Abstract
Pancreatic ductal adenocarcinoma (PDAC) is a highly malignant disease, but the genetic basis of PDAC is still unclear. In this study, Nectin-2 and DDX3 expression in 106 PDAC, 35 peritumoral tissues, 55 benign pancreatic lesions, and 13 normal pancreatic tissues were measured by immunohistochemical methods. Results showed that the percentage of positive Nectin-2 and DDX3 expression was significantly higher in PDAC tumors than in peritumoral tissues, benign pancreatic tissues, and normal pancreatic tissues (P < 0.01). The percentage of cases with positive Nectin-2 and DDX3 expression was significantly lower in PDAC patients without lymph node metastasis and invasion and having TNM stage I/II disease than in patients with lymph node metastasis, invasion, and TNM stage III/IV disease (P < 0.05 or P < 0.01). Positive DDX3 expression is associated with poor differentiation of PDAC. Kaplan-Meier survival analysis showed that positive Nectin-2 and DDX3 expression were significantly associated with survival in PDAC patients (P < 0.001). Cox multivariate analysis revealed that positive Nectin-2 and DDX3 expression were independent poor prognosis factors in PDAC patients. In conclusion, positive Nectin-2 and DDX3 expression are associated with the progression and poor prognosis in PDAC patients.
1. Introduction
Pancreatic ductal adenocarcinoma (PDAC) has one of the worst prognoses among cancers and is the fourth leading cause of cancer-related deaths worldwide [1]. In 2014, there were 39,590 pancreatic cancer deaths in the United States, and the annual deaths from PDAC continue to increase [2]. Despite the progress made in diagnostic technology, the survival statistics demonstrated that only 8% of new diagnoses are early-stage disease with resectable tumor, while most pancreatic cancers are diagnosed at advanced stages with metastasis [3]. A study from the National Cancer Database of USA revealed that only 52% of patients with early-stage disease underwent surgical resection [4]. Among these patients with local disease, the 5-year postsurgical survival rate was only 23% [2]. The survival rate in patients with unresectable tumors is lower than 1% [5]. Current radiotherapy, chemotherapy, and other therapeutic strategies exhibit limited impact on the prognosis of PDAC. This might be because of a lack of thorough understanding of the molecular and genetic bases of PDAC.
Poliovirus receptor-related 2 protein (PRR2), also called Nectin-2 or CD112, is a novel cell adhesion molecule of the immunoglobulin superfamily (IgSF) [6, 7]. Besides its functions as an adhesion molecule, Nectin-2 has other important biological functions, such as being a receptor of some viruses and binding to the surface CD226 receptor of NK and cytotoxic T lymphocytes (CTL) cells to activate NK cells and CTL killing activity. Nectin-2 is expressed on the surface of tumor cells, and its recognition by NK cells plays a role in antitumor immunity [8, 9]. Recently, Nectin-2 expression was found to be closely related to the tumorigenesis and prognosis of neuroblastoma [10], multiple myeloma [11], acute myeloid leukemia [12], and Juventus sarcoma [13]. Also, Nectin-2 is highly expressed in some epithelial cancers, such as breast cancer [14, 15], ovarian cancer [15], gallbladder cancer [16], and cervical cancer [17], and higher Nectin-2 expression was found in more malignant cancers with rapid progression and poor prognosis. The expression of Nectin-2 in PDAC has not been reported.
Human DDX3 is an ATP-dependent RNA helicase of the DEAD-box family and is widely expressed in a variety of tissues [18, 19]. DDX3 plays an important role in the regulation of gene expression, such as transcription, splicing, mRNA transport, and translation [20]. DDX3 is also involved in cell cycle regulation and apoptosis [21]. DDX3 functions as an ATP-dependent enzyme to promote p21WAF1/CIPI promoter activity and subsequent p21WAF1/CIPI gene expression [22], and DDX3 further inhibits tumor growth by serving as a tumor suppressor gene [23]. In recent years, DDX3 has been demonstrated to be associated with the occurrence of breast cancer [24], non-small cell lung cancer [25, 26], oral squamous cell carcinoma [27], and gallbladder cancer [16]. The expression and biological significance of DDX3 have not been reported in PDAC.
In this study, Nectin-2 and DDX3 expression in 106 PDAC, 35 peritumoral tissues, 55 benign pancreatic lesions, and 13 normal pancreatic tissues were measured by immunohistochemistry. The clinicopathological significance of Nectin-2 and DDX3 expression and their associations with the prognosis of PDAC were analyzed.
