Abstract
Despite improvements in service delivery and patient management, low birth weight among infants has been a persistent challenge in South Africa. The study aimed to explore the relationship between depression before pregnancy and the low birth weight (LBW) of infants in post-apartheid South Africa. This study utilized data from Waves 1 and 2 of the South African National Income Dynamics Study, the main outcome being a dichotomous measure of child LBW (<2500 g) drawn from the Wave 2 child questionnaire. Depressive symptoms of non-pregnant women was the main predictor drawn from the Wave 1 adult questionnaire. Depressive symptoms were screened using the 10-item four-point Likert version of the Center for Epidemiologic Studies Depression Scale (CES-D) instrument. A total score of 10 or greater on the CES-D indicates a positive screen for depressive symptoms. An adjusted logistic regression model was used to examine the relationship between women’s depression before pregnancy and infant LBW. A sample size of 651 women in Wave 1 was linked to 672 newborns in Wave 2. The results of the adjusted logistic regression model indicated depressive symptoms (CES-D ≥ 10) prior to pregnancy were associated with infant LBW (adjusted OR 2.84, 95 % CI 1.08–7.46). Another significant covariate in the model was multiple childbirths. Our finding indicates that women’s depressive symptoms prior to pregnancy are associated with the low birth weight of newborns and suggests that this association may not be limited to depression present during the ante-natal phase.
Keywords: Depression prior to pregnancy, Low birth weight, South Africa
Introduction
Low birth weight (LBW), a serious adverse pregnancy outcome, is one of the leading causes of perinatal mortality as well as short- and long-term neonatal morbidity in infants and children [1]. For mothers, giving birth to and caring for LBW infants may be a stressful experience and includes the risk of depression [2]. Efforts to improve women’s and children’s health are ongoing public health challenges in South Africa [3]. Infant morbidity problems, such as LBW, remain a significant cause for concern in that country. With the proportion of LBW newborns (12–15 %) in South Africa being approximately twice that of the Organisation for Economic Cooperation and Development’s average estimate [4], the magnitude of the public health challenge is considerable.
The etiology of infant LBW is often unclear, but studies suggest a host of factors, including but not limited to: smoking, racial/ethnic disparities, age, multiple pregnancies, and hypertension [5–9]. Structural barriers, such as the lack of pre-natal care at the community level [10], are understood to be a risk factor for infant LBW. Furthermore, studies have indicated that depression, an issue affecting approximately 39 % of pregnant women in South Africa [11], may be an additional significant risk factor for LBW; a meta-analysis of studies from developing countries has indicated that maternal depression or psychological distress during pregnancy is one of the most significant risk factors for and a correlate of LBW [12].
The impact of depression in women (during pregnancy and postpartum) on child outcome is a complex phenomenon that requires consideration of the chronicity, severity and timing of maternal depressive symptomatology in relation to childbirth [13]. Much of the current research in the field has focused on depression during ante-natal phases, with the results indicating that a prior history of depression is a significant risk factor for ante-natal depression [14]. Few studies have investigated women’s mental health before pregnancy begins; a U.S. study, however, found that approximately half of the women with post-natal depression felt depressed before or during pregnancy [15]; this finding has significant implications for developing countries, where mental health treatment is often not readily offered. In South Africa, despite the prevalence of depression for pregnant women, research suggests a treatment gap (as high as 75 % in one report [16]) in access to services for common mental disorders.
To date, few studies have explored the independent association between depression before pregnancy and newborn LBW. While a limited number of studies in developed nations have examined the possible impact of broad maternal measures, including preconception stress [17] and mental health status [18] on adverse birth outcomes, even fewer have looked at the issue of depression before pregnancy, specifically in sub-Saharan Africa. The purpose of our current study was to explore this relationship in South Africa with the hypothesis that significant depressive symptoms in women before pregnancy are associated with a greater risk of their having LBW newborns.
