Abstract
Background:
There appears to be very little in the research literature on the safety of thrust joint manipulation (TJM) when applied to the thoracic spine.
Purpose:
To retrospectively analyze all available documented case reports in the literature describing patients who had experienced severe adverse events (AE) after receiving TJM to their thoracic spine.
Data Sources:
Case reports published in peer reviewed journals were searched in Medline (using Ovid Technologies, Inc.), Science Direct, Web of Science, PEDro (Physiotherapy Evidence Database), Index of Chiropractic literature, AMED (Allied and Alternative Medicine Database), PubMed and the Cumulative Index to Nursing and Allied Health (CINHAL) from January 1950 to February 2015.
Study Selection:
Case reports were included if they: (1) were peer-reviewed; (2) were published between 1950 and 2015; (3) provided case reports or case series; and (4) had TJM as an intervention. Articles were excluded if: (1) the AE occurred without TJM (e.g. spontaneous); (2) the article was a systematic or literature review; or (3) it was written in a language other than English or Spanish.
Data Extraction:
Data extracted from each case report included: gender; age; who performed the TJM and why; presence of contraindications; the number of manipulation interventions performed; initial symptoms experienced after the TJM; as well as type of severe AE that resulted.
Results:
Ten cases, reported in 7 case reports, were reviewed. Cases involved females (8) more than males (2), with mean age being 43.5 years (SD=18.73, Range = 17 -71). The most frequent AE reported was injury (mechanical or vascular) to the spinal cord (7/10), with pneumothorax and hematothorax (2/10) and CSF leak secondary to dural sleeve injury (1/10).
Limitations:
There were only a small number of case reports published in the literature and there may have been discrepancies between what was reported and what actually occurred, since physicians dealing with the effects of the AE, rather than the clinician performing the TJM, published the cases.
Conclusions:
Serious AE do occur in the thoracic spine, most commonly, trauma to the spinal cord, followed by pneumothorax. This suggests that excessive peak forces may have been applied to thoracic spine, and it should serve as a cautionary note for clinicians to decrease these peak forces.
Keywords: Adverse events, Manipulation, Thoracic spine, Injury, Chiropractic, Osteopathy, Orthopedic manipulative therapy
Introduction
Spinal manipulation is utilised by physical therapists, chiropractors and other healthcare practitioners to treat a multitude of musculoskeletal disorders, most commonly mechanical back and neck pain, headaches and spinal stiffness.1–6 A significant problem with research into spinal manipulation is that a precise definition is often lacking, and the terms ‘joint manipulation’ and ‘joint mobilisation’ are often used interchangeably as if they are one and the same.7 Many clinicians contend that they are not the same, and without appropriate clarity on this issue, it is impossible to compare and contrast these interventions, their outcomes (benefits) or their associated adverse events [(AEs) risks]. Thrust joint manipulation (TJM) to the spine differs significantly from non-thrust joint mobilisation in that the rate of vertebral joint motion (the speed of the technique) does not allow the patient to prevent its occurrence. Thrust joint manipulation techniques involve the application of high-velocity low-amplitude forces directed to spinal joints with the intent of achieving joint cavitation or an audible pop. Non-thrust spinal mobilisation techniques involve cyclic low-velocity forces through varying amplitudes of motion with no intent to achieve joint cavitation. The safety of TJM to the spine has been an issue of significant debate over the past decade, with much of the focus being on AEs associated with its application to the cervical spine,8–11 and to a lesser extent the lumbar spine.12–14 For the purposes of this article, we define an AE as the sequelae following TJM to the spine that are medium to long term in duration, with moderate to severe symptoms, and of a nature that is serious, distressing and unacceptable to the patient and requires further treatment.11,15,16
There appears to be very little in the research literature on the safety of TJM when applied to the thoracic spine, and indeed it appears that physical therapists may be more comfortable providing it to this area of the spine as opposed to the cervical and lumbar regions.17 Thrust joint manipulation to the thoracic spine has been recommended in the management of patients with mechanical neck pain;18–21 found to provide short-term success in some individuals with shoulder pain;22,23 and also reported to be beneficial in the management of temporomandibular disorders when combined with mobilisation with movement and dry needling.24 While it appears to receive scant attention in the literature, it is evident that there is some risk associated with the application of TJM to the thoracic spine just as there is in the other areas of the spine. Clinicians are encouraged to appropriately screen their patients for the presence of any contraindications and/or precautions when considering TJM to any area of the spine, and it should be remembered that all clinical trials reporting on the benefits of TJM to the spine have excluded patients with known contraindications and precautions to manipulation.