2. Materials and Methods
2.1. Clinical Data
106 PDAC tumors, 35 peritumoral tissues, 55 pancreatic tissues with benign lesions, and 13 normal pancreatic tissues were collected from January 2000 to December 2011. PDAC was diagnosed based on the recent US Armed Forces Institute of Pathology Fascicle on pancreatic neoplasms [28]. PDAC tumor tissues were collected before radiotherapy or chemotherapy. The peritumoral tissues were collected ≥2 cm from the edge of PDAC tumors. Forty-five PDAC cases were female, while 61 were male with an average age of 54.50 ± 11.53 years. Thirty-eight PDAC (35.9%) tumors were well differentiated, 35 (33.0%) were moderately differentiated, and 33 (31.1%) were poorly differentiated. Thirteen PDAC tumors had a maximum tumor size <3 cm, 68 had a maximum tumor size of 3 to 5 cm, and 25 had a maximum tumor size >5 cm. Twenty-nine cases had regional lymph node metastasis, and 64 had invasion to surrounding tissues and organs of the pancreas. Eleven, forty-two, thirty-seven, and sixteen patients had TNM clinical stages I, II, III, and IV disease, respectively. The survival information of 106 PDAC cases was collected by letters or telephone calls. The PDAC cases were followed up for 2 years. Among the 106 cases with PDAC, 77 patients survived shorter than 1 year and 29 patients survived longer than 1 year with a mean survival time of 9.44 ± 0.69 months. Twelve, ten, eight, and five peritumoral tissues were normal, mild dysplasia, moderate dysplasia, and severe dysplasia. The 55 benign pancreatic specimens were collected from 29 males and 26 females with 13 cases ≤45 years old and 42 cases >45 years old. Twenty, twenty, and fifteen cases with benign lesions had chronic pancreatitis, adenoma, and intraepithelial neoplasia, respectively. Ten, six, and four of the twenty patients with chronic pancreatitis had mild, moderate, and severe pancreatitis, respectively. Among the 20 adenomas, 15 were serous adenomas and 5 were mucinous adenomas, respectively. Four, three, and two adenomas had mild, moderate, and severe dysplasia, respectively. Among the 15 intraepithelial neoplasias, 6, 5, and 4 were grade I, grade II, and grade III intraepithelial neoplasia. Thirteen normal pancreatic tissues were collected from surgery of pancreatic adenoma. All tissues were treated with 4% formaldehyde and then paraffin-embedded.
2.2. Immunohistochemistry
The rabbit anti-human Nectin-2 and DDX3 antibodies were purchased from Abgent Company (California, USA). Nectin-2 and DDX3 were immunohistologically stained using EnVision detection kit (Dako Laboratories, California, USA). Briefly, 4 µm sections were cut from paraffin-embedded tissues. After sections were deparaffinized and incubated with 3% H2O2, sections were incubated with Nectin-2 or DDX3 antibody for 1 hr at room temperature (RT). After washing with PBS, solution A was applied to the sections for 30 min at RT, followed by incubation with color development solution and hematoxylin counter staining. 400 cells from 10 random fields were counted. Cases were positive if ≥25% of cells were positive and negative if <25% of cells were positive [29]. Positive control biopsies were provided with the EnVision detection kit. 5% fetal bovine serum was used as negative control.
2.3. Statistical Analysis
Data were analyzed using SPSS15.0 statistical package. The relationships between Nectin-2 and DDX3 expression and histological or clinical factors were analyzed by χ 2 test or Fisher's exact test. Univariate survival analysis was conducted with Kaplan-Meier method (log-rank test). Multivariate analysis was performed with Cox proportional hazard model and the 95% confidence interval was calculated. P < 0.05 was considered statistically significant.
