There is growing evidence that obese adults without metabolic risk factor clustering (the so-called “healthy obese”) progress to unhealthy obesity over time (1). However, the pathophysiological changes underlying the long-term transition into an unhealthy obese state have not been well characterized. To inform clinical management of healthy obesity, we aimed to identify the metabolic risk factors responsible for this transition, as well as the timing of their onset.
Repeat clinical data were drawn from the Whitehall II cohort study of British adults. We grouped participants as normal-weight (body mass index [BMI] 18.5 to 24.9 kg/m2), overweight (BMI 25 to 29 kg/m2), or obese (BMI ≥30 kg/m2), and as healthy (2) if they were free of any the following characteristics: high-density lipoprotein cholesterol <1.03 mmol/l (men) and <1.29 mmol/l (women); blood pressure ≥130/85 mm Hg or antihypertension medication use; fasting plasma glucose ≥5.6 mmol/l or diabetic medication use; triglycerides ≥1.7 mmol/l; and homeostatic model–assessed insulin resistance >2.83 (baseline 90th percentile value). Participants provided written informed consent. The University College London research ethics committee provided ethical approval.
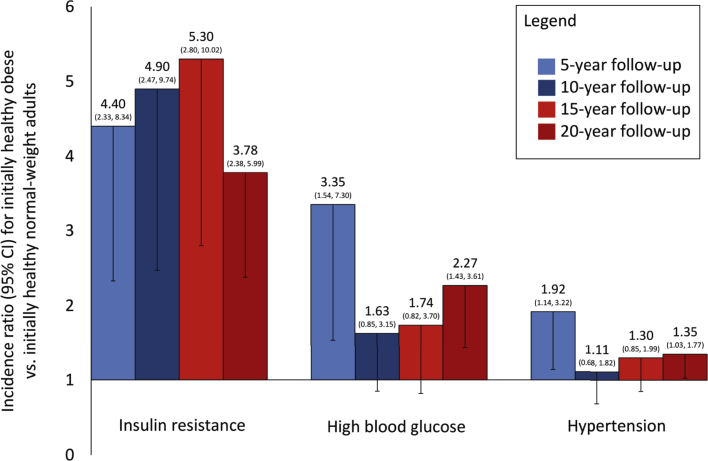
Cross-tabulations were used to describe incidence of each of these 5 metabolic risk factors at 5- (1997 to 1999), 10- (2002 to 2004), 15- (2007 to 2009), and 20-year (2012 to 2014) follow-ups for healthy normal-weight, overweight, or obese participants at baseline (1992 to 1994). Poisson regression models with robust error variances were used to estimate age-, sex-, and ethnicity-adjusted incidence ratios and 95% confidence intervals for having each metabolic risk factor at follow-up for healthy obese compared with healthy normal-weight adults at baseline.
Among 2,878 adults with anthropometric and metabolic risk factor data at each time point, 1,120 adults (39 to 61 years of age; 68% male) were free of all metabolic risk factors at baseline. This initially healthy status was progressively rarer among those in higher BMI groups, representing 51.5%, 25.8%, and 13.4% of normal-weight, overweight, and obese adults, respectively. Of the healthy obese participants, 57.1% had at least 1 metabolic risk factor at the 5-year follow-up, with corresponding proportions being 64.3% at 10 years and 78.6% at 20 years. These proportions were smaller (32.8%, 46.7%, and 60.3%) among initially healthy normal-weight participants.
After 5 years (Figure 1), relative to initially healthy normal-weight adults, initially healthy obese adults were 4.40 times more likely to be insulin resistant, 3.35 times more likely to have high blood glucose, and 1.92 times more likely to be hypertensive (all p < 0.05). Incident insulin resistance remained higher over all subsequent follow-ups among baseline healthy obese compared with healthy normal-weight adults. Case numbers were small for 20-year incidence of low high-density lipoprotein cholesterol (2 cases) and high triglycerides (3 cases) among healthy obese adults, with little difference in risk compared with healthy normal-weight adults over time. Additional data are available on request.
Figure 1.