Whenever TJM is deemed to be appropriate for a patient's presenting musculoskeletal condition, the clinician should determine the safety of the technique by identifying preexisting conditions that might indicate a patient's risk for an AE. Contraindications (Table 1) and precautions (Table 2) to the application of TJM in the thoracic spine have been identified to assist clinicians with decision-making.25 Thrust joint manipulation should never be performed when contraindications or precautions are present, suggesting that risks for an AEs are unacceptably high for that patient.
Table 1. Absolute contraindications to performing thrust joint manipulation (TJM) to the thoracic spine.
| Bony issues |
| Any pathology that may have led to bony compromise |
| Tumour, e.g. metastatic disease |
| Infection, e.g. tuberculosis, osteomyelitis |
| Metabolic, e.g. osteomalacia, osteoporosis |
| Congenital, e.g. dysplasias, congenital fusions |
| Iatrogenic, e.g. long-term corticosteroid medication, surgical fusions, recent surgery |
| Inflammatory, e.g. rheumatoid arthritis, ankylosing spondylitis, acute soft tissue injury, connective tissue disease, synovial cysts |
| Traumatic, e.g. fracture, dislocation, ligamentous rupture, instability |
| Neurological issues |
| Any pathology that may affect the neurological system |
| Acute cervical, thoracic or lumbar myelopathy |
| Spinal cord compression |
| Cauda equina syndrome |
| Nerve root compression with increasing neurological deficit, bilateral hyper-reflexia/sensory loss |
| Sudden vomiting/nausea/vertigo |
| Vascular issues |
| Any pathology that may have led to vascular compromise |
| Diagnosed vertebrobasilar insufficiency or cervical artery abnormalities |
| Aortic aneurysm |
| Bleeding diatheses, e.g. haemophilia, anticoagulant therapy |
| Angina pectoris |
| Untreated cardiac insufficiency, untreated cardiac dysthymias |
| Acute abdominal pain with guarding |
| Clinical issues |
| Any matter that may increase the risk of harm to the patient |
| Lack of adequate subjective and objective examination by clinician |
| Lack of diagnosis |
| Lack of skill/expertise by clinician |
| Lack of consent from the patient |
Table 2. Relative precautions to performing thrust joint manipulation (TJM) to the thoracic spine.
| Adverse reaction to previous TJM |
| Inflammatory joint processes |
| Minor osteoporosis |
| Disc herniation and disc protrusion |
| Spondylolisthesis |
| Hypermobility or ligamentous laxity |
| Arterial calcification |
| Arterial hypertension |
| Serious degenerative joint diseases |
| Growing children |
| Serious kyphosis and scoliosis |
| Herpes zoster on the thoracic spine |
| Vertigo |
| Systemic infections |
| Psychological dependence upon manipulation |
| Pain with a psychological overlay |
| No change or worsening of symptoms after multiple manipulations |
While suggestions have been made to guide clinical reasoning and reduce the risk of AE, there is evidence that unwanted side effects are quite common following TJM to the thoracic spine. For the purposes of this article, we define an unwanted side effect as short term, mild in nature, non-serious, transient and reversible consequences of the treatment such as increase in pain, headache, discomfort and fatigue.11,15,16 In a study involving 465 patients receiving TJM to one or more areas of their spine, 283 (60.9%) reported at least one post treatment side effect.26 The most commonly reported side effects were headache (19.8%), stiffness (19.5%), worsening of presenting symptoms (15.2%), radiating discomfort (12.1%) and fatigue (12.1%),26 and the number and type of side effects were comparable to previously reported studies.27–29 Of the 930 manipulations provided to the 465 patients, the cervical spine was targetted most frequently (38.6%), followed by the thoracic spine (25.7%), lumbar spine (23.6%) and sacroiliac joint (12.1%). In a more recent clinical trial comparing TJM to the cervical spine versus the thoracic spine in patients with acute neck pain, Puentedura et al.16 reported a higher incidence of side effects for patients receiving TJM to the thoracic spine (8 out of 10) versus TJM to the cervical spine (1 out of 14) after the first treatment. One reason for this may have been the number of TJM techniques provided to the respective spinal regions. Patients in the cervical TJM group received an average of two thrusts (one rotary technique to each side of the neck), whereas the thoracic TJM group received an average of five thrusts (three different techniques with two being repeated when cavitation did not occur).
