Abstract
In order to elucidate the prevalence of individual complications and its relation to the age of patients and to the duration of diabetes in Korean diabetics, the authors observed 1442 diabetic patients (816 males and 626 females, with the age range 11 to 86) who were treated at the Chonnam University Hospital from 1982 to 1986.
The results were as follows:
-
1) The overall prevalence of the diabetic complication was 38.6%, and prevalence of age group under 20 was 31%, and 30%, 24%, 31%, 45% and 49% for 3rd, 4th, 5th, 6th and over 6th decade, respectively. An increase in incidence after 40 years of age was noted.
Among all complications, cardiovascular complication (25.7%) had the highest incidence while others were in the following order neuropathy (24.2%), retinopathy (24.0%), nephropathy (15.5%), infection (10.5%), and acute diabetic coma (2.1%). The prevalence of complication was not significantly different in sexes, however, increasing prevalence was noted after 40 years of age.
2) In neuropathy, peripheral type was the most common, and background retinopathy was frequently observed. Proliferative diabetic retinopathy was reported in 22 cases from the total of 26 cases of retinopathy in patients over 40 years of age. Seventy percent of patients with nephropathy had proteinuria with no significant in BUN and creatinine levels; and the dominant groups was males over 40 years of age.
3) Hypertension was the most common cardiovascular complication with no gender difference, while atherosclerosis and cerebral thrombosis were frequently observed in males over 40 years of age. Foot gangrene was seen in all age groups but it was especially prevalent in males in their sixties.
4) Among infectious complications, pulmonary tuberculosis had the highest frequency (21.6%), and skin infection (19.2%), and urinary tract infection (17.4%) were common complications; also emphysematous pyelonephritis was found in 2 cases.
These results suggest that chronic diabetic complications relate to the duration of the disease and to the age of patients. The prevalence rate of diabetic complications should be evaluated considering factors such as racial and socioeconomic conditions, and possible risk factors for individual complications.
With the clinical use of insulin and antibiotics, mortality from acute diabetic complications, such as coma or infections, showed significant decrease in contrast to the increasing prevalence of late complications which became the major causes of fatality in diabetics. Although these chronic complications were rising, determination of the exact prevalence in the population was difficult and varied in every report due to their occurrence in various combinations.
This study was performed to elucidate (1) the prevalence of individual complication and (2) its relation to the age of patients and (3) its relation to the duration of diabetes in korean diabetics.
Keywords: Prevalence of diabetic complications, Neuropathy, Retinopathy, Nephropathy, Cardiovascular complications, Infections, Diabetic coma
MATERIALS AND METHODS
The study was carried on 1442 diabetic patients [816 males and 626 females; age range 11 to 86 (Table 1)], and male to female ratio of 1.3:1 who were treated at the Chonnam University Hospital from 1982 to 1986.
Table 1.
Diabetic Subjects and Prevalence of Complications
| Sex | Age (years)
|
Total | |||||
|---|---|---|---|---|---|---|---|
| – 19 | 20 – 29 | 30 – 39 | 40 – 49 | 50 – 59 | 60 – | ||
| Male | 19 (2) | 30 (11) | 96 (17) | 251 (75) | 260 (111) | 160 (74) | 816 (290) |
| (35.5%) | |||||||
| Female | 7 (6) | 34 (8) | 59 (20) | 155 (51) | 239 (113) | 132 (69) | 626 (267) |
| (42.7%) | |||||||
|
| |||||||
| Total | 26 (8) | 64 (19) | 155 (37) | 406 (126) | 499 (224) | 292 (143) | 1,442 (557) |
| (31%) | (30%) | (24%) | (31%) | (45%) | (49%) | (38.6%) | |
Number in parentheses show prevalence of complications
Neuropathy was determined by clinical manifestations, Shellong test, and the changes in heart rate in response to forced respiration. Retinopathy was defined by fundoscopic examination and fluorescein retinal angiography. Furthermore, nephropathy, except patients with severe systemic disease or urinary tract infections, was determined by proteinuria and abnormal increase in serum BUN and creatinine levels. Infectious disease was confirmed on the basis of peripheral blood findings, radiological findings, as well as, bacteriological culture study. Cardiovascular complications were determined by clinical manifestations, physical findings, and diagnostic tests.
