Abstract
Smoke-free legislation is associated with improved early-life outcomes; however its impact on perinatal survival is unclear. We linked individual-level data with death certificates for all registered singletons births in England (1995–2011). We used interrupted time series logistic regression analysis to study changes in key adverse perinatal events following the July 2007 national, comprehensive smoke-free legislation. We studied 52,163 stillbirths and 10,238,950 live-births. Smoke-free legislation was associated with an immediate 7.8% (95%CI 3.5–11.8; p < 0.001) reduction in stillbirth, a 3.9% (95%CI 2.6–5.1; p < 0.001) reduction in low birth weight, and a 7.6% (95%CI 3.4–11.7; p = 0.001) reduction in neonatal mortality. No significant impact on SIDS was observed. Using a counterfactual scenario, we estimated that in the first four years following smoke-free legislation, 991 stillbirths, 5,470 cases of low birth weight, and 430 neonatal deaths were prevented. In conclusion, smoke-free legislation in England was associated with clinically important reductions in severe adverse perinatal outcomes.
Fifty years after the official recognition of its adverse health effects, tobacco smoking remains the primary cause of preventable mortality worldwide1. Besides affecting smokers’ health, exposure to second-hand smoke (SHS) is estimated to cause over 600,000 deaths annually worldwide2. Children account for over a quarter of these deaths and over half of the estimated 10.9 million disability-adjusted life years (DALYs) attributable to SHS exposure2. Among the key adverse outcomes associated with early-life SHS exposure are low birth weight (birth weight <2,500 grams)1,3, stillbirth1,4,5, and early-life mortality1, including sudden infant death syndrome (SIDS)1,6.
Population-level reductions in SHS exposure and active smoking can effectively be achieved by implementing legislation to prohibit smoking in enclosed public places and the workplace7. This is associated with significant health benefits among adults7,8. In a comprehensive assessment of its early-life health impact, we recently demonstrated that smoke-free legislation was associated with 10% reductions in both preterm birth and hospitalisations for childhood asthma9. The improvements in perinatal outcomes are likely mediated via reductions in maternal SHS exposure as well as active maternal smoking9,10,11,12,13,14. The data were however equivocal in relation to the impact on low birth weight babies9. We furthermore failed to identify any studies investigating the impact of smoke-free legislation on perinatal mortality, which was identified as a key knowledge gap9. Perinatal mortality is the primary contributor to the considerable global burden of under-five-mortality15. Given the urgent need for novel interventions in order to meet the fourth Millenium Development Goal of reducing this burden16, and the fact that only around 15% of the world’s population is currently covered by comprehensive smoke-free legislation17, the potential scope for improving early life outcomes is substantial.
We sought to address this by investigating the association between the 2007 national introduction of smoke-free legislation in England and various indicators of early-life mortality – namely stillbirth, neonatal mortality, and SIDS – in a national birth cohort of over 10 million singleton births. Given the conflicting evidence from previous studies9, we also evaluated the association between the legislation and low birth weight and updated our meta-analysis using these data. We hypothesised that smoke-free legislation would be associated with a reduced risk of developing the adverse perinatal outcomes evaluated.
Results
Study population
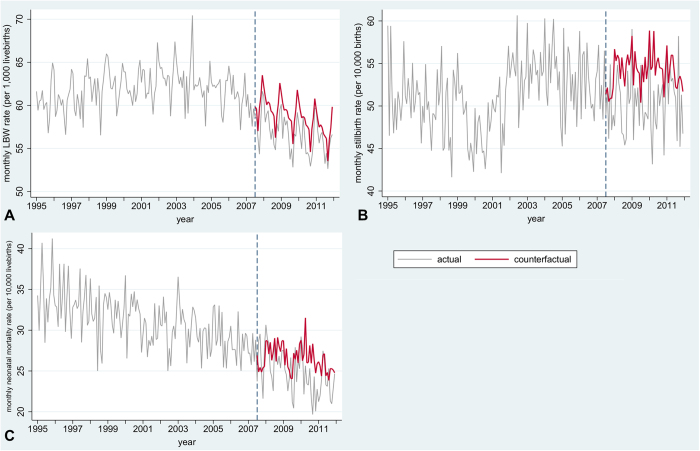
During the study period, 10,291,113 singleton births were registered in England, including 52,163 stillbirths (0.5%; Fig. 1). Among the 10,238,950 singleton live-births, birth weight was recorded for 10,193,544 (99.6%), 606,800 (6.0%) of whom had low birth weight and 97,246 (1.0%) of whom had very low birth weight. Infant death occurred among 47,032 (0.5%) live-born infants and included 23,929 (0.2%) early neonatal deaths, 7,271 (0.1%) late neonatal deaths, and 15,832 (0.2%) post-neonatal deaths. 4,782 infant deaths were categorised as SIDS.
Figure 1. Flow diagram describing base population and number of individuals with primary and secondary outcomes.
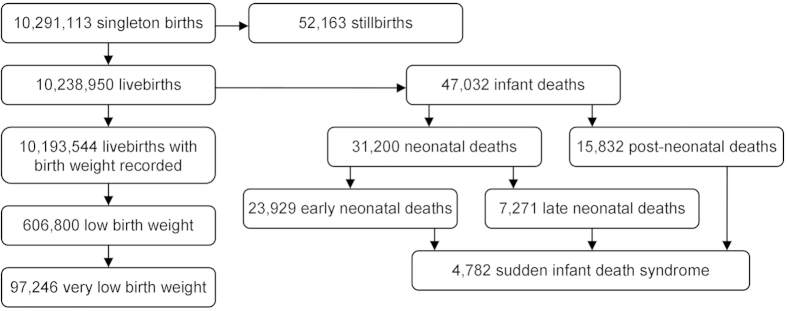
.
Stillbirth and early-life mortality were highly associated with low birth weight categories and low socioeconomic status, and less strongly with other demographic characteristics (Table 1). Important predictors of low birth weight included female sex, being a firstborn child, and low socioeconomic status (Table 2).
Table 1. Demographic characteristics according to mortality categories.
