Abstract
Objective
The U.S. Public Health Service Clinical Practice Guideline recommends that physicians provide tobacco cessation interventions to their patients at every visit. While many studies have examined the extent to which physicians implement the guideline's “5 A's”, few studies have examined the extent to which physicians implement the guideline's “5 R's” which are to be used in a Motivational Interviewing (MI) consistent style with smokers not ready to quit. This study examined the extent to which physicians in usual practice and without specific training administered the 5 R's including the use of an MI style.
Methods
Thirty-eight physicians were audio recorded during their routine clinical practice conversations with smokers.Recordings were coded by independent raters on the implementation of each of the 5 A's, 5 R's and MI counseling style.
Results
Results revealed that for patients not ready to quit smoking, physicians most frequently discussed the patient's personal relevance for quitting and the risks of smoking. Roadblocks and rewards were discussed relatively infrequently. MI skill code analyses revealed that physicians, on average, had moderate scores for acceptance and autonomy support, a low to moderate score for collaboration and low scores for empathy and evocation.
Conclusion
Results suggest that for the Clinical Guideline to be implemented appropriately physicians will need specialized training or will need to be able to refer patients to counselors with the necessary expertise. Counseling efforts could increase providers’ willingness to implement guideline recommendations and therefore to enhance the person-centeredness of clinical care.
Keywords: Clinical guideline implementation, empathy, motivational interviewing, patient-provider communication, person-centered healthcare, physician counseling skills, physician perspectives, self-efficacy, smoking cessation counseling
Introduction
Tobacco use remains the leading cause of preventable death in the U.S. and the U.S. Preventative Services Task Force recommends that physicians screen all adults for tobacco use and provide tobacco cessation interventions to their patients [1]. To help with this effort, the U.S. Public Health Service (USPHS) published the Clinical Practice Guideline [2-4] in which it is recommended that physicians implement a series of steps known as the “5 A's” with every individual patient. The 5 A's are: 1) ask about tobacco use at every visit; 2) advise all tobacco users to quit; 3) assess readiness to quit; 4) assist tobacco users (who are ready) with a quit plan and 5) arrange follow-up visits. For those who are unwilling to try to quit, the most recent version of the guideline recommends the use of principles of Motivational Interviewing [5,6] to implement the “5 R's” which are to: 1) encourage the patient to indicate the personal relevance for quitting tobacco use; 2) ask the patient to identify potential risks of tobacco use; 3) ask the patient to identify potential rewards of stopping tobacco use; 4) ask the patient to identify barriers or roadblocks to quitting and 5) the motivational intervention should be repeated every time an unmotivated patient visits the clinic setting. The guideline highlights 4 Motivational Interviewing principles which are to express empathy, develop discrepancy (between smoking behavior and the patient's goals and values), roll with resistance and support self-efficacy [5]. This approach is consistent with current efforts to increase the person-centeredness of clinical practice.
Although the guideline was created to encourage and assist health providers, the evidence to date suggests most physicians fail to comply with all of the steps [6-10]. For example, a national survey demonstrated that from 2001 to 2003, physicians failed to assess patients’ smoking status during 32% of the visits they conducted [11]. Similarly, poor rates of compliance for the guideline recommendations were also found in a sample of Medicaid enrollees who reported that at their last healthcare provider visit 13% of providers failed to ask about their smoking status, 35% failed to give advice on quitting, 49% failed to assess the patient's willingness to quit, 76% failed to offer any assistance and 87% failed to give follow-up appointments [12].
