Abstract
OBJECTIVE:
Youth with type 1 diabetes mellitus are at risk for poor glycemic control as they age into adulthood. The aim of this study was to describe sociodemographic and clinical correlates of poor glycemic control associated with the transfer of care from pediatric to adult diabetes providers among a cohort of youth with type 1 diabetes diagnosed in adolescence.
METHODS:
Analyses included 185 adolescent participants with recently diagnosed type 1 diabetes in the SEARCH for Diabetes in Youth Study with pediatric care at baseline who were age ≥18 years at follow-up. Demographic and clinical factors were measured by survey and laboratory results. Survival analysis was used to estimate the age of transition. Logistic regression analysis assessed the association of demographic and clinical factors with the transition of care and poor glycemic control at follow-up.
RESULTS:
Fifty-seven percent of participants had transitioned to adult diabetes care providers by the follow-up visit. The estimated median age of transition of care was 20.1 years (95% confidence interval 19.8–20.4). Older age, lower baseline glycosylated hemoglobin, and less parental education were independently associated with increased odds of transition. The odds of poor glycemic control at follow-up were 2.5 times higher for participants who transitioned to adult care compared with those who remained in pediatric care.
CONCLUSIONS:
Transferring from pediatric to adult care, experienced by more than half the sample, was associated with an increased risk of poor glycemic control at follow-up. These findings suggest that young adults need additional support when moving to adult care.
Keywords: Transition of Care, adolescence, diabetes
What’s Known on This Subject:
Most children with type 1 diabetes get care from pediatric-trained providers, and must transfer care to adult providers once in adulthood. The timing of this change in providers and its relationship to glycemic control is not well understood.
What This Study Adds:
In this cohort, the estimated median age to transition to adult care was 20.1 years and 77% had left pediatric care by age 21. Leaving pediatric care was associated with a 2.5-fold increase in odds of having poor glycemic control.
Children and adolescents with type 1 diabetes mellitus will require lifelong access to medical care and relatively intensive daily self-management to maximize adult health outcomes and health-related quality of life. Most children with type 1 diabetes are cared for by pediatric-trained providers (either endocrinologists or general pediatricians), requiring transfer of care to an adult-trained provider once they approach adulthood. Patterns of transfer vary by location and health care delivery system, and are influenced by local practices and resources, patient/family preferences, and national policies.1–3 Although recent work has focused on understanding access to care and health outcomes during this period, these patterns have not been well described for youth with diabetes in the United States.1,2,4–6
Glycemic control, critical to long-term optimal outcomes for diabetes, has been shown to be poor for many youth as they age into adulthood.7–10 Many age-related factors could contribute to poor glycemic control, including changes in biological and psychosocial factors, and changes in access to care.4,5 More specifically, the impact of age-related changes in diabetes care providers on glycemic control is not well understood.
The longitudinal cohort in the SEARCH for Diabetes in Youth study (SEARCH) provides an opportunity to study changes in health care providers as youth age into adulthood. Furthermore, the study allows us to explore the association between changes in health care providers and glycemic control. We hypothesized that older age and female gender would be associated with greater odds of transitioning to adult care, and those changing to adult care would have worse glycemic control. A more thorough understanding of the transition period can inform policy and practice changes to best support youth with diabetes as they age into adulthood.
Methods
Study Overview and Procedures
SEARCH is a multicenter study that began conducting population-based ascertainment in 2001 among youth who were <20 years of age when diagnosed with diabetes.11 SEARCH recruited youth from 4 geographically defined populations in the United States, Indian Health Service beneficiaries from several American Indian populations, and enrollees in several managed health care plans. Institutional review board(s) for each of the 6 study sites approved the study protocol. All registered participants were asked to complete a brief initial survey; survey respondents were invited to a research visit. During this visit, informed consent and assent (when applicable) were obtained, questionnaires were administered, and physical measurements and fasting blood samples were obtained from metabolically stable participants (no episodes of diabetic ketoacidosis during the previous month) after a minimum 8-hour overnight fast. Youth whose diabetes was diagnosed in 2002 through 2005 were invited for follow-up visits at approximately 12, 24, and 60 months after their initial visit.
