Abstract
A 54-year-old woman presented to the ophthalmology emergency department with a 10-day history of blurred vision. The best-corrected visual acuities and Ishihara colour vision were bilaterally reduced with a left relative afferent pupillary defect. Slit-lamp examination was otherwise normal. Retrobulbar optic neuritis (ON) was presumed as she had suffered with this previously and was known to have multiple sclerosis (MS). She was recalled the following week for visual field (VF) testing, which was not available at the time of presentation. VFs demonstrated an incongruous left homonymous hemianopia. She was immediately referred to the medical team to investigate for a stroke, which was subsequently excluded. Thereafter, a trial of pulsed methylprednisolone was commenced, resulting in near complete resolution of the hemianopia. This case demonstrates not only the importance of VF testing, but also how ON may present with any field defect, including mimicking a stroke, a point valuable to ophthalmologists and medics alike.
Background
Although a homonymous hemianopia is classically identified as a sign of a stroke, it may also less commonly be associated with optic neuritis (ON). Therefore, if there is no evidence of a stroke after thorough investigation, ON should be considered as a differential diagnosis. It is well recognised that ON may present with a multitude of associated visual field (VF) defects. If the process is inflammatory rather than ischaemic, not only is the prognosis better but the patient will also improve more rapidly with corticosteroid treatment.
This case also highlights the importance of VF testing at the time of presentation to ensure treatment is not delayed, if the patient has indeed suffered a stroke. Fortunately, in this case, there was no evidence of a stroke, though in the absence of VF testing, this may have been overlooked. Even if formalised fields are not available, VF to confrontation should be performed to rule out any other gross pathology.
The process of these investigations resulted in a more time consuming and convoluted patient journey but, she was grateful for the through work up and treatment provided. This case proved not only intellectually stimulating but also an important reminder of the variety of presentations that ON may have, and should be considered as a differential diagnosis for patients being investigated for a stroke.