Although the evidence indicates that the guidelines are in general terms not adequately implemented, the majority of research studies have assessed providers’ adherence to the 5 A's through self-report surveys [11-13]. Retrospective reports by patients and physicians are subject to recall [14,15] and potential social desirability [16] biases. Few studies have conducted direct observation of physician-patient encounters to determine adherence to the guideline. Furthermore, another limitation of the literature is that few studies have examined physicians’ behavior toward patients who are not ready to quit smoking (i.e., adherence to the 5 R's). To date, only one study has reported on physician adherence to the 5 R's with patients who are not ready to quit smoking among a national random sample of African American physicians [7]. Balls et al's retrospective survey of physicians’ practices on tobacco cessation counseling indicated that the physicians were most likely to explain the risks of smoking (65%), provide examples of why quitting was relevant (59%) and ask their patients about the rewards of quitting (58%). The physicians were less likely to discuss roadblocks (33%) and use repetition (4%). The researchers did not assess adherence to Motivational Interviewing principles.
The purpose of this study was to use direct observation to examine the extent to which physicians adhered to guideline recommendations by: 1) completing the 5 A's and, for patients not ready to quit smoking, the 5 R's, 2) employing a counseling style that was consistent with MI principles when administering the 5 R's. Physicians in the study were not trained in Motivational Interviewing, which is recommended by the guideline. However, the goal of the study was to assess the extent to which physicians’ natural counseling styles corresponded with Motivational Interviewing principles.
Methods
Participants
To assess physician's adherence to the guideline and style of counseling, a research assistant shadowed patients during routine practice and made audio recordings of the encounters. This study was conducted at a primary care outpatient clinic in a non-profit hospital in a large Midwestern city. Procedures were approved and monitored by the affiliated Institutional Review Boards. Physicians and patients who were recruited for the study were told the study was focused on understanding counseling styles that physicians typically employ with their patients when talking about smoking. Forty-one physicians were approached with 38 agreeing to participate in the study (93%). Three refused because of limited time and/or scheduled patient appointments that day. Potential patient participants were identified as smokers by physicians’ schedule. Of the 56 potential patient participants invited, 48 agreed (86%) to be in the study. Seven participants refused because of limited time and/or not wanting to be involved in research.
Measures
Demographics and descriptive characteristics
Physicians and patients completed a brief questionnaire assessing demographic and descriptive characteristics including age, gender, ethnicity, income and physician's level of training.
Coding of audio recorded encounters
Audio-recordings of any patient-physician dialogue related to smoking were transcribed verbatim and coded by two independent raters based on the Clinical Practice Guideline and the Motivational Interviewing Skill Code Version 2.1 [17].
U.S. Public Health Service Clinical Practice Guideline
Following the 5 A's and 5 R's of the Clinical Practice Guideline [4] raters coded whether or not each step was followed. Specifically, raters coded whether or not the physician asked about tobacco use, advised the patient to quit, assessed readiness to quit, assisted with a quit plan if ready and arranged follow-up. For patients not ready to quit raters also coded whether the physician discussed the relevance of quitting for the patient, the potential risks of tobacco use, the potential rewards of stopping tobacco use and roadblocks to quitting. Raters did not code Repeat because raters only coded one audio file of the one interaction between the physician and patient.
MISC
The MISC is designed to assess counselor adherence to the principles of Motivational Interviewing. The system includes global ratings that reflect the overall impression and specific behavior counts of Motivational Interviewing consistent and Motivational Interviewing inconsistent behaviors. Global scores of the MISC include acceptance, empathy, collaboration, evocation and autonomy support which are defined in Table 1 and are rated on a 7-point Likert scale. Scores can range from 1 (low) to 7 (high) on adherence to MI principles with specific criteria given for low versus high ratings on each element. The threshold for competency on each of these scales has been suggested as 6 or higher [18].
Table 1.