Study Population
Given our study’s focus on changes in providers and glycemic control during the transition to adulthood, we restricted this analysis to youth who were seen by a pediatric provider at baseline and had at least 1 follow-up study visit after reaching age 18 years. Thus, inclusion criteria were as follows: SEARCH participants with physician-diagnosed type 1 diabetes newly diagnosed between 2002 through 2005 who were ≥13 years at their baseline visit and had at least 1 follow-up visit after age 18, and who also had a glycosylated hemoglobin (A1c) measurement at both their baseline and follow-up visits. Individuals whose first study visit occurred within the first 3 months after diagnosis of diabetes were excluded because of potentially unstable initial A1c measurement. Only those who identified their diabetes provider as pediatric (general pediatric or pediatric endocrinologist) at the baseline visit were included in our cohort. We excluded 24 participants who saw adult providers at baseline, and 61 whose type of provider at the baseline visit could not be identified, including those who reported that their provider was a physician assistant or nurse, replied “other/don’t know,” or reported no provider for diabetes care. We were unable to identify the type of practices with which the nurses, nurse practitioners, and physician assistants were affiliated, which may have been pediatric or adult-trained physicians. An additional 27 individuals were excluded because their type of diabetes provider at a follow-up visit could not be determined.
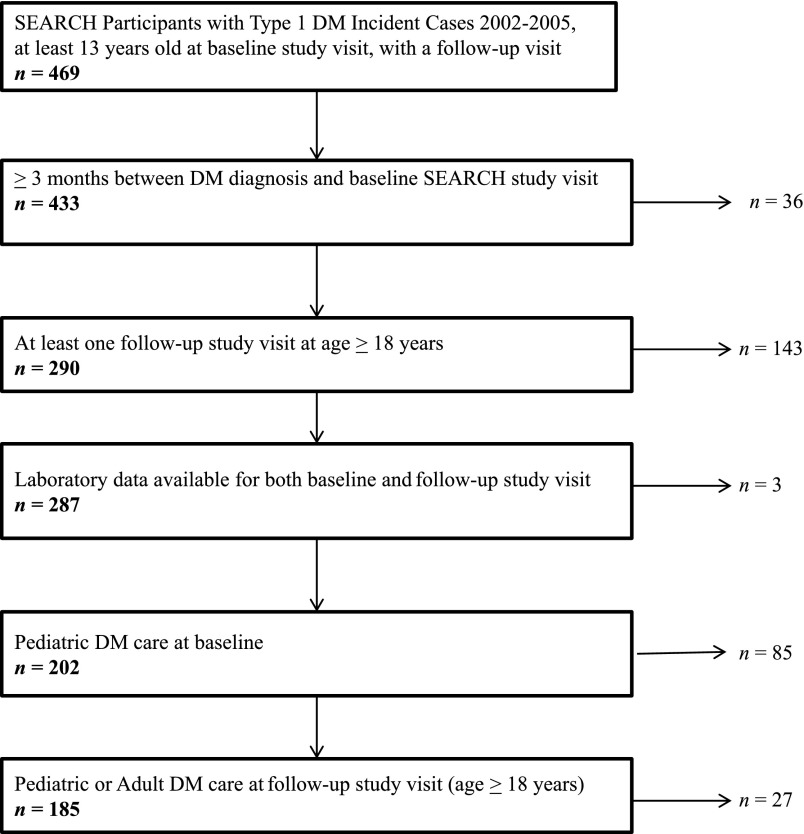
When an individual had multiple follow-up visits, information from the latest follow-up visit with the longest time interval from the baseline visit for which the type of provider could be identified was used for analysis. An exception was that all available follow-up visits were used in the model estimating age at transition as described later in this article. Figure 1 illustrates the inclusion criteria for participants in these analyses.