Thrust joint manipulation techniques to the thoracic spine have been shown to involve greater maximum instantaneous rates of loading to the spinal motion segments when compared to the lumbar spine, with one study reporting it to be 1.7–1.8 times higher.30 In that study, maximum peak load through the thoracic spine was 562.68 N (126.5 lbs-force) recorded during a posterior to anterior thrust technique, whereas it was 441.11 N (99.2 lbs-force) for side-lying lumbar rotation.30 Sran et al.31 conducted a biomechanical study to quantify the failure load of mid-thoracic vertebrae under posterior to anterior load, and found a mean in vitro failure load of 479 N (range was 200–728 N). This may raise some concerns about the strength and depth of TJM techniques in the thoracic spine. In another study measuring chest compressions during typical and maximal effort by chiropractors performing thoracic manipulations, researchers found attainment of 1.8 and 4.5% of total chest depth, respectively.32 This was found to be only 22.7% of the compression required for greater than 10% risk of an Abbreviated Injury Scale (AIS) level 1 injury.32 Findings such as this may account for the clinical observations of increased post treatment side effects following TJM to the thoracic spine, and lead us to reconsider the relative safety of TJM to the thoracic spine.
After an extensive search, the authors were unable to find any published systematic review of AEs following TJM to the thoracic spine. Accordingly, we set out to perform a systematic review and retrospectively analyse all available documented case reports in the literature describing patients who had experienced severe AE after receiving TJM to their thoracic spine.
Methods
Case reports published in peer reviewed journals involving AE following TJM to the thoracic spine were found by searching Medline (using OVID), Science Direct, Web of Science, PEDro (Physiotherapy Evidence Database), Index of Chiropractic literature, AMED (Allied and Alternative Medicine Database), PubMed and the Cumulative Index to Nursing and Allied Health (CINHAL) from January 1950 to February 2015. Initial search terms included any combination of the following: thoracic manipulation, adjustment, chiropractic, manual therapy, physical therapy, physiotherapy, osteopathy, epidural haematoma, pneumothorax, safety, AE, side effect, injury and risk. In addition we tracked citations from articles.
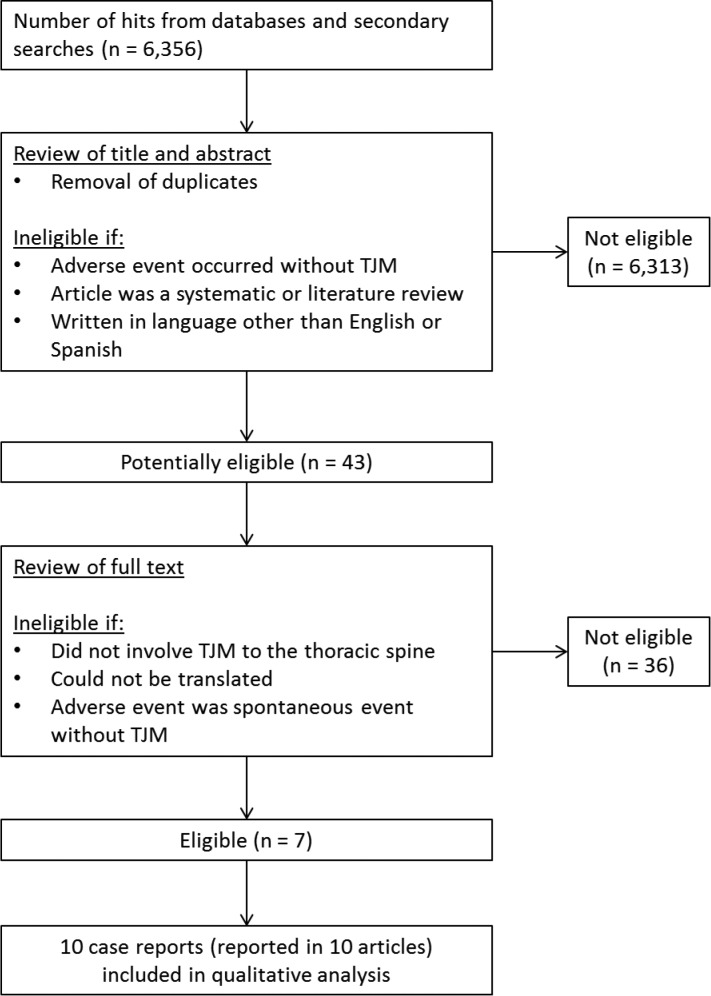
Titles and abstracts of articles identified with search terms were screened by the two authors. Articles were included if they: (1) were peer-reviewed; (2) were published between 1950 and 2015; (3) provided case reports or case series; and (4) had TJM as an intervention. Articles were excluded if: (1) the AE occurred without TJM (e.g. spontaneous); (2) the article was a systematic or literature review; or (3) it was written in a language other than English or Spanish. See Fig. 1 for a summary of the article retrieval and review process.