Definitions of the Global Ratings of the MISC
| Style | Definition |
|---|---|
| Acceptance | Provider communicates unconditional positive regard for the patient. |
| Empathy | Provider understands or makes an effort to understand the patient's perspective. |
| Collaboration | Provider negotiates with their patient and avoids an authoritarian role. |
| Evocation | Provider emphasizes drawing out the patient's ideas instead of educating or giving information without permission. |
| Autonomy support | Provider conveys understanding that the variables associated with change are within the patient and cannot be imposed by others. |
MISC Behavior Count Categories
MISC behavioral categories coded included advice, affirm, confront, direct, emphasize control, giving information, question, raise concern, reflect, reframe, support and warn. These are defined in Table 2. Three of the categories require differentiating between subcategories. Specifically, the categories advise and raise concern both require determining if the advice or raising of concern was done with or without permission. Similarly, the behavioral category of question requires raters to determine if the question was closed (i.e., with a limited set of response options such as yes/no) or open-ended. As displayed in Table 2, all behavioral categories except for giving information are seen as either Motivational Interviewing consistent or Motivational Interviewing inconsistent. Motivational Interviewing consistent behaviors are believed to enhance patients’ motivation and benefit compared with MI inconsistent behaviors which are thought to be counter-productive [19-21].
Table 2.
Definitions and Examples of the Behavior Count Categories of the MISC
| Category | Definition | Example |
|---|---|---|
| Giving Information | Provider gives information to the patient, educates, or explains something. | “People who smoke can get COPD, emphysema and have a higher risk for lung cancer, heart disease and many other things.” |
| MI Consistent | ||
| Advise with Permission | The provider gives advice, makes a suggestion, or offers a solution with prior permission from the patient | “Would it be all right if I suggested something?” |
| Affirm | Provider comments on the strength or efforts made by the patient in the form of appreciation, confidence, or reinforcement | “You've made a huge cut in your smoking.” “You've accomplished a difficult task.” |
| Emphasize Control | Provider directly acknowledges the patient's freedom of choice and autonomy. | “It's your decision whether you quit or not.” “You're setting your own goals and boundaries.” |
| Open Question | Provider asks a question that allows a wide range of possible answers, seeks information, invites the patient's perspective | “Tell me about your smoking.” “How might you be able to do that?” |
| Raise Concern with Permission | With the patient's permission, the provider points out a possible problem with the patient's plan and contains language that demonstrates the provider's own concern rather than fact. | “Is it OK if I tell you a concern that I have about that? I wonder if it puts you in a situation where it might be easy to start smoking again.” |
| Reflection | Provider responds to the patient with a statement that repeats or rephrases what the patient has said. | “You don't like what smoking does to your health, but it reduces your stress.” “So you said you smoke about 10 cigarettes a day.” |
| Reframe | Provider changes the emotional valence of the patient's experience by placing it in a new light. | “Each attempt can move you closer to success.” In response to patient saying, “I've tried to quit before and failed.” |
| Support | Provider makes sympathetic, compassionate, or understanding comments | “That must have been difficult.” “I'm here to help you with this.” |
| MI Inconsistent | ||
| Advising without Permission | Without prior permission from the patient, the provider gives advice, makes a suggestion, or offers a solution or possible action. | “You could ask your friends not to smoke at your house.” |
| Confront | Provider directly disagrees, argues, corrects, shames, blames, criticizes, or questions the patient's honesty. | “Don't you understand what smoking is doing to your health?” “You're willing to jeopardize the baby's health just for cigarettes.” |
| Direct | Provider gives an order, command, or direction. | “You've got to stop smoking.” “You must have more respect for yourself.” |
| Closed Question | Provider asks a question that implies a short answer, specifies a restricted range, | “How long have you been smoking?” “On a scale from 1 to 10, how motivated are you to quit?” |
| Raise Concern without Permission | Without the permission of the patient, the provider points out a possible problem with the patient's plan and contains language that demonstrates the provider's own concern rather than fact. | “I'm worried that you may have trouble when you're around your old friends.” |
| Warn | Provider warns or threatens the patient, implying negative consequences if the patient does not take a certain action. | “If you get bored you'll smoke.” “You're going to relapse if you don't get out of this relationship.” |
Procedure
Two raters were trained and supervised by an expert in Motivational Interviewing (DC) in the use of the coding scheme until an acceptable level of inter-rater reliability was reached on consecutive practice sessions. The coders first listened to the audio-recordings of the consultation without stopping and then reviewed the transcript to conduct behavioral counts. Global ratings were then completed and, lastly, scores on administration of each of the 5 A's and 5 R's were given. Disagreements between coders were discussed and final decisions were made by consensus. All the audio-recordings were double coded and inter-rater reliability was assessed.