FIGURE 1.
Inclusion criteria for transition of care analysis. DM, diabetes mellitus.
Independent Variables
Demographic Characteristics
Sociodemographic factors known to be associated with health care use and health outcomes in other studies were selected for inclusion in these analyses. Race/ethnicity was self-reported, using the standard 2000 census questions and categorized as non-Hispanic white, Hispanic, non-Hispanic black, or other race/ethnicity; these categories were further combined as non-Hispanic white versus nonwhite participants. Highest parental education was based on self- or parent-reported highest parental education. Health insurance at the time of each study visit was recorded by participants as private insurance, Medicaid/Medicare (including other state-funded sources), other (including Indian Health Service, student health clinics, military, or other/unknown sources), or none; health insurance status was categorized as private versus nonprivate (combining Medicaid, Medicare, or other state-funded sources, other, or none).
Clinical Characteristics
Medical comorbidities were asthma, kidney disease, celiac disease, hypertension, or polycystic ovarian syndrome based on self or parental report. Duration of diabetes was the number of months elapsed between diagnosis of diabetes and baseline study visit. Time between the baseline and follow-up study visit is recorded in months. Hemoglobin A1c was measured in whole blood with an automated nonporous ion-exchange high-performance liquid chromatography system (model G-7; Tosoh Bioscience, Montgomeryville, PA) by using blood samples drawn at the baseline visit and again at the last available follow-up visit.
Outcome Variables
“Leaving pediatric care” was defined as reporting a pediatric diabetes care provider at the baseline visit and an adult diabetes care provider at the last available follow-up visit. Glycemic control at the follow-up visit was based on hemoglobin A1c measured at the last available follow-up visit. “Poor glycemic control” was defined as ≥9% based on the Diabetes Control and Complications Trial study documenting risk for complications among those >18 years old.12 We defined “age at transition” as occurring between the age at the last study visit where the participant reported a pediatric provider and the age at the next study visit when the participant reported an adult provider, with age estimated using the methods described as follows.
Statistical Analyses
All analyses were performed with SAS (version 9.2; SAS Institute, Cary, NC). Summary statistics were calculated to describe the sociodemographic and clinical characteristics for the cohort. We used separate multivariable logistic regression models to (1) identify sociodemographic and clinical characteristics that were independently associated with leaving pediatric diabetes care; and (2) identify predictors of poor glycemic control at follow-up. Independent variables included in both multivariable models were sociodemographic factors (age at follow-up, race/ethnicity, gender, type of insurance at follow-up, highest parental education) and disease-related factors (diabetes duration, hemoglobin A1c, presence of a medical comorbidity at baseline visit). Both models were adjusted for SEARCH study site and the time between the baseline and follow-up visits. The second model included the outcome variable from the first model as an indicator denoting whether an individual had transitioned from a pediatric to an adult diabetes care provider by the follow-up visit. To assess if the effects of age and hemoglobin A1c on our outcomes were linear (ie, their effect on the outcome was the same for both low and higher values of age and A1c) we tested quadratic terms for age and hemoglobin A1c. As these terms were both nonsignificant, they were excluded from the final models.
To estimate the age at transition of care, we performed a survival analysis by using all available visits for our cohort. We used maximum likelihood methods to fit a lognormal distribution with right and interval censored data. Participants who had transitioned to adult care by any of their follow-up visits were considered interval censored between their age at their last pediatric visit and their age at first transition, whereas participants who were still in pediatric care at their last follow-up visit were considered right censored at their follow-up age.
Results
Of the 185 youth included in this report, the average age at diagnosis of diabetes was 15 years. The baseline visit was ∼11 months after diagnosis, when participants were, on average, 16 years old (Table 1). Almost 60% were male, and 76% were non-Hispanic white. The last follow-up visit took place about 4.5 years after the baseline visit at an average age of 20.5 years. Approximately 86% of individuals had private insurance at both the baseline and follow-up visits. Two percent were uninsured at the baseline visit, which increased to 4% at follow-up.