3. Results
3.1. Nectin-2 and DDX3 Expression in Normal, Benign, and Malignant Pancreatic Tissues
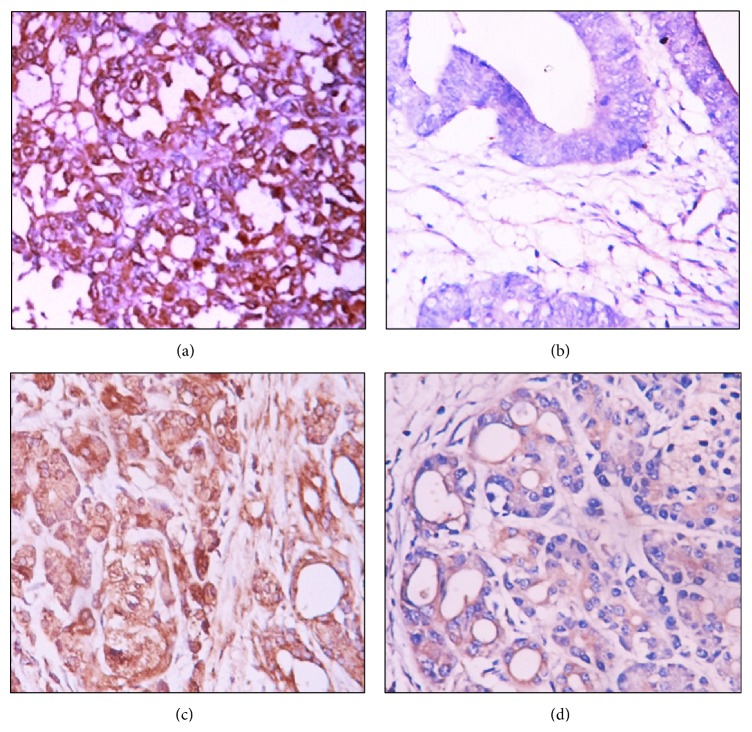
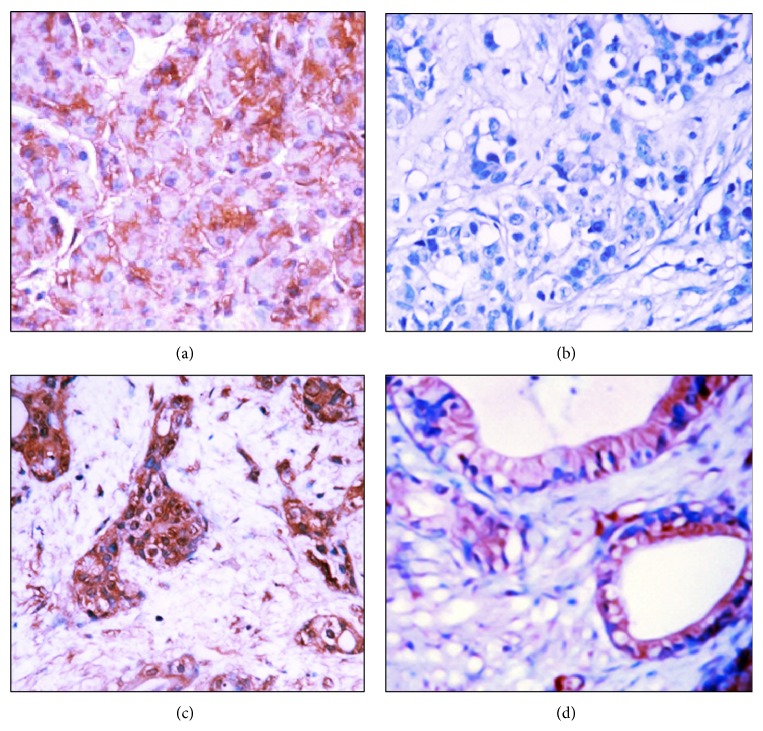
Positive Nectin-2 (Figure 1) and DDX3 (Figure 2) expression were mainly located in the cytoplasm. Among the 106 cases with PDAC, positive Nectin-2 and DDX3 expression were observed in 58 and 55 cases, respectively. Among the 35 peritumoral tissues, positive Nectin-2 and DDX3 expression were observed in 9 and 8 tissues, respectively. Among the 55 cases with benign pancreatic lesions, positive Nectin-2 and DDX3 expression were observed in 10 and 11 cases, respectively. Both Nectin-2 and DDX3 were negative in all 13 normal pancreatic tissues. Peritumoral tissues and benign lesions with positive Nectin-2 and DDX3 expression exhibited dysplasia or grade II or III intraepithelial neoplasia (Table 1). The percentage of positive Nectin-2 and DDX3 expression was significantly higher in PDAC tumors than in peritumoral tissues, benign lesions, and normal pancreatic tissues (P < 0.01 or P < 0.001). Among the 55 cases with benign pancreatic lesions, the percentages of positive Nectin-2 expression in chronic pancreatitis, adenomas, and intraepithelial neoplasia were 15.0%, 20.0%, and 20.0%, respectively. The percentages of positive DDX3 expression in chronic pancreatitis, adenoma, and intraepithelial neoplasia were 10.0%, 30.0%, and 20.0%, respectively. No significant differences in the percentage of positive Nectin-2 and DDX3 expression were observed between three types of benign lesions (P > 0.05).
Figure 1.
Nectin-2 expression in malignant and benign tissues. (a) Nectin-2 positive expression in poorly differentiated PDAC. (b) Nectin-2 negative expression in well differentiated PDAC. (c) Nectin-2 positive expression in peritumoral tissue. (d) Nectin-2 positive expression in adenoma. Magnification ×200. Cells with brown granules in the cytoplasm were identified as Nectin-2 positive.
Figure 2.
DDX3 expression in malignant and benign tissues. (a) DDX3 positive expression in poorly differentiated PDAC. (b) DDX3 negative expression in moderately differentiated PDAC. (c) DDX3 positive expression in intraepithelial neoplasia. (d) DDX3 positive expression in chronic pancreatitis tissue. Magnification ×200. Cells with brown granules in the cytoplasm were identified as DDX3 positive.