Case presentation
A 54-year-old woman presented to the accident and emergency department of the Bristol Eye Hospital, in April of 2014, with blurred vision. It had been blurred for 10 days at presentation. Visual acuities were 6/24 unaided and 6/12 pinhole oculus dextra (OD or right) and 6/18 unaided oculus sinistra (OS or left), with no pinhole improvement. Medical history included relapsing remitting multiple sclerosis (MS), hypertension, frozen shoulder, previous Bell’s palsy, glandular fever and a caesarean section. Ophthalmic history included diplopia and previous ON.
On examination, the patient was recorded as having a left relative afferent pupillary defect (RAPD) and Ishihara colour vision was reduced to 2/17 OD and 4/17 OS. Examination of the anterior and posterior segments, ocular motility and intraocular pressures were reported as normal. Differential diagnoses of ON and visual migraine were recorded and the patient was recalled a week later to perform Humphrey VF testing, as this was not available at the time of presentation.
Investigations
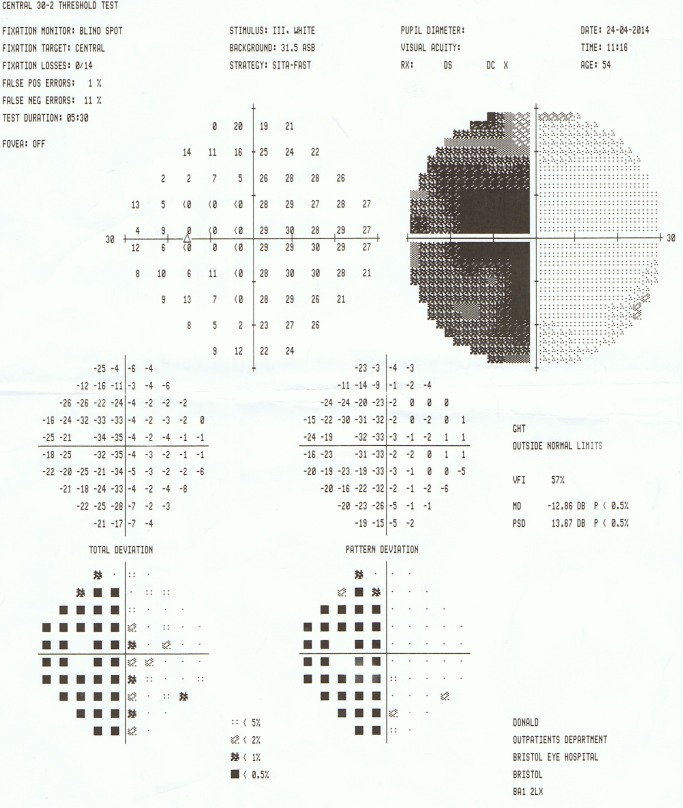
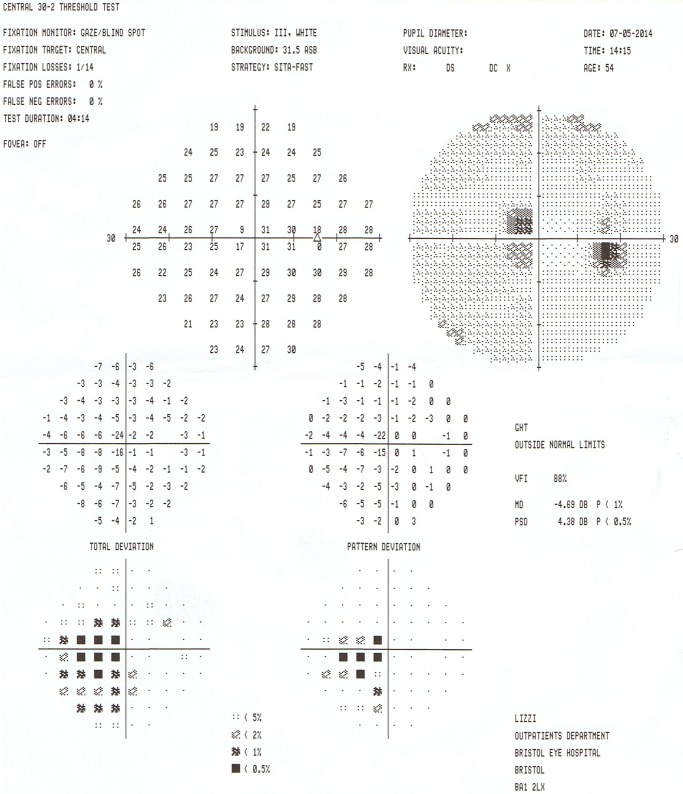
Humphrey 30-2 VF revealed an incongruous left homonymous hemianopia with reliable indices bilaterally at the patient's return visit, leading to an updated presumed diagnosis of a cerebrovascular accident (figure 1 LE/figure 1 RE comprise figure 1). An urgent blood assay and blood pressure were checked (122/77 pulse 69) and the patient was referred immediately to the medical team at the Bristol Royal Infirmary.
Figure 1.
Humphrey Visual Fields 30-2: Left homonymous hemianopia, pre-treatment.
Figure 1.
Continued.
Her ABCD2 score was 2/7, with the two points awarded for duration of symptoms. Blood pressure and heart rate were within normal parameters and bloods found the full count to be normal apart from a slight elevation in red cells (5.04 (3.80–4.80)), normal erythrocyte sedimentation rate, plasma viscosity, C reactive protein, cholesterol and glucose. The patient's creatinine was very mildly elevated at 86 (45–84).