RESULTS
The prevalence for the diabetic complication was 38.6% (Table 1) in all patient group age distribution of 31% for under 20 and 30%, 24%, 31%, 45% and 49% for 3rd, 4th, 5th, 6th and over 6th decade, respectively. There was a tendency of increasing incidence after 40 years of age.
Among the total complications, cardiovascular complication was most prevalent with incidence of 25.7% and others in the following order of neuropathy (24.2%), retinopathy (24.0%), nephropathy (15.5%), infection (10.5%) and acute diabetic coma (2.1%) (Fig. 1).
Fig. 1.
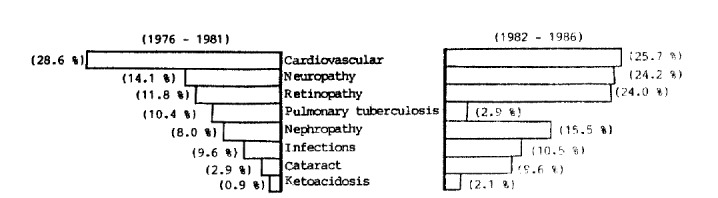
Comparison of the prevalence of diabetic complications in two study periods.
There was no significant difference in prevalence of diabetic complications between male and female (Table 1).
In neuropathy, peripheral type was the most common complication and background retinopathy was frequently observed in diabetic retinopathy. Proliferative diabetic retinopathy was noted in 22 cases of 26 cases in patients over 40 years of age. Seventy percent of patients with nephropathy had proteinuria despite of normal BUN and creatinine levels, and the majority of patients were distributed in males over 40 years of age.
Hypertension was the most common cardiovascular complication in both genders, while atherosclerosis and cerebral thrombosis tended to be present in males over 40 years of age. Foot gangrene appeared in all age groups and most prevalent males in their sixties.
Among infectious diseases, pulmonary tuberculosis showed the highest frequency (21.6%) and skin infection (19.2%) and urinary tract infection (17.4%) were common, also emphysematous pyelonephritis was found in 2 cases.
The duration of diabetes for each major complications is shown in Table 6. Prevalence of diabetic complications increased parallely with the duration of the illness. The mean duration of diabetes for cardiovascular complication was 5.89 years and neuropathy with 5.96 years while retinopathy 7.14 years and nephropathy 7.9 years, which are rather longer than cardiovascular complication or neuropathy (Fig. 3).
Table 6.
The Relation Between Prevalence of Complications and the Durations of Diabetes
| Duration of diabetes (years)
|
|||
|---|---|---|---|
| Under 4 | 5–9 | Over 10 | |
| Neuropathy | 200/1,146 (17.5%) | 75/186 (40.3%) | 70/110 (63.6%) |
| Retinopathy | 155/1,146 (13.5%) | 57/186 (30.6%) | 61/110 (55.5%) |
| Nephropathy | 52/1,146 (4.5%) | 33/186 (17.7%) | 44/110 (40.0%) |
| Cardiovascular Complications | 121/1,146 (10.6%) | 50/186 (26.9%) | 55/110 (50.0%) |
Fig. 3.
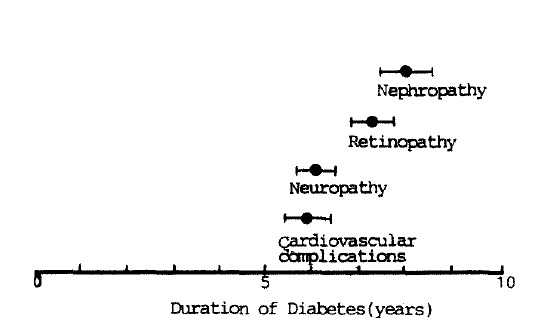
Mean duration of diabetes in various complications (Mean ± SE).
