Description
A 71-year-old woman was transported by ambulance to the emergency department with decreased consciousness. Paramedics noted mild left hemifacial drooping. On initial assessment, the patient was disoriented but had a Glasgow Coma Score of 15/15. Neurological examination revealed an upper motor neuron weakness of the left face, with normal tone, power, reflexes and sensation in all limbs.
An urgent CT scan of the head was performed (figure 1). The radiologist noted bifrontal deep white matter low attenuation. A collateral history from the patient's general practitioner revealed a history of bilateral frontal stereotactic leucotomies in 1969, for severe schizophrenia. Examination of the bone window revealed chronic bone deformity at the site of a previous frontal craniotomy (figure 2).
Figure 1.

Axial computerised tomography showing bilateral areas of low attenuation in the frontal/prefrontal cortex.
Figure 2.
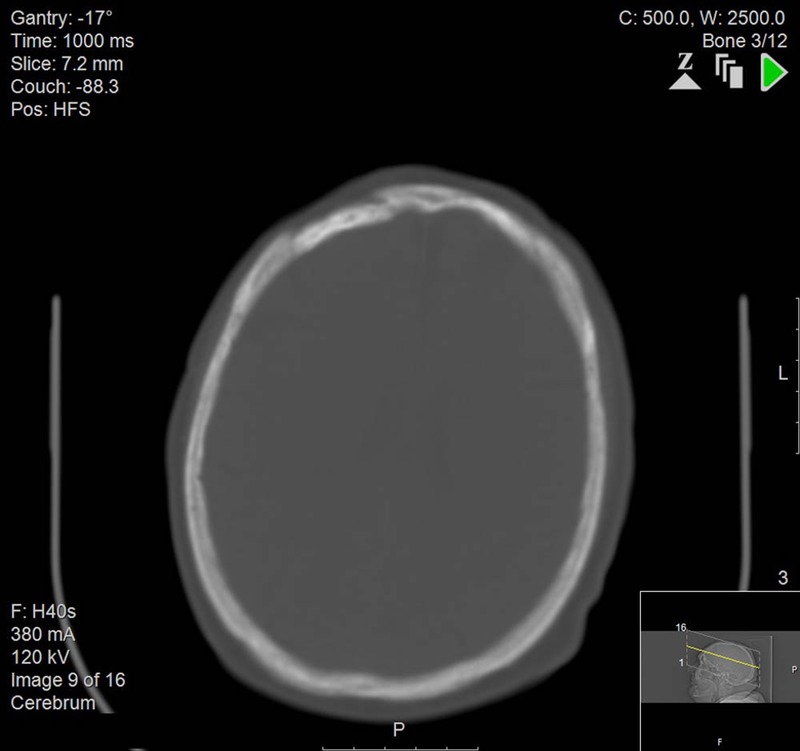
Axial computerised tomography (bone window) showing old right-sided craniotomy.
Her acute presentation to hospital was eventually ascribed to a urinary tract infection, which was successfully treated with antibiotic therapy.
Frontal lobotomy (more commonly known in the UK as ‘prefrontal leucotomy’) is an extinct procedure. It was historically performed in cases of intractable psychiatric illness.1 The aim was to interrupt the long tracts of the prefrontal cortex via blunt mechanical trauma. Although the procedure generated worldwide controversy, its inventor—Dr Egas Moniz—received a Nobel Prize for his work. It was gradually superceded by newer antipsychotic medications in the 1960's.2 Although some psychosurgical procedures are still rarely carried out today, the frontal lobotomy has been consigned to history.
Although no longer practiced, the sequelae of the frontal lobotomy may be observed today in older psychiatric patients. The characteristic bilateral areas of low attenuation seen on CT must be differentiated from cerebral infarction and sequelae of old contusions.3
Learning points.
Although a historic procedure, the effects of frontal lobotomies may still be encountered in older psychiatric patients.
If information is limited, previous psychosurgical intervention should be considered in cases of bifrontal areas of low attenuation on CT scanning.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Soares MS, Paiva WS, Guertzenstein EZ et al. Psychosurgery for schizophrenia: history and perspectives. Neuropsychiatr Dis Treat 2013;9:509–15. doi:10.2147/NDT.S35823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faria M. Violence, mental illness and the brain—a brief history of psychosurgery: part 1—from trephination to lobotomy. Surg Neurol Int 2013;4:49 doi:10.4103/2152-7806.110146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uchino A, Kato A, Yuzuriha T et al. Cranial MR imaging of sequelae of prefrontal lobotomy. AJNR Am J Nueroradiol 2001;22:301–4. [PMC free article] [PubMed] [Google Scholar]


