Abstract
Total parenteral nutrition (TPN) administration in a mouse model leads to a local mucosal inflammatory response, resulting in a loss of epithelial barrier function (EBF). Although, the underlying mechanisms are unknown, a major contributing factor is a loss of growth factors and subsequent critical downstream signaling. An important component of these is the p-Akt pathway. An additional contributing factor to the loss of EBF with TPN is an increase in proinflammatory cytokine abundance within the mucosal epithelium, including TNF-α and IFN-γ. Loss of critical nutrients, including glutamine and glutamate, may affect EBF, contributing to the loss of tight junction proteins. Finding protective modalities for the small intestine during TPN administration may have important clinical applications. Supplemental glutamine and glutamate may be examples of such agents.
Keywords: small intestine, p-Akt, parenteral nutrition, epithelial barrier function
Introduction
Parenteral nutrition (PN) is commonly used as treatment for many patients, ranging from short-term use in patients with gastrointestinal dysfunction[1], to long-term use in patients with short bowel syndrome[2, 3]. While it is lifesaving for many, PN use is associated with numerous complications, including an increase in infections[4, 5]. While the precise etiology of this increased rate of infections has not been fully established, it is known that organisms arising from enteric flora constitute a large percent of these infections. This suggests that a major loss of epithelial barrier function (EBF) could be a contributing factor leading to this increase in infectious complications. Additional contributing factors include a loss of local growth factors and increase in several proinflammatory mucosal cytokines. This review summarizes the work done by our laboratory and others on TPN-associated loss of EBF.
TPN administration results in a proinflammatory cytokine state within the intestinal mucosa
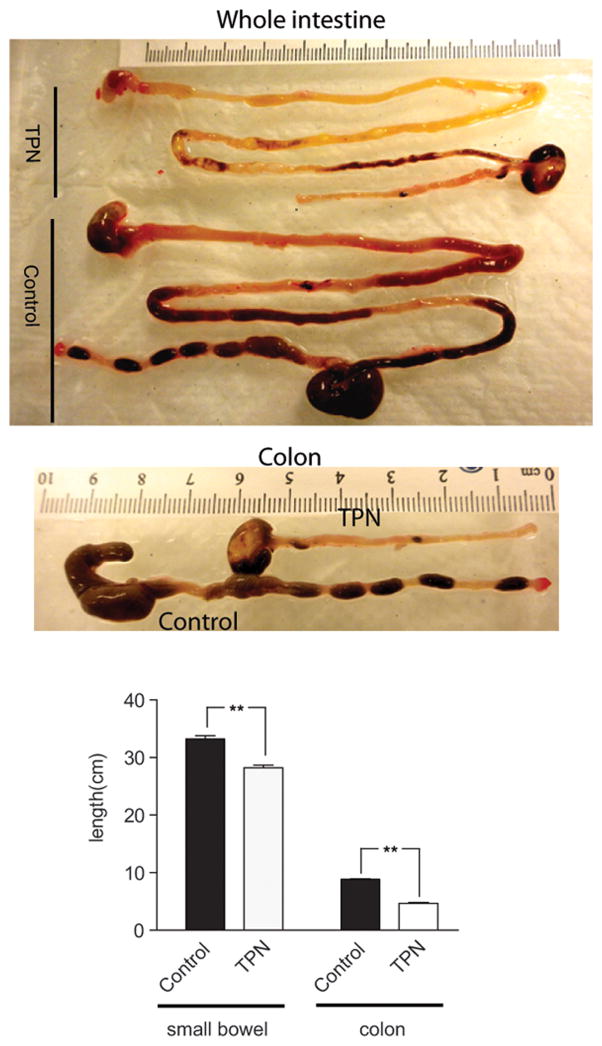
The development of these inflammatory changes is complex and leads to atrophy of small bowel villi, an increase in epithelial cell (EC) apoptosis[6, 7], and a decrease in EC proliferation. This results in a marked reduction in the length of the small and large bowel (Figure 1). Increases in TNF-α and INF-γ both appear to contribute to the loss of EBF found with TPN administration. Blockade of TNF signaling with the use of TNF-receptor knockout mice demonstrate that the major mediator of mucosal atrophy is via the TNF-R1 signaling pathway, and without an intact path, mucosal atrophy is significantly prevented [8]. Blockade of IFN-γ signaling using INF-γ–knockout mice has also been shown to be effective in preventing the loss of EBF [7, 9].