Table 1.
Comparison of Nectin-2 and DDX3 expression in normal, benign, and malignant pancreatic tissues.
| Tissue types | Case number | Nectin-2 positive (%) | DDX3 positive (%) |
|---|---|---|---|
| Pancreatic ductal adenocarcinoma | 106 | 58 (54.7) | 55 (51.9) |
| Peritumoral tissues | 35 | 9 (25.7)∗∗ | 8 (22.9)∗∗ |
| Benign tissues | 55 | 10 (18.2)∗∗ | 11 (20.0)∗∗ |
| Normal pancreatic tissues | 13 | 0 (0.0)∗∗ | 0 (0.0)∗∗ |
Compared to pancreatic ductal adenocarcinoma, ∗∗ P < 0.01.
3.2. Associations between Nectin-2 and DDX3 Expression and Clinicopathological Features of PDAC
The percentage of positive Nectin-2 and DDX3 expression was significantly higher in PDAC cases with poor differentiation, invasion to surrounding tissues and organs, lymph node metastasis, and TNM stages III and IV disease than in cases with well differentiated tumor, no invasion, no lymph node metastasis, and TNM stages I and II disease (P < 0.05 or P < 0.01) (Table 2). No significant differences were observed in patients with different age, sex, and tumor size (P > 0.05). Among the 58 cases with positive Nectin-2 expression, positive DDX3 expression was observed in 45 cases. Of the 45 cases with negative Nectin-2 expression, 38 cases were DDX3 negative, suggesting positive correlation between Nectin-2 and DDX3 expression in cases with PDAC (P = 0.000).
Table 2.
Correlations of Nectin-2 and DDX3 protein expression with the clinicopathological characteristics of pancreatic ductal adenocarcinoma.
| CPC | Case number | Nectin-2 | DDX3 | ||||
|---|---|---|---|---|---|---|---|
| Positive number (%) | χ 2 | P value | Positive number (%) | χ 2 | P value | ||
| Age (year) | |||||||
| ≤45 | 22 | 12 (54.5) | 0.000 | 0.986 | 14 (63.6) | 1.535 | 0.215 |
| >45 | 84 | 46 (54.8) | 41 (48.8) | ||||
| Sex | |||||||
| Male | 61 | 33 (54.1) | 0.022 | 0.882 | 31 (50.8) | 0.066 | 0.798 |
| Female | 45 | 25 (55.6) | 24 (53.3) | ||||
| Differentiation | |||||||
| Well | 38 | 16 (42.1) | 4.424 | 0.109 | 14 (36.8) | 9.341 | 0.009 |
| Moderately | 35 | 20 (57.1) | 17 (48.6) | ||||
| Poorly | 33 | 22 (66.7) | 24 (72.7) | ||||
| Tumor size | |||||||
| ≤3 cm | 13 | 5 (38.5) | 2.258 | 0.323 | 6 (46.2) | 0.345 | 0.841 |
| 3–5 cm | 68 | 37 (54.5) | 35 (51.5) | ||||
| >5 cm | 25 | 16 (64.0) | 14 (56.0) | ||||
| Lymph node metastasis | |||||||
| No | 77 | 34 (44.2) | 12.670 | 0.000 | 35 (45.5) | 4.664 | 0.031 |
| Yes | 29 | 24 (82.8) | 20 (69.0) | ||||
| Invasion | |||||||
| No | 42 | 14 (33.3) | 12.838 | 0.000 | 13 (31.0) | 12.212 | 0.000 |
| Yes | 64 | 44 (68.8) | 42 (65.6) | ||||
| TNM stage | |||||||
| T1 | 11 | 4 (36.4) | 13.190 | 0.004 | 3 (27.3) | 14.848 | 0.002 |
| T2 | 42 | 16 (38.1) | 16 (38.1) | ||||
| T3 | 37 | 25 (67.6) | 22 (59.5) | ||||
| T4 | 16 | 13 (81.3) | 14 (87.5) | ||||
CPC: clinical and pathological characteristics.
3.3. The Relationship between Clinicopathological Characteristics, Nectin-2 and DDX3 Expression, and Survival of PDAC Patients
Kaplan-Meier survival analysis showed that poor differentiation, larger maximum tumor size, high TNM stage, lymph node metastasis and invasion, and positive Nectin-2 and DDX3 expression are significantly correlated with the shorter survival in PDAC cases (P < 0.05, P < 0.01, or P < 0.001). Patients with positive Nectin-2 and DDX3 expression survived significantly shorter than patients with negative Nectin-2 and DDX3 expression (P = 0.000) (Table 3, Figure 3). Cox multivariate analysis showed that differentiation, tumor size, TNM stage, lymph node metastasis, and invasion were independent prognostic factors and negatively correlated with survival. Positive Nectin-2 (Table 4) and DDX3 (Table 5) expression negatively correlated with survival, positively correlated with mortality, and were risk factors in PDAC. Both Nectin-2 and DDX3 are independent prognostic factors (Tables 4 and 5).