TABLE 1.
Descriptive Characteristics of the Study Population (n = 185)
| Characteristics | Baseline, n(%) | Follow-up, n(%) |
|---|---|---|
| Sociodemographic factors | ||
| Age in years (mean ± SD) | 15.9 ± 1.7 | 20.5 ± 1.5 |
| Male gender | 106 (57%) | — |
| Race/Ethnicity | ||
| White, non-Hispanic | 140 (76%) | — |
| African-American, non-Hispanic | 19 (10%) | — |
| Hispanic | 18 (10%) | — |
| Other | 8 (4%) | — |
| Insurance status | ||
| Has private health insurance | 158 (86%) | 154 (83%) |
| Medicaid/Medicare/Other | 23 (12%) | 23(13%) |
| Uninsured | 4 (2%) | 8 (4%) |
| Highest parental education | ||
| ≤ High school | 33 (18%) | — |
| Some college | 47 (26%) | — |
| ≥ Bachelor’s degree | 104 (57%) | — |
| Disease factors | ||
| Age at diagnosis, y, mean ± SD | 15.0 ± 1.8 | — |
| Diabetes duration at baseline visit, mo, mean ± SD | 11.2 ± 6.9 | — |
| Time between visits, mo,a mean ± SD | 55.5 ± 16.2 | |
| Have a comorbidityb | 50 (27%) | 56 (30%) |
| Hemoglobin A1c, %, mean ± SD | 7.49 ± 1.74 | 9.21 ± 2.37 |
| Poor glycemic controlc | 20 (11%) | 84 (45%) |
| Care factors | ||
| Leave pediatrics by last follow-up visitd | ||
| Overall | 106 (57%) | |
| Age 18–20 at follow-up | 58/123 (47%) | |
| Age 21 and over at follow-up | 48/62 (77%) |
Denominators are sometimes less than 185 because of missing data. —, item not measured at the follow-up visit.
Time between visits: average time (in months) elapsed between baseline and follow-up visits.
Have a medical comorbidity: Presence of at least one of the following physician-diagnosed conditions (as reported by study participants): asthma, polycystic ovarian disease, kidney disease, celiac disease, or hypertension.
Poor glycemic control: hemoglobin A1c ≥9.0%
Leave pediatrics by follow-up: participant reporting that primary diabetes provider is an adult-trained physician at the last follow-up visit.
Transition From Pediatric Care
Overall, 57% of the sample had switched to an adult diabetes care provider by the last follow-up visit. This proportion increased with increasing age; only 47% of those aged 18 to 20 years at the last follow-up had changed to adult diabetes care providers, whereas 77% of those 21 and older had changed. The estimated median age of transition of care was 20.1 years old (95% confidence interval (CI) 19.8–20.4).
As depicted in Table 2, in the multiple logistic regression analysis model controlling for sociodemographic and disease-related factors, a 1-year increase in age was associated with a 1.87 increased odds of leaving pediatric care (95% CI 1.39–2.51, P < .001) (Table 2). In addition, those with higher baseline hemoglobin A1c values were less likely to leave pediatric care; the odds of leaving pediatric care decreased by 27% for every 1-unit increase in A1c (P = .013) after controlling for age and other confounding factors. Higher parental education at baseline (bachelor’s degree or higher) was significantly associated with reduced odds of leaving pediatric care, compared with those having less education (odds ratio = 0.34, 95% CI 0.14–0.82).
TABLE 2.