Figure 1.
(A) Representative image of harvested intestine from control (chow fed) and TPN mice. Note the significantly reduced length of both small and large intestine. (B) Mean length in centimeters of small and large bowel (colon) from control and TPN mice. **P < 0.01.
Microbiome and TPN
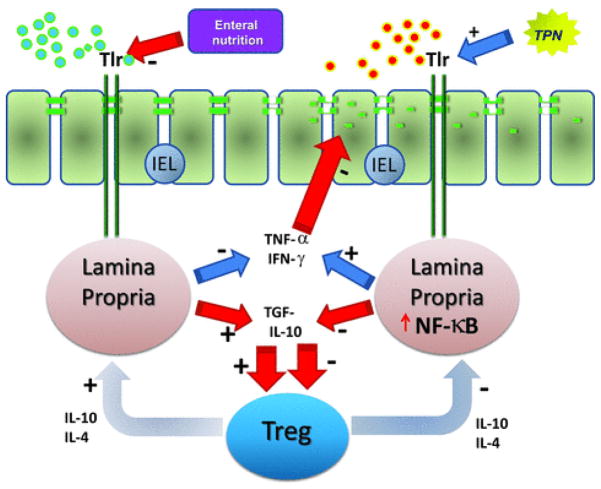
Previous studies from our laboratory and others have shown in a mouse model of total PN (TPN) in which the gut is devoid of all nutrients and where there are a number of significant physical and immunologic changes in the intestinal mucosa[9–13]. Data from our laboratory demonstrates that these intestinal changes are intimately associated with alterations in the luminal microbiome[14]. Our laboratory identified a major shift in the microbiome, from a normally benign composition of mostly firmacutes, to a predominantly Gram-negative, proteobacteria population. This shift in the microbiome was strongly correlated with a proinflammatory state characterized by an up regulation in Toll-like receptor (TLR) signaling, including TLR2, TLR4 and TLR9[15]. As well, this led to a marked downstream increase in NF-κB activation within the lamina propria, with a resultant increase in inflammatory cytokines INF-γ and TNF-α, as well as a decreased population of T-regulatory cells[16]. Blockade of this signaling pathway using MyD88 knockout mice demonstrated a significant prevention of NF-κB activation, prevention of a proinflammatory state, preservation of T-regulatory cell population, and prevention of the loss of EBF[17]. Taken together, this suggests that unique strategies to prevent these major microbiome changes, or block TLR signaling, during TPN administration may prove to be a strategy to prevent the adverse effects of intestinal atrophy and loss of EBF (Fig. 2).
Figure 2.
Summary of potential signaling changes with TPN administration. Note loss of nutrients with TPN administration results in a change in the microbiome (represented by the red dots). This leads to enhanced signaling via toll-like receptors (Tlr) activating lamina propria lymphoid tissue leading to NF-κB nuclear transcription and a proinflammatory state within the mucosa, with increases in TNF-α and IFN-γ, and loss of TNF-β and IL-10. These changes lead to a loss of TREG cells and an exacerbation in the proinflammatory state. In total this leads to a loss of epithelial barrier function.
TPN results in a loss of local growth factor production: implications for loss of epithelial barrier function
The pathophysiology of TPN-driven EC apoptosis, decreased EC proliferation and loss of EBF is complex. Although conventionally viewed as a mediator of cellular death, TNF-α signaling has also been closely linked with cell survival and regulation of proliferation. In fact, effective epidermal growth factor (EGF) signaling requires both an intact TNF-α [18, 19] and ErbB1 receptor pathways. Both EGF and ErbB1 are markedly diminished with TPN administration[8]. The combination of a proinflammatory state, with loss of EGF signaling leads to an imbalance between TNFR1/TNFR2 and EGF signaling. Such a deranged state may well be a major contributing factor to TPN-associated mucosal atrophy and loss of EBF.
Aside from a loss of ErbB ligands, TPN has also been shown to result in a loss of two other key mucosal growth factors, keratinocyte growth factor (KGF)[20–22] and glucagon-like peptide-2 (GLP-2)[23]. Each of these factors are contributors to maintenance of the intestinal barrier function [24, 25], and loss of these factors appear to be major contributors to TPN-associated intestinal atrophy[23].