| Live-births (n = 10,238,950) | Stillbirths (n = 52,163) |
Infant deaths (n = 47,032) |
||||||
|---|---|---|---|---|---|---|---|---|
| All infant deaths (n = 47,032) |
Neonatal deaths (n = 31,200) |
Post-neonatal deaths (n = 15,832) | SIDS (4,782) | |||||
| All neonatal deaths (n = 31,200) | Early neonatal deaths (n = 23,929) | Late neonatal deaths (n = 7,271) | ||||||
| Maternal age (years) | ||||||||
| <20 | 691,251 (6.8) | 4,229 (8.1) | 4,999 (10.6) | 2,886 (9.3) | 2,132 (8.9) | 754 (10.4) | 2,113 (13.3) | 953 (19.9) |
| 20–24 | 1,926,659 (18.8) | 10,007 (19.3) | 10,356 (22.0) | 6,457 (20.7) | 4,884 (20.4) | 1,573 (21.6) | 3,899 (24.6) | 1,465 (30.6) |
| 25–29 | 2,874,147 (28.1) | 13,689 (26.2) | 12,392 (26.3) | 8,354 (26.8) | 6,392 (26.7) | 1,962 (27.0) | 4,038 (25.5) | 1,077 (22.5) |
| 30–34 | 2,954,400 (28.9) | 13,668 (26.2) | 11,225 (23.9) | 7,848 (25.2) | 6,131 (25.6) | 1,717 (23.6) | 3,377 (21.3) | 793 (16.6) |
| 35–39 | 1,487,027 (14.5) | 8,046 (15.4) | 6,330 (13.5) | 4,461 (14.3) | 3,476 (14.5) | 985 (13.5) | 1,869 (11.8) | 403 (8.4) |
| ≥40 | 305,415 (3.0) | 2,454 (4.7) | 1,730 (3.7) | 1,194 (3.8) | 914 (3.8) | 280 (3.9) | 536 (3.4) | 91 (1.9) |
| Missing | 51 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Parity | ||||||||
| 0 | 2,441,463 (40.6) | 10,849 (38.0) | 10,353 (42.6) | 7,637 (45.7) | 5,950 (46.1) | 1,687 (44.3) | 2,716 (35.7) | 386 (27.4) |
| 1 | 2,188,681 (36.4) | 9,040 (31.6) | 7,141 (29.4) | 4,748 (28.4) | 3,643 (28.3) | 1,105 (29.0) | 2,393 (31.4) | 451 (32.0) |
| 2 | 884,312 (14.7) | 4,630 (16.2) | 3,712 (15.3) | 2,349 (15.2) | 1,788 (13.9) | 561 (14.7) | 1,363 (17.9) | 302 (21.4) |
| ≥3 | 496,592 (8.3) | 4,053 (14.2) | 3,102 (12.8) | 1,960 (11.7) | 1,507 (11.7) | 453 (11.9) | 1,142 (15.0) | 270 (19.2) |
| Missing | 4,227,902 (41.3) | 23,591 (45.2) | 22,724 (48.3) | 14,093 (46.5) | 11,041 (46.1) | 3,465 (47.7) | 8,218 (51.9) | 3,373 (70.5) |
| Marital status | ||||||||
| Married | 6,011,122 (58.7) | 28,573 (54.8) | 24,308 (51.7) | 16,694 (53.5) | 12,888 (53.9) | 3,806 (52.3) | 7,614 (48.1) | 1,409 (29.5) |
| Not married | 4,227,828 (41.3) | 23,590 (45.2) | 22,724 (48.3) | 14,506 (46.5) | 11,041 (46.1) | 3,465 (47.7) | 8,218 (51.9) | 3,373 (70.5) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sex | ||||||||
| Male | 5,251,746 (51.3) | 27,509 (52.7) | 26,571 (56.5) | 17,532 (56.3) | 13,479 (56.3) | 4,083 (56.2) | 9,009 (56.9) | 2,821 (59.0) |
| Female | 4,987,201 (48.7) | 24,654 (47.3) | 20,461 (43.5) | 13,638 (43.7) | 10,450 (43.7) | 3,188 (43.8) | 6,823 (43.1) | 1,961 (41.0) |
| Missing | 3 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Birth weight (grams) | ||||||||
| <1000 | 41,737 (0.4) | 15,719 (30.4) | 16,073 (35.3) | 13,826 (46.3) | 11,496 (50.6) | 2,330 (32.8) | 2,247 (14.3) | 66 (1.4) |
| 1000–1499 | 55,509 (0.5) | 6,500 (12.6) | 3,708 (8.1) | 2,732 (9.2) | 2,011 (8.8) | 721 (10.2) | 976 (6.2) | 151 (3.2) |
| 1500–2499 | 509,554 (5.0) | 11,722 (22.7) | 7,175 (15.8) | 4,202 (14.1) | 3,055 (13.4) | 1,147 (16.2) | 2,973 (19.0) | 869 (18.3) |
| 2500–3999 | 8,422,413 (82.6) | 15,719 (30.4) | 17,009 (37.4) | 8,174 (27.4) | 5,482 (24.1) | 2,692 (37.9) | 8,835 (56.4) | 3442 (74.5) |
| ≥4000 | 1,164,331 (11.4) | 2,051 (4.0) | 1,538 (3.4) | 906 (3.0) | 694 (3.1) | 212 (3.0) | 632 (4.0) | 220 (4.6) |
| Missing | 45,406 (0.4) | 453 (0.9) | 1,529 (3.3) | 1,360 (4.4) | 1,191 (5.0) | 169 (2.3) | 169 (1.1) | 34 (0.7) |
| IMD quintile | ||||||||
| 1 (most deprived) | 1,817,749 (18.2) | 11,127 (21.7) | 10,359 (22.6) | 6,910 (22.8) | 5,296 (22.8) | 1,614 (22.6) | 3,449 (22.2) | 991 (21.4) |
| 2 | 2,618,898 (26.3) | 14,467 (28.2) | 13,546 (29.6) | 8,980 (29.6) | 6,895 (29.7) | 2,085 (29.2) | 4,566 (29.4) | 1,253 (27.0) |
| 3 | 2,241,333 (22.5) | 11,099 (21.6) | 9,954 (21.7) | 6,598 (21.7) | 5,005 (21.6) | 1,593 (22.3) | 3,356 (21.6) | 1,079 (23.3) |
| 4 | 1,953,029 (19.6) | 8,984 (17.5) | 7,536 (16.4) | 4,892 (16.1) | 3,737 (16.1) | 1,155 (16.2) | 2,644 (17.0) | 816 (17.6) |
| 5 (least deprived) | 1,344,295 (13.5) | 5,664 (11.0) | 4,466 (9.7) | 2,960 (9.8) | 2,264 (9.8) | 696 (9.7) | 1,506 (9.7) | 497 (10.7) |
| Missing | 263,646 (2.6) | 822 (1.6) | 1,171 (2.5) | 860 (2.8) | 732 (3.1) | 128 (1.8) | 311 (2.0) | 146 (3.1) |
| Region | ||||||||
| Greater London | 1,891,740 (19.0) | 11,258 (21.9) | 9,163 (20.0) | 6,046 (19.9) | 4,551 (19.6) | 1,495 (20.9) | 3,117 (20.1) | 716 (15.4) |
| North East | 471,619 (4.7) | 2,458 (4.8) | 2,102 (4.6) | 1,347 (4.4) | 998 (4.3) | 349 (4.9) | 755 (4.9) | 277 (6.0) |
| North West | 1,355,390 (13.6) | 7,131 (13.9) | 6,907 (15.1) | 4,439 (14.6) | 3,360 (14.5) | 1,079 (15.1) | 2,468 (15.9) | 879 (18.8) |
| Yorkshire and the Humber | 1,000,678 (10.0) | 5,517 (10.7) | 5,286 (11.5) | 3,421 (11.3) | 2,568 (11.1) | 854 (12.0) | 1,865 (12.0) | 493 (10.6) |
| East Midlands | 726,852 (7.3) | 3,615 (7.0) | 3,354 (7.3) | 2,316 (7.6) | 1,775 (7.6) | 531 (7.4) | 1,074 (6.9) | 348 (7.5) |