Analysis
Descriptive statistics were used to describe basic characteristics of the sample (e.g., age, level of experience and gender). Frequencies and means were used as appropriate to describe the use of the 5 A's and/or 5 R's and adherence to MI principles.
Results
Sample Characteristics
Participants included both physicians (54%) and physicians in training (46%) and included a nearly equal proportion of men and women (51% female). Physician's ages ranged from 25 to 72 years old (M = 37.56, SD = 10.83). Sixty-seven percent of the physicians identified as White, 17% identified as Asian and 16% identified as ‘other’. Patient participant's ages ranged from 25 to 67 years old (M = 46.19, SD = 9.96) and included a slightly higher proportion of women than men (57% female). The majority of patients identified as African-American (65%) and had an income ≤ $2,000 a month (73%). Audio-recordings of 38 physician-patient encounters were analyzed and each physician contributed only one sample recording.
The MISC also provides summary scores of key indexes of MI adherence derived from the behavioral categories and these can be compared with suggested thresholds competent performance (see Table 3).
Table 3.
Physician's Proficiency and Competency
| Behavior Indicator | Formula for Summary | Summary Score | Competency |
|---|---|---|---|
| Percent Open Questions (%OQ) | Open Questions/Open + Closed Questions | 14% | 70% |
| Reflection to Question Ratio (%R/Q) | Total Reflections/ Open + Closed Questions | 0.53 | 2 |
| Percent MI-Consistent (%MICO) | MI-Consistent/MI- Consistent + MI- Inconsistent | 39% | 100% |
Inter-rater Reliability
Inter-rater reliability for the rating the 5 A's and 5 R's, MISC global ratings and behavioral categories was assessed by calculating the intra-class correlation coefficient (ICC). The ICC is a conservative measure that takes the frequency of equal ratings into account, as well as the possible systematic differences between raters into account [22]. Guidelines for assessing the ICC coefficient are: 1.00 - 0.75 is excellent; 0.74 - 0.60 is good, 0.40 - 0.59 is fair and < 0.40 is poor [23]. As displayed in Tables 4 and 5, the ICC coefficients for MISC Global scores and MISC behavioral categories ranged from 0.50 (Autonomy-support) to 0.965 (number of closed questions), with the majority of the ratings in the “good” to “excellent” range.
Table 4.
Mean Frequencies, Range and ICC of MISC Global Scores
| MI Variable | Mean (SD) | Range | ICC |
|---|---|---|---|
| Acceptance | 4.53 (1.11) | 2-7 | 0.743 |
| Autonomy support | 4 (0.96) | 1-6 | 0.496 |
| Collaboration | 3.32 (1.12) | 1-6 | 0.671 |
| Empathy | 2.95 (1.37) | 1-6 | 0.763 |
| Evocation | 2.74 (1.06) | 1-6 | 0.600 |
Table 5.