TPN-associated loss of EBF[26, 27] may well result in increases in bacterial translocation[28–30]. The barrier function of the epithelium is the sum of several physiological processes, including the synthesis and release of mucus from goblet cells, transcytosis of dimeric secretory IgA, luminally directed water movement, and the physical integrity of the epithelial layer itself. [31] Breakdown in EBF and immunologic derangement can lead to the systemic dissemination of pathogens that often lead to the development of multi-organ dysfunction. [32]These findings have been shown in both mouse models and in humans [33] on PN.
TPN-associated loss of p-Akt abundance and loss of tight junctional proteins
Loss of growth factor signaling may lead to a loss of downstream phosphatidylinositol 3-kinase (PI3K)/p-Akt signaling. This may have significant implications as a critical role of PI3K/Akt signaling in resistance to apoptosis has been reported in multiple cell types[34, 35]. Our previous data has shown that TPN administration led to decreased p-Akt activity in small bowel ECs, contributing to the TPN-associated loss of proliferation and increased apoptosis[36]. TCL1 is a novel Akt-activating peptide (a head-to-tail dimer of the Akt-binding domain of T-cell lymphoma-1) [37]. We used this peptide, or an inactive mutant sequence TCL1G, conjugated to a transactivator of transcription peptide sequence (TAT), to promote intracellular uptake. This led to a significant increase in p-Akt, as well as prevention in both the loss of EC proliferation and rise in apoptosis with TPN[11].
The PI3K/p-Akt signaling may well have implications on preservation of EBF. PI3K/p-Akt signaling has been reported to affect electrogenic intestinal transport [38]. However, this action may be partial in that these authors showed that the application of the PI3 kinase inhibitor, Wortmannin or LY294002, did not significantly alter transepithelial potential difference or resistance. Junctional proteins play a crucial role in the epithelial barrier, and these can be reflected by the measurement of the transepithelial potential difference and resistance. Zonula occludens protein 1 (ZO-1) acts as a functional cross-linker between the E-cadherin/catenin complex and actin-based cytoskeleton. [39]. Other critical factors that modulate EBF include the family of claudins, and these may change significantly with various disease processes, such as Crohn’s disease [40, 41]. In our mice using Western immunoblots to measure junctional protein expression, we found a significant reduction in the abundance of tight junction proteins ZO-1 and occludin, as well as the adhesion junctional protein E-Cadherin compared to sham (enterally fed) groups. TCL-1 administration (which drives p-Akt abundance) partially prevented the loss of ZO-1 and E-Cadherin expression; however, TCL-1 did not impact the loss of occludin expression. As well, TER was not significantly affected in the TCL-1 TPN group compared to control TPN groups. Thus, the partial prevention of the loss of p-Akt, was unable to fully prevent the loss of EBF in this TPN model. Claudins also were differentially expressed with TPN, including a loss of claudins 7 and 15 [12].
As mentioned above, our laboratory’s data also showed that downregulation of E-cadherin expression in TPN mice is tightly related to a decrease in the p-Akt activity [36]. Additionally, we showed an association linking the loss of EC proliferation and increase of EC apoptosis, to a decline in the downstream signaling of the p-Akt pathway via GSK3 β and mTOR pathways [11]. Interestingly, supplementation of TPN mice with intravenous glutamine prevented the loss of p-Akt abundance, and resulted in a recovery of EC proliferation as well as barrier function[42] (see next section on nutrient supplementation). These findings are similar to the McKay group, which recently reported that PI3K and protein kinase C (PKC) were mediators of IFN-γ–induced increases in epithelial paracellular permeability and the transcytosis of noninvasive, nonpathogenic Escherichia coli passage across monolayers of human gut derived epithelial cells. Although Akt is an important mediator of many PI3K-dependent events, this event was Akt independent[43, 44]. This may explain our lack of impacting EBF by driving p-Akt abundance.