Table 3.
Correlations of clinicopathological characteristics and Nectin-2 and DDX3 expression with mean survival in patients with pancreatic ductal adenocarcinoma.
| Groups | Case number (n) | Mean survival (median) month |
χ 2 | P value |
|---|---|---|---|---|
| Sex | ||||
| Male | 61 | 9.98 (13) | 1.656 | 0.198 |
| Female | 45 | 8.61 (11.5) | ||
| Age (year) | ||||
| ≤45 | 22 | 8.18 (11) | 2.144 | 0.143 |
| >45 | 84 | 9.73 (13) | ||
| Differentiation | ||||
| Well | 38 | 11.27 (13.5) | 17.786 | 0.000 |
| Moderately | 35 | 9.74 (12) | ||
| Poorly | 33 | 6.86 (8) | ||
| Tumor size | ||||
| <3 cm | 13 | 13.46 (13) | 7.504 | 0.023 |
| 3~5 cm | 68 | 9.34 (12) | ||
| >5 cm | 25 | 7.40 (13.5) | ||
| TNM stage | ||||
| I | 11 | 16.46 (17.5) | 80.807 | 0.000 |
| II | 42 | 11.37 (12.5) | ||
| III | 37 | 7.14 (9.5) | ||
| IV | 16 | 4.56 (5) | ||
| Lymph node metastasis | ||||
| No | 77 | 10.64 (13) | 27.120 | 0.000 |
| Yes | 29 | 6.35 (7) | ||
| Invasion | ||||
| No | 42 | 13.33 (14.5) | 46.949 | 0.000 |
| Yes | 54 | 6.83 (9.5) | ||
| Nectin-2 | ||||
| − | 48 | 12.63 (13.5) | 44.074 | 0.000 |
| + | 56 | 6.73 (8.5) | ||
| DDX3 | ||||
| − | 55 | 12.05 (14.5) | 28.608 | 0.000 |
| + | 51 | 6.98 (10) |
Figure 3.
Nectin-2 and DDX3 expression and survival in patients with PDAC. (a) Kaplan-Meier plots of overall survival in patients with PDAC and with positive and negative Nectin-2 expression. (b) Kaplan-Meier plots of overall survival in patients with PDAC and with positive and negative DDX3 expression.
Table 4.
Multivariate Cox regression analysis of survival rate in patients with pancreatic ductal adenocarcinoma.
| Group | Factors | B | SE | Wald | P | RR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Differentiation | Well/moderately/poorly | 1.287 | 0.466 | 7.63 | 0.006 | 3.62 | 1.45 | 9.03 |
| Tumor size | <3 cm/3–5 cm/>5 cm | 1.589 | 0.627 | 6.42 | 0.011 | 4.90 | 1.43 | 16.04 |
| Lymph node metastasis | no/yes | 2.574 | 0.782 | 10.83 | 0.001 | 13.12 | 2.83 | 60.75 |
| Invasion | no/yes | 2.693 | 0.801 | 11.30 | 0.001 | 14.78 | 3.07 | 71.02 |
| TNM stage | I/II/III/IV | 1.485 | 0.537 | 7.65 | 0.006 | 4.41 | 1.54 | 12.65 |
| Nectin-2 | −/+ | 3.016 | 0.865 | 12.16 | 0.000 | 20.41 | 3.75 | 111.21 |
CI: confidence interval.
Table 5.
Multivariate Cox regression analysis of survival rate in patients with pancreatic ductal adenocarcinoma.
| Group | Factors | B | SE | Wald | P | RR | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Differentiation | Well/moderately/poorly | 1.126 | 0.409 | 7.58 | 0.006 | 3.08 | 1.38 | 6.87 |
| Tumor size | <3 cm/3–5 cm/>5 cm | 1.633 | 0.661 | 6.10 | 0.013 | 5.12 | 1.40 | 18.70 |
| Lymph node metastasis | No/yes | 2.785 | 0.822 | 11.48 | 0.001 | 16.20 | 3.23 | 81.14 |
| Invasion | No/yes | 2.874 | 0.817 | 12.37 | 0.000 | 17.71 | 3.57 | 87.82 |
| TNM stage | I/II/III/IV | 1.762 | 0.628 | 7.87 | 0.005 | 5.82 | 1.70 | 19.9 |
| DDX3 | −/+ | 2.141 | 0.674 | 10.9 | 0.001 | 8.51 | 2.27 | 31.88 |
CI: confidence interval.