| West Midlands | 1,097,732 (11.0) | 5,924 (11.5) | 6,292 (13.7) | 4,411 (14.5) | 3,557 (15.3) | 853 (11.9) | 1,881 (12.1) | 539 (11.6) |
| East of England | 1,026,552 (10.3) | 4,670 (9.1) | 3,819 (8.3) | 2,494 (8.2) | 1,931 (8.3) | 563 (7.9) | 1,325 (8.5) | 364 (7.9) |
| South East | 812,769 (8.1) | 3,508 (6.8) | 2,650 (5.8) | 1,724 (5.7) | 1,317 (5.7) | 407 (5.7) | 926 (6.0) | 326 (7.0) |
| South Central | 721,568 (7.2) | 3,422 (6.7) | 2,833 (6.2) | 1,862 (6.1) | 1,390 (6.0) | 472 (6.6) | 971 (6.3) | 281 (6.1) |
| South West | 870,404 (8.7) | 3,838 (7.5) | 3,455 (7.5) | 2,280 (7.5) | 1,749 (7.7) | 541 (7.6) | 1,139 (7.3) | 420 (9.1) |
| Missing | 263,646 (2.6) | 822 (1.6) | 1,171 (2.5) | 860 (2.8) | 732 (3.1) | 128 (1.8) | 311 (2.0) | 146 (3.1) |
| Urbanisation level | ||||||||
| Urban | 9,759,136 (97.8) | 50,371 (98.1) | 45,115 (98.4) | 29,828 (98.3) | 22,787 (98.2) | 7,041 (98.6) | 15,287 (98.5) | 4,563 (98.4) |
| Rural | 216,168 (2.2) | 970 (1.9) | 746 (1.6) | 512 (1.7) | 410 (1.8) | 102 (1.4) | 234 (1.5) | 73 (1.6) |
| Missing | 263,646 (2.6) | 822 (1.6) | 1,171 (2.5) | 860 (2.8) | 732 (3.1) | 128 (1.8) | 311 (2.0) | 146 (3.1) |
Numbers represent numbers of babies in each stratum. Percentages in parentheses relate to all babies with valid data for that particular variable. For missing data, percentages of the full sample are given. SIDS = sudden infant death syndrome; IMD = Index of Multiple Deprivation.
Table 2. Demographic characteristics according to birth weight categories.
| Birth weight ≥ 2,500 g (n = 9,586,744) | Low birth weight (n = 606,800) | Very low birth weight (n = 97,246) | Birth weight missing (n = 45,406) | |
|---|---|---|---|---|
| Maternal age (years) | ||||
| <20 | 632,058 (6.6) | 56,372 (9.3) | 8,999 (9.3) | 2,821 (6.2) |
| 20–24 | 1,785,158 (18.6) | 133,010 (21.9) | 19,669 (20.2) | 8,491 (18.7) |
| 25–29 | 2,697,989 (28.1) | 163,814 (27.0) | 25,485 (26.2) | 12,344 (27.2) |
| 30–34 | 2,791,293 (29.1) | 150,470 (24.8) | 24,480 (25.2) | 12,637 (27.9) |
| 35–39 | 1,397,224 (14.6) | 82,428 (13.6) | 14,705 (15.1) | 7,375 (16.3) |
| ≥40 | 283,019 (3.0) | 20,706 (3.4) | 3,908 (4.0) | 1,691 (3.7) |
| Missing | 4 (0.0) | 0 (0.0) | 0 (0.0) | 47 (0.1) |
| Parity | ||||
| 0 | 2,271,216 (40.0) | 156,788 (50.1) | 24,541 (50.2) | 13,495 (52.6) |
| 1 | 2,095,213 (36.9) | 86,370 (27.6) | 13,165 (26.9) | 7,098 (27.7) |
| 2 | 841,217 (14.8) | 40,002 (12.8) | 6,282 (12.9) | 3,093 (12.1) |
| ≥3 | 465,144 (8.2) | 29,492 (9.4) | 4,875 (10.0) | 1,956 (7.6) |
| Missing | 3,913,954 (40.8) | 294,148 (48.5) | 48,383 (49.8) | 19,800 (43.6) |
| Marital status | ||||
| Married | 5,672,849 (59.2) | 312,659 (51.5) | 48,865 (50.2) | 25,614 (56.4) |
| Not married | 3,913,895 (40.8) | 294,141 (48.5) | 48,381 (49.8) | 19,792 (43.6) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0) |
| Sex | ||||
| Male | 4,939,679 (51.5) | 288,753 (47.6) | 49,784 (51.2) | 23,314 (51.3) |
| Female | 4,647,062 (48.5) | 318,047 (52.4) | 47,462 (48.8) | 22,092 (48.7) |
| Missing | 3 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0) |
| IMD quintile | ||||
| 1 (most deprived) | 1,676,895 (18.0) | 129,769 (21.7) | 21,871 (22.8) | 11,085 (26.4) |
| 2 | 2,439,576 (26.1) | 168,089 (28.0) | 27,599 (28.8) | 11,233 (26.8) |
| 3 | 2,100,475 (22.5) | 132,485 (22.1) | 21,227 (22.1) | 8,373 (20.0) |
| 4 | 1,842,889 (19.7) | 102,493 (17.1) | 15,510 (16.1) | 7,647 (18.2) |
| 5 (least deprived) | 1,274,139 (13.7) | 66,542 (11.0) | 9,692 (10.1) | 3,614 (8.6) |
| Missing | 252,770 (2.6) | 7,422 (1.2) | 1,347 (1.4) | 3,454 (7.6) |
| Region | ||||
| Greater London | 1,754,925 (18.8) | 120,352 (20.1) | 21,381 (22.3) | 16,463 (39.2) |
| North East | 440,830 (4.7) | 29,295 (4.9) | 4,579 (4.8) | 1,494 (3.6) |
| North West | 1,265,206 (13.6) | 85,422 (14.3) | 13,108 (13.7) | 4,762 (11.4) |
| Yorkshire and the Humber | 932,580 (10.0) | 64,903 (10.8) | 9,851 (10.7) | 3,195 (7.6) |
| East Midlands | 680,606 (7.3) | 45,086 (7.5) | 6,932 (7.2) | 1,160 (2.8) |
| West Midlands | 1,020,237 (10.9) | 75,470 (12.6) | 12,132 (12.7) | 2,025 (4.8) |
| East of England | 969,400 (10.4) | 54,056 (9.0) | 8,422 (8.8) | 3,096 (7.4) |
| South East | 769,979 (8.2) | 40,383 (6.7) | 5,996 (6.3) | 2,407 (5.7) |
| South Central | 680,340 (7.3) | 38,901 (6.5) | 6,345 (6.6) | 2,327 (5.5) |
| South West | 819,871 (8.8) | 45,510 (7.6) | 7,153 (7.5) | 5,023 (12.0) |
| Missing | 252,770 (2.6) | 7,422 (1.2) | 1,347 (1.4) | 3,454 (7.6) |
| Urbanisation level | ||||
| Urban | 9,128,455 (97.4) | 589,290 (98.3) | 94,414 (98.6) | 41,391 (98.7) |
| Rural | 205,519 (2.6) | 10,088 (1.7) | 1,485 (1.4) | 561 (1.3) |
| Missing | 252,770 (2.6) | 7,422 (1.2) | 1,347 (1.4) | 3,454 (7.6) |
Numbers represent numbers of live-born babies in each stratum. Percentages in parentheses relate to all babies with valid data for that particular variable. For missing data, percentages of the full sample are given. IMD = Index of Multiple Deprivation.