Recently, it has been reported that TLR2-induced TJ modulation strongly interrelates with promotion of intestinal epithelial cell survival through the PI3K/Akt pathway [45]. An ex vivo culture model of primary IEC showed functionally that TLR2 activation promotes cell survival by inhibiting apoptosis. This effect requires the adaptor molecule MyD88, which contains a p85-binding site [46], as a putative mechanism to recruit PI3K downstream on ligand stimulation. TLR2 stimulation efficiently preserves ZO-1–associated barrier integrity against stress-induced damage, which is controlled by the PI3K-Akt-pathway via MyD88. As well, intestinal epithelial cell TLR2 functions via PI3KAkt to attenuate the MAPK-NF-κB–signaling cascade. Therefore, the complex interactions of an upregulation of TLR2 in our TPN model may well interrelate with the loss of epithelial cell proliferation and EBF. Since a major signaling mechanism for TLR4 is via lipopolysaccharide, much attention has been focused on how to block this signal. Intestinal alkaline phosphatase (IAP), which is released by the brush border of epithelial cells can neutralize LPS and normalize the intestinal microbiota [47]. It will be fascinating to explore whether nutrient deprivation, with TPN, can influence IAP production.
Loss of critical nutrients may be a contributing factor to the development of EBF loss
With the comprehensive clinical application of TPN, it would seem that clinicians have achieved consensus about the optimal TPN formula. However, even with the prerequisite of enough caloric intake, there still are two problems not well-handled in the current approach to clinical TPN administration: loss of critical nutrients in the TPN solution and the lost luminal sensing for nutrients in the gut. Each of these may contribute to TPN-associated EBF disruption. These two issues are an emerging research focus in this field.
To address the first issue, we compared the difference between TPN versus TPN plus partial (25%) oral feeding on the intestinal immune system[48]. This small amount of enteral feeding significantly prevented atrophy of the intestinal epithelium and changes in IEL phenotypes seen with TPN. As there was a prevention in the upregulation of proinflammatory cytokines (which downregulated normal tight junction function) with partial enteral feeding, the results suggests that the major factor responsible for TPN-associated loss of EBF, bacterial translocation (BT) and intraepithelial lymphocytes (IEL)-changes, is the lack of enteral feeding and not just the administration of the TPN solution itself.
Of great interest is to identify critical nutrients that could be involved in EBF protective mechanisms, thereby helping us greatly improve the formula of TPN solution. Since glutamine (GLN) has been shown to be an important amino acid in the modulation of EBF under various luminal threats, such as endotoxin lipopolysaccharide, we investigated the benefits of GLN supplementation on TPN mice[42]. Intravenous GLN supplementation significantly prevented the loss of EBF and mucosal atrophy in TPN mice. This was shown with an accompanied decreased intestinal permeability, increased expression of tight junction proteins (including ZO-1, occluding, and junctional adhesion molecule-1), as well as prevention of changes in IEL-derived cytokine profile. It appears that GLN showed this EBF protective effect in TPN mice by regulating the phenotype and function of IEL, potentially via an immunomodulatory effect of GLN[42].
The glutamine studies described above were supplemented intravenously. It is also possible that that the lack of luminal nutrients with TPN administration not only leads to some certain nutritional deficiencies, but may also cause the loss of gut sensing. An increasing literature has shown gut taste receptors (TRs), located throughout the gastrointestinal tract, to be involved in gastrointestinal mucosal defense mechanisms[49]. It is clear that a variety of TRs are present throughout the gastrointestinal tract, and that these are predominately located in enteroendocrine cells and ECs on the luminal side of the mucosa, facing a variety of nutritive and non-nutritive stimuli signals[50]. Interestingly, growing evidence has demonstrated that certain sweet receptors and umami receptors may be under dynamic regulation under different metabolic (glucose/GLM) and luminal stimuli (acid injury/luminal microbiota); and may have particular relevance in disease conditions such as diabetes[51]. This suggests that there may exist a compensatory mechanism balancing nutrient sensing and absorption[52]. Furthermore, through activating TRs, taste stimulants supplementation could enhance the function of the intestinal immune system[53]. Potentially, this stimulation could enhance EBF.