4. Discussion
The expression of Nectin-2 and DDX3 in PDAC has not been previously reported, although their expressions have been associated with the progression and prognosis of a variety of tumors. This study investigated Nectin-2 and DDX3 protein expression in PDAC tumors, peritumoral tissues, benign pancreatic lesions, and normal pancreatic tissues using immunohistochemistry. A significant increase in Nectin-2 and DDX3 expression in PDAC tumors was observed. Positive Nectin-2 and DDX3 expressions are associated with poor differentiation, invasion, metastasis, and poor prognosis of PDAC.
Nectin-2 is located at the connections between endothelial cells, and the interactions between these two subtypes transfer extracellular signaling into cells [30]. Takahashi et al. [31] study found that Nectin-2 plays important roles in cell adhesion, migration, and polarization [6]. These functions of Nectin-2 implicate its possible roles in tumor cell survival and proliferation. Indeed, a previous study using a polyclonal antibody specific to Nectin-2 showed that Nectin-2 is involved in the proliferation of ovarian cancer cells [32]. Moreover, recent studies have demonstrated that Nectin-2 is highly expressed in epithelial malignancies and correlates with high malignancy, fast progression, and/or poor prognosis of human breast cancer [14, 15], ovarian cancer [15], gallbladder cancer [16], and the invasive squamous carcinomas of the human uterine cervix [17]. However, the clinical significance of Nectin-2 has not yet been addressed in PDAC. This study first demonstrated that positive Nectin-2 expression significantly correlated with clinical progression, as indicated by large tumor size, lymph node metastasis, and tumor cell invasion. The observed association between Nectin-2 positive expression and the progression of PDAC may be associated with its functions in cell proliferation, migration, and signaling transduction. Moreover, positive Nectin-2 expression correlated with shorter survival. Cox multivariate analysis suggested that positive Nectin-2 expression is an independent prognostic factor associated with poor prognosis in PDAC patients.
Human DDX3 plays an important role in gene expression and the translation process. DDX3 is also involved in cell cycle regulation and cell apoptosis [33]. DDX3 promotes p21WAF1/CIP1 promoter activity and subsequent gene expression, which can inhibit tumor growth, making DDX3 a tumor suppressor gene [34]. However, reports on the roles of DDX3 in various cancers are controversial. For example, elevated DDX3 expression has been observed in tumor tissues of breast cancer [24], non-small cell lung cancer [25, 26], oral squamous cell carcinoma [27], and gallbladder cancer [16]. DDX3 is also found to be involved in carcinogenesis through enhancing cellular proliferation and maintaining genomic integrity [35]. A recent study found low/negative DDX3 expression in tumor cells of oral squamous cell carcinoma, which was significantly associated with aggressive clinical manifestations, and DDX3 is an independent survival predictor in nonsmoker patients with oral squamous cell carcinoma [27]. In contrast, high DDX3 expression is closely correlated with progression and poor prognosis of gallbladder cancer [16]. Therefore, the current findings suggest that the role of DDX3 in cancer is tumor type specific. In this study, DDX3 protein expression was significantly increased in PDAC tumors. This is the first study that reported DDX3 expression in PDAC. Moreover, positive DDX3 expression was significantly related to poor differentiation of the tumor and severe clinical manifestations. Positive DDX3 expression also correlated with shorter survival and poor prognosis in PDAC patients.
5. Conclusions
This study suggests that Nectin-2 and DDX3 are involved in the progression of PDAC, and positive Nectin-2 and DDX3 expression were associated with shorter survival and poor prognosis in patients with PDAC. Positive Nectin-2 and DDX3 expression could be diagnostic markers of PDAC.
Conflict of Interests
All authors declared no conflict of interests.
