegaly is mentioned in [Table 2].
Table 2.
Acquired conditions associated with eyelash trichomegaly
Drugs associated with eyelash trichomegaly
Prostaglandin analogues like latanoprost, bimatoprost: Most commonly reported cause of eyelash trichomegaly.
Epidermal growth factor receptor inhibitors: cetuximab,[14] Panitumumab; tyrosine kinase inhibitors: erlotinib,[15] gefitinib[16]
Interferon-α2b[17]
Zidovudine
Phenytoin
Diazoxide, minoxidil
Acetazolamide
Cyclosporine, tacrolimus
Topiramate
Psoralens
Corticosteroids
Streptomycin
Penicillamine
Epidermal growth factor receptor inhibitors
Epidermal growth factor receptor inhibitors are used to treat a variety of solid tumors like bladder, breast, colorectal, head and neck, lung, and ovarian cancers. There are two classes of drugs that target the epidermal growth factor receptor: monoclonal antibodies that block the receptor itself (cetuximab, panitumumab) and small molecules that inhibit the tyrosine kinase activity, thereby blocking receptor activation (gefitinib, erlotinib).
Trichomegaly induced by EGFR inhibitors, a result of enhanced terminal differentiation, usually occurs after 2-5 months of treatment, and can be associated with hypertrichosis in other areas.
The cutaneous adverse effects of these agents have been grouped into a condition known as PRIDE (papulopustules and/or paronychia, regulatory abnormalities of hair growth, itching, and dryness due to epidermal growth factor receptor inhibitors) syndrome.[18]
The authors postulated that, in a similar way that the presence of erlotinib-induced rash has been correlated with tumor response, the presence of eyelash trichomegaly might also be used as a useful clinical tool to assess for antineoplastic therapy success.[19]
Interferon alpha
The first report of interferon-associated eyelash trichomegaly was in two patients with B-cell lymphoma treated with interferon.[20] After 4 months of treatment, both patients began to note that their eyelashes had thickened, curled, and reached lengths of 20–65 mm.
Prostaglandins
Acquired eyelash trichomegaly has been reported with topical use of latanoprost. The effects of prostaglandin F2-alpha and latanoprost have been found to stimulate not only murine hair follicles and follicular melanocytes but also the conversion from telogen to anagen phase. This side effect has also been tried for cosmetic effects. The Food and Drug Administration approved bimatoprost 0.03% solution for treatment of patients with hypotrichosis of the eyelashes in December 2009.[21]
Approach to the patient with eyelash trichomegaly
This should include an overall evaluation of the patient's history and other concurrent medical problems.
The onset of eyelash trichomegaly is an important point for delineating a specific etiology. If present from birth, one should look for other hair anomalies or facial features that may be present (such as alopecia, synophrys) and may suggest one of the congenital syndromes described earlier.
If onset is in later life, one should focus on medications or topical products and a risk assessment for HIV or hepatitis virus should be made.
Treatment
The main treatment of eyelash hypertrichosis involves regular trimming of the eyelashes if they cause symptoms.[22] Sometimes antibiotics and artificial tears may be necessary for local irritation or meibomitis.[23]
Conclusion
Eyelash trichomegaly, an uncommon finding, has been reported in association with a wide variety of conditions. Its clinical significance and underlying pathophysiology is yet to be discovered, but factors such as prostaglandins, immune system regulation, and epidermal growth factor receptors appear to be involved. The prognostic value of eyelash trichomegaly in oncology remains to be confirmed; some investigators suggest that the long eyelashes represent a clinical marker associated with a positive response to antineoplastic therapy.
In the future, drugs such as the prostaglandin analogs and epidermal growth factor receptor inhibitors that are associated with eyelash trichomegaly may represent potential for novel treatments of various types of hair loss.
What is new?
Trichomegaly is not only the increase in length of hair; but also refers to increased pigmentation, curling or thickness of hair.
Detailed list of causes of trichomegaly has been incorporated in this article including the newer drugs associated with trichomegaly.
Underlying pathophysiology of trichomegaly is included in this discussion.