Mean Frequencies, Range and ICC of MISC Behavioral Categories
| MI Variable | Mean (SD) | Range | ICC |
|---|---|---|---|
| Giving information | 4.89 (5.06) | 0-20 | 0.895 |
| MI Consistent | |||
| Advise with permission | 0.03 (0.16) | 0-1 | 0.570 |
| Affirm | 1.26 (2.09) | 0-8 | 0.944 |
| Emphasize control | 0.39 (0.86) | 0-3 | 0.856 |
| Open questions | 1.03 (1.15) | 0-4 | 0.933 |
| Reflections | 3.34 (4.33) | 0-24 | 0.924 |
| Support | 0.32 (0.57) | 0-2 | 0.688 |
| Reframe | 0.13 (0.41) | 0-2 | 0.727 |
| MI Inconsistent | |||
| Advise without permission | 2.37 (2.58) | 0-9 | 0.787 |
| Confrontation | 0.13 (0.41) | 0-2 | 0.725 |
| Closed questions | 6.18 (5.00) | 0-23 | 0.965 |
| Raise concern without permission | 0.68 (1.34) | 0-5 | 0.783 |
| Warn | 0.61 (1.50) | 0-8 | 0.881 |
Physician use of the 5 A's and 5 R's
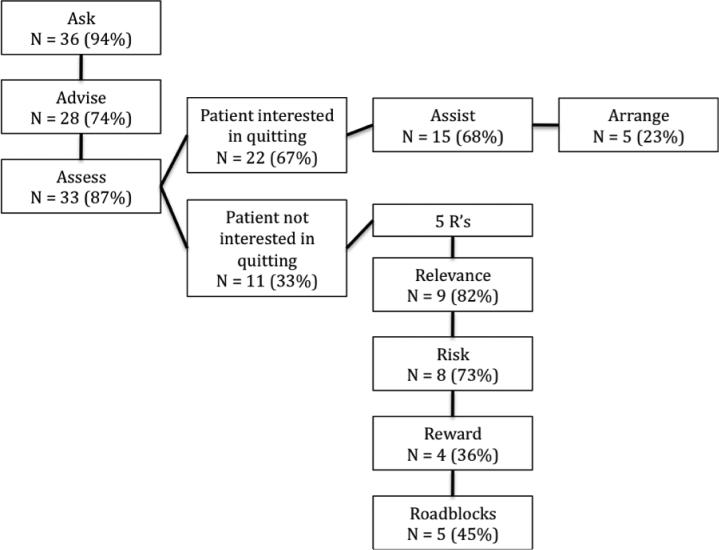
Figure 1 presents the frequency with which physicians used the 5 A's and 5 R's with their patients for quitting smoking. With respect to the 5A's, almost all physicians asked about patient's smoking status and a high proportion also advised their patient to quit and assessed their patient's interest in quitting. Physicians were less likely to offer their patient assistance to quit and only a small proportion of physicians arranged a follow-up appointment.
Figure 1.
Physician use of 5 A's and R's. This figure presents the frequency with which physicians used the 5 A's and 5 R's with their patients for quitting smoking
Regarding the 5 R's, physicians are encouraged to administer all of the 5 R's with patients who are advised to quit but indicate they are not ready to quit. As can be seen in Figure 1, of the patients who were assessed for readiness to quit by physicians, one-third communicated that they were not ready to quit. With these patients a high proportion of physicians discussed the personal relevance of quitting and the great majority discussed the risks of smoking. However, fewer than half of the physicians discussed the roadblocks to quitting and the rewards of quitting.
MISC Global scores
The results of the MISC coding of global dimensions are presented in Table 4. Based on the suggested threshold for competency of 6 or greater out of 7, the mean MISC global scores indicated that physicians, on average, had moderate to poor scores on the global dimensions. Scores were moderate for acceptance and autonomy support, low-moderate for collaboration and low for empathy and evocation.
MISC Behavioral Categories
The results of MISC coding of the behavioral categories are displayed in Table 5.
Overall, coding revealed that physicians were most likely to give information during counseling sessions. Physicians also more frequently used Motivational Interviewing inconsistent strategies than Motivational Interviewing consistent strategies. Specifically, physicians were most likely to rely on the Motivational Interviewing inconsistent strategies of asking closed questions and advising without permission. Physicians rarely raised concern without permission or providing warnings and were least likely to use confronting.
In terms of MI consistent strategies, physicians were most likely to provide reflective and affirming statements. However, they were unlikely to ask for permission before offering advice, reframe patients’ statements, make supportive statements or emphasize patients’ control.