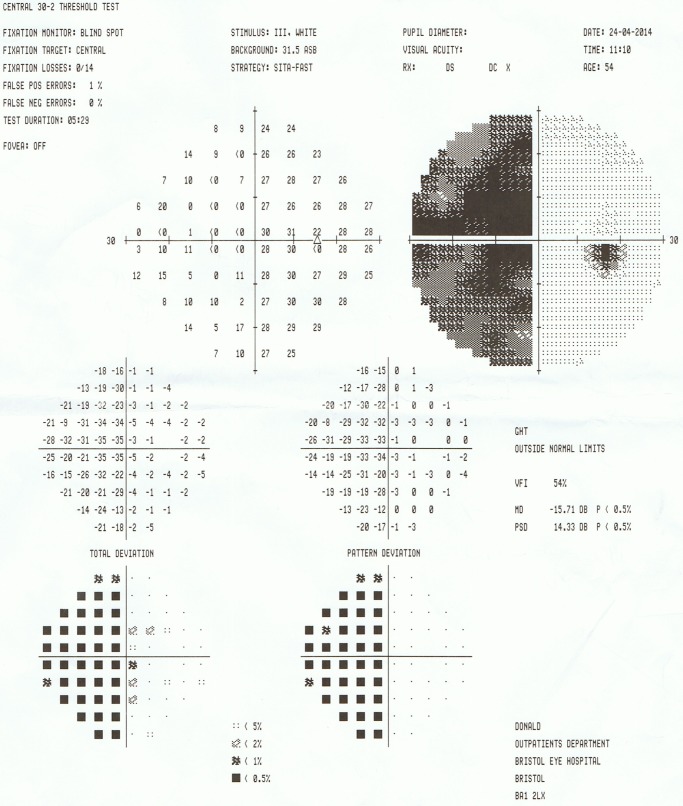
An inpatient MRI (figure 2) reported the “findings in keeping with MS flair with acute plaques involving the left periventricular deep white matter, the trigone of lateral ventricle and right inferior thalamus, likely accounting for the clinical symptoms. No definite evidence of infarct or ischaemic changes”.
Figure 2.
MRI scan showing lesions over right thalamus (A) and left periventricular matter (B).
Differential diagnosis
Initially, ON and migraine were felt to be the most likely diagnoses. On observation of the homonymous hemianopsia on the VF, appropriate reflections over the differential diagnosis were performed and a stroke was promptly investigated. Once excluded, the possibility of bilateral ON was revisited and a trial of steroid treatment started.
Treatment
Following the first dose of intravenous methylprednisolone, an improvement in visual acuity was noted. The patient received three doses over a 3-day period prior to discharge from hospital, with continued outpatient care.
Outcome and follow-up
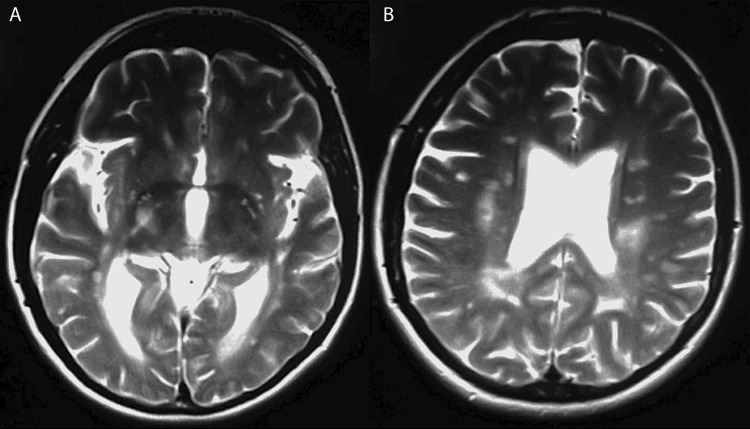
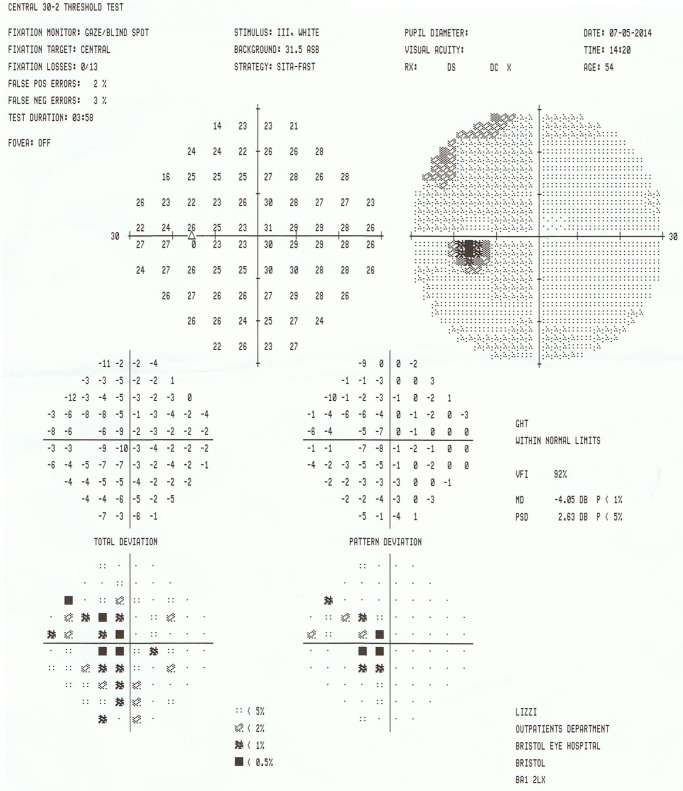
Ophthalmic follow-up 3 weeks after initial presentation found the patient's vision to have improved to 6/6 OD and 6/9 OS. No RAPD was present. Anterior segment and pressures were normal. Pallor of the left optic nerve head was now evident. Fields had improved greatly to show only minimal patchy loss, confirming a predominately inflammatory process and the diagnosis of ON opposed to an ischaemic process whereby limited improvement would be seen (figure 3 LE/figure 3 RE comprise figure 3). She was discharged from further follow-up.