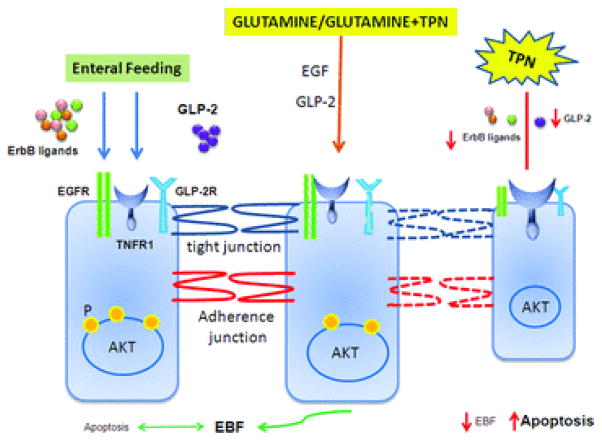
Recently, the umami receptor stimulant, glutamate (GLM) has been shown to enhance duodenal mucosal defense mechanisms through the taste receptors T1R1/T1R3 and GLM receptors[54]. The Wang group reported that perfusion of L-Glu/IMP increased portal venous concentrations of GLP-2 and GLP-1, increases duodenal bicarbonate secretion (DBS) [55]. Another recent in vitro study demonstrated that similar to GLN, GLM treatment reduced the permeability of IEC monolayers[56], thereby enhancing EBF. Although there are no publications examining the action of GLM on EBF during TPN administration, it is quite possible that stimulation of these taste receptors may act in this way, and thus, restoring gut nutritional sensing could be a potential strategy to improve EBF in TPN patients. A summary of these findings is given in Figure 3.
Figure 3.
Summary of the potential mechanisms which may be involved in sustaining epithelial barrier function via the p-Akt signaling pathway. Note loss of local growth factors, including EGF and GLP2, along with respective receptors results in loss of EBF. Restitution of EBF, along with epithelial cell proliferation and prevention of apoptosis, occurs in TPN mice with supplementation of glutamine or glutamate, as well as with exogenous growth factors.
Conclusions
While providing the essential macro- and micronutrients required during a prolonged fasting state, the administration of TPN also leads to small bowel atrophy, increase in EC apoptosis, and increases in proinflammatory mediators. The resultant effect is a significant loss of EBF, predominantly via a loss of critical tight junction proteins. The mechanisms for these actions are complex, but decreases in the p-Akt signaling pathway, and an increase in proinflammatory cytokines, likely play important roles. The additional administration of glutamine, the principal energy source for enterocytes, helps prevent these deleterious effects TPN has on the small bowel. Conceivably directed enteral stimulates, such as glutamate, may also demonstrate intestinal protection via signaling of intestinal taste receptors. By continuing to examine the mechanisms of TPN related complications in the small bowel, and potential protective modalities, the harmful effects of this life-prolonging therapy may be eliminated.
Acknowledgments
This work was supported by NIH-R01 AI-44076-11.
Footnotes
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Braga M, et al. ESPEN Guidelines on Parenteral Nutrition: surgery. Clin Nutr. 2009;28:378–386. doi: 10.1016/j.clnu.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Duro D, Kamin D, Duggan C. Overview of pediatric short bowel syndrome. J Pediatr Gastroenterol Nutr. 2008;47(Suppl 1):S33–36. doi: 10.1097/MPG.0b013e3181819007. [DOI] [PubMed] [Google Scholar]
- 3.Spencer A, et al. Mortality and Outcomes of Pediatric Short Bowel Syndrome: Redefining Predictors of Success. Annals of Surgery. 2005;242:1–10. doi: 10.1097/01.sla.0000179647.24046.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gogos CA, Kalfarentzos F. Total parenteral nutrition and immune system activity: a review. Nutrition. 1995;11:339–344. [PubMed] [Google Scholar]
- 5.Perioperative total parenteral nutrition in surgical patients. The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. N Engl J Med. 1991;325:525–532. doi: 10.1056/NEJM199108223250801. [DOI] [PubMed] [Google Scholar]
- 6.Wildhaber BE, et al. TPN-induced apoptosis in mouse intestinal epithelium: Regulation by the BCL-2 protein family. Ped Surg Int. 2002;18:570–575. doi: 10.1007/s00383-002-0869-1. [DOI] [PubMed] [Google Scholar]