Odds Ratios for Independent Variables Predicting Leaving Pediatric Care and Going to Adult Diabetes Care at Follow-up Visita
| Variable | Unadjusted Results | Adjusted Resultsa | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | P Value | Odds Ratio | 95% CI | P Value | |
| Sociodemographic factors | ||||||
| Age, y, at follow-up | 1.74 | 1.37–2.23 | <.001 | 1.87 | 1.39–2.51 | <.001 |
| Male versus female | 0.78 | 0.43–1.41 | .412 | 0.97 | 0.47–2.02 | .939 |
| Nonwhite versus NH white | 1.68 | 0.83–3.40 | .146 | 1.59 | 0.52–4.89 | .418 |
| Not private versus private insurance at follow-upb | 1.22 | 0.55–2.69 | .623 | 1.39 | 0.49–3.93 | .532 |
| Highest parental education | .039 | .034 | ||||
| Some college versus ≤ high school | 1.35 | 0.52–3.47 | 1.10 | 0.33–3.68 | — | |
| ≥ College graduate versus ≤ high school | 0.55 | 0.25–1.23 | 0.37 | 0.12–1.17 | — | |
| ≥ College graduate versus some college | 0.41 | 0.20–0.85 | 0.34 | 0.14–0.82 | — | |
| Disease factors | ||||||
| Diabetes duration at baseline visit | 1.02 | 0.98–1.07 | .319 | 1.05 | 0.99–1.11 | .136 |
| Have a comorbidity at baselinec | 1.47 | 0.75–2.86 | .263 | 0.92 | 0.39–2.21 | .857 |
| Hemoglobin A1c at baseline | 0.85 | 0.71–1.01 | .062 | 0.73 | 0.57–0.94 | .013 |
NH, non-Hispanic
Model controlled for SEARCH study site, time elapsed between baseline and follow-up visits as well as variables presented in the table.
Not private group consists of n = 23 (74%) publically insured and n = 8 (26%) uninsured.
Have a comorbidity: presence of at least 1 of the following physician-diagnosed conditions (as reported by study participants): asthma, polycystic ovarian disease, kidney disease, celiac disease, or hypertension.
Poor Metabolic Control at Follow-Up
Average hemoglobin A1c was 7.5% at baseline and 9.2% at the follow-up visit. At baseline, 11% had poor glycemic control compared with 45% at the follow-up visit. In the adjusted model, the odds of having poor glycemic control at the follow-up visit were 2.46 times higher for those who left pediatric care (95% CI 1.09–5.55, P = .031) than for those who remained in pediatric care (Table 3). In addition, nonwhite participants had 3.44 times the adjusted odds of having poor glycemic control at follow-up compared with non-Hispanic white participants (95% CI 1.17–10.1, P = .025). Higher baseline hemoglobin A1c was also a significant independent predictor of poor control at follow-up. For every 1-unit increase in hemoglobin A1c at baseline, young adults had 1.84 times the odds of having poor control at follow-up (95% CI 1.38–2.45, P < .001).
TABLE 3.
Odds Ratios for Independent Variables Predicting Poor Glycemic Control at Follow-up Visit (Hemoglobin A1c ≥9%)a
| Variable | Unadjusted Results | Adjusted Results | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% Confidence Limits | P Value | Odds Ratio | 95% Confidence Limits | P Value | |
| Sociodemographic factors | ||||||
| Age, y, at follow-up | 0.79 | 0.65–0.97 | .025 | 0.77 | 0.59–1.01 | .063 |
| Male versus female | 0.63 | 0.35–1.14 | .127 | 0.70 | 0.34–1.43 | .326 |
| Nonwhite versus NH white | 2.18 | 1.10–4.33 | .025 | 3.44 | 1.17–10.1 | .025 |
| Not private versus private insurance at follow-upb | 2.17 | 0.98–4.78 | .055 | 1.47 | 0.55–3.88 | .443 |
| Highest parental education | .897 | .352 | ||||
| Some college versus ≤ high school | 0.94 | 0.38–2.28 | — | 2.04 | 0.64–6.53 | — |
| ≥ College graduate versus ≤ high school | 0.84 | 0.38–1.85 | — | 2.27 | 0.74–7.01 | — |
| ≥ College graduate versus some college | 0.90 | 0.45–1.80 | — | 1.12 | 0.49–2.56 | — |
| Disease factors | ||||||
| Diabetes duration at baseline visit | 1.02 | 0.98–1.07 | .333 | 0.98 | 0.93–1.04 | .457 |
| Have a comorbidity at baselinec | 1.15 | 0.60–2.21 | .666 | 1.01 | 0.44–2.29 | .991 |
| Hemoglobin A1c at baseline | 1.65 | 1.32–2.07 | <.001 | 1.84 | 1.38–2.45 | <.001 |
| Care factors | ||||||
| Leave pediatrics by follow-upd | 1.18 | 0.66–2.12 | .577 | 2.46 | 1.09–5.55 | .031 |
NH, non-Hispanic.