Methods
Study Design and Sample
This study analyzed publicly available data from the first (version 4) and second waves (version 2) of the South African National Income Dynamics Study (SA-NIDS). Designed as the first longitudinal panel survey of a nationally representative sample of households in South Africa, Waves 1 and 2 assessments of the SA-NIDS were initiated in 2008 and 2010 respectively. A stratified, two-stage cluster sample design was used for the SA-NIDS. The household datasets contained approximately 7300 (2008) and 6800 (2010) successfully participating households across 400 primary sampling areas, with the proportion of household responses being 67 and 74 % for Waves 1 and 2 respectively. Household, adult and childhood questionnaires were administered by trained fieldworkers in all three waves. In Waves 1 and 2, the household questionnaires were completed by the oldest woman in the household or by another household member knowledgeable about the living arrangements. The adult questionnaires were administered to every consenting household member aged 15 or older in Waves 1 and 2, and included approximately 15,600 and 17,600 successfully interviewed participants, resulting in response rates of 93 and 96 % for Waves 1 and 2 respectively.
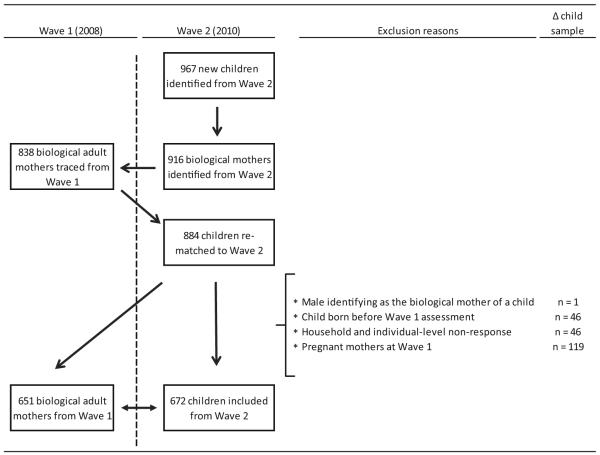
In Wave 2, approximately 9,850 child questionnaires were successfully administered to mother/caregiver of children aged 14 years and younger, or another household member who was knowledgeable about the child, with the proportion of successful response being 98 %. Using a retrospective cohort method, our study focused on the 672 Wave 2 child study participants (born between both waves’ assessments) for whom the 651 biological mothers who were not pregnant during Wave 1 could be identified (some being multiple births) after an exclusion process. The identification process of the study participants is described in Fig. 1. The exclusion criteria for child study participants included: (a) his or her being born before Wave 1, and (b) household- or individual-level non-response/availability. The exclusion criteria for the female study participants included: (a) pregnancy during Wave 1 assessment and (b) any male identifying as the biological mother of the child. The use of the SA-NIDS de-identified data was deemed exempt by the University of KwaZulu-Natal Biomedical Research Ethics Committee (EXM04/13).
Fig. 1.
Sample flow chart
Measures
Child low birth weight (LBW), defined as a weight of <2500 g, was an important variable in the childhood questionnaire. Child weight is based on self-report, and gestational age in weeks was not available. Depressive symptoms, the main predictor of our study, were identified from the Wave 1 adult questionnaire, and were assessed using the Center for Epidemiologic Studies Depression (CES-D) scale [19], a widely used screening tool for depression with valid psychometric properties [20]. SA-NIDS utilized the shorter 10-item version of the CES-D scale [21]. Study participants were asked how often they had experienced symptoms associated with depression over the past week: “0” being “rarely or none of the time (<1 day)” and “3” being “almost or all of the time (5–7 days).”A total of 10 or more on this scale indicates a positive screen for significant depressive symptoms and the possibility of a depressive disorder being present [21].