Smoke-free legislation and early-life outcomes
Introduction of smoke-free legislation was associated with an immediate 7.8% (95% CI 3.5 to 11.8; p < 0.001) reduction in odds of being stillborn, a 3.9% (95% CI 2.6 to 5.1; p < 0.001) reduction in odds of having low birth weight, and a 7.6% (95% CI 3.4 to 11.7; p = 0.001) decrease in odds of neonatal mortality over-and-above the underlying temporal trend (Table 3 and Supplementary Table S1). No significant change in odds of SIDS was observed: 1.8% (95% CI −8.4 to 13.2; p = 0.74).
Table 3. Impact of smoke-free legislation on primary and secondary outcomes.
| |
Sensitivity analyses |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Primary analysis |
Model 1 |
Model 2 |
||||||||||
| N | OR | 95%CI | P-value | N | OR | 95%CI | P-value | N | OR | 95%CI | P-value | |
| Primary outcomes | ||||||||||||
| Low birth weight | 9,933,349 | 0.961 | 0.949–0.974 | <0.001 | 5,822,837 | 0.980 | 0.962–0.998 | 0.032 | 9,933,349 | 0.963 | 0.951–0.976 | <0.001 |
| Stillbirth | 9,984,278 | 0.922 | 0.881–0.965 | <0.001 | 5,850,909 | 0.910 | 0.855–0.970 | 0.003 | 9,984,278 | 0.919 | 0.878–0.962 | <0.001 |
| Neonatal mortality | 9,933,349 | 0.924 | 0.883–0.966 | 0.001 | 5,822,837 | 0.932 | 0.877–0.991 | 0.025 | 9,933,349 | 0.924 | 0.883–0.966 | 0.001 |
| SIDS | 9,933,349 | 1.018 | 0.916–1.132 | 0.735 | 5,822,837 | 0.990 | 0.808–1.213 | 0.924 | 9,933,349 | 1.018 | 0.916–1.132 | 0.735 |
| Secondary outcomes | ||||||||||||
| Very low birth weight | 9,933,349 | 1.010 | 0.978–1.042 | 0.558 | ||||||||
| Early neonatal mortality | 9,933,349 | 0.958 | 0.890–1.032 | 0.258 | ||||||||
| Late neonatal mortality | 9,911,272 | 0.863 | 0.793–0.940 | 0.001 | ||||||||
| Post-neonatal mortality | 9,904,292 | 0.954 | 0.900–1.010 | 0.106 | ||||||||
| Infant mortality | 9,933,349 | 0.937 | 0.904–0.971 | <0.001 | ||||||||
Odds ratios indicate odds of developing outcome in period after versus period before July 2007, when smoke-free legislation was introduced. Primary models are adjusted for non-linear underlying time trends (via B-splines), month, maternal age, maternal marital status, sex, socioeconomic status, region, and urbanisation level and based on individual-level analysis of complete cases. Mortality models are furthermore adjusted for birth weight. For sensitivity analyses, model 1 is the complete case model with additional adjustment for parity, whereas in model 2 missing data for parity are imputed. OR = odds ratio; CI = confidence interval; SIDS = sudden infant death syndrome.
The reduction in neonatal mortality was primarily attributable to an impact on late neonatal deaths: −13.7% (95% CI −20.7 to −6.0; p = 0.001; Table 3 and Supplementary Table S2). A significant immediate reduction in overall odds of infant mortality was also observed: −6.3% (95% CI −9.6 to −2.9; p < 0.001). Smoke-free legislation was not associated with significant changes in the odds of the other secondary outcomes (Table 3).
Sensitivity analyses
The findings were highly robust in pre-specified (Table 3) and post-hoc sensitivity analyses (Supplementary Table S3).
Counterfactual estimates of cases averted
Using a counterfactual scenario (Figs 2 and 3), we estimated that in the first four years following the implementation of smoke-free legislation in England 5,470 cases of low birth weight, 992 stillbirths, and 501 infant deaths, including 430 neonatal deaths, were averted.
Figure 2. Actual and counterfactual rates for primary outcomes.
Actual rates are based on all registered singleton births in England for stillbirth (n = 10,291,113) and all singleton live-births for the other outcomes (n = 10,238,950). Counterfactual rates are model-predicted rates based on a complete case scenario but without impact of smoke-free legislation (n = 9,984,278 for stillbirth, n = 9,933,349 for other outcomes). Only outcomes where smoke-free legislation had a significant impact are shown. A: low birth weight; B: stillbirth; C: neonatal mortality. Models are adjusted for non-linear underlying time trends, seasonality, maternal age, maternal marital status, sex, socioeconomic status, region, and urbanisation level and based on complete cases. Mortality models are also adjusted for birth weight. Dotted line represents introduction of smoke-free legislation. Note different scales on Y-axis.
Figure 3. Actual and counterfactual rates for secondary outcomes.
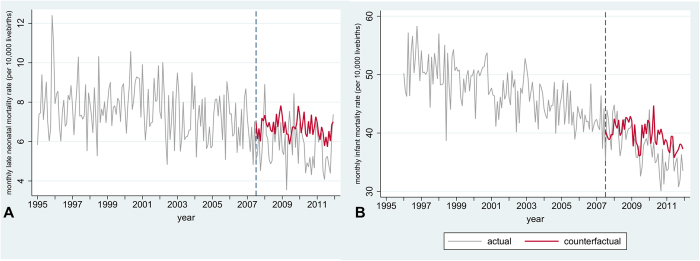
Actual rates are based on all registered live-births in England for infant mortality (n = 10,238,950) and on all babies alive at day seven after birth for late neonatal mortality (n = 10,207,750). Counterfactual rates are model-predicted rates based on a complete case scenario but without impact of smoke-free legislation (n = 9,911,272 for late neonatal mortality, n = 9,933,349 for infant mortality). Only outcomes where smoke-free legislation had a significant impact are shown. A: late neonatal mortality (n = 9,911,272); B: infant mortality (n = 9,933,349). Models are adjusted for non-linear time trends, month, maternal age, maternal marital status, sex, birth weight, socioeconomic status, region, and urbanisation level and based on complete cases. Dotted line represents introduction of smoke-free legislation. Note different scales on Y-axis.
Discussion
Introduction of smoke-free legislation in England was associated with clinically important reductions in stillbirth, low birth weight, and neonatal and infant mortality.
Analysing over 10 million births this is, to the best of our knowledge, one of the largest studies to have investigated the impact of smoke-free legislation on early life health, and the first to focus on perinatal mortality9. We obtained data from national birth and death registries, which constitute the primary source for the production of English national statistics, thereby minimising risks of individuals being missed. Registration of individual data items attained a high level of completeness, with over 97% of individuals having complete data on all covariates included in the primary analyses.