With respect to the summary indexes, physicians in the present study were well below the recommended thresholds for competence, with a relatively low percent of open questions asked, a low ratio of reflections to questions and an overall low proportion of Motivational Interviewing consistent statements.
Discussion
The purpose of the current study was to directly observe the content and communication styles physicians employ when counseling their patients about smoking. With respect to following the steps of the 5A's outlined in the clinical guideline, the current study indicated that a very high proportion of physicians asked patients about their smoking status (95%) which compares very favorably with a rate of 68% reported in a 2001-2003 national survey [11].
Although not as many physicians advised their patients to quit (74%) or assessed their patient's readiness to quit (87%), these proportions were relatively high and also compared favorably to previous findings [11]. Of the 5A's, the steps physicians were least likely to complete were the final steps of offering their patients assistance to quit (68%) and arranging follow-up (23%). This pattern is similar to the pattern observed in prior studies although the absolute rates for these steps were also higher than previously reported (e.g., 24% for assist and 13% for arrange; [12,24]).
With respect to following the steps of the 5 R's, similar to the study by Balls and colleagues [7], physicians were most likely to discuss the relevance (82%) and risks of smoking (73%) with patients and much less likely to address rewards of quitting (36%) and roadblocks (45%) to quitting. While it is encouraging that physicians are generally discussing the personal relevance of quitting and highlighting the risk of smoking, the lack of attention to all the elements suggests potential opportunities for enhancing motivation may be being missed and that physicians may not intuitively think of exploring these areas.
Overall, these findings are similar to those of other studies [8-10] in that physicians generally failed to adhere to all of the components of the USPHS Guideline. The generally higher frequency of adherence to the steps than observed in previous studies may perhaps be attributable to the stimulus cue of having a research assistant in the room during the appointment, but physicians were not in any way informed or reminded of the clinical guideline prior to the study which suggests that these behaviors were not inconsistent with their regular training and practice. Furthermore, in spite of any elevation in performance compared to usual practice, the findings highlight that physicians are still in need of encouragement and assistance to complete all of the elements. With respect to the extent to which the recommended principles of Motivational Interviewing were followed when completing the 5 R's, the results indicated that physicians’ scores were relatively low. However, physicians were able to communicate acceptance and support for their patient's autonomy to a moderate extent which is encouraging, given that physicians were working with low income patients that mostly had a different ethnic background than themselves. Unfortunately, the physicians were low on communicating empathy, evoking their patient's ideas and fostering collaboration, key elements of person-centered practice.
Results were similar with respect to specific MI consistent and inconsistent behaviors where physician's use of MI consistent skills was low and well below thresholds of competence. However, it is important to note that physicians very rarely used confrontation (i.e., arguing, shaming, blaming and questioning patients’ honesty) which appears to be the most damaging MI inconsistent behavior [19,20]. Of the MI inconsistent strategies physicians were most likely to use closed questions which, although less damaging, likely contributed to the lack of empathy, collaboration and evocation. The behavior counts also suggested that whereas physicians’ motivational efforts relied very little on MI consistent evoking strategies (such as open questions and reflections), but rather focused on giving information.
Taken together the findings suggest that while physicians are accepting of their patients’ struggles with smoking and recognize that the decision to change needs to be placed in the hands of the patient, they are not sufficiently engaging patients in a collaborative dialogue that fully explores all aspects of the patients motivation and perceived obstacles. This likely reflects physicians’ lack of training and skill in advanced motivational counseling techniques [7,25,26] that would go beyond simply providing information. It likely also reflects systemic constraints such as lack of time for engaging in more extended dialogues [27-29]. Similar results have been found among primary care residents discussing alcohol consumption with patients [30]. Residents who were not trained in MI were less likely to use person-centered strategies compared to the trained residents. Although this study provides novel findings regarding physician's motivational counseling efforts, a number of limitations should be acknowledged. As noted, the findings likely represent the “best case scenario” in terms of physician practice because the audio recordings were made with a research assistant present who may have cued more smoking related treatment. This study also relied on a relatively small convenience sample of physicians and physician residents, who may not be representative of physicians practicing in many other settings. However, the general pattern of findings is similar to those observed in other studies which increases confidence in the findings.