Figure 1.
Retrieval and review process.
Results
Demographics
A total of 10 cases, reported in seven articles, were analysed for this systematic review33–39 (Table 3). Language translation was not required in any of the cases. The 10 cases involved two males and eight females. The mean age of the patients was 43.5 years (SD = 18.73, Range = 17–71 years).
Table 3. The 10 cases of serious adverse events (AEs) reported in seven published articles.
| No. | Authors and year | Age (years), sex | Interval to symptom onset | Practitioner | Thoracic level manipulated | AE |
| 1 | Ruelle et al. (1999)35 | 64, F | 2 hours | Chiropractor | Lumbar and thoracic spine | Acute epidural haematoma T9–11 |
| 2 | Oppenheim et al. (2005)39 | 60, F | Not known | Chiropractor | Upper thoracic spine | T4–5 collapse; cord compression |
| 3 | 56, F | Not known | Chiropractor | Upper thoracic spine | T4 pathology; epidural tumour | |
| 4 | 71, F | Not known | Chiropractor | Upper thoracic spine | T4 fracture; lung CA | |
| 5 | 32, M | Not known | Chiropractor | Middle thoracic spine | Thoracic syrinx, swollen cord | |
| 6 | Lopez-Gonzalez and Peris-Celda (2011)33 | 45, F | 2 hours | Chiropractor | Middle thoracic spine | Traumatic T8–T9 disc herniation; complete T6 level paraplegia secondary to spinal cord ischaemia |
| 7 | Lee et al. (2011)34 | 38, F | 4 hours | Chiropractor | Cervical and upper thoracic spine | Acute epidural haematoma T1–7 |
| 8 | Struewer et al. (2013)38 | 17, M | 2 days | Osteopath | Middle thoracic spine | Large left hematothorax |
| 9 | Masneri et al. (2007)37 | 20, F | 24 hours | Lay person | Middle thorax | Right pneumothorax |
| 10 | Donovan et al. (2007)36 | 32, F | 2 weeks | Physical Therapist | Cervical and upper thoracic spine | CSF leak and spontaneous intracranial hypotension from dural sleeve tear C8–T5 |
Adverse events
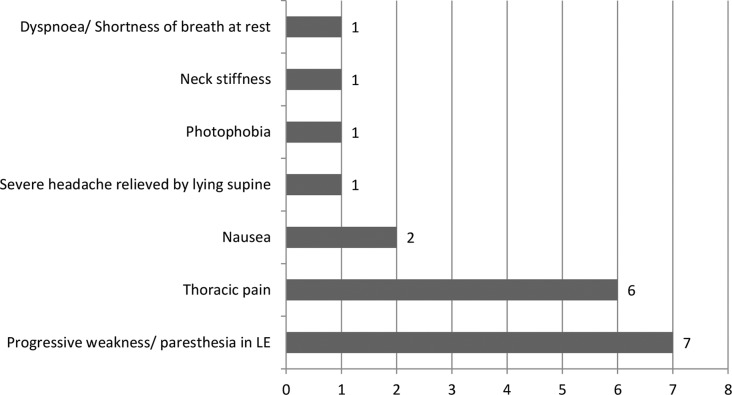
The most frequent AE reported was injury (mechanical or vascular) to the spinal cord (7 out of the 10 cases). The next most reported AE was pneumothorax and hematothorax (2 out of 10 cases) and cerebrospinal fluid (CSF) leak secondary to dural sleeve injury was reported in the final case. The most common post-manipulation symptoms described were progressive weakness/paraesthesia in the lower extremities (n = 7), thoracic pain (n = 6), nausea (n = 2) and single incidences of shortness of breath/dyspnoea at rest, neck stiffness, photophobia and severe headache relieved by lying supine (Fig. 2).
Figure 2.
Frequency of symptoms associated with adverse events (AEs) following thrust joint manipulation (TJM) to the thoracic spine.
Chiropractors were involved in the majority of injuries following TJM to the thoracic spine with 70% (n = 7) of the cases analysed. An osteopathic physician, physical therapist and a lay person were involved in the remaining 30% (n = 3) of the cases. All of the cases were published by neurosurgery and emergency medicine physicians providing patient care following the AE, and there was insufficient information in the case reports to determine if the TJM provided to the thoracic spine was appropriate, or if there were any contraindications or precautions to TJM in the thoracic spine that could have alerted the clinician providing the TJM to increased risks of AE and hence prevented them.