Our study has a number of potential limitations. We had no individual-level information on maternal smoking status during pregnancy. We were therefore unable to assess whether a possible reduction in maternal smoking following introduction of smoke-free legislation, as observed by others, contributed to the observed improvement in perinatal outcomes10,11,12,13,14. Also, a gestational age indicator was missing from the data, as this information was only recorded as an individual item by the Office for National Statistics from 2006 onwards. It was thus not possible to distinguish between the most common underlying causes of low birth weight: intrauterine growth restriction (i.e. being small for gestational age) and reduced length of gestation (i.e. being born preterm)18. In a recent meta-analysis, we demonstrated that smoke-free legislation was associated with reductions in the incidence of preterm birth and of being very small for gestational age9, suggesting that both mechanisms are likely to have contributed to the observed reduction in low birth weight identified. Similarly, we were unable to assess whether the decreases in neonatal and infant mortality identified may in part have been mediated via a reduction in preterm births9. It is however important to note that although missing data on gestational age and maternal smoking status limited the opportunity for a detailed assessment of possible causal pathways (Supplementary Figure S1), this had no bearing on the validity of our findings in relation to the main hypothesis under investigation.
When interpreting our findings it should be noted that over 50% of employed adults already worked in a smoke-free workplace before the legislation was implemented19. There is thus a risk that our study under-estimated the true potential impact of smoke-free legislation, which may be larger in countries with a lower proportion of smoke-free environments prior to implementation. In this respect, it is also important to note that this study was undertaken in a country with comparatively good early life outcomes when judged against international standards20,21.
National public health interventions typically do not allow evaluation through randomised controlled study designs22. We therefore evaluated the impact of smoke-free legislation by undertaking a quasi-experimental study, accepting consequential limitations in causal inference22. It is in such contexts important to consider other factors that may help inform causal reasoning. Particularly noteworthy is that the reductions in adverse early-life outcomes we identified are in line with previous studies demonstrating particular perinatal health benefits as described above (i.e. reductions in low birth weight, being small for gestational age, and preterm birth)11,12,13,23,24,25,26,27,28. Furthermore, the link between smoke-free legislation and these reductions is highly plausible given that both SHS exposure and active smoking are well-established risk factors for adverse pregnancy outcomes and infant death1. Meta-analyses of studies among non-smoking women have shown that SHS exposure during pregnancy was associated with a 1.32 (95% CI 1.07 to 1.63; p = 0.02) times increased risk of low birth weight and a 1.23 (95% CI 1.09 to 1.38; p < 0.001) times increased risk of stillbirth3,4. Furthermore, a dose-dependent inverse relationship between maternal urinary cotinine levels (as a proxy for SHS exposure) and offspring birth weight has recently been described29. Contemporary studies assessing the impact of SHS exposure on neonatal mortality are however lacking4,30. As for active maternal smoking during pregnancy, a reduction in which is highly likely to be on the causal pathway between smoke-free legislation and improved perinatal outcomes (Supplementary Figure S1)1,10,11,12,13,14 there is a strong association with adverse pregnancy outcomes as demonstrated by studies reporting a 36–60% increased risk for stillbirth and a 20% increased risk for neonatal mortality1,5. Observational and experimental studies have found that maternal smoking cessation normalises these risks1,31,32,33. For example, a randomised controlled trial of a counselling intervention that successfully reduced SHS exposure during pregnancy reported a significant improvement in birth outcomes34. We are unaware of other public health interventions or changes in perinatal practice co-occurring with the implementation of smoke-free legislation in England that may have been responsible for such substantial immediate reductions in several key adverse perinatal outcomes.
Although no previous studies have investigated the impact of smoke-free legislation on perinatal mortality, several have studied its effect on birth weight11,12,13,23,24,25,26,35. In a recent meta-analysis of six studies, no significant overall impact on low birth weight could be demonstrated: −1.7% (95% CI −5.1 to 1.6; p = 0.31)9. We identified no new eligible studies in an update of this systematic review and meta-analysis (Supplementary Figure S2), focusing on (very) low birth weight and early-life mortality and following the methods described earlier36 Adding data from the current study to the existing meta-analyses, the overall reductions in the risk of low birth weight (7 studies, >12.1 million subjects: −2.20% [95% CI −4.95 to 0.54], p = 0.115) and very low birth weight (3 studies, >10.2 million subjects: −2.61% [95% CI −12.15 to 6.95], p = 0.591) following introduction of smoke-free legislation were not statistically significant. Of note however, the two studies that demonstrated a significant reduction in low birth weight were performed in countries where smoke-free legislation has been particularly comprehensive and compliance high12. Meta-analyses of smoke-free legislation and adult health have consistently shown that its health impact is larger when legislation is more comprehensive8,37. Additional studies are needed to study whether the same accounts for perinatal outcomes, which could further strengthen the case for WHO recommendations to implement comprehensive smoke-free laws17.
The association between smoke-free legislation and mortality was primarily attributable to a reduction in late neonatal mortality, which likely relates to the recognised association between antenatal smoke exposure and common causes of death in the late neonatal period38 such as necrotising enterocolitis39, bronchopulmonary dysplasia40,41, and sepsis42. We were unable to assess the differential association between smoke-free legislation and specific causes of death (except for SIDS) as this information was lacking from our data. Post-hoc sensitivity analyses indicate that the reduction in early-life mortality following smoke-free legislation was likely related to mechanisms other than improvement (i.e. increase) in birth weight.
Whereas we identified an overall association between smoke-free legislation and reduced infant mortality, we were surprised by the finding that SIDS was not affected1,5. Boldo et al. previously estimated that SHS exposure was responsible for 310–420 SIDS cases annually in Europe, amounting to 1.6 excess cases per 100,000 in 20056. It is possible that our study lacked power to detect small changes in this rare outcome although the point estimate was not suggestive of possible benefit (Table 3). As SIDS is a diagnosis per exclusionem, temporal changes in the diagnostic approach towards unexplained infant death (e.g. changes in the proportion of explained deaths, changes in post-mortem examination rates, inter-observer variation in diagnostic criteria) may have resulted in unexplained variation43,44. Misclassification of SIDS may furthermore have influenced the data45. Of note, a recent multi-country ecological analysis found that higher tobacco taxes, but not smoke-free laws, were associated with significant reductions in SIDS rates46.
The impact of smoke-free legislation on perinatal and early-life health is likely to have been mediated via several routes. A number of previous studies have demonstrated important drops in maternal smoking during pregnancy following implementation of smoke-free legislation1,10,11,12,13,14. In Scotland, for example, maternal smoking during pregnancy dropped from 25.4% to 18.8%12. At the same time, similar reductions in low birth weight were identified among women who smoked and those who did not smoke during pregnancy12, suggesting that at least part of the effect is mediated via mechanisms other than reducing active maternal smoking. Improvements in perinatal outcomes were observed among Norwegian mothers whose workplace became smoke-free13. In Belgium, both the smoking ban in pubs and restaurants, as well as the workplace ban benefitted perinatal health23. Smoke-free legislation has furthermore been associated with important drops in smoking in the home through social norm spreading47,48,49,50. The impact observed in our study is therefore likely to result from a mixture of reduced active smoking and reduced SHS exposure in the workplace, public places, and the home environment.