- 7.Yang H, et al. Interferon-gamma expression by intraepithelial lymphocytes results in a loss of epithelial barrier function in a mouse model of total parenteral nutrition. Ann Surg. 2002;236:226–234. doi: 10.1097/00000658-200208000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng Y, Teitelbaum DH. Epidermal Growth Factor/TNF-alpha Transactivation Modulates Epithelial Cell Proliferation and Apoptosis in a Mouse Model of Parenteral Nutrition. Am J Physiol Gastrointest Liver Physiol. 2011 doi: 10.1152/ajpgi.00142.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang H, Teitelbaum DH. Intraepithelial lymphocyte-derived interferon-gamma evokes enterocyte apoptosis with parenteral nutrition in mice. Am J Physiol Gastrointest Liver Physiol. 2003;284:G629–G637. doi: 10.1152/ajpgi.00290.2002. [DOI] [PubMed] [Google Scholar]
- 10.Li J, et al. Effect of parenteral and enteral nutrition on gut-associated lymphoid tissue. Journal of Trauma. 1995;39:44–51. doi: 10.1097/00005373-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Feng Y, McDunn JE, Teitelbaum DH. Decreased phospho-Akt signaling in a mouse model of total parenteral nutrition: a potential mechanism for the development of intestinal mucosal atrophy. Am J Physiol Gastrointest Liver Physiol. 2010;298:G833–841. doi: 10.1152/ajpgi.00030.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun X, et al. Decline in intestinal mucosal IL-10 expression and decreased intestinal barrier function in a mouse model of total parenteral nutrition. Am J Physiol Gastrointest Liver Physiol. 2008;294:G139–147. doi: 10.1152/ajpgi.00386.2007. [DOI] [PubMed] [Google Scholar]
- 13.Feng Y, et al. Dissociation of E-Cadherin and beta-catenin in a mouse model of total parenteral nutrition: A mechanism for the loss of epithelial cell proliferation and villus atrophy. J Physiol (London) 2009;587:641–654. doi: 10.1113/jphysiol.2008.162719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miyasaka E, et al. Total Parenteral Nutrition (TPN) in a Mouse Model Leads to Major Population Shifts in the Intestinal Microbiome. Gastroenterology. 2011;140:1. [Google Scholar]
- 15.Miyasaka E, et al. Removal of Enteral Nutrition With Total Parenteral Nutrition in Mice Leads to Changes in Bacterial Flora and an Associated Increased Toll-Like Receptors in the Small Intestinal Lamina Propria. Gastroenterology. 2010;138:S-608–609. [Google Scholar]
- 16.Miyasaka E, Teitelbaum D. Loss of Small-Intestine Lamina Propria T-Regulatory Cells in a Mouse-Model of Total Parenteral Nutrition (TPN) J Surg Res. 2010;158:330. [Google Scholar]
- 17.Miyasaka E, Feng Y, Teitelbaum D. Total Parenteral Nutrition In A Mouse Model Results In A Proinflammatory State In The Lamina Propria: A Myd88-dependent Mechanisms Of Action. Surgery. 2011 Abstract in Press. [Google Scholar]
- 18.McElroy SJ, et al. Tumor necrosis factor inhibits ligand-stimulated EGF receptor activation through a TNF receptor 1-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2008;295:G285–293. doi: 10.1152/ajpgi.00425.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamaoka T, et al. Transactivation of EGF receptor and ErbB2 protects intestinal epithelial cells from TNF-induced apoptosis. Proc Natl Acad Sci U S A. 2008;105:11772–11777. doi: 10.1073/pnas.0801463105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang H, et al. Intestinal intraepithelial lymphocyte gammadelta-T cell-derived keratinocyte growth factor modulates epithelial growth in the mouse. J Immunol. 2004;172:4151–4158. doi: 10.4049/jimmunol.172.7.4151. [DOI] [PubMed] [Google Scholar]
- 21.Yang H, Wildhaber BE, Teitelbaum DH. Keratinocyte growth factor improves epithelial function after massive small bowel resection. J Parenter Enteral Nutr. 2003;27:198–206. doi: 10.1177/0148607103027003198. [DOI] [PubMed] [Google Scholar]
- 22.Yang H, et al. 2002 Harry M. Vars Research Award. Keratinocyte growth factor stimulates the recovery of epithelial structure and function in a mouse model of total parenteral nutrition. JPEN J Parenter Enteral Nutr. 2002;26:333–340. doi: 10.1177/0148607102026006333. discussion 340-331. [DOI] [PubMed] [Google Scholar]