Conclusion
This naturalistic and observationally-based evaluation of physician's efforts to address smoking with their patients highlights the ongoing need to improve treatment for one of the most important health problems in the U.S. While physicians are making efforts in this arena their treatment continues to fall well short of the empirically supported treatment guidelines. This study highlights that physicians lack the necessary advanced counseling skills for motivating patients. There is a great need to identify more effective ways to provide individual patients with the empirically supported treatment they deserve, whether through improved physician training or systems of referral to trained counselors. Without such approaches, a move to person-centered care in this context is likely to be impeded.
Acknowledgements
Research reported in this article was partially supported by the National Cancer Institute of the National Institutes of Health under award number R01CA133068.
Footnotes
Conflicts of Interest
The author declare no conflict of interest.
References
- 1.U.S. Preventive Services Task Force . Guide to Clinical Preventive Services. Second Edition Office of Disease Prevention and Health Promotion; Washington, DC: 1996. [Google Scholar]
- 2.Fiore M, Bailey WC, Cohen SJ, et al. Smoking cessation: Clinical practice guideline no. Vol. 18. US Department, of Health and Human Services, Public Health Service; Maryland: 1996. [Google Scholar]
- 3.Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: Clinical practice guideline. US Department of Health and Human Services, Public Health Service; Maryland: 2000. [Google Scholar]
- 4.Fiore MC, Jaén CR, Baker TB, et al. Clinical Practice Guideline. U.S. Department of Health and Human Services Public Health Service; Maryland: 2008. Treating tobacco use and dependence: 2008 Update. [Google Scholar]
- 5.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd edn. Guilford Press; New York: 2002. [Google Scholar]
- 6.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 3rd edn. Guilford Press; New York: 2012. [Google Scholar]
- 7.Balls JE, Price JH, Dake JA, Jordan TR, Khuder S. African American Primary Care Physicians' Perceptions and Practices Regarding Smoking Cessation. Journal of the National Medical Association. 2010;102:579–589. doi: 10.1016/s0027-9684(15)30635-0. [DOI] [PubMed] [Google Scholar]
- 8.Ferketich AK, Khan Y, Wewers ME. Are physicians asking about tobacco use and assisting with cessation? Results from the 2001–2004 national ambulatory medical care survey. Preventive Medicine. 2006;43:472–476. doi: 10.1016/j.ypmed.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Jordan TR, Dake JR, Price JH. Best practices for smoking cessation in pregnancy: Do obstetrician / gynecologists use them in practice? Journal of Women's Health. 2006;15:400–441. doi: 10.1089/jwh.2006.15.400. [DOI] [PubMed] [Google Scholar]
- 10.Stevens VJ, Solberg LI, Quinn VP, Rigotti NA, Hollis JA, Smith KS, Zapka JG, France E, Vogt T, Gordon N, Fishman P, Boyle RG. Relationship between tobacco control policies and the delivery of smoking cessation services in nonprofit HMOs. Journal of the National Cancer Institute Monographs. 2005;35:75–80. doi: 10.1093/jncimonographs/lgi042. [DOI] [PubMed] [Google Scholar]
- 11.Thorndike AN, Regan S, Rigotti NA. The Treatment of Smoking by US Physicians During Ambulatory Visits: 1994–2003. American Journal of Public Health. 2007;97:1878–1883. doi: 10.2105/AJPH.2006.092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chase EC, McMenamin SB, Halpin HA. Medicaid provider delivery of the 5A's for smoking cessation counseling. Nicotine & Tobacco Research. 2007;9:1095–1101. doi: 10.1080/14622200701666344. [DOI] [PubMed] [Google Scholar]