Our findings add an important new dimension to the emerging evidence on the benefits of smoke-free legislation to child health9,51, adding to the already well-established broad range of health benefits among adults7,8. Smoke-free laws are an inexpensive and efficient means to achieve sizeable improvements in population health52. Such laws are supported by the public, with support increasing further (particularly amongst smokers) following implementation53. Considering that only around 15% of the world’s population is currently protected by comprehensive smoke-free laws17, and that low birth weight and perinatal mortality remain the primary causes of childhood morbidity and mortality worldwide18,21,54, accelerated action to implement smoke-free legislation is likely to help save considerable numbers of young lives across the globe and through doing so enhance the much-needed progress in meeting the fourth Millennium Development Goal.
Since the majority of the burden of early-life morbidity and mortality occurs in low- and middle-income countries18,21, there is a particular need for studies assessing the impact of smoke-free legislation in these regions9. Work is also needed to determine the impact of tobacco control policies on marginalised populations in high-income country settings, as variation in maternal smoking across socioeconomic subgroups has been shown to account for approximately one-third of the inequalities in stillbirths and infant deaths55. Finally, research also needs to investigate the differential early-life health impact of varying degrees of comprehensiveness of smoke-free laws (e.g. extending the legislation to outdoor public places, private cars and homes) and different approaches to enforcement and success with compliance8.
In conclusion, we present evidence that implementation of smoke-free legislation in England was associated with substantial perinatal and early-life benefits, with over 5,000 cases of low birth weight and almost 1,500 deaths averted within four years.
Methods
This study was performed according to a pre-specified and registered research protocol (ClinicalTrials.gov NCT02039583). Using a national dataset of all singleton births registered in England between 1995 and 2011, we analysed the association between the July 2007 implementation of smoke-free legislation and the odds of stillbirth, low birth weight, and early-life mortality.
Ethical considerations
This study was reviewed by the National Health Services (NHS) South East Scotland Research Ethics Service and The University of Edinburgh’s Centre for Population Health Sciences Ethics Review Group. Both committees provided an exemption from formal ethical assessment based on the use of anonymised, unidentifiable data.
Implementation of smoke-free legislation
The intervention under study was the implementation of smoke-free legislation in England on 1 July 200756. From this date, smoking was prohibited in enclosed public places and workplaces in England, with very few exemptions (e.g. specialist tobacconist shops, designated rooms in palliative care hospices and in prisons). Immediate and sustained high levels of compliance with the smoke-free law have been attained, with over 98% of public premises and vehicles (e.g. taxis, private hire vehicles, coaches, and buses) found to be smoke-free in the first year following its implementation57.
Outcome definitions
Four primary outcomes were evaluated: low birth weight (live-birth with birth weight <2,500 grams); stillbirth (intrauterine death from 24 weeks of gestation); neonatal death (death in the first 28 days of life); SIDS (death within the first year of life coded on the death certificate as International Classification of Diseases (ICD) 10-U R95, or R99 with no other specification).
In addition, we considered the following secondary outcomes: very low birth weight (live-birth with birth weight <1,500 grams); early neonatal death (death in the first week of life); late neonatal death (death between 7 and 28 days of life); post-neonatal death (death between 28 days of life and the first birthday); and infant death (death within the first year of life).
Data on gestational age were not available through the Office for National Statistics before 2006, restricting the pre-legislation period to only 1.5 years. Given the recognised seasonal variation in gestational age we considered this period insufficient to estimate underlying trends pre-legislation, and therefore decided a priori not to involve preterm birth as an outcome or intermediate variable in our analyses.
Data sources and study population
Individual-level data on all registered singleton births in England between 1 January 1995 and 31 December 2011 were obtained via the government’s Office for National Statistics. Data were linked by the Office for National Statistics to death certificates for stillbirths and for all infants dying before their first birthday. To minimise the risks of individuals being identified, individual-level continuous variables were categorized as follows: month and year of birth; month and year of death; timing of death (stillbirth/early neonatal/late neonatal/post-neonatal); sex; birth weight (<1,000 grams/1,000–1,499 grams/1,500–2,499 grams/2,500–3,999 grams/≥4,000 grams); maternal marital status (married /not married); maternal parity; and maternal age (<20 years/20–24 years/25–29 years/30–34 years/35–39 years/≥40 years). The individual-level data also included Government Office Region, urbanisation level (urban/rural, based on Office for National Statistics classification for small area geographies), and socioeconomic status measured using the Index of Multiple Deprivation (in quintiles), these being derived from maternal post code of residence. The Index of Multiple Deprivation is a relative measure of deprivation at the small-area level58; an aggregate score is produced from 38 indicators in seven domains, namely: income; employment; health; education; crime; access to services; and living environment58.
Statistical analyses
The patterning of demographic data was initially tabulated by timing of death and birth weight categories. Separate logistic regression models using individual-level data were then developed to investigate the association between the introduction of smoke-free legislation and the odds of developing each outcome12. Akaike’s and Schwarz’s Bayesian information criteria (AIC and BIC, respectively) were used to select the optimal model from among six options (Supplementary Figure S3): a linear time-trend model with a sudden (‘step’) change in the odds of developing the outcome at the time of introduction of smoke-free legislation; a linear time-trend model with a gradual (‘slope’) change in odds following the introduction of smoke-free legislation; a linear time-trend model with both a step and a slope change; and three models with a step change only and the underlying time trends being modelled via linear, quadratic, and cubic B-splines, respectively59. A continuous time variable based on month of birth was used for linear time trend models. Via addition of these temporal trend terms all models thus accounted for the pre-existing (i.e. before introduction of smoke-free legislation) underlying trend in the odds of developing each outcome. The step change was modeled using a dummy variable code ‘0’ before and ‘1’ after the introduction of smoke-free legislation19. An interaction term between this dummy and the continuous time variable was included to model a slope change51,60. In addition, a categorical variable for month was added to each model to account for any seasonality in the data51,60.
The following categorical covariates were included in each model to account for potential individual-level confounding: sex; maternal age; maternal marital status; Index of Multiple Deprivation quintile; region; and urbanisation level. All mortality-related outcomes were also adjusted for birth weight.
Among the model covariates, data on parity were missing for a substantial portion of the study population (41.3%), as this variable had been recorded for married women only. All other covariates had 0–3% missing data. Since logistic regression analysis needs to be undertaken on cases with complete data for all covariates, parity was excluded from the primary models to maximise power. We performed two sets of pre-specified sensitivity analyses to investigate potential residual confounding resulting from exclusion of parity as a covariate. In the first set, models were re-run with parity included, analysing individuals with complete data only. In the second set, multiple imputations were performed using chained equations to impute missing data for parity, creating five unique datasets12. Models were then re-run on the imputed data. Sensitivity analyses were conducted for the primary outcomes only to minimise risks associated with multiple testing.