Statistical Analysis
First, the demographic and clinical characteristics of newborn children from Wave 2 (i.e. born between both waves’ assessments) and female study participants from Wave 1 who were younger than 50 years old were described. Analyses involving proportion (%) were adjusted by post-stratification weight from corresponding waves. Secondly, we conducted bivariate analyses to determine the association between demographic/clinical factors and child birth weight (<2500 and ≥2500 g) and depression status among the “future mothers” in Wave 1 (i.e. matched to children in Wave 2) based on self-report (CES-D scores of <and ≥10) using Pearson Chi-square statistics (χ2). While second-order Rao and Scott [22] design-adjusted Pearson χ2 is preferable for analyzing survey data with a complex design, a narrow sub-population focus containing stratum with a single sampling unit limited the use of this procedure. Lastly, analyses involving unadjusted and adjusted logistic regression were used to explore the association between depression in the above-mentioned women at Wave 1 and child LBW outcome at Wave 2. The adjusted regression model controlled for characteristics of women, children and household; specifically, data on women included race, education, age, perceived health, marital status, settlement type, employment status, cigarette smoking status, high blood pressure or diabetes, and body mass index (BMI) classification. Child data included race, gender, government child support status, and number of siblings born after Wave 1, with the household data consisting of residential geographical location. Furthermore, we controlled for whether the study participant had experienced childbirth 1 year prior to the Wave 1 assessment in a separate regression model as the post-natal period may be an important confounder. Strong measures of medication use, alcohol consumption, and pre-term child outcome were not available. Regressions predicting child outcome were adjusted from the post-stratification weight in Wave 2. Post-stratification weights were adjusted to the agesex-race distribution produced by Statistics South Africa based on population estimates. To address concerns related to missing values in complex survey data, we performed (100) multiple imputations by chained equations. The regression analyses were based on a dataset with imputation. All analyses were conducted using STATA 13.
Results
Our results were based on a final study sample size of 651 women in Wave 1 who were linked to 672 newborns in Wave 2. They are presented with respect to the child and adult sample characteristics, and the relationship between women’s depressive symptoms before pregnancy and child low birth weight.
Child and Adult Sample Characteristics
Newly born child study participants (Wave 2) were 51.9 % female and 84.7 % Black African, with 58.5 % being recipients of government child support and 8.4 % being part of multiple birth groups. The weighted mean age of the maternal respondents was 25.5 years old, with the majority being Black African (88.9 %), approximately two-thirds having completed high school equivalent schooling (69.2 %), and 65.4 % having never been married. Approximately 7.1 % were cigarette smokers and 4.3 % had either high blood pressure or diabetes. More than a quarter of the sample was obese (25.7 %).
Infant Low Birth Weight and Maternal Depressive Symptom Covariates
Of the newly born child study participants in Wave 2, 14.8 % were reported to weigh <2500 g. The analyses by low/normal birth weight (Table 1) indicate that the number of siblings born after Wave 1 (χ2 = 13.5, p = 0.01) was associated with child low birth weight. There was no association between LBW and gender, race, or government child support recipient status.
Table 1.
Child characteristics at Wave 2
| Variable | Categories | Overall |
Normal birth weight (≥2500 g) |
Low birth weight (<2500 g) |
χ2, p | |||
|---|---|---|---|---|---|---|---|---|
| % | n* | % | n | % | n | |||
| Gender | Male | 48.1 | 313 | 85.6 | 219 | 14.4 | 22 | 0.12, 0.73 |
| Female | 51.9 | 359 | 84.8 | 251 | 15.2 | 28 | ||
| Race/ethnicity | Black African | 84.7 | 562 | 83.3 | 397 | 16.7 | 42 | 0.01, 0.93 |
| Non-Black African | 15.3 | 110 | 95.0 | 73 | 5.0 | 8 | ||
| Child grant | No | 44.5 | 256 | 88.2 | 180 | 11.8 | 17 | 0.27, 0.61 |
| Yes | 55.5 | 412 | 82.8 | 288 | 17.3 | 32 | ||
| Number of siblings born after Wave 1 |
0 | 92.5 | 631 | 88.0 | 445 | 12.0 | 43 | 13.5, <0.01 |
| 1 | 5.1 | 38 | 65.4 | 24 | 34.6 | 5 | ||
| 2 | 2.4 | 3 | 33.3 | 1 | 66.7 | 2 | ||
% based on post-stratification weight from Wave 2
Tabulation of observed value and p value of χ2 based on available data (* therefore comparisons of n values across columns are cautioned)
Overall, 36.6 % of female study participants had depressive symptoms with scores of CES-D ≥ 10 (Wave 1). Higher depression status (Table 2) was significantly related to age (χ2 = 10.2, p = 0.04), education (χ2 = 6.4, p = 0.04), race/ethnicity (χ2 = 5.9, p = 0.02), blood pressure/diabetes (χ2 = 4.5, p = 0.03), and perceived health status (χ2 = 12.6, p = 0.01), but not significantly related to other covariates such as cigarette smoking, employment status and BMI.