Occurrence of neuropathy in combination with retinopathy was the most common diabetic complication as evidenced by 121 cases of retinopathy in conjunction with nephropathy from a total of 291 cases. All three complications appearing in one patient, was noted in 54 cases.
DISCUSSION
Diabetic neuropathy as well as macroangiopathy appeared at various clinical stages of diabetes mellitus1,2), therefore, the prevalence may be varied depending on the criteria of diagnosis. In these authors’ study, neuropathy (which was defined with definite clinical manifestations, positive Schellong test, and cardiac beat changes in response to deep respiration) was observed in 355 cases with prevalence of 24.6% which was somewhat higher from those in other Asian countries3).
It is well known that peripheral neuropathy is the most common form of diabetic neuropathy4) and this was confirmed in this study with prevalence of 83.4%. Prevalence of neuropathy reflected the duration of diabetes, i.e., under four years it was 17.5%, and for over 5 years-48.9%. These data showed an increase in prevalence according to duration of the illness as reported by others5,6).
The incidence of retinopathy differed diagnosed either by direct ophthalmoscopic examinations of fluorescein retinal angiography7), and its tendency was to increase with age and with the duration of diabetes. In this study, based on a large number of diabetic patients who were initially free of complications, cumulative incidence of diabetic retinopathy was as 34.5% after 20 years later10). In this study, the prevalence of diabetic retinopathy was 22.5% and it was more frequently observed with increased duration of the illness, especially after 5 years and it had higher incidence as compared to these authors’ previous study (Fig. 4).
Fig. 4.
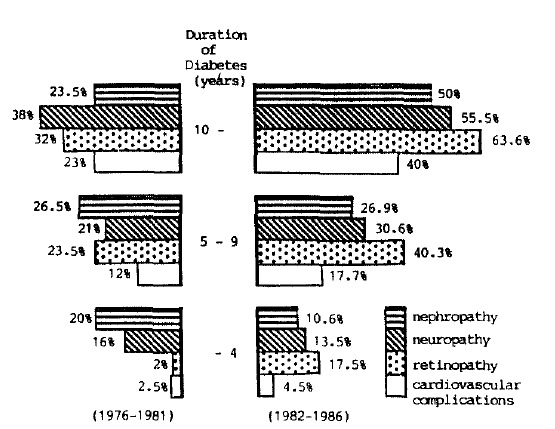
Comparisons of the duration of diabetes and prevalence of major complications in two study periods.
The mortality from diabetic nephropathy seems to increase recently and it is a problem to control terminal renal failure in diabetics. The overall prevalence rate of diabetic nephropathy was 15.5% in this study group, which was rather lower than that of Japan11), but higher than other reports12,13), however, the incidence was higher than in these authors’ study (Fig. 1). Socioeconomic conditions and racial factors could be involved in such discrepancies14,15). Similar to other reports16–18) the prevalence of diabetic nephropathy increased according to the duration of diabetes, old age group, and in male.
Cardiovascular diseases are well known as the most common complication and major causes of premature mortality in diabetics today19,20). These results indicated that the prevalence of cardiovascular complications was 25.7% which was lower than those in Western countries21), Japan22) and Taiwan3) but similar to those in other Asian countries23–25). Since ischemic heart disease, including myocardial infarction, was not included in this study, the exact prevalence of cardiovascular disease and/or ischemic heart disease could be higher than this of this study. Prevalence of cardiovascular complications was increased according to the duration of diabetes, but was not related to sexes, which differs from other reports18,26,27).
The results suggest that chronic diabetic complications are related to the duration of disease and to the age of patients. Also, the prevalence rate of diabetic complications should be evaluated while considering other relevant factors, such as racial and socioeconomic status, and also, the possible risk factors for all complications.
Fig. 2.
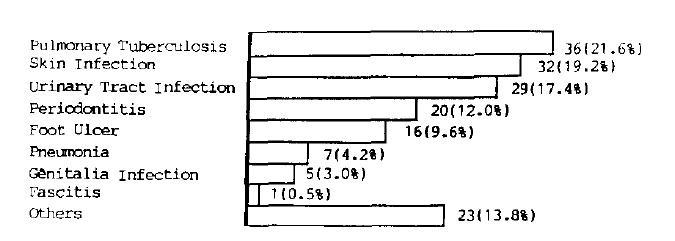
The prevalence of infections in 1,442 diabetic patients.