- 23.Feng Y, Holst J, Teitelbaum D. Total Parenteral Nutrition(TPN)-Associated Atrophy is Associated With Loss of Intestinal Epithelial Cell (EC) Migration: Modulation of Action by Epidermal Growth Factor (EGF) and Glucagon-Like Peptide-2(GLP-2) Gastroenterology. 2011;140:S-170–S-171. [Google Scholar]
- 24.Tsai C, Hill M, Drucker K. Biological determinants of intestinotrophic properties of GLP-2 in vivo. American Journal of Physiology. 1997;272:G662–G668. doi: 10.1152/ajpgi.1997.272.3.G662. [DOI] [PubMed] [Google Scholar]
- 25.Brubaker P, et al. Circulating and tissue forms of the intestinal growth factor, glucagon-like peptide-2. Endocrinology. 1997;138:4837–4843. doi: 10.1210/endo.138.11.5482. [DOI] [PubMed] [Google Scholar]
- 26.Yang H, Finaly R, Teitelbaum DH. Alteration in epithelial permeability and ion transport in a mouse model of total parenteral nutrition. Crit Care Med. 2003;31:1118–1125. doi: 10.1097/01.CCM.0000053523.73064.8A. [DOI] [PubMed] [Google Scholar]
- 27.Sun X, et al. Decline in intestinal mucosal IL-10 expression and decreased intestinal barrier function in a mouse model of total parenteral nutrition. Am J Physiol Gastrointest Liver Physiol. 2008;294:G139–147. doi: 10.1152/ajpgi.00386.2007. [DOI] [PubMed] [Google Scholar]
- 28.Kudsk KA, et al. Enteral versus parenteral feeding. Effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992;215:503–511. doi: 10.1097/00000658-199205000-00013. discussion 511-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kiristioglu I, et al. Total parenteral nutrition-associated changes in mouse intestinal intraepithelial lymphocytes. Digestive Diseases and Sciences. 2002;47:1147–1157. doi: 10.1023/a:1015066813675. [DOI] [PubMed] [Google Scholar]
- 30.Kiristioglu I, Teitelbaum DH. Alteration of the intestinal intraepithelial lymphocytes during total parenteral nutrition. J Surg Res. 1998;79:91–96. doi: 10.1006/jsre.1998.5408. [DOI] [PubMed] [Google Scholar]
- 31.Clayburgh DR, Shen L, Turner JR. A porous defense: the leaky epithelial barrier in intestinal disease. Lab Invest. 2004;84:282–291. doi: 10.1038/labinvest.3700050. [DOI] [PubMed] [Google Scholar]
- 32.Kristof K, et al. Impact of molecular mimicry on the clinical course and outcome of sepsis syndrome. Mol Immunol. 2011;49:512–517. doi: 10.1016/j.molimm.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 33.Buchman AL, et al. Parenteral nutrition is associated with intestinal morphologic and functional changes in humans. JPEN J Parenter Enteral Nutr. 1995;19:453–460. doi: 10.1177/0148607195019006453. [DOI] [PubMed] [Google Scholar]
- 34.Chang F, et al. Involvement of PI3K/Akt pathway in cell cycle progression, apoptosis, and neoplastic transformation: a target for cancer chemotherapy. Leukemia. 2003;17:590–603. doi: 10.1038/sj.leu.2402824. [DOI] [PubMed] [Google Scholar]
- 35.Bouchard V, et al. B1 integrin/Fak/Src signaling in intestinal epithelial crypt cell survival: integration of complex regulatory mechanisms. Apoptosis. 2008;13:531–542. doi: 10.1007/s10495-008-0192-y. [DOI] [PubMed] [Google Scholar]
- 36.Feng Y, et al. Dissociation of E-cadherin and beta-catenin in a mouse model of total parenteral nutrition: a mechanism for the loss of epithelial cell proliferation and villus atrophy. J Physiol. 2009;587:641–654. doi: 10.1113/jphysiol.2008.162719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McDunn J, et al. Peptide-mediated activation of Akt and extracellular regulated kinase signaling prevents lymphocyte apoptosis. FASEB J. 2008;22:561–568. doi: 10.1096/fj.07-8283com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rexhepaj R, et al. PI3-kinase-dependent electrogenic intestinal transport of glucose and amino acids. Pflugers Arch. 2007;453:863–870. doi: 10.1007/s00424-006-0154-6. [DOI] [PubMed] [Google Scholar]