Table 2.
Demographic of non-pregnant women at Wave 1
| Overall |
CES-D (<10) |
CESD (≥10) |
χ2, p | ||||
|---|---|---|---|---|---|---|---|
| % | n* | % | n | % | n | ||
| Age group | |||||||
| 15–19 | 21.2 | 173 | 64.2 | 116 | 35.8 | 49 | 10.2, 0.04 |
| 20–24 | 26.0 | 179 | 72.5 | 119 | 27.5 | 49 | |
| 25–29 | 25.0 | 123 | 59.7 | 77 | 40.3 | 42 | |
| 30–34 | 19.5 | 103 | 54.4 | 49 | 45.6 | 43 | |
| 35+ | 8.4 | 72 | 64.7 | 44 | 35.3 | 26 | |
| Education | |||||||
| Less than HS | 1.9 | 18 | 42.4 | 7 | 57.6 | 11 | 6.4, 0.04 |
| Completes HS | 69.2 | 471 | 64.0 | 307 | 36.0 | 148 | |
| Beyond HS | 29.0 | 160 | 63.3 | 92 | 36.7 | 50 | |
| Race/ethnicity | |||||||
| Black African | 88.9 | 544 | 61.6 | 333 | 38.4 | 187 | 5.9, 0.02 |
| Non-Black African | 11.1 | 107 | 78.1 | 73 | 21.9 | 22 | |
| Marital status | |||||||
| Married | 21.0 | 123 | 57.8 | 66 | 42.2 | 49 | 5.7, 0.06 |
| Living with partner/separated | 13.6 | 73 | 58.0 | 45 | 42.0 | 27 | |
| Never married | 65.4 | 454 | 66.4 | 294 | 33.6 | 133 | |
| Employment statusa | |||||||
| Not economically active | 38.0 | 256 | 64.1 | 168 | 35.9 | 88 | 3.6, 0.30 |
| Unemployed—discouraged | 8.2 | 66 | 76.4 | 46 | 23.6 | 20 | |
| Unemployed—strict | 24.6 | 128 | 57.2 | 77 | 42.8 | 51 | |
| Employed | 29.1 | 158 | 65.0 | 111 | 35.0 | 47 | |
| Overall perceived health status | |||||||
| Excellent | 37.9 | 233 | 71.1 | 170 | 28.9 | 63 | 12.6, 0.01 |
| Very good | 25.0 | 171 | 58.5 | 104 | 41.5 | 67 | |
| Good | 28.4 | 154 | 60.7 | 103 | 39.3 | 51 | |
| Fair | 6.9 | 40 | 57.4 | 20 | 42.6 | 20 | |
| Poor | 1.7 | 13 | 61.8 | 7 | 38.2 | 6 | |
| Smoking | |||||||
| Not smoking | 92.9 | 562 | 63.7 | 367 | 36.3 | 195 | 1.5, 0.22 |
| Currently smoking | 7.1 | 53 | 59.7 | 39 | 40.3 | 14 | |
| High blood pressure/diabetes | |||||||
| No | 95.8 | 584 | 63.2 | 391 | 36.9 | 193 | 4.5, 0.03 |
| Yes | 4.3 | 31 | 68.5 | 15 | 31.5 | 16 | |
| BMI | |||||||
| Underweight | 4.3 | 39 | 68.5 | 28 | 31.5 | 11 | 5.4, 0.14 |
| Normal | 43.9 | 233 | 55.1 | 147 | 44.9 | 86 | |
| Overweight | 26.2 | 129 | 61.8 | 74 | 38.2 | 55 | |
| Obese | 25.7 | 135 | 71.6 | 94 | 28.4 | 41 | |
% based on post-stratification weight from Wave 1. Tabulation of observed value and p value of Chi-square based on available data (* therefore comparisons of n values across columns are cautioned)
Definitions and categorization of employment is provided by Statistics South Africa [30]
Relationship Between Depressive Symptoms Before Pregnancy and Low Birth Weight
Among children who were LBW, 43.1 % had mothers with significant depressive symptoms, compared to 31.4 % among children with normal birth weight. The results of the unadjusted logistic regression model indicate that depressive symptoms prior to pregnancy was not significantly associated with child LBW (OR 1.84, 95 % CI 0.80–4.30). However, the adjusted logistic regression model (Table 3) indicated that depressive symptoms prior to pregnancy was associated with child LBW (adjusted OR 2.84, 95 % CI 1.08–7.46). The other significant covariate in the model was the presence of siblings born after Wave 1 (adjusted OR 4.05, 95 % CI 1.21–13.5). Controlling for the potential role of post-natal depression on the outcome did not alter the significance of the above adjusted regression result.