References
- 1.Jemal A., Siegel R., Ward E., Hao Y., Xu J., Thun M. J. Cancer statistics, 2009. CA: A Cancer Journal for Clinicians. 2009;59(4):225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R., Ma J., Zou Z., Jemal A. Cancer statistics, 2014. CA: Cancer Journal for Clinicians. 2014;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 3.Kuhlmann K. F. D., de Castro S. M. M., Wesseling J. G., et al. Surgical treatment of pancreatic adenocarcinoma: actual survival and prognostic factors in 343 patients. European Journal of Cancer. 2004;40(4):549–558. doi: 10.1016/j.ejca.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Winner M., Goff S. L., Chabot J. A. Neoadjuvant therapy for Non-metastatic Pancreatic Ductal Adenocarcinoma. Seminars in Oncology. 2015;42(1):86–97. doi: 10.1053/j.seminoncol.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Von Hoff D. D., Ervin T., Arena F. P., et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. The New England Journal of Medicine. 2013;369(18):1691–1703. doi: 10.1056/nejmoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takai Y., Irie K., Shimizu K., Sakisaka T., Ikeda W. Nectins and nectin-like molecules: roles in cell adhesion, migration, and polarization. Cancer Science. 2003;94(8):655–667. doi: 10.1111/j.1349-7006.2003.tb01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takai Y., Ikeda W., Ogita H., Rikitake Y. The immunoglobulin-like cell adhesion molecule nectin and its associated protein afadin. Annual Review of Cell and Developmental Biology. 2008;24:309–342. doi: 10.1146/annurev.cellbio.24.110707.175339. [DOI] [PubMed] [Google Scholar]
- 8.Castriconi R., Dondero A., Corrias M. V., et al. Natural killer cell-mediated killing of freshly isolated neuroblastoma cells: critical role of DNAX accessory molecule-1-poliovirus receptor interaction. Cancer Research. 2004;64(24):9180–9184. doi: 10.1158/0008-5472.can-04-2682. [DOI] [PubMed] [Google Scholar]
- 9.Fuchs A., Colonna M. The role of NK cell recognition of nectin and nectin-like proteins in tumor immunosurveillance. Seminars in Cancer Biology. 2006;16(5):359–366. doi: 10.1016/j.semcancer.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Tomasec P., Wang E. C. Y., Davison A. J., et al. Downregulation of natural killer cell-activating ligand CD155 by human cytomegalovirus UL141. Nature Immunology. 2005;6(2):181–188. doi: 10.1038/ni1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Sherbiny Y. M., Meade J. L., Holmes T. D., et al. The requirement for DNAM-1, NKG2D, and NKp46 in the natural killer cell-mediated killing of myeloma cells. Cancer Research. 2007;67(18):8444–8449. doi: 10.1158/0008-5472.can-06-4230. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-Correa B., Gayoso I., Bergua J. M., et al. Decreased expression of DNAM-1 on NK cells from acute myeloid leukemia patients. Immunology and Cell Biology. 2012;90(1):109–115. doi: 10.1038/icb.2011.15. [DOI] [PubMed] [Google Scholar]
- 13.Verhoeven D. H. J., de Hooge A. S. K., Mooiman E. C. K., et al. NK cells recognize and lyse Ewing sarcoma cells through NKG2D and DNAM-1 receptor dependent pathways. Molecular Immunology. 2008;45(15):3917–3925. doi: 10.1016/j.molimm.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Martin T. A., Lane J., Harrison G. M., Jiang W. G. The expression of the nectin complex in human breast cancer and the role of Nectin-3 in the control of tight junctions during metastasis. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0082696.e82696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oshima T., Sato S., Kato J., et al. Nectin-2 is a potential target for antibody therapy of breast and ovarian cancers. Molecular Cancer. 2013;12(1, article 60) doi: 10.1186/1476-4598-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miao X., Yang Z.-L., Xiong L., et al. Nectin-2 and DDX3 are biomarkers for metastasis and poor prognosis of squamous cell/adenosquamous carcinomas and adenocarcinoma of gallbladder. International Journal of Clinical & Experimental Pathology. 2013;6(2):179–190. [PMC free article] [PubMed] [Google Scholar]
- 17.Guzman G., Oh S., Shukla D., Valyi-Nagy T. Nectin-1 expression in the normal and neoplastic human uterine cervix. Archives of Pathology and Laboratory Medicine. 2006;130(8):1193–1195. doi: 10.5858/2006-130-1193-NEITNA. [DOI] [PubMed] [Google Scholar]
- 18.Linder P. Yeast RNA helicases of the DEAD-box family involved in translation initiation. Biology of the Cell. 2003;95(3-4):157–167. doi: 10.1016/s0248-4900(03)00032-7. [DOI] [PubMed] [Google Scholar]
