Sir,
Isotretinoin is a gold standard drug in the armamentarium of a dermatologist for the treatment of acne vulgaris. It is the only oral drug acting on all the four pathophysiologic factors of acne vulgaris: Androgen-derived overproduction of sebum (seborrhea), ductal hypercornification (closed and open comedones), changes in microbial flora and immunologic processes and inflammation.[1] Retinal (vitamin A aldehyde) is a vital component of the photo-transduction process which is essential for normal human vision. Retinal is the crucial chromophore which combines with both rod and cone opsins to form rhodopsin and activated cone opsins. Night blindness (nyctalopia) is the most common and earliest symptom of vitamin A deficiency.[2] Isotretinoin (13-cis retinoic acid) slows rhodopsin regeneration and chromophore recycling by inhibition of the retinoid isomerase and 11-cis retinol dehydrogenase enzymes that are necessary for the synthesis of 11-cis retinal. Administering isotretinoin in patients who already have low vitamin A stores may lead to rapid development of night blindness.[3] To the best our knowledge, this is the first documented case of night blindness due to isotretinoin from India.
A 16-year-old male presented to our OPD with grade 3 acne vulgaris with moderate degree of scarring. We prescribed the patient oral isotretinoin 20 mg, prednisolone 30 mg (to counteract isotretinoin-induced flare) and topical facial cleansers. The patient reported back 1 week later with complaint of decreased night vision and almost becoming blind after the onset of dark. The cumulative dose of isotretinoin after which patient developed defective night vision was 140 mg. An urgent ophthalmic consultation was sought for his deranged night vision. His visual acuity was normal (6/6) in both the eyes. There was no defect in his color vision. Fundus examination showed early changes of myopia. The Amsler grid testing for central vision was within normal limits. Electroretinography (ERG) and dark adaptation (DA) tests were suggestive of poor rod function. ERG was performed by dilating patient's eyes (using a combination of tropicamide 1.0% and phenylephrine hydrochloride 2.5%) prior to dark adaptation for 30 minutes. The eyes were then anaesthetized (tetracaine hydrochloride 0.5%) before placing contact lens electrodes. After dark adaptation, the scoptic response was elicited using a full field dome by a dim flash of light and the amplitude and implicit times were recorded. Isotretinoin was discontinued and the patient was started on vitamin A supplements (25,000 units) daily for 4 weeks. The patient responded completely to vitamin A supplementation (25,000 units) and his night vision recovered completely. Currently, the patient is being treated for his acne vulgaris with oral antibiotics and beta-hydroxy acid (salicylic acid in spirit; 20-30%) based peels. Repeat ophthalmic evaluation showed normal dark adaptation studies.
As per the report of Teo and Yazdabadi (2014), till date there are 10 documented cases of isotretinoin-induced night blindness in the English literature.[4] Night blindness is a common and potentially hazardous side effect of isotretinoin therapy especially in young population which can make night driving a life-threatening task. Hence, it is prudent on the part of treating dermatologist to forewarn the patients regarding this potential unwanted side effect and encourage them to report changes in their night vision. Our patient developed visual symptoms within 7 days of isotretinoin therapy which resolved after 1 month of vitamin A supplementation. Halpagi et al. reported similar clinical findings in a 21-year-old female student who developed night blindness after 2 weeks of isotretinoin therapy.[5] It has been hypothesized that prior hypovitaminosis A can be a predisposing factor for isotretinoin-induced nyctalopia.[6] Does administration of isotretinoin in patients having low serum vitamin A levels makes them more susceptible to visual problems is a question yet to be answered with robust evidence. We were not able to measure serum vitamin A level in our patient. It can be postulated that isotretinoin may act as an antagonist and interfere with vitamin A in the visual pathway.
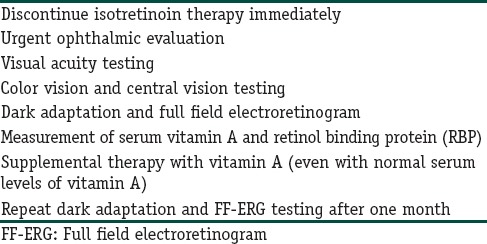
We suggest that the following protocol should be adopted in management of isotretinoin-induced night blindness [Table 1].
Table 1.
Management protocol in isotretinoin induced night blindness
Some class of patients (pilots, vehicle drivers and army men) who require an intact night vision should be screened for any delayed dark adaption before prescribing isotretinoin. However, it must be stressed that screening for retinoid-induced ocular toxicity may not be practical in routinely busy and resource poor settings.
Dermatologist must be aware of this rare but potentially sight threatening adverse effect of isotretinoin. Our case highlights that patients should be adequately educated about such rare and potential side effects of isotretinoin and proactively managed before permanent visual damage sets in.
References
- 1.Webster GF. The pathophysiology of acne. Cutis. 2005;76(2 Suppl):4–7. [PubMed] [Google Scholar]
- 2.Harris EW, Loewenstein JI, Azar D. Vitamin A deficiency and its effects on the eye. Int Ophthalmol Clin. 1998;38:155–61. doi: 10.1097/00004397-199803810-00013. [DOI] [PubMed] [Google Scholar]
- 3.Danby FW. Night blindness, vitamin A deficiency, and isotretinoin psychotoxicity. Dermatol Online J. 2003;9:30. [PubMed] [Google Scholar]
- 4.Teo K, Yazdabadi A. Isotretinoin and night blindness. Australas J Dermatol. 2014;55:222–4. doi: 10.1111/ajd.12107. [DOI] [PubMed] [Google Scholar]
- 5.Halpagi P, Grigg J, Klistorner A, Damian DL. Night blindness following low-dose isotretinoin. J Eur Acad Dermatol Venereol. 2008;22:893–4. doi: 10.1111/j.1468-3083.2007.02495.x. [DOI] [PubMed] [Google Scholar]
- 6.Welsh BM, Smith AL, Elder JE, Varigos GA. Night blindness precipitated by isotretinoin in the setting of hypovitaminosis A. Australas J Dermatol. 1999;40:208–10. doi: 10.1046/j.1440-0960.1999.00363.x. [DOI] [PubMed] [Google Scholar]