Figure 3.
Humphrey Visual Fields 30-2: Resolution of homonymous hemianopia, post-treatment.
Figure 3.
Continued.
Discussion
ON refers to an acute, demyelinating or idiopathic optic neuropathy and is classified as (1) retrobulbar ON with normal disc appearance, (2) papillitis involving the anterior aspect of the ON, which manifests with swelling of the optic disc, (3) perineuritis with involvement of the optic nerve sheath rather than the optic nerve parenchyma (seen radiographically), per se, and the optic disc in this setting may or may not be swollen and (4) neuroretinitis, with optic disc oedema and a ‘star figure’ of macular exudates. The vision loss is quite variable and ranges from mild to no light perception in the latter.1
In the 15-year follow-up report from the Optic Neuritis Treatment Trial, diffuse and central field loss predominated in the affected eye at the initial visit, then, most commonly, partial arcuate, paracentral and arcuate type of nerve fibre bundle-type VF defects predominated during follow-up.2 Pau et al,1 in their ON review, highlighted that “the pattern of VF loss in ON is of limited value in distinguishing ON from other optic neuropathies but hemianopic VF defects are uncommon and should raise suspicion for a compressive or alternate aetiology to ON.”
The BJO published a paper in 1975, which found that of 300 patients with an ON, only 4 (1.3%) had homonymous VF defects and reported that they are rare despite the frequency of pathological involvement of the retrochiasmal visual pathways.3 Plant et al4 studied patients with symptomatic retrochiasmal lesions in MS and described the variations of VF loss according to the different levels of damage involved. It was evident that incongruous homonymous hemianopic field defects manifested when lesions involved the level of thalamus, lateral geniculate nucleus and optic tract, as in our case. Specifically, the lateral geniculate nucleus-related VF loss was already known since 1971 from two cases reported by Gunderson and Hoyt.5 In our case, (1) the involvement of the right inferior thalamus and (2) the anatomically close proximity of lateral geniculate nucleus and thalamus, explains the contralateral hemianopic defect.
Furthermore, homonymous hemianopias can be part of a more extensive neuro-ophthalmological manifestation named ‘optic tract syndrome’. Wernicke6 first described it in 1883 in patients with hemianopsia, where he noticed that they had a contralateral dilated pupil. Later on, Behr,7 in 1924, described a syndrome occurring when the optic tract is injured, which can manifest with various neurological signs, one of them being the contralateral pupillary abnormal response. Further studies supported that association along with other neurological manifestations.8 9 In our case, the patient had a contralateral RAPD suggesting the possibility of the abovementioned syndrome.
Irrespective of the clinical examination signs, these patients warrant further investigations to exclude any other intracranial pathology. Once alternative intracranial pathology has been excluded, then ON should remain in the list of differential diagnoses. In our case, once confirmed, intravenous steroids were administered for a 3-day period due to extend of the field defect and the impact on the patient’s activities of daily living. This is in keeping with the Royal College of Physicians guidelines, which state, “Any individual who experiences an acute episode (including ON) sufficient to cause distressing symptoms or an increased limitation on activities should be offered a course of high-dose corticosteroids. The course should be started as soon as possible after onset of the relapse and should be either: intravenous methylprednisolone, 500 mg—1 g daily, for between 3 and 5 days or high-dose oral methylprednisolone, 500 mg—2 g daily, for between 3 and 5 days.”10
Patient's perspective.