Table 3.
Association between depression and low birth weight using logistics regression
| Adjusted OR | SE | t | p | 95 % CI | ||
|---|---|---|---|---|---|---|
| Depression | 2.84 | 1.40 | 2.13 | 0.03 | 1.08 | 7.46 |
| Race: [Black African] | ||||||
| Non-Black African | 2.38 | 7.50 | 0.27 | 0.78 | <0.01 | 1209.73 |
| Education: [moderate] | ||||||
| Low | 0.51 | 0.89 | −0.38 | 0.70 | 0.02 | 15.77 |
| High | 1.74 | 0.91 | 1.05 | 0.29 | 0.62 | 4.87 |
| Age groups: [15–19] | ||||||
| 20–24 | 0.46 | 0.36 | −1.00 | 0.32 | 0.10 | 2.11 |
| 25–29 | 1.86 | 1.38 | 0.84 | 0.40 | 0.44 | 7.96 |
| 30–34 | 0.74 | 0.62 | −0.36 | 0.72 | 0.14 | 3.81 |
| 35+ | 2.47 | 2.20 | 1.02 | 0.31 | 0.43 | 14.20 |
| Perceived health status: [good] | ||||||
| Excellent/very good | 1.38 | 1.11 | 0.40 | 0.69 | 0.28 | 6.69 |
| Fair/poor | 0.90 | 0.48 | −0.19 | 0.85 | 0.32 | 2.55 |
| Marital status: [never married] | ||||||
| Married | 0.37 | 0.29 | −1.27 | 0.20 | 0.08 | 1.71 |
| Living with partner/separated | 1.91 | 1.21 | 1.02 | 0.31 | 0.55 | 6.61 |
| Settlement typea: [rural] | ||||||
| Tribal authority | 0.83 | 0.75 | −0.21 | 0.83 | 0.14 | 4.92 |
| Urban formal | 2.19 | 1.99 | 0.86 | 0.39 | 0.37 | 13.06 |
| Urban informal | 1.94 | 2.09 | 0.61 | 0.54 | 0.23 | 16.01 |
| Employment: [not economically active] | ||||||
| Unemployed—discouraged | 0.92 | 0.88 | −0.09 | 0.93 | 0.14 | 6.05 |
| Unemployed—strict | 0.26 | 0.19 | −1.83 | 0.07 | 0.06 | 1.11 |
| Employed | 1.50 | 0.90 | 0.68 | 0.50 | 0.46 | 4.89 |
| Smoker: [no] | 2.53 | 2.39 | 0.98 | 0.33 | 0.40 | 16.16 |
| High blood pressure/diabetes: [no] | 0.62 | 0.65 | −0.46 | 0.65 | 0.08 | 4.81 |
| BMI (underweight) | ||||||
| Normal | 4.82 | 7.81 | 0.97 | 0.33 | 0.20 | 117.91 |
| Overweight | 2.67 | 4.41 | 0.59 | 0.55 | 0.10 | 69.44 |
| Obese | 2.73 | 4.46 | 0.62 | 0.54 | 0.11 | 67.79 |
| Child gender: [male] | 1.11 | 0.52 | 0.23 | 0.82 | 0.45 | 2.77 |
| Child race: [Black African] | 0.19 | 0.62 | −0.51 | 0.61 | <0.01 | 110.42 |
| Recipient of child support grant: [no] | 1.54 | 0.73 | 0.91 | 0.36 | 0.61 | 3.93 |
| Number of siblings born between Waves 1 and 2 | 4.05 | 2.49 | 2.27 | 0.02 | 1.21 | 13.55 |
100 multiple imputations. Above regression adjusted for post stratification weight from Wave 2. Reference category in bracket
Definitions and categorization of settlement type is provided by Statistics South Africa [30]
Discussion