- 13.Ward MM, Vaughn TE, Uden-Holman T, Doebbeling BN, Clarke WR, Woolson RF. Physician knowledge, attitudes and practices regarding a widely implemented guideline. Journal of Evaluation in Clinical Practice. 2002;8:155–162. doi: 10.1046/j.1365-2753.2002.00337.x. [DOI] [PubMed] [Google Scholar]
- 14.Bradburn N, Rips L, Shevell S. Answering autobiographical questions: the impact of memory and inference on surveys. Science. 1987;236:157–161. doi: 10.1126/science.3563494. [DOI] [PubMed] [Google Scholar]
- 15.Gorin AA, Stone AA. Recall biases and cognitive errors in retrospective self-reports: A call for momentary assessments. In: Baum A, Revenson T, Singer J, editors. Handbook of Health Psychology. Erlbaum; New Jersey: 2001. [Google Scholar]
- 16.Nederhof A. Methods of coping with social desirability bias: a review. European Journal of Social Psychology. 1985;15:263–280. [Google Scholar]
- 17.Moyers T, Martin T, Catley D, Harris KJ, Ahluwalia JS. Assessing the integrity of motivational interviewing interventions: Reliability of the Motivational Interviewing Skills Code. Behavioural and Cognitive Psychotherapy. 2003;31:177–184. [Google Scholar]
- 18.Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Catley D, Harris KJ, Mayo MS, Hall S, Okuyemi KS, Boardman T, Ahluwalia J. Adherence to principles of motivational interviewing and client within-session behavior. Behavioural and Cognitive Psychotherapy. 2006;34:43–56. [Google Scholar]
- 20.Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using Motivational Interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? Journal of Substance Abuse Treatment. 2006;31:329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology. 2009;77:1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shrout PE, Fleiss JL. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychology Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 23.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6:284–290. [Google Scholar]
- 24.Goldstein MG, Niaura R, Willey-Lessne C, DePue J, Eaton C, Rakowski W, Dube C. Physicians counseling smokers. A population-based survey of patients' perceptions of health care provider–delivered smoking cessation interventions. Archives of Internal Medicine. 1997;157:1313–1319. doi: 10.1001/archinte.157.12.1313. [DOI] [PubMed] [Google Scholar]
- 25.Applegate B, Sheffer C, Payne T, Crew K, Payne T, Smith P. A survey of the tobacco related knowledge, attitudes, and behaviors of primary care providers in Mississippi. Journal of Evaluation in Clinical Practice. 2008;14:537–544. doi: 10.1111/j.1365-2753.2007.00910.x. [DOI] [PubMed] [Google Scholar]
- 26.Richmond R, Zwar N, Taylor R, Hunnisett J, Hyslop F. Teaching about tobacco in medical schools: A worldwide study. Drug and Alcohol Review. 2009;28:484–497. doi: 10.1111/j.1465-3362.2009.00105.x. [DOI] [PubMed] [Google Scholar]
- 27.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PC, Rubin HR. Why don't physicians follow clinical practice guidelines? A framework for improvement. Journal of the American Medical Association. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 28.Orleans CT, Glynn TJ, Manley MW, Slade J. Minimal contact quit smoking strategies for medical settings. In: Orleans CT, Slade J, editors. Nicotine Addiction Principles and Management. Oxford University Press; New York: 1993. [Google Scholar]
- 29.Walsh JM, McPhee SJ. A systems model of clinical preventive care: An analysis of factors influencing patient and physician. Health Education Quarterly. 1992;19:157–175. doi: 10.1177/109019819201900202. [DOI] [PubMed] [Google Scholar]
- 30.Chossis I, Lane C, Gache P, Michaud PA, Pecoud A, Rollnick S, Daeppen JB. Effect of training on primary care residents' performance in brief alcohol intervention: A randomized controlled trial. Journal of General Internal Medicine. 2007;22:1144–1149. doi: 10.1007/s11606-007-0240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]