Discussion
There were a surprisingly small number of case reports involving serious AE following TJM to the thoracic spine reported in the literature. Rather than infer that serious AE following TJM to the thoracic spine are extremely rare, it is more likely that such events are under-reported. The worldwide web has many pages devoted to listings of people who have suffered harm (in many cases death) from TJM, and while the majority of these reports involve TJM to the cervical spine, there are many involving TJM to the thoracic and lumbar spines also. The results of this review indicate that there is a need for more accurate and full reporting of harms associated with TJM to the thoracic spine.
The most frequently reported AE following TJM to the thoracic spine involved acute trauma to the spinal cord (Cases 1–7 in Table 3). It is presumed that the TJM technique may have been given with such force that it either bruised the cord, fractured a thoracic vertebra or herniated a thoracic disc which then led to damage to the cord. Three of the most commonly used TJM techniques in the thoracic spine include the prone posterior-to-anterior thrust (Fig. 3), the supine thrust (Fig. 4) and the seated traction thrust (Fig. 5). As previously reported, there are reports of maximum peak force loads exceeding 125 lb-force to the thoracic spinal motion segments,30 and therefore, clinicians should be wary of the maximum applied forces they use when administering these techniques. Closely monitoring the amount of force applied during the performance of a TJM requires skill and clinical experience to ensure that loads do not exceed the tolerance of the vertebrae and lead to unwanted side effects at best, and serious AEs at worst.
Figure 3.
Performance of the prone posterior-to-anterior thrust joint manipulation (TJM) to the thoracic spine.
Figure 4.
Performance of the supine thrust joint manipulation (TJM) to the thoracic spine.
Figure 5.
Performance of the seated traction thrust joint manipulation (TJM) to the thoracic spine.
As well as possessing skill in the administration of the TJM technique, the clinician should be observant and able to recognise any signs indicating that their patient may be at increased risk of experiencing a serious AE. This would involve screening for any contraindications and precautions to TJM in the thoracic spine (Table 1). For the cases reported in this review, there was insufficient information about each patient to determine if there may have been some underlying bony and/or neurological issues, which placed them at greater risk of AE following TJM. It is possible that the clinicians may have failed to recognise signs of these underlying issues, but equally, it is possible that the patients presented without such signs for the clinicians to detect. The inability to recognise such signs may be attributed to the lack of reliable and valid screening tools, as well as poor history taking and insufficient clinical reasoning. However, it is also possible that clinicians had no intent to screen for contraindications due to lack of knowledge, poor clinical judgement or carelessness. Regardless of the evidence, or lack thereof, it is the responsibility of the clinician to perform screening examinations and clearly document their use to reduce legal risk if an AE was to occur with TJM to the thoracic spine.40–43
>With uncertainty regarding screening tools, clinicians must use other strategies (e.g. red flags) for decision-making when deciding whether or not to use TJM.40 The most common preexisting conditions were likely to be metabolic pathologies such as osteopenia or osteoporosis. These conditions are clear contraindications to TJM and should have been easily identifiable through a detailed patient history. With the lack of accurate screening tools, it is prudent for the clinician to perform a thorough history to ensure patient safety.40 Also, with the understanding that TJM techniques to the thoracic spine involve higher peak forces, clinicians should use not only clinical reasoning to determine whether or not TJM is appropriate and safe, but they should also consider their own skill level, the preferences of the referring provider and the demeanour and goals of the patient.40,41
Demographics of the patient population were comparable to those reported in previous literature regarding AE for TJM to the cervical spine.44–46 In our review, the majority of the AEs were severe and irreversible. However, according to current literature, transient events (unwanted side effects) are more common than severe AE.26,47 In fact, transient side effects are reported to occur in 60.9% of all TJM.26,27 The discrepancy in representation of severity is likely because transient side effects tend to be under-reported. Severe complications are more likely to require medical attention and, therefore, be documented.48 Additionally, the purpose of this review was to analyse cases with severe AE rather than transient side effects following TJM to the thoracic spine.
The distribution of clinicians in our review mirrors those described by both Di Fabio,44 Ernst45 and Puentedura et al.11 Chiropractors were found to be involved in the majority of severe AE resulting from TJM to the thoracic spine. This result may be simply because TJM is the most common treatment intervention used in the practice of chiropractic and is performed with greater frequency by chiropractors than any other clinician.