- 39.Itoh M, et al. Involvement of ZO-1 in cadherin-based cell adhesion through its direct binding to alpha catenin and actin filaments. J Cell Biol. 1997;138:181–192. doi: 10.1083/jcb.138.1.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zeissig S, et al. Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn’s disease. Gut. 2007;56:61–72. doi: 10.1136/gut.2006.094375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Markov AG, et al. Segmental expression of claudin proteins correlates with tight junction barrier properties in rat intestine. J Comp Physiol B. 2010;180:591–598. doi: 10.1007/s00360-009-0440-7. [DOI] [PubMed] [Google Scholar]
- 42.Nose K, et al. Glutamine prevents total parenteral nutrition-associated changes to intraepithelial lymphocyte phenotype and function: a potential mechanism for the preservation of epithelial barrier function. J Interferon Cytokine Res. 2010;30:67–80. doi: 10.1089/jir.2009.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smyth D, et al. Interferon-gamma-induced increases in intestinal epithelial macromolecular permeability requires the Src kinase Fyn. Lab Invest. 2011;91:764–777. doi: 10.1038/labinvest.2010.208. [DOI] [PubMed] [Google Scholar]
- 44.McKay DM, et al. Phosphatidylinositol 3′-kinase is a critical mediator of interferon-gamma-induced increases in enteric epithelial permeability. J Pharmacol Exp Ther. 2007;320:1013–1022. doi: 10.1124/jpet.106.113639. [DOI] [PubMed] [Google Scholar]
- 45.Cario E, Gerken G, Podolsky D. Toll-Like Receptor 2 Controls Mucosal Inflammation by Regulating Epithelial Barrier Function. Gastroenterology. 2007;132:1359–1374. doi: 10.1053/j.gastro.2007.02.056. [DOI] [PubMed] [Google Scholar]
- 46.Arbibe L, et al. Toll-like receptor 2-mediated NF-kappa B activation requires a Rac1-dependent pathway. Nat Immunol. 2000;1:533–540. doi: 10.1038/82797. [DOI] [PubMed] [Google Scholar]
- 47.Malo MS, et al. Intestinal alkaline phosphatase preserves the normal homeostasis of gut microbiota. Gut. 2010;59:1476–1484. doi: 10.1136/gut.2010.211706. [DOI] [PubMed] [Google Scholar]
- 48.Wildhaber BE, et al. Lack of enteral nutrition--effects on the intestinal immune system. J Surg Res. 2005;123:8–16. doi: 10.1016/j.jss.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 49.Yasumatsu K, et al. Multiple receptors underlie glutamate taste responses in mice. Am J Clin Nutr. 2009;90:747S–752S. doi: 10.3945/ajcn.2009.27462J. [DOI] [PubMed] [Google Scholar]
- 50.Wu SV, et al. Expression of bitter taste receptors of the T2R family in the gastrointestinal tract and enteroendocrine STC-1 cells. Proc Natl Acad Sci U S A. 2002;99:2392–2397. doi: 10.1073/pnas.042617699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fujita Y, et al. Incretin release from gut is acutely enhanced by sugar but not by sweeteners in vivo. Am J Physiol Endocrinol Metab. 2009;296:E473–479. doi: 10.1152/ajpendo.90636.2008. [DOI] [PubMed] [Google Scholar]
- 52.Margolskee RF, et al. T1R3 and gustducin in gut sense sugars to regulate expression of Na+-glucose cotransporter 1. Proc Natl Acad Sci U S A. 2007;104:15075–15080. doi: 10.1073/pnas.0706678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xue H, Field CJ. New role of glutamate as an immunoregulator via glutamate receptors and transporters. Front Biosci (Schol Ed) 2011;3:1007–1020. doi: 10.2741/205. [DOI] [PubMed] [Google Scholar]
- 54.Akiba Y, et al. Luminal L-glutamate enhances duodenal mucosal defense mechanisms via multiple glutamate receptors in rats. Am J Physiol Gastrointest Liver Physiol. 2009;297:G781–791. doi: 10.1152/ajpgi.90605.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang JH, et al. Umami receptor activation increases duodenal bicarbonate secretion via glucagon-like peptide-2 release in rats. J Pharmacol Exp Ther. 2011;339:464–473. doi: 10.1124/jpet.111.184788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vermeulen MA, et al. Glutamate reduces experimental intestinal hyperpermeability and facilitates glutamine support of gut integrity. World J Gastroenterol. 2011;17:1569–1573. doi: 10.3748/wjg.v17.i12.1569. [DOI] [PMC free article] [PubMed] [Google Scholar]