Model controlled for SEARCH study site, time elapsed between baseline and follow-up visits as well as variables presented in the table.
Not private group consists of n = 23 (74%) publically insured and n = 8 (26%) uninsured.
Have a comorbidity: presence of at least 1 of the following physician-diagnosed conditions (as reported by study participants): asthma, polycystic ovarian disease, kidney disease, celiac disease, or hypertension.
Leave pediatrics by follow-up: participant reporting that primary diabetes provider is an adult-trained physician at the follow-up visit.
Discussion
Recent guidelines from the American Academy of Pediatrics, the American College of Physicians, the American Academy of Family Practice,13 and the American Diabetes Association3 reaffirm that all young adults with diabetes should transition to adult-oriented medical care between 18 and 21 years of age. For our study population, we estimate that the median age of transition to adult care is 20.1 years with 77% of young adults >21 years of age having left pediatric care. To our knowledge, this is the first US study to describe the change to adult care and factors associated with this transition for a diverse cohort of adolescents and young adults with type 1 diabetes.
As expected, we found that older age predicted leaving pediatric care. In addition, we found that those youth with higher hemoglobin A1c at their baseline visit were less likely to leave pediatric care. One possible explanation for this finding is that pediatric providers may have a higher level of concern for patients in poor control, and as a result continue to care for these patients longer in an attempt to prevent worsening of their glycemic control. This may include the recognition that such patients have greater need of psychosocial resources that may be more available in the pediatric setting. Our data also suggest that youth of more educated parents (bachelor’s degree or more) are less likely to leave pediatric care. Future research is needed to examine the reasons behind these observations. Other sociodemographic factors (race/ethnicity, type of insurance), diabetes duration, and presence of medical comorbidities, did not affect the transition to adult care.
We also found that leaving pediatric care was associated with a 2.5-fold increase in the odds of being in poor glycemic control at the follow-up visit compared with those who stay in pediatric care, after controlling for both sociodemographic and disease-related factors. Access to care (based on type of health insurance at the follow-up visit as a proxy measure) did not mediate the relationship between transition to adult care and poorer glycemic control. However, most youth in this cohort had health insurance as young adults, and we did not see a difference in glycemic control between the private and nonprivately insured groups in young adulthood. Other evidence that transition-related problems in adult care are unrelated to insurance coverage comes from countries with universal health insurance systems, such as Canada and Europe. These studies have found that youth with diabetes are often not following up in a timely way with new providers even though they have access to this care.3,8,9,14–16 These individuals are also at risk for nonadherence with recommended visit frequency or disease self-management tasks, and have more diabetes-related hospitalizations after leaving pediatric care.
The finding that individuals from nonwhite and Hispanic ethnic/racial backgrounds had increased risk of poor control at follow-up, even after controlling for a number of socioeconomic variables and baseline hemoglobin A1c, is concerning. Previous research has suggested that African American and Hispanic youth are at risk for poor glycemic control while in pediatric care, although some studies have found that socioeconomic variables account for this effect.7,17,18 Young adults from minority racial/ethnic backgrounds are considered at increased risk of poor transition outcomes.19 Given our findings, this warrants further evaluation in future studies.