Limitations
There are several limitations of our review that need to be acknowledged. Despite a thorough and systematic search for relevant cases, we were only able to find a very small number of cases in a smaller number of published reports. Our search may not have been exhaustive due to exclusion prior to 1950 and use of limited search engines. Other factors that may have contributed to our limited findings include the following: a paucity of reports written by clinicians regarding AE after TJM to the thoracic spine; and stipulations of settlements on litigated cases may not have allowed information regarding those cases to be made public.
Based on the results of this review, we propose that cases regarding AE to TJM in the thoracic spine should provide more standardised information. This should include detailed information regarding the manipulation technique, as proposed by Mintken et al.7 The six categories suggested include: (1) rate of force application; (2) location in range of available movement; (3) direction of force; (4) target of force; (5) relative structural movement and (6) patient position.7 Additionally, cases should include: total number of TJM techniques performed; for what condition the TJM was performed; which clinician performed the TJM; and a description of examination procedures used by the clinician to rule out contraindications and precautions.
Conclusion
This review showed that serious AEs do occur in the thoracic spine. The most commonly reported AE involved trauma to the spinal cord, followed by pneumothorax. This suggests that excessive peak forces may have been applied to thoracic spine, and it should serve as a cautionary note for clinicians to work on their TJM skills to decrease these peak forces. Finally, we recommend the performance of a thorough examination and the use of sound clinical reasoning as a means whereby the likelihood of AE's may be mitigated. Clinicians should always endeavour to reduce risks associated with TJM and improve patient safety.
Disclaimer Statements
Contributors Emilio Puentedura provided the research proposal, research design, conducted the systematic review, data appraisal and analysis, writing and editing of the manuscript. William O'Grady assisted with the systematic review, data appraisal and analysis, contributed to the writing and editing of the manuscript.
Funding There is no funding for this article.
Conflicts of interest The authors report no conflicts-of-interests.
Ethics approval The protocol for this study was reviewed and deemed excluded from IRB review (exempt) by the UNLV Office for the Protection of Human Research Subjects.
References
- 1.Kuczynski JJ, Schwieterman B, Columber K, Knupp D, Shaub L, Cook CE. Effectiveness of physical therapist administered spinal manipulation for the treatment of low back pain: a systematic review of the literature. Int J Sports Phys Ther. 2012;7(6):647–62. [PMC free article] [PubMed] [Google Scholar]
- 2.Goertz CM, Pohlman KA, Vining RD, Brantingham JW, Long CR. Patient-centered outcomes of high-velocity, low-amplitude spinal manipulation for low back pain: a systematic review. J Electromyogr Kinesiol. 2012;22(5):670–91. doi: 10.1016/j.jelekin.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Rodine RJ, Vernon H. Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the Neck Disability Index. J Can Chiropr Assoc. 2012;56(1):18–28. [PMC free article] [PubMed] [Google Scholar]
- 4.Michaleff ZA, Lin CW, Maher CG, van Tulder MW. Spinal manipulation epidemiology: systematic review of cost effectiveness studies. J Electromyogr Kinesiol. 2012;22(5):655–62. doi: 10.1016/j.jelekin.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Vernon H. The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials. Cephalalgia. 2003;23(6):479–480. doi: 10.1046/j.1468-2982.2003.05551.x. [author reply 471–80] [DOI] [PubMed] [Google Scholar]
- 6.Bronfort G, Assendelft WJ, Evans R, Haas M, Bouter L. Efficacy of spinal manipulation for chronic headache: a systematic review. J Manipulative Physiol Ther. 2001;24(7):457–66. [PubMed] [Google Scholar]