Drugs with side effect of trichomegaly such as latanoprost approved for hypotrichosis of eyelashes.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Santmyire-Rosenberger BR, Albert M. Acquired trichomegaly with topiramate. J Am Acad Dermatol. 2005;53:362–3. doi: 10.1016/j.jaad.2005.01.121. [DOI] [PubMed] [Google Scholar]
- 2.Jayamanne DG, Dayan MR, Porter R. Cyclosporin induced trichomegaly of accessory lashes as a cause of ocular irritation. Nephrol Dial Transplant. 1996;11:1159–61. [PubMed] [Google Scholar]
- 3.Manjunatha NP, Gnanaraj L. Isolated trichomegaly causing mechanical ptosis. J Pediatr Ophthalmol Strabismus. 2008;45:384. doi: 10.3928/01913913-20081101-08. [DOI] [PubMed] [Google Scholar]
- 4.Woo TL, Francis IC. Intermittent blurred vision and trichomegaly due to latanoprost. Clin Experiment Ophthalmol. 2001;29:272–3. doi: 10.1046/j.1442-9071.2001.00416.x. [DOI] [PubMed] [Google Scholar]
- 5.Sasaki S, Hozumi Y, Kondo S. Influence of prostaglandin F2alpha and its analogues on hair regrowth and follicular melanogenesis in a murine model. Exp Dermatol. 2005;14:323–8. doi: 10.1111/j.0906-6705.2005.00270.x. [DOI] [PubMed] [Google Scholar]
- 6.Nazareth MR, Bunimovich O, Rothman IL. Trichomegaly in a 3-year-old girl with alopecia areata. Pediatr Dermatol. 2009;26:188–93. doi: 10.1111/j.1525-1470.2009.00902.x. [DOI] [PubMed] [Google Scholar]
- 7.Sharma RC, Mahajan VK, Sharma NL, Sharma A. Trichomegaly of the eyelashes in dermatomyositis. Dermatology. 2002;205:305. doi: 10.1159/000065852. [DOI] [PubMed] [Google Scholar]
- 8.Santiago M, Travassos AC, Rocha MC, Souza S. Hypertrichosis in systemic lupus erythematosus (SLE) Clin Rheumatol. 2000;19:245–6. doi: 10.1007/s100670050168. [DOI] [PubMed] [Google Scholar]
- 9.Marks MB. Recognizing the allergic person. Am Fam Physician. 1977;16:72–9. [PubMed] [Google Scholar]
- 10.Grossman MC, Cohen PR, Grossman ME. Acquired eyelash trichomegaly and alopecia areata in a human immunodeficiency virus-infected patient. Dermatology. 1996;193:52–3. doi: 10.1159/000246202. [DOI] [PubMed] [Google Scholar]
- 11.Patrizi A, Neri I, Trestini D, Landi C, Ricci G, Masi M. Acquired trichomegaly of the eyelashes in a child with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 1998;11:89–91. doi: 10.1111/j.1468-3083.1998.tb00967.x. [DOI] [PubMed] [Google Scholar]
- 12.Vélez A, Kindelán JM, García-Herola A, García-Lázaro M, Sánchez-Guijo P. Acquired trichomegaly and hypertrichosis in metastatic adenocarcinoma. Clin Exp Dermatol. 1995;20:237–9. doi: 10.1111/j.1365-2230.1995.tb01310.x. [DOI] [PubMed] [Google Scholar]
- 13.Almagro M, del Pozo J, García-Silva J, Martínez W, Castro A, Fonseca E. Eyelash length in HIV-infected patients. AIDS. 2003;17:1695–6. doi: 10.1097/00002030-200307250-00015. [DOI] [PubMed] [Google Scholar]
- 14.Bouché O, Brixi-Benmansour H, Bertin A, Perceau G, Lagarde S. Trichomegaly of the eyelashes following treatment with cetuximab. Ann Oncol. 2005;16:1711–2. doi: 10.1093/annonc/mdi300. [DOI] [PubMed] [Google Scholar]
- 15.Papadopoulos R, Chasapi V, Bachariou A. Trichomegaly induced by erlotinib. Orbit. 2008;27:329–30. doi: 10.1080/01676830802222936. [DOI] [PubMed] [Google Scholar]
- 16.Pascual JC, Bañuls J, Belinchon I, Blanes M, Massuti B. Trichomegaly following treatment with gefitinib (ZD1839) Br J Dermatol. 2004;151:1111–2. doi: 10.1111/j.1365-2133.2004.06265.x. [DOI] [PubMed] [Google Scholar]
- 17.Goksugur N, Karabay O. Eyelash and eyebrow trichomegaly induced by interferon-alfa 2a. Clin Exp Dermatol. 2007;32:583–4. doi: 10.1111/j.1365-2230.2007.02454.x. [DOI] [PubMed] [Google Scholar]
- 18.Lacouture ME, Lai SE. The PRIDE (Papulopustules and/or paronychia, Regulatory abnormalities of hair growth, Itching, and Dryness due to Epidermal growth factor receptor inhibitors) syndrome. Br J Dermatol. 2006;155:852–4. doi: 10.1111/j.1365-2133.2006.07452.x. [DOI] [PubMed] [Google Scholar]
- 19.Carser JE, Summers YJ. Trichomegaly of the eyelashes after treatment with erlotinib in non-small cell lung cancer. J Thorac Oncol. 2006;1:1040–1. [PubMed] [Google Scholar]
- 20.Foon KA, Dougher G. Increased growth of eyelashes in a patient given leukocyte a interferon. N Engl J Med. 1984;311:1259. [PubMed] [Google Scholar]
- 21.Mechcatie E. Bimatoprost approved for eyelash lengthening. Skin Allergy News. 2009;40:10. [Google Scholar]
- 22.Dueland S, Sauer T, Lund-Johansen F, Ostenstad B, Tveit KM. Epidermal growth factor receptor inhibition induces trichomegaly. Acta Oncol. 2003;42:345–6. doi: 10.1080/02841860310006038. [DOI] [PubMed] [Google Scholar]
- 23.Zhang G, Basti S, Jampol LM. Acquired trichomegaly and symptomatic external ocular changes in patients receiving epidermal growth factor receptor inhibitors: Case reports and a review of literature. Cornea. 2007;26:858–60. doi: 10.1097/ICO.0b013e318064584a. [DOI] [PubMed] [Google Scholar]