Fig. 5.
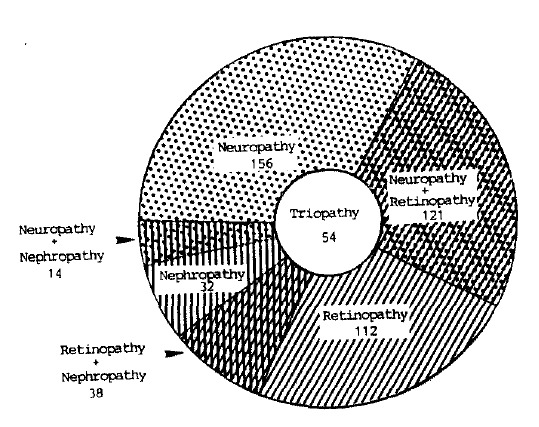
The various combinations of diabetic neuropathy retinopathy and nephropathy.
Table 2.
Age and Sex Distributions of Diabetic Neuropathy
| Sex | Age (years)
|
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| – 19 | 20 – 29 | 30 – 39 | 40–49 | 50 – 59 | 60 – | |||
| Peripheral neuropathy | M/F | 1/2 | 4/4 | 11/10 | 38/36 | 74/68 | 28/30 | 156/140 |
| Autonomic neuropathy | M/F | 0/1 | 1/0 | 1/0 | 3/3 | 4/5 | 6/4 | 15/13 |
| Combined neuropathy | M/F | 0/0 | 1/1 | 0/1 | 4/2 | 8/6 | 6/2 | 19/12 |
|
| ||||||||
| Total | M/F | 1/3 | 6/5 | 12/11 | 35/41 | 86/69 | 40/36 | 190/165 |
M : Male,
F : Female
Table 3.
Age and Sex Distributions of Eye Complications
| Sex | Age (years)
|
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| – 19 | 20 – 29 | 30 – 39 | 40 – 49 | 50 – 59 | 60 – | |||
| Retinopathy | ||||||||
| Background retinopathy | M/F | 1/7 | 5/5 | 2/13 | 44/20 | 64/59 | 45/34 | 161/138 |
| Proliferative retinopathy | M/F | 0/0 | 1/0 | 1/2 | 1/3 | 8/6 | 4/0 | 15/11 |
|
| ||||||||
| Total | M/F | 1/7 | 6/5 | 3/15 | 45/23 | 72/65 | 49/34 | 176/149 |
|
| ||||||||
| Cataract | M/F | 0/0 | 1/0 | 0/0 | 4/4 | 13/20 | 21/18 | 39/42 |
Table 4.
Age and Sex Distributions of Diabetic Nephropathy
| Sex | Age (years)
|
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| – 19 | 20 – 29 | 30 – 39 | 40 – 49 | 50 – 59 | 60 – | |||
| Proteinuria | M/F | 0/0 | 4/0 | 2/4 | 11/7 | 29/9 | 16/16 | 62/36 |
| Proteinuria with increased BUN & creatinine | M/F | 0/1 | 0/0 | 2/0 | 3/2 | 4/4 | 17/5 | 26/12 |
|
| ||||||||
| Total | M/F | 0/1 | 4/0 | 4/4 | 14/9 | 33/13 | 33/21 | 88/48 |
Table 5.