- 7.Mintken PE, Derosa C, Little T, Smith BA. Model for standardizing manipulation terminology in physical therapy practice. J Man Manip Ther. 2008;16(1):50–6. doi: 10.1179/106698108790818567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivett DA. Adverse events and the vertebral artery: can they be averted? Man Ther. 2006;11(4):241–2. doi: 10.1016/j.math.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Tuchin P. A replication of the study ‘adverse effects of spinal manipulation: a systematic review’. Chiropr Man Therap. 2012;20(1):30. doi: 10.1186/2045-709X-20-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sweeney A, Doody C. Manual therapy for the cervical spine and reported adverse effects: a survey of Irish manipulative physiotherapists. Man Ther. 2010;15(1):32–6. doi: 10.1016/j.math.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Puentedura EJ, March J, Anders J, Perez A, Landers MR, Wallmann HW et al. Safety of cervical spine manipulation: are adverse events preventable and are manipulations being performed appropriately? A review of 134 case reports. J Man Manip Ther. 2012;20(2):66–74. doi: 10.1179/2042618611Y.0000000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boucher P, Robidoux S. Lumbar disc herniation and cauda equina syndrome following spinal manipulative therapy: a review of six court decisions in Canada. J Forensic Leg Med. 2014;22:159–69. doi: 10.1016/j.jflm.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 13.Lisi AJ, Holmes EJ, Ammendolia C. High-velocity low-amplitude spinal manipulation for symptomatic lumbar disk disease: a systematic review of the literature. J Manipulative Physiol Ther. 2005;28(6):429–42. doi: 10.1016/j.jmpt.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Oliphant D. Safety of spinal manipulation in the treatment of lumbar disk herniations: a systematic review and risk assessment. J Manipulative Physiol Ther. 2004;27(3):197–210. doi: 10.1016/j.jmpt.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 15.Carnes D, Mullinger B, Underwood M. Defining adverse events in manual therapies: a modified Delphi consensus study. Man Ther. 2010;15(1):2–6. doi: 10.1016/j.math.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Puentedura EJ, Landers MR, Cleland JA, Mintken PE, Huijbregts P, Fernandez-de-Las-Penas C. Thoracic spine thrust manipulation versus cervical spine thrust manipulation in patients with acute neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(4):208–20. doi: 10.2519/jospt.2011.3640. [DOI] [PubMed] [Google Scholar]
- 17.Puentedura EJ, Reilly S, Slaughter R, Ventura E. Utilization of spinal manipulation: a survey study. Las Vegas: University of Nevada Las Vegas; 2015. [Google Scholar]
- 18.Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10(2):127–35. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Phys Ther. 2007;87(4):431–40. doi: 10.2522/ptj.20060217. [DOI] [PubMed] [Google Scholar]
- 20.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87(1):9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 21.Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90(9):1239–50. doi: 10.2522/ptj.20100123. [DOI] [PubMed] [Google Scholar]
- 22.Mintken PE, Cleland JA, Carpenter KJ, Bieniek ML, Keirns M, Whitman JM. Some factors predict successful short-term outcomes in individuals with shoulder pain receiving cervicothoracic manipulation: a single-arm trial. Phys Ther. 2010;90(1):26–42. doi: 10.2522/ptj.20090095. [DOI] [PubMed] [Google Scholar]
- 23.Rhon DI, Boyles RE, Cleland JA, Brown DL. A manual physical therapy approach versus subacromial corticosteroid injection for treatment of shoulder impingement syndrome: a protocol for a randomised clinical trial. BMJ Open. 2011;1(2):e000137. doi: 10.1136/bmjopen-2011-000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez-Iglesias J, Cleland JA, Neto F, Hall T, Fernandez-de-las-Penas C. Mobilization with movement, thoracic spine manipulation, and dry needling for the management of temporomandibular disorder: a prospective case series. Physiother Theory Pract. 2013;29(8):586–95. doi: 10.3109/09593985.2013.783895. [DOI] [PubMed] [Google Scholar]
- 25.Gatterbauer A. Contraindications in osteopathy. Vienna: Vienna School of Osteopathy, Danube University Krem; 2009. [Google Scholar]
- 26.Cagnie B, Vinck E, Beernaert A, Cambier D. How common are side effects of spinal manipulation and can these side effects be predicted? Man Ther. 2004;9(3):151–6. doi: 10.1016/j.math.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Senstad O, Leboeuf-Yde C, Borchgrevink C. Frequency and characteristics of side effects of spinal manipulative therapy. Spine (Phila Pa 1976) 1997;22(4):435–440. doi: 10.1097/00007632-199702150-00017. [discussion 431–40] [DOI] [PubMed] [Google Scholar]
- 28.Leboeuf-Yde C, Hennius B, Rudberg E, Leufvenmark P, Thunman M. Side effects of chiropractic treatment: a prospective study. J Manipulative Physiol Ther. 1997;20(8):511–5. [PubMed] [Google Scholar]