Our finding suggests that women’s depressive symptoms prior to pregnancy may be a contributing risk factor for low birth weight in their newborns. The odds of LBW were higher among female study participants with significantly higher levels of depressive symptoms, highlighting the need to improve the mental health of women even before pregnancy begins. Using longitudinal datasets from the SA-NIDS, our study contributes to the identification of risk factors for LBW infants and their mothers, including the possible consequences of untreated depression before pregnancy. Although our finding is based on significant risk depression symptomatology rather than a clinical diagnosis, this study further highlights the need to promote access to care in order to address one of the leading public health challenges in South Africa.
Our main finding leads us to consider the possible mechanisms by which exposure to psychological distress (i.e. depression) before pregnancy directly and indirectly affects infant LBW. Perhaps the most plausible explanation is that depression prior to pregnancy (e.g. a history of depression) is a major risk factor for antenatal depression, which in turn is a known predictor of infant LBW [14]. In addition, depression in itself can be a barrier to seeking medical treatment during pregnancy [23] due to factors such as a lack of trust in mental health care providers, limited access to facilities, and stigma related to depression [24–26]. Based on a conceptual framework by Kramer et al. [27], another plausible explanation is that social disparities (e.g., low socioeconomic status) lead to a greater susceptibility for developing mental health problems and other unhealthy behaviors, like smoking—all of which contribute to the risk of infant LBW.
While the major strengths of this study include the use of nationally representative longitudinal household survey data with good response rates, there are several limitations. First, it was based on self-reported depressive symptoms of participants and did not have information related to a formal diagnosis of depression. Secondly, gestational age, which can confound the relationship between preconception depression and infant low birth weight, was not available. Lastly, measures of alcohol/drug or anti-depressant medication use were not available in the study; future studies should include substance use as part of investigating the relationship between depression and LBW outcomes.
Although depression during pregnancy is often understood to be a significant risk factor for low infant birth weight [12], the selection of intervention type for depression, including the use of antidepressants during pregnancy, remains controversial. It has been 30 years since the U.S. Institute of Medicine’s interdisciplinary committee discussed the challenges in preventing LBW [28]. Despite the subsequent expansion of prenatal care service in the U.S., LBW rates have not declined. This lack of improvement is partly attributed to an ineffective treatment model; thus, a review of the program structure of prenatal care is warranted, including the timing of services [29].