Age and Sex Distributions of Diabetic Cardiovascular Complications
| Sex | Age (years)
|
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| – 19 | 20 – 29 | 30 – 39 | 40 – 49 | 50 – 59 | 60 – | |||
| Hypertension | M/F | 0/0 | 3/0 | 2/8 | 17/20 | 33/54 | 25/30 | 80/92 |
| Atherosclerosis | M/F | 0/0 | 0/0 | 0/0 | 5/0 | 7/1 | 0/2 | 12/3 |
| Cerebral thrombosis | M/F | 0/0 | 0/0 | 0/1 | 3/1 | 7/3 | 2/1 | 12/3 |
| Gangrene | M/F | 1/1 | 2/1 | 1/0 | 4/1 | 9/4 | 1/2 | 18/9 |
|
| ||||||||
| Total | M/F | 1/1 | 5/1 | 3/9 | 29/22 | 56/42 | 28/35 | 122/110 |
REFERENCES
- 1.Boulton AJM, Scarpello JHB, Martin TRP, Pilling D, Ward JD. Claudication in neuropathic with supra-normal pressure indices. Diabetologia. 1981;20:666. [Google Scholar]
- 2.Ward JD. The diabetic leg. Diabetologia. 1982;22:141–47. doi: 10.1007/BF00283741. [DOI] [PubMed] [Google Scholar]
- 3.Tsai SJ. Diabetes Mellitus in Asia. In: Baba S, Goto Y, Fukui I, editors. Proceedings of the Second Symposium, Kyoto 1975. Excerpta Medica; Amsterdam: 1975. pp. 69–73. ICS 390. [Google Scholar]
- 4.Ellenberg M. Diabetic neuropathy. In: Ellenberg M, Rifkin H, editors. Diabetes Mellitus Theory and Practice. 3rd ed. New Hyde Park, New York: Medical Examination Publishing Co; 1983. pp. 777–801. [Google Scholar]
- 5.Piratt J. Diabetic neuropathy: a metabolic or a vascular disease? Diabetes. 1965;14:1–9. doi: 10.2337/diab.14.1.1. [DOI] [PubMed] [Google Scholar]
- 6.Piratt J. Diabetes mellitus and its degenerative complications: a prospective study of 4,400 patients between 1947 and 1973. Diabetes Care. 1978;1:168–88. 252–63. [Google Scholar]
- 7.Tiengo A, Segatoi T, Briani G, Setti A, Del-Prato S, Devide A, Padovan D, Virgili F, ad Crepaldi G. The presence of retinopathy in patients with secondary diabetes following pancreatectomy or chronic pancreatitis. Diabetes Care. 1983;6:570–74. doi: 10.2337/diacare.6.6.570. [DOI] [PubMed] [Google Scholar]
- 8.Leibowita The Framingham Eye Study. V Diabetic retinopathy. Surv Ophthalmol. 1980 May-Jun;24(Suppl.):401. [PubMed] [Google Scholar]
- 9.Mitchell P. The prevalence of diabetic retinopathy: A study of 1300 diabetics from Newcastle and the Hunter Valley. Aust J Ophthalmol. 1980;8:241. doi: 10.1111/j.1442-9071.1980.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 10.Couet C, Genton P, Pointel JP, Louis J, Gross P, Saudax E, Debry G, Drouin P. The prevalence of retinopathy is similar in Diabetes Mellitus secondary to chronic pancreatitis with or without pancreatectomy and in idiopathic Diabetes Mellitus. Diabetes Care. 1985;8:323–28. doi: 10.2337/diacare.8.4.323. [DOI] [PubMed] [Google Scholar]
- 11.Miki E, Kuzuja T, Ide T. Frequency, degree, and progression with time of proteinuria in diabetic patients. Lancet. 1972;1:922. doi: 10.1016/s0140-6736(72)91493-6. [DOI] [PubMed] [Google Scholar]
- 12.Klimt CR, Knatterud GL, Meinert CL, Prout TE. The University Group Diabetes Program: A study of the effects of hypoglycemic agents on vascular complications in patients with adult-onset diabetes. I. Design, methods and baseline characteristics. Diabetes. 1970;19(Suppl 2):747. [PubMed] [Google Scholar]