- 29.Barrett AJ, Breen AC. Adverse effects of spinal manipulation. J R Soc Med. 2000;93(5):258–9. doi: 10.1177/014107680009300511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gudavalli MR. Instantaneous rate of loading during manual high-velocity, low-amplitude spinal manipulations. J Manipulative Physiol Ther. 2014;37(5):294–9. doi: 10.1016/j.jmpt.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Sran MM, Khan KM, Zhu Q, McKay HA, Oxland TR. Failure characteristics of the thoracic spine with a posteroanterior load: investigating the safety of spinal mobilization. Spine (Phila Pa 1976) 2004;29(21):2382–8. doi: 10.1097/01.brs.0000143110.59837.f2. [DOI] [PubMed] [Google Scholar]
- 32.Stemper BD, Hallman JJ, Peterson BM. An experimental study of chest compression during chiropractic manipulation of the thoracic spine using an anthropomorphic test device. J Manipulative Physiol Ther. 2011;34(5):290–6. doi: 10.1016/j.jmpt.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Lopez-Gonzalez A, Peris-Celda M.Acute paraplegia after chiropraxis Eur Spine J. 201120Suppl 2):S143–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee TH, Chen CF, Lee TC, Lee HL, Lu CH. Acute thoracic epidural hematoma following spinal manipulative therapy: case report and review of the literature. Clin Neurol Neurosurg. 2011;113(7):575–7. doi: 10.1016/j.clineuro.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 35.Ruelle A, Datti R, Pisani R. Thoracic epidural hematoma after spinal manipulation therapy. J Spinal Disord. 1999;12(6):534–6. [PubMed] [Google Scholar]
- 36.Donovan JS, Kerber CW, Donovan WH, Marshall LF. Development of spontaneous intracranial hypotension concurrent with grade IV mobilization of the cervical and thoracic spine: a case report. Arch Phys Med Rehabil. 2007;88(11):1472–3. doi: 10.1016/j.apmr.2007.08.111. [DOI] [PubMed] [Google Scholar]
- 37.Masneri DA, Helphenstine JS, Masneri SM, Miller MA, Levsky ME. Trauma-induced pneumothorax after “bear-hug back crack” home remedy: attempted spinal manipulation by a layperson. J Am Osteopath Assoc. 2007;107(9):411–3. [PubMed] [Google Scholar]
- 38.Struewer J, Frangen TM, Ziring E, Hinterseher U, Kiriazidis I. Massive hematothorax after thoracic spinal manipulation for acute thoracolumbar pain. Orthop Rev. 2013;5(3):e27. doi: 10.4081/or.2013.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oppenheim JS, Spitzer DE, Segal DH. Nonvascular complications following spinal manipulation. Spine J. 2005;5(6):660–666. doi: 10.1016/j.spinee.2005.08.006. [discussion 666–67] [DOI] [PubMed] [Google Scholar]
- 40.Childs JD, Flynn TW, Fritz JM, Piva SR, Whitman JM, Wainner RS et al. Screening for vertebrobasilar insufficiency in patients with neck pain: manual therapy decision-making in the presence of uncertainty. J Orthop Sports Phys Ther. 2005;35(5):300–6. doi: 10.2519/jospt.2005.35.5.300. [DOI] [PubMed] [Google Scholar]
- 41.Kerry R, Taylor AJ, Mitchell J, McCarthy C, Brew J. Manual therapy and cervical arterial dysfunction, directions for the future: a clinical perspective. J Man Manip Therapy. 2008;16(1):39–48. doi: 10.1179/106698108790818620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kerry R, Taylor AJ, Mitchell J, McCarthy C. Cervical arterial dysfunction and manual therapy: a critical literature review to inform professional practice. Man Ther. 2008;13(4):278–88. doi: 10.1016/j.math.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 43.Thomas LC, Rivett DA, Attia JR, Parsons M, Levi C. Risk factors and clinical features of craniocervical arterial dissection. Man Ther. 2011;16(4):351–6. doi: 10.1016/j.math.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 44.Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79(1):50–65. [PubMed] [Google Scholar]
- 45.Ernst E. Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 1995-2001. Med J Aust. 2002;176(8):376–80. doi: 10.5694/j.1326-5377.2002.tb04459.x. [DOI] [PubMed] [Google Scholar]
- 46.Ernst E. Adverse effects of spinal manipulation: a systematic review. J R Soc Med. 2007;100(7):330–8. doi: 10.1258/jrsm.100.7.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thiel HW, Bolton JE, Docherty S, Portlock JC. Safety of chiropractic manipulation of the cervical spine: a prospective national survey. Spine. 2007;32(31):2375–8. doi: 10.1097/BRS.0b013e3181557bb1. [DOI] [PubMed] [Google Scholar]
- 48.Ernst E. Prospective investigations into the safety of spinal manipulation. J Pain Symptom Manage. 2001;21(3):238–42. doi: 10.1016/s0885-3924(00)00262-1. [DOI] [PubMed] [Google Scholar]