Abstract
Here we report a case of a young male who developed full blown iatrogenic Cushing's syndrome after use of superpotent clobetasol propionate cream 0.05% for long duration to suppress psoriatic skin lesions. He also developed osteoporosis and hypogonadism. This case demonstrates that injudicious use of topical steroids can have disastrous consequences.
Keywords: Iatrogenic Cushing's, psoriasis, topical steroid
What was known?
Iatrogenic Cushing's is a well-documented phenomenon with prolonged use of high dose oral and inhaled corticosteroids.
Introduction
The availability of topical glucocorticosteroids is the most important milestone in dermatologic therapy ever achieved, owing to potent anti-inflammatory and antiproliferative effects. However, the same mechanisms of action responsible for the improvement of dermatologic inflammatory conditions can cause adverse effects.
When reaching pharmacological levels, exogenous corticosteroids often lead to complete Cushing's syndrome causing skin manifestations, suppression of the hypothalamic-pituitary-adrenal (HPA) axis and growth retardation in children exposed to long-term potent and super potent topical formulations of steroids.[1,2,3] We report this case of a young male who developed iatrogenic Cushing's syndrome after use of topical clobetasol propionate.
Case Report
A 15-year-old young male presented with generalized pustular psoriasis along with extensive striae all over the body. He also complained of progressive weight gain, body ache, and generalized weakness. History as obtained from the parents and the past documents revealed that initial presentation at about 5 years back was suggestive of psoriasis vulgaris that slowly progressed to involve wider regions of the body. Past treatments included occasional courses of low dose oral methotrexate (2.5 mg every 12 h for two to three doses every week). However, potent topical corticosteroids like clobetasol propionate cream 0.05% usually with salicylic acid was repeatedly advised during this period. It was revealed that the same was continued almost continuously since then with or without the advice of the doctor over wide body surfaces to suppress the disease aggravation that was a regular occurrence after every attempt to withdraw the topical medication.
On examination, his height was 136 cm (<3rd percentile) and weight was 68 kg (>97th percentile). He had plethoric face, prominent neck hump, pink striae, easy bruising, and vellous hypertrichosis [Figure 1]. There was erythroderma studded with small pustules. Pustules were found to be present in small groups or along the margins of some scaly plaques typical of psoriasis vulgaris, especially on the back. On healing, pustules left prominent scaling patches. Some pustules merged with others and formed lakes of pus. They were mostly present on trunk and limbs, but few pustules were also noted on face.
Figure 1.
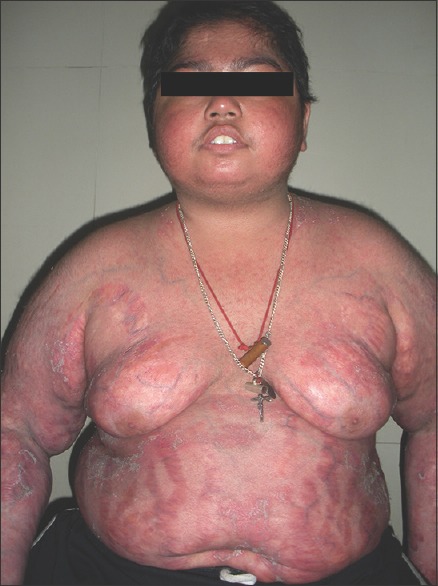
Moon face with plethora
Broad pink striae were present over the abdomen and thighs along with psoriatic skin lesions [Figure 2]. He had bilateral gynecomastia and bilateral small testis (3 ml) and Tanner stage 2 pubic hair. He had significant proximal muscle weakness of lower limbs with preservation of deep tendon reflexes.
Figure 2.

Typical broad pink striae and gynecomastia
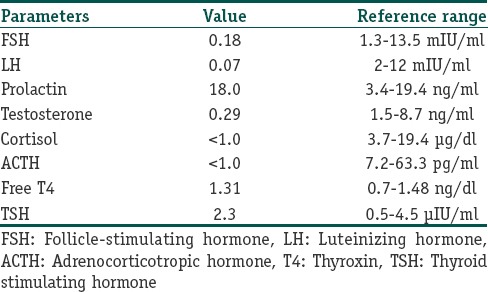
On investigation, testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) were low [Table 1]. Serum cortisol (<1 μg/dl) and adrenocorticotropic hormone (ACTH) were also very low [Table 1]. Other routine laboratory parameters were normal. Dual energy X-ray absorptiometry (DEXA) scan of spine revealed significant osteoporosis (T score - 3.2).
Table 1.