A change in odds of developing low birth weight following the introduction of smoke-free legislation is potentially on the causal pathway between smoke-free legislation and any observed impact on early-life mortality (Supplementary Figure S1). We therefore performed additional post-hoc sensitivity analyses to test whether exclusion of birth weight as a covariate from the models had any impact on the observed association between smoke-free legislation and early-life mortality.
In order to estimate the absolute impact of smoke-free legislation for outcomes that were significantly affected, we developed counterfactual scenarios51,60. For each individual, a predicted risk of developing the outcome was calculated using the Betas from the primary models, but setting the ban dummy at ‘0’ for the entire study period. This counterfactual risk thus represented the theoretical risk of developing the outcome, had smoke-free legislation not been implemented. We then subtracted the actual risk from the counterfactual risk, producing an excess risk for each individual. These were summed for the first four full years following smoke-free legislation, producing an estimate of the total number of cases averted for each outcome.
All analyses were undertaken using Stata SE version 12.0 (Statacorp, TX).
Sample size considerations
As we used the maximum time span and population available, sample size calculations were redundant. Given the national nature of this evaluation, we estimated that we would have adequate power to detect clinically relevant temporal changes in the outcomes of interest9. A number of studies have previously assessed the impact of smoke-free legislation on low birth weight11,12,13,23,24,25,26. Our approach was comparable to that previously employed in Scotland12. Using data on 757,795 deliveries occurring between 1996 and 2009, this work showed an immediate −9.9% (95% CI −14.2 to −5.2; p < 0.001) drop in low birth weight babies12. Given the longer study period (1995–2011) and the much larger population size (n > 10 million), the current study was expected to have sufficient power to detect a similar reduction in low birth weight babies in England, if present. Earlier studies of the impact of smoke-free laws on SIDS are hampered by their ecological design and these were therefore not suitable to inform deliberations on power considerations for the current study27,46.
Additional Information
How to cite this article: Been, J. V. et al. Impact of smoke-free legislation on perinatal and infant mortality: a national quasi-experimental study. Sci. Rep. 5, 13020; doi: 10.1038/srep13020 (2015).
Supplementary Material
Acknowledgments
We thank the staff at the Office for National Statistics for their help in protocol development and data extraction. We also thank Dr. Valéria Lima Passos PhD and Dr. Rob Elton PhD for statistical advice. Funding: JVB is supported by fellowships from Thrasher Research Fund, Netherlands Lung Foundation, and the International Pediatric Research Foundation. AS is supported by The Commonwealth Fund, a private independent foundation based in New York City; the views presented here are those of the author and not necessarily those of The Commonwealth Fund, its directors, officers, or staff. The study sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Footnotes
Author Contributions J.V.B. co-conceived the study, developed the methods, updated the systematic review, performed and interpreted the analyses, and wrote the paper. D.F.M. developed the methods, supported and interpreted the analyses, and commented on the manuscript. C.M., J.P.P. and C.P.v.S. developed the methods, interpreted the analyses, and commented on the manuscript. A.S. developed the methods, supervised and interpreted the analyses, and commented on drafts of the manuscript. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- US Department of Health and Human Services, The health consequences of smoking-50 years of progress. A report of the Surgeon General. (2014) Available at: http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. (Accessed 22nd May 2015).
- Oberg M., Jaakkola M. S., Woodward A., Peruga A. & Pruss-Ustun A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 377, 139–146 (2011). [DOI] [PubMed] [Google Scholar]
- Leonardi-Bee J., Smyth A., Britton J. & Coleman T. Environmental tobacco smoke and fetal health: systematic review and meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 93, F351–F361 (2008). [DOI] [PubMed] [Google Scholar]
- Leonardi-Bee J., Britton J. & Venn A. Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis. Pediatrics 127, 734–741 (2011). [DOI] [PubMed] [Google Scholar]
- Flenady V. et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet 377, 1331–1340 (2011). [DOI] [PubMed] [Google Scholar]
- Boldo E. et al. Health impact assessment of environmental tobacco smoke in European children: sudden infant death syndrome and asthma episodes. Public Health Rep. 125, 478–487 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan J. E., Clarke A., Doherty K. & Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. CD005992 (2010). [DOI] [PubMed] [Google Scholar]
- Tan C. E. & Glantz S. A. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation 126, 2177–2183 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Been J. V. et al. Effect of smoke-free legislation on perinatal and child health: systematic review and meta-analysis. Lancet 383, 1549–1560 (2014). [DOI] [PubMed] [Google Scholar]
- Nguyen K. H., Wright R. J., Sorensen G. & Subramanian S. V. Association between local indoor smoking ordinances in Massachusetts and cigarette smoking during pregnancy: a multilevel analysis. Tob. Control 22, 184–189 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page R. L. 2nd, Slejko J. F. & Libby A. M. A citywide smoking ban reduced maternal smoking and risk for preterm births: a Colorado natural experiment. J. Womens Health (Larchmt) 21, 621–627 (2012). [DOI] [PubMed] [Google Scholar]
- Mackay D. F., Nelson S. M., Haw S. J. & Pell J. P. Impact of Scotland’s smoke-free legislation on pregnancy complications: retrospective cohort study. PLoS Med. 9, e1001175 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharadwaj P., Johnsen J. V. & Loken K. V. Smoking bans, maternal smoking, and birth outcomes. IZA discussion paper No. 7006. (2012). Available at: http://ftp.iza.org/dp7006.pdf. (Accessed 23rd May 2015).
- Adams E. K. et al. Reducing prenatal smoking: the role of state policies. Am. J. Prev. Med. 43, 34–40 (2012). [DOI] [PubMed] [Google Scholar]
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385, 117–171 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations, The Millennium Development Goals report 2014. (2014). Available at: http://www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf. (Accessed 23rd May 2015)
- World Health Organization, WHO report on the global tobacco epidemic, 2013. Enforcing bans on tobacco advertising, promotion and sponsorship. (2013). Available at: http://www.who.int/tobacco/global_report/2013/en. (Accessed 23rd May 2015).
- World Health Organization & UNICEF, Low birth weight. Country, regional and global estimates 2004. (2004). Available at: http://www.unicef.org/publications/files/low_birthweight_from_EY.pdf. (Accessed 23rd May 2015).
- Sims M., Maxwell R., Bauld L. & Gilmore A. Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction. BMJ 340, c2161 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euro Peristat, European perinatal health report. Health and care of pregnant women and babies in Europe in 2010. (2010). Available at: http://www.europeristat.com/images/doc/Peristat%202013%20V2.pdf. (Accessed 23rd May 2015).
- UNICEF, World Health Organization, World Bank and UN-DESA Population Division, Levels and trends in child mortality. (2013). Available at: http://www.childinfo.org/files/Child_Mortality_Report_2013.pdf. (Accessed 23rd May 2015).