Unmeasured factors may account for the variation in timing of the transfer to adult care for these youth. Patient factors, such as psychosocial readiness for transition, could be influencing providers’ and families’ willingness to “let go” and move on to adult care.20 Practice and environmental factors, such as the presence of policies around transferring care in adulthood and/or access to adult-trained type 1 diabetes specialists, could also be important.
Further research is urgently needed to explore reasons why glycemic control deteriorates in late adolescence and young adulthood and if alterations in the timing of transfer from pediatric to adult care can prevent this outcome. Young adulthood is a time of multiple changes, not only in health care needs, but also physical maturation and evolving relationships with others. A better understanding of how life transitions affect health-related behaviors, access to health care, and health care use is needed. More specifically, research focused on examining patient, parent, and provider attitudes and behaviors, as well as health care system processes and obstacles will help to identify potential causes and interventions that may mitigate the risk of deteriorating glycemic control with transition in this population.
Research is also needed to understand how providers can best support the adolescent/young adult population. Previous studies have shown that physician continuity and intensive care coordination can help improve patient transition to adult care.3,21,22 Studies of various counseling strategies, including family-oriented counseling and youth empowerment strategies, are also promising.23
Limitations
We cannot identify participants’ exact age or hemoglobin A1c value at the time of transfer to adult care from these data nor can we measure the amount of time that elapsed between changing providers and the next follow-up study visit. In addition, all participants were adolescents who had been recently diagnosed with diabetes at the time of study entry, constraining the observed duration of illness. Indeed, youth diagnosed with type 1 diabetes during their teenage years may be different from those who are diagnosed at a younger age who will have had diabetes for many years at the time of their transition and may have had more time to develop their self-management skills and prepare for transition. In addition, those more recently diagnosed (even as far out as 1 year) may have better glycemic control than those who have had their disease for longer, perhaps because of residual islet cell function.7,24 Restricting our cohort to relatively recently diagnosed adolescents also likely explains the difference in the observed glycemic control in our cohort compared with the SEARCH study participants as a whole.7 The interpretation of the statistically significant relationship between race/ethnicity and glycemic control at follow-up is limited by the relatively small sample of nonwhite participants (n = 45, 24% of the cohort) resulting in a wide confidence interval for the effect. Despite the limitations, these analyses are based on a subset of one of the largest longitudinal cohorts of youth with type 1 diabetes in the United States.
Conclusions
In this cohort of youth who were diagnosed with type 1 diabetes during their adolescent years, the estimated median age of transition to adult care is 20.1 years with 34% and 18% remaining in pediatric care on their 21st and 22nd birthdays, respectively. Leaving pediatric care is associated with poor glycemic control in young adults with type 1 diabetes, independent of previous poor glycemic control. These findings suggest that to safely follow current guidelines, young adults who transition to adult care require additional support to maximize their health outcomes that will extend for some time beyond the transfer to an adult provider. Further studies are needed to understand the factors mediating the relationship between changing provider and diabetes disease outcomes, as well as the type and duration of assistance needed to eliminate the transition-related deterioration in glycemic control.
Acknowledgments
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible. SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases.
Site Contract Numbers: Kaiser Permanente Southern California (U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Kuakini Medical Center (U58CCU919256 and U01 DP000245), Children’s Hospital Medical Center (Cincinnati) (U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01 DP000254, and U18DP002708-01), University of Washington School of Medicine (U58/CCU019235-4, U01 DP000244, and U18DP002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01 DP000250, and 200-2010-35171).
The authors acknowledge the involvement of General Clinical Research Centers at the South Carolina Clinical and Translational Research Institute, at the Medical University of South Carolina (National Institutes of Health/National Center for Research Resources grant number UL1RR029882); Children’s Hospital and Regional Medical Center (grant Number M01RR00037); Colorado Pediatric General Clinical Research Center (grant Number M01 RR00069) and the Barbara Davis Center at the University of Colorado at Denver (DERC NIH P30 DK57516); and the Institutional Clinical and Translational Science Award, National Institutes of Health/