Incidence of Metabolic Risk Factors Among Initially Healthy Obese Compared With Initially Healthy Normal-Weight Adults Over 20 Years (n = 1,120)
Results are incidence ratios and 95% confidence intervals (CI) for having each metabolic risk factor at follow-up, on the basis of Poisson regression models with robust error variances. Models are adjusted for age, sex, and ethnicity. Little difference in high-density lipoprotein cholesterol or triglycerides was observed between groups. Baseline healthy status is defined as having none of 5 metabolic risk factors (hypertension, low high-density lipoprotein cholesterol, high triglycerides, insulin resistance, and high blood glucose).
The risk of developing insulin resistance, high blood glucose, and hypertension was 2 to 5 times higher among initially healthy obese adults compared with their healthy normal-weight counterparts, and these changes were evident after only 5 years of follow-up. There was little difference in progression to dyslipidemia. However, the key factor explaining the long-term decline of healthy obesity was insulin resistance, which was consistently most common among healthy obese adults over time.
Healthy obese adults are known to experience an elevated future risk of type 2 diabetes (3) and cardiovascular disease (4) compared with healthy normal-weight counterparts. That insulin resistance is an established indicator of future impaired glucose metabolism (5) may explain their much higher incidence of type 2 diabetes (relative risk near 4.0) (3) and slightly higher incidence of cardiovascular disease (relative risk near 1.2) (4), given that earlier onset of risk factors leads to a greater cumulated exposure and higher disease risk. Overall, our findings suggest that healthy obesity is strongly linked with future insulin resistance that subsequently induces cardiometabolic pathology.
Footnotes
Please note: Mr. Bell is supported by an Economic and Social Research Council (ESRC) studentship. Dr. Hamer is supported by the British Heart Foundation (RE/10/005/28296). Dr. Singh-Manoux has received research support from the U.S. National Institutes of Health (NIH) National Institute of Aging (NIA) (R01AG013196; R01AG034454). Dr. Sabia has received research support from the NIH NIA (R01AG034454) and ESRC (ES/J023299/1). Dr. Kivimäki has received research support from the Medical Research Council (MR/K013351/1); the National Heart, Lung, and Blood Institute (R01HL36310); the NIA (R01AG034454); NordForsk (75021); and an ESRC professorial fellowship (ES/J023299/1). The funders had no role in the study design; in the collection, analysis and interpretation of data; in writing of the report; or in the decision to submit the paper for publication. The developers and funders of Whitehall II do not bear any responsibility for the analyses or interpretations presented here. The authors declare that there is no duality of interest associated with this manuscript. Dr. Batty has reported that he has no relationships relevant to the contents of this paper to disclose. The authors thank all of the participating civil service departments and their welfare, personnel, and establishment officers; the British Occupational Health and Safety Agency; the British Council of Civil Service Unions; all participating civil servants in the Whitehall II study; and all members of the Whitehall II study team. The Whitehall II Study team comprises research scientists, statisticians, study coordinators, nurses, data managers, administrative assistants and data entry staff, who make the study possible. Whitehall II data, protocols, and other metadata are available to bona fide researchers for research purposes. Please refer to the Whitehall II data sharing policy.
References
- 1.Bell J.A., Hamer M., Sabia S. The natural course of healthy obesity over 20 years. J Am Coll Cardiol. 2015;65:101–102. doi: 10.1016/j.jacc.2014.09.077. [DOI] [PubMed] [Google Scholar]
- 2.Wildman R.P., Muntner P., Reynolds K. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering - prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004) Arch Intern Med. 2008;168:1617–1624. doi: 10.1001/archinte.168.15.1617. [DOI] [PubMed] [Google Scholar]
- 3.Bell J.A., Kivimaki M., Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15:504–515. doi: 10.1111/obr.12157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kramer C.K., Zinman B., Retnakaran R. Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Ann Intern Med. 2013;159:758–769. doi: 10.7326/0003-4819-159-11-201312030-00008. [DOI] [PubMed] [Google Scholar]
- 5.Tabák A.G., Jokela M., Akbaraly T.N. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet. 2009;373:2215–2221. doi: 10.1016/S0140-6736(09)60619-X. [DOI] [PMC free article] [PubMed] [Google Scholar]