Hormonal profile of the patient
Discussion
Children are more prone to the development of systemic reactions to topically applied corticosteroid medication because of their higher ratio of total body surface area to body weight, but rare in adults. Prolonged use of topical corticosteroids causes systemic adverse effects including Cushing's syndrome and HPA axis suppression, growth impairment in children, and cataract.[4] These side effects may occur if topical corticosteroids are absorbed in significant amounts through the inflamed skin, particularly when applied to large skin areas,[5] although is less common than that of the oral or parenteral route. At least 43 cases with iatrogenic Cushing syndrome from very potent topical steroid usage (clobetasol) in children and adult have been published over the last 35 years particularly in developing countries. In the children group (n = 22), most are infants with diaper dermatitis. For the adult group (n = 21), the most common purpose of steroid use was for treatment of psoriasis.[6]
Excess glucocorticoids leads to short stature due to suppression of growth hormone releasing hormone (GHRH) and GH release from the hypothalamus and pituitary, respectively. Our patient had poor height gain probably due to same reason.[7]
Exogenous glucocorticoids suppress luteinizing hormone releasing hormone (LHRH) from hypothalamus and LH and FSH from pituitary resulting in hypogonadotropic hypogonadism. Our case had the same picture as also demonstrated by Luton et al.[8]
Osteoporosis is a common and severe adverse effect of glucocorticoid excess and one of the major limitations to long-term glucocorticoid therapy. A significant number of patients on long-term steroid therapy will have at least some loss of bone density, and oral and inhaled corticosteroid use are associated with increased bone fractures.[9,10] The bone loss caused by glucocorticoids tends to be in trabecular bone as opposed to cortical bone. Therefore, most loss is in the vertebrae and ribs of the axial skeleton.
This case exemplifies severe iatrogenic Cushing's syndrome with hypogonadotropic hypogonadism and osteoporosis in children induced by injudicious use of potent topical steroids (clobetasol) to suppress recurrent flare of psoriatic skin lesions and therefore, we physicians should always be cautious about it.
What is new?
Iatrogenic Cushing's is also caused by potent topical corticosteroids, when used for long duration over large inflamed skin areas.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Katar S, Akdeniz S, Ozbek MN, Yaramiş A. Infantile iatrogenic Cushing's syndrome. Indian J Dermatol. 2008;53:190–1. doi: 10.4103/0019-5154.44793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abma EM, Blanken R, De Heide LJ. Cushing's syndrome caused by topical steroid therapy for psoriasis. Neth J Med. 2002;60:148–50. [PubMed] [Google Scholar]
- 3.Ermis B, Ors R, Tastekin A, Ozkan B. Cushing's syndrome secondary to topical corticosteroids abuse. Clin Endocrinol (Oxf) 2003;58:795–6. doi: 10.1046/j.1365-2265.2003.18021.x. [DOI] [PubMed] [Google Scholar]
- 4.Kristmundsdottir F, David TJ. Growth impairment in children with actopic eczema. J R Soc Med. 1987;80:9–12. doi: 10.1177/014107688708000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carruthers JA, August PJ, Staughton RC. Observations on systemic effects of topical clobetasol propionate (Dermovate) Br Med J. 1975;4:203–4. doi: 10.1136/bmj.4.5990.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tempark T, Phatarakijnirund V, Chatproedprai S, Watcharasindhu S, Supornsilchai V, Wananukul S. Exogenous Cushing's syndrome due to topical corticosteroid application: Case report and review of literature. Endocrine. 2010;38:328–34. doi: 10.1007/s12020-010-9393-6. [DOI] [PubMed] [Google Scholar]
- 7.Takasashi H, Bando H, Zhang C, Yamasaki R, Saito S. Mechanism of impaired growth hormone secretion in patients with Cushing's disease. Acta Endocrinol (Copenh) 1992;127:13–7. doi: 10.1530/acta.0.1270013. [DOI] [PubMed] [Google Scholar]
- 8.Luton JP, Thiebolt P, Valcke JC, Mahoudeau JA, Bricaire H. Reversible gonadotropin deficiency in male Cushing disease. J Clin Endocrinol Metab. 1977;45:488–95. doi: 10.1210/jcem-45-3-488. [DOI] [PubMed] [Google Scholar]
- 9.Millard TP, Antoniades L, Evans AV, Smith HR, Spector TD, Barker JN. Bone mineral density of patients with chronic plaque psoriasis. Clin Exp Dermatol. 2001;26:446–8. doi: 10.1046/j.1365-2230.2001.00855.x. [DOI] [PubMed] [Google Scholar]
- 10.Nymann P, Kollerup G, Jemec GB, Grossmann E. Decreased bone mineral density in patients with pustulosis Palmaris et plantaris. Dermatology. 1996;192:307–11. doi: 10.1159/000246400. [DOI] [PubMed] [Google Scholar]