Further studies are needed to identify evidence-based, culturally-appropriate interventions for developing countries such as South Africa. Although our study limitations prevent firm conclusions regarding the causal relationship between depressive symptoms prior to pregnancy and infant low birth weight, our findings contribute to a better understanding of the timing of risk associated with depression in women and infant outcome. While reaffirming the need for an integrative health approach for women in community-based settings to better address multiple high-risk factors [29], our study highlights the general importance of detecting and treating depression in women of child-bearing age to reduce adverse pregnancy outcomes.
Acknowledgments
Dr. Tomita was supported by NIH Research Training Grant (R25 TW009337) funded by the Fogarty International Center and the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The data was accessed through Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2008 and 2010–2011, Wave 1 and 2 (dataset). Version 4.1 for Wave 1 and version 1.0 for Wave 2. Cape Town: Southern Africa Labour and Development Research Unit (producer), 2013. Cape Town: Data First (distributor), 2013.
Footnotes
Conflict of interest All authors have approved the manuscript as submitted and none of the authors have a conflict of interest to declare.
Contributor Information
Andrew Tomita, Department of Psychiatry, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Private Bag X7, Congella, Durban 4013, South Africa; Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA.
Charlotte A. Labys, Department of Psychiatry, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Private Bag X7, Congella, Durban 4013, South Africa
Jonathan K. Burns, Department of Psychiatry, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Private Bag X7, Congella, Durban 4013, South Africa
References
- 1.Goldenberg RL, Culhane JF. Low birth weight in the United States. American Journal of Clinical Nutrition. 2007;85(2):584S–590S. doi: 10.1093/ajcn/85.2.584S. [DOI] [PubMed] [Google Scholar]
- 2.Vigod SN, Villegas L, Dennis CL, et al. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: A systematic review. BJOG. 2010;117(5):540–550. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- 3.Chopra M, Daviaud E, Pattinson R, et al. Saving the lives of South Africa’s mothers, babies, and children: Can the health system deliver? Lancet. 2009;374(9692):835–846. doi: 10.1016/S0140-6736(09)61123-5. [DOI] [PubMed] [Google Scholar]
- 4.Organisation for Economic Cooperation and Development Infant health: Low birth weight. 2011 http://dx.doi.org/10.1787/health_glance-2011-11-en.
- 5.Zimmer-Gembeck MJ, Helfand M. Low birthweight in a public prenatal care program: Behavioral and psychosocial risk factors and psychosocial intervention. Social Science and Medicine. 1996;43(2):187–197. doi: 10.1016/0277-9536(95)00361-4. [DOI] [PubMed] [Google Scholar]
- 6.Teitler JO, Reichman NE, Nepomnyaschy L, et al. A cross-national comparison of racial and ethnic disparities in low birth weight in the United States and England. Pediatrics. 2007;120(5):e1182–e1189. [Google Scholar]
- 7.Khoshnood B, Wall S, Lee KS. Risk of low birth weight associated with advanced maternal age among four ethnic groups in the United States. Maternal Child Health Journal. 2005;9(1):3–9. doi: 10.1007/s10995-005-2446-4. [DOI] [PubMed] [Google Scholar]
- 8.Blondel B, Kogan MD, Alexander GR, et al. The impact of the increasing number of multiple births on the rates of preterm birth and low birthweight: An international study. American Journal of Public Health. 2002;92(8):1323–1330. doi: 10.2105/ajph.92.8.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odell CD, Kotelchuck M, Chetty VK, et al. Maternal hypertension as a risk factor for low birth weight infants: Comparison of Haitian and African-American women. Maternal Child Health Journal. 2006;10(1):39–46. doi: 10.1007/s10995-005-0026-2. [DOI] [PubMed] [Google Scholar]