“Having had MS for 17 years, I believe that any unusual symptoms I suffer can be attributed to the disease. I was not panicking about my gradual loss of vision and was in no rush to go to the doctors, as there is little that doctors can do and a previous regime of steroids hadn't made any improvements in my symptoms. However, I was shocked, on my second appointment to the Bristol Eye Hospital, to be told I had possibly suffered a mild stroke. This was discovered due to the results of a field of vision test. I had suffered with double vision during a previous relapse and although this loss of vision was different I wasn't panicking as I could still see a certain amount and the loss was white patches as opposed to dark patches. I am happy that the doctors I saw at the eye hospital took the possibility of a stroke seriously and forwarded me to Bristol Royal Infirmary.”
Learning points.
Optic neuritis may present with a diverse variety of visual field defects, including unusual presentations such as a homonymous hemianopia.
Hemianopic visual field defects warrant prompt further investigation for intracranial pathology.
Bilateral optic neuritis should be considered as a differential diagnosis in cases of homonymous hemianopia.
Visual field testing is an essential tool in aiding diagnosis and monitoring of the disease process.
Acknowledgments
The authors would like to thank our patient, who kindly agreed in utilising her case for the education of our colleagues worldwide.
Footnotes
Contributors: All the authors contributed to this case. KM wrote up the case and has the role of corresponding author, while RG was the consultant in charge and responsible for this patient. GV edited the case and prepared the manuscript for submission, including any necessary changes indicated by the editorial group.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pau D, Zubidi N, Yalamanchili S et al. Optic neuritis: review. Eye 2011; 25:833–42. 10.1038/eye.2011.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keltner J, Johnson C, Cello K et al. Visual field profile of optic neuritis: a final follow-up report from the optic neuritis treatment trial from baseline through 15 years. Arch Ophthalmol 2010;128:330–7. 10.1001/archophthalmol.2010.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawkins K, Behrens M. Homonymous hemianopia in multiple sclerosis. With report of bilateral case. Br J Ophthalmol 1975;59:334–7. 10.1136/bjo.59.6.334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plant GT, Kermode AG, Turano G et al. Symptomatic retrochiasmal lesions in multiple sclerosis: clinical features, visual evoked potentials, and magnetic resonance imaging. Neurology 1992;42:68–76. 10.1212/WNL.42.1.68 [DOI] [PubMed] [Google Scholar]
- 5.Gunderson CH, Hoyt WF. Geniculate hemianopia: incongruous homonymous field defects in two patients with partial lesions of the lateral geniculate nucleus. J Neurol Neurosurg Psychiatry 1971;34:1–6. 10.1136/jnnp.34.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wernicke C. Ueber hemiopische pupillenreaction. Fortschr Med 1883;1:49–53. [Google Scholar]
- 7.Behr C. Die Untersuchungsmethoden: II. Die Lehre von Pupillenbewegungen. In: Graefe A, Saemische I, eds. Handbuch der gesamtem Augenheilkunde, vol 2 Leipzig, East Germany: W Engelmann, 1924:115–17. [Google Scholar]
- 8.Lowenstein O. Clinical pupillary symptoms in lesions of optic nerve, optic chiasm, and optic tract. AMA Arch Ophthalmol 1954;52:385–403. 10.1001/archopht.1954.00920050387006 [DOI] [PubMed] [Google Scholar]
- 9.Herman P. The Behr pupil revisited. Anisocoria following cerebrovascular accidents. Stroke 1975;6:697–702. 10.1161/01.STR.6.6.697 [DOI] [PubMed] [Google Scholar]
- 10.Royal College of Physicians. Multiple sclerosis: National clinical guideline for diagnosis and management in primary and secondary care. https://www.rcplondon.ac.uk/sites/default/files/documents/multiple-sclerosis-guideline.pdf.Accessed August 2014