- 19.Rosner A., Rinkevich B. The DDX3 subfamily of the DEAD box helicases: divergent roles as unveiled by studying different organisms and in vitro assays. Current Medicinal Chemistry. 2007;14(23):2517–2525. doi: 10.2174/092986707782023677. [DOI] [PubMed] [Google Scholar]
- 20.Schröder M. Human DEAD-box protein 3 has multiple functions in gene regulation and cell cycle control and is a prime target for viral manipulation. Biochemical Pharmacology. 2010;79(3):297–306. doi: 10.1016/j.bcp.2009.08.032. [DOI] [PubMed] [Google Scholar]
- 21.Choi Y.-J., Lee S.-G. J. The DEAD-box RNA helicase DDX3 interacts with DDX5, co-localizes with it in the cytoplasm during the G2/M phase of the cycle, and affects its shuttling during mrnp export. Journal of Cellular Biochemistry. 2012;113(3):985–996. doi: 10.1002/jcb.23428. [DOI] [PubMed] [Google Scholar]
- 22.Chao C.-H., Chen C.-M., Cheng P.-L., Shih J.-W., Tsou A.-P., Lee Y.-H. W. DDX3, a DEAD box RNA helicase with tumor growth-suppressive property and transcriptional regulation activity of the p21waf1/cip1 promoter, is a candidate tumor suppressor. Cancer Research. 2006;66(13):6579–6588. doi: 10.1158/0008-5472.CAN-05-2415. [DOI] [PubMed] [Google Scholar]
- 23.Chang P.-C., Chi C.-W., Chau G.-Y., et al. DDX3, a DEAD box RNA helicase, is deregulated in hepatitis virus-associated hepatocellular carcinoma and is involved in cell growth control. Oncogene. 2006;25(14):1991–2003. doi: 10.1038/sj.onc.1209239. [DOI] [PubMed] [Google Scholar]
- 24.Bol G. M., Raman V., van der Groep P., et al. Expression of the RNA helicase DDX3 and the hypoxia response in breast cancer. PLoS ONE. 2013;8(5) doi: 10.1371/journal.pone.0063548.e63548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu D.-W., Lee M.-C., Wang J., Chen C.-Y., Cheng Y.-W., Lee H. DDX3 loss by p53 inactivation promotes tumor malignancy via the MDM2/Slug/E-cadherin pathway and poor patient outcome in non-small-cell lung cancer. Oncogene. 2014;33(12):1515–1526. doi: 10.1038/onc.2013.107. [DOI] [PubMed] [Google Scholar]
- 26.Wu D.-W., Liu W.-S., Wang J., Chen C.-Y., Cheng Y.-W., Lee H. Reduced p21WAF1/CIP1 via alteration of p53-DDX3 pathway is associated with poor relapse-free survival in early-stage human papillomavirus-associated lung cancer. Clinical Cancer Research. 2011;17(7):1895–1905. doi: 10.1158/1078-0432.ccr-10-2316. [DOI] [PubMed] [Google Scholar]
- 27.Lee C.-H., Lin S.-H., Yang S.-F., et al. Low/negative expression of DDX3 might predict poor prognosis in non-smoker patients with oral cancer. Oral Diseases. 2014;20(1):76–83. doi: 10.1111/odi.12076. [DOI] [PubMed] [Google Scholar]
- 28.Hruban R. H., Pitman M. B., Klimstra D. S. Tumors of the Pancreas. Fascicle 6. Vol. 4. Washington, DC, USA: American Registry of Pathology—AFIP; 2007. (AFIP Atlas of Tumor Pathology). [Google Scholar]
- 29.Wang W., Yang Z.-L., Liu J.-Q., Jiang S., Miao X.-Y. Identification of CD146 expression, angiogenesis, and lymphangiogenesis as progression, metastasis, and poor-prognosis related markers for gallbladder adenocarcinoma. Tumor Biology. 2012;33(1):173–182. doi: 10.1007/s13277-011-0260-8. [DOI] [PubMed] [Google Scholar]
- 30.Lopez M., Aoubala M., Jordier F., Isnardon D., Gomez S., Dubreuil P. The human poliovirus receptor related 2 protein is a new hematopoietic/endothelial homophilic adhesion molecule. Blood. 1998;92(12):4602–4611. [PubMed] [Google Scholar]
- 31.Takahashi K., Nakanishi H., Miyahara M., et al. Nectin/PRR: an immunoglobulin-like cell adhesion molecule recruited to cadherin-based adherens junctions through interaction with Afadin, a PDZ domain-containing protein. The Journal of Cell Biology. 1999;145(3):539–549. doi: 10.1083/jcb.145.3.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oshima T., Sato S., Kato J., et al. Nectin-2 is a potential target for antibody therapy of breast and ovarian cancers. Molecular Cancer. 2013;12, article 60 doi: 10.1186/1476-4598-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodamilans B., Montoya G. Expression, purification, crystallization and preliminary X-ray diffraction analysis of the DDX3 RNA helicase domain. Acta Crystallographica Section F: Structural Biology and Crystallization Communications. 2007;63(4):283–286. doi: 10.1107/S1744309107006434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Botlagunta M., Vesuna F., Mironchik Y., et al. Oncogenic role of DDX3 in breast cancer biogenesis. Oncogene. 2008;27(28):3912–3922. doi: 10.1038/onc.2008.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGivern D. R., Lemon S. M. Tumor suppressors, chromosomal instability, and hepatitis C virus-associated liver cancer. Annual Review of Pathology: Mechanisms of Disease. 2009;4:399–415. doi: 10.1146/annurev.pathol.4.110807.092202. [DOI] [PMC free article] [PubMed] [Google Scholar]