- Biglan A., Ary D. & Wagenaar A. C. The value of interrupted time-series experiments for community intervention research. Prev. Sci. 1, 31–49 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox B., Martens E., Nemery B., Vangronsveld J. & Nawrot T. S. Impact of a stepwise introduction of smoke-free legislation on the rate of preterm births: analysis of routinely collected birth data. BMJ 346, f441 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaral M. The effect of local smoking ordinances on fetal development: evidence from California. (2009). Available at: http://www.pacific.edu/Documents/school-college/economics/smokingban_paper_Amaral.pdf. (Accessed 23rd May 2015).
- Hade E. Analysis of the association between birth outcomes and the Ohio tobacco ban. In: Analyses of the impact of the Ohio smoke-free workplace act. (2011). Available at: http://www.odh.ohio.gov/~/media/ODH/ASSETS/Files/web%20team/features/reportsonsmokefreeworkplaceact.ashx. (Accessed 23rd May 2015)
- Kabir Z. et al. Low birthweight and preterm birth rates 1 year before and after the Irish workplace smoking ban. BJOG 116, 1782–1787 (2009). [DOI] [PubMed] [Google Scholar]
- Markowitz S. The effectiveness of cigarette regulations in reducing cases of sudden infant death syndrome. J. Health. Econ. 27, 106–133 (2008). [DOI] [PubMed] [Google Scholar]
- Kabir Z., Daly S., Clarke V., Keogan S. & Clancy L. Smoking ban and small-for-gestational age births in Ireland. PLoS One 8, e57441 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunyer J. et al. Exposure to second-hand smoke and reproductive outcomes depending on maternal asthma. Eur. Respir. J. 40, 371–376 (2012). [DOI] [PubMed] [Google Scholar]
- Salmasi G., Grady R., Jones J. & McDonald S. D. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 89, 423–441 (2010). [DOI] [PubMed] [Google Scholar]
- McCowan L. M. et al. Spontaneous preterm birth and small for gestational age infants in women who stop smoking early in pregnancy: prospective cohort study. BMJ 338, b1081 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas C. I. et al. Smoking and smoking cessation during early pregnancy and its effect on adverse pregnancy outcomes and fetal growth. Eur. J. Pediatr. 169, 741–748 (2010). [DOI] [PubMed] [Google Scholar]
- Suzuki K. et al. Effect of maternal smoking cessation before and during early pregnancy on fetal and childhood growth. J. Epidemiol. 24, 60–66 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Mohandes A. A., Kiely M., Blake S. M., Gantz M. G. & El-Khorazaty M. N. An intervention to reduce environmental tobacco smoke exposure improves pregnancy outcomes. Pediatrics 125, 721–728 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz S., Adams E. K., Dietz P. M., Kannan V. & Tong V. Smoking policies and birth outcomes: estimates from a new era. NBER working paper No. 17160. (2011). Available at: http://www.nber.org/papers/w17160. (Accessed 23rd May 2015).
- Been J. V., Nurmatov U., van Schayck C. P. & Sheikh A. The impact of smoke-free legislation on fetal, infant and child health: a systematic review and meta-analysis protocol. BMJ Open 3, e002261 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H. et al. The effects of smoke-free legislation on acute myocardial infarction: a systematic review and meta-analysis. BMC Public Health 13, 529 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel R. M. et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N. Engl. J. Med. 372, 331–340 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downard C. D. et al. Maternal cigarette smoking and the development of necrotizing enterocolitis. Pediatrics 130, 78–82 (2012). [DOI] [PubMed] [Google Scholar]
- Antonucci R., Contu P., Porcella A., Atzeni C. & Chiappe S. Intrauterine smoke exposure: a new risk factor for bronchopulmonary dysplasia? J. Perinat. Med. 32, 272–277 (2004). [DOI] [PubMed] [Google Scholar]
- Spiegler J. et al. Influence of smoking and alcohol during pregnancy on outcome of VLBW infants. Z. Geburtsh. Neonatol. 217, 215–219 (2013). [DOI] [PubMed] [Google Scholar]
- Sochaczewska D., Czeszynska M. B., Konefal H. & Garanty-Bogacka B. [Maternal active or passive smoking in relation to some neonatal morphological parameters and complications]. Ginekol. Pol. 81, 687–692 (2010). [PubMed] [Google Scholar]
- Vege A. & Rognum T. O. Use of new Nordic criteria for classification of SIDS to re-evaluate diagnoses of sudden unexpected infant death in the Nordic countries. Acta Paediatr. 86, 391–396 (1997). [DOI] [PubMed] [Google Scholar]
- Corbin T. Investigation into sudden infant deaths and unascertained infant deaths in England and Wales, 1995-2003. Health. Stat. Q. 27, 17–23 (2005). [PubMed] [Google Scholar]
- Winkel B. G. et al. Sudden unexpected death in infancy in Denmark. Scand. Cardiovasc. J. 45, 14–20 (2011). [DOI] [PubMed] [Google Scholar]
- King C., Markowitz S. & Ross H. Tobacco control policies and sudden infant death syndrome in developed nations [published online July 24, 2014]. Health Econ. 10.1002/hec.3090. [DOI] [PubMed] [Google Scholar]
- Lee J. T., Glantz S. A. & Millett C. Effect of smoke-free legislation on adult smoking behaviour in England in the 18 months following implementation. PLoS One 6, e20933 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mons. U. et al. Impact of national smoke-free legislation on home smoking bans: findings from the International Tobacco Control Policy Evaluation Project Europe Surveys. Tob. Control 22, e2–e9 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng K. W., Glantz S. A. & Lightwood J. M. Association between smokefree laws and voluntary smokefree-home rules. Am. J. Prev. Med. 41, 566–572 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazar G. P. et al. Association between being employed in a smoke-free workplace and living in a smoke-free home: evidence from 15 low and middle income countries. Prev. Med. 59, 47–53 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Been J. V., Millett C., Lee J. T., van Schayck C. P. & Sheikh A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections [published online May 28, 2015]. Eur. Respir. J. 10.1183/09031936.00014615. [DOI] [PubMed] [Google Scholar]
- Kalkhoran S. & Glantz S. A. Smoke-free policies: cleaning the air with money to spare. Lancet 383, 1526–1528 (2014). [DOI] [PubMed] [Google Scholar]
- Diepeveen S., Ling T., Suhrcke M., Roland M. & Marteau T. M. Public acceptability of government intervention to change health-related behaviours: a systematic review and narrative synthesis. BMC Public Health 13, 756 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L. et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379, 2151–2161 (2012). [DOI] [PubMed] [Google Scholar]
- Gray R. et al. Contribution of smoking during pregnancy to inequalities in stillbirth and infant death in Scotland 1994-2003: retrospective population based study using hospital maternity records. BMJ 339, b3754 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://www.smokefreeengland.co.uk. (Accessed 26th March 2014).
- http://www.smokefreeengland.co.uk/thefacts/national-compliance-data.html. (Accessed 4th August 2014).
- https://www.gov.uk/government/collections/english-indices-of-deprivation#documents. (Accessed 26th March 2014).
- de Boor C. A Practical Guide To Splines. (Springer, 2001). [Google Scholar]
- Millett C., Lee J. T., Laverty A. A., Glantz S. A. & Majeed A. Hospital admissions for childhood asthma after smoke-free legislation in England. Pediatrics 131, e495–e501 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.