- 13.Knatterud GL, Klimt CR, Goldner MG. The University Group Diabetes Program. Effects of hypoglycemic agents on vascular complications with adult-onset diabetes. VIII. Evaluation of insulin therapy: Final report. Diabetes. 1982;31(Suppl 5):1. [PubMed] [Google Scholar]
- 14.Light G, Barker CO, Wilber JA. Diabetic nephropathy-Georgia. MMWR. 1981;30:296. [Google Scholar]
- 15.Easterling RE. Racial factors in the incidence and causation of end-stage renal disease. Trans Soc Artif Intern Organs. 1977;23:28. doi: 10.1097/00002480-197700230-00008. [DOI] [PubMed] [Google Scholar]
- 16.West KM, Erdreich LJ, Stober JA. A detailed study of risk factors for retinopathy and nephropathy in diabetes. Diabetes. 1980;29:501. doi: 10.2337/diab.29.7.501. [DOI] [PubMed] [Google Scholar]
- 17.Kamenetzky SA, Bennett PH, Dippe SE. A clinical and histologic study of diabetic nephropathy in the Pima Indians. Diabetes. 1974;23:61. doi: 10.2337/diab.23.1.61. [DOI] [PubMed] [Google Scholar]
- 18.Krolewski AS, Warram JH, Christstlieb Ar. In: Onset, course complications, and prognosis of diabetes mellitus in Joslin’s Diabetes Mellitus. VII ed. Marble A, Krall LP, Bradley RF, Christileb AP, Soeldner JS, editors. Philadelphia: Lea and Febiger; 1985. pp. 251–277. [Google Scholar]
- 19.Jarrett RJ, Keen H, Chakrabarti R. Diabetes hyperglycemia and arterial disease. In: Keen H, Jarrett RJ, editors. Complications of diabetes. 2nd ed. Arnold; London: 1982. pp. 179–184. [Google Scholar]
- 20.West KM. Epidemiology of diabetes and its vascular lesions. Elsevier; New York: 1978. pp. 353–369. [Google Scholar]
- 21.Entmacher PS, Krall LP, Kranczer SN. Diabetes mortality from vital statistics. In: Marble A, Krall LP, Bradley RF, Christlieb AR, Soeldner JS, editors. Joslin’s Diabetes Mellitus. VII ed. Philadelphia: Lea and Febiger; 1985. pp. 278–297. [Google Scholar]
- 22.Okuno G, Tako H, Fukuda K, Okamoto K, Kashihara T, Takenaka H, Toda Y. In: Diabetes Mellitus in Asia Proceedings of the second Symposium, Kyoto, 1875. Baba S, Goto Y, Fukui I, editors. Excerpta Medica; Amsterdam: 1975. pp. 183–188. ICS 390. [Google Scholar]
- 23.Fernand RE. Diabetes Mellitus in Asia. In: Baba S, Goto Y, Fukui I, editors. Proceedings of the Second Symposium, Kyoto 1975. Excerpta Medica; Amsterdam: 1975. pp. 98–108. ICS 390. [Google Scholar]
- 24.Young RTT, Warg CCL, Chan LKF. Diabetes Mellitus in Asia. In: Baba S, Goto Y, Fukui I, editors. Proceedings of Second Symposium, Kyoto 1975. Excerpta Medica; Amsterdam: 1975. pp. 131–136. ICS 390. [Google Scholar]
- 25.Sukono, Soewignjo S, Suharto In. Diabetes Mellitus in Asia. In: Baba S, Goto Y, Fukui I, editors. Proceedings of the Second Symposium, Kyoto 1975. Excerpta Medica; Amsterdam: 1975. pp. 196–201. ICS 390. [Google Scholar]
- 26.Baba S, Doi K, Morita S, Ikuno T, Yoshida Y, Morita S, Yokono K, Imamura Y, Taniguchi H. Diabetes Mellitus in Asia. In: Melish JS, Hanna J, Baba S, editors. Proceedings of the Third Symposium Honolulu, 1981. Excerpta medica; Amsterdam-Oxford-Princeton: 1982. pp. 77–87. ICS 549. [Google Scholar]
- 27.Yeung RTT, Wang CST, Kwan S. Diabetes Mellitus in Asia. In: Melish JS, Hanna J, Baba S, editors. Proceedings of the Third Symposium Honolulu, 1981. Excerpta Medica; Amsterdam-Oxford-Princeton: 1982. pp. 277–281. ICS 549. [Google Scholar]