- 10.Abu-Ghanem S, Sheiner E, Sherf M, et al. Lack of prenatal care in a traditional community: Trends and perinatal outcomes. Archives of Gynecology and Obstetrics. 2012;285(5):1237–1242. doi: 10.1007/s00404-011-2153-x. [DOI] [PubMed] [Google Scholar]
- 11.Manikkam L, Burns JK. Antenatal depression and its risk factors: An urban prevalence study in KwaZulu-Natal. South African Medical Journal. 2012;102(12):940–944. doi: 10.7196/samj.6009. [DOI] [PubMed] [Google Scholar]
- 12.Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brennan PA, Hammen C, Andersen MJ, et al. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36(6):759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- 14.Marcus SM, Flynn HA, Blow FC, et al. Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health. 2003;12(4):373–380. doi: 10.1089/154099903765448880. [DOI] [PubMed] [Google Scholar]
- 15.Dietz PM, Williams SB, Callaghan WM, et al. Clinically identified maternal depression before, during, and after pregnancies ending in live births. American Journal of Psychiatry. 2007;164(10):1515–1520. doi: 10.1176/appi.ajp.2007.06111893. [DOI] [PubMed] [Google Scholar]
- 16.Petersen I, Lund C. Mental health service delivery in South Africa from 2000 to 2010: One step forward, one step back. South African Medical Journal. 2011;101(10):751–757. [PubMed] [Google Scholar]
- 17.Class QA, Khashan AS, Lichtenstein P, et al. Maternal stress and infant mortality: The importance of the preconception period. Psychological Science. 2013;24(7):1309–1316. doi: 10.1177/0956797612468010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Witt WP, Wisk LE, Cheng ER, et al. Preconception mental health predicts pregnancy complications and adverse birth outcomes: A national population-based study. Maternal and Child Health Journal. 2012;16(7):1525–1541. doi: 10.1007/s10995-011-0916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radloff LS. The CES-D scale. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 20.Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, et al. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 21.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 22.Rao JNK, Scott AJ. On Chi-squared tests for multiway contingency tables with cell proportions estimated from survey data. Annals of Statistics. 1984;12(1):46–60. [Google Scholar]
- 23.Joyce K, Diffenbacher G, Greene J, Sorokin Y. Internal and external barriers to obtaining prenatal care. Social Work in Health Care. 1984;9(2):89–96. doi: 10.1300/j010v09n02_09. [DOI] [PubMed] [Google Scholar]
- 24.Kopelman RC, Moel J, Mertens C, et al. Barriers to care for antenatal depression. Psychiatric Services. 2008;59(4):429–432. doi: 10.1176/appi.ps.59.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myer L, Harrison A. Why do women seek antenatal care late? Perspectives from rural South Africa. Journal of Midwifery & Women’s Health. 2003;48(4):268–272. doi: 10.1016/s1526-9523(02)00421-x. [DOI] [PubMed] [Google Scholar]
- 26.Jesse DE, Dolbier CL, Blanchard A. Barriers to seeking help and treatment suggestions for prenatal depressive symptoms: Focus groups with rural low-income women. Issues in Mental Health Nursing. 2008;29(1):3–19. doi: 10.1080/01612840701748664. [DOI] [PubMed] [Google Scholar]
- 27.Kramer MS, Séguin L, Lydon J, et al. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatric and Perinatal Epidemiology. 2000;14(3):194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine Preventing low birthweight. 1985 http://www.ncbi.nlm.nih.gov/books/NBK214468/pdf/TOC.pdf.
- 29.Krans EE, Davis MM. Preventing low birthweight: 25 years, prenatal risk, and the failure to reinvent prenatal care. American Journal of Obstetrics and Gynecology. 2012;206(5):398–403. doi: 10.1016/j.ajog.2011.06.082. [DOI] [PubMed] [Google Scholar]
- 30.Statistics South Africa . Concept and definitions. Statistics South Africa; Pretoria: 2004. [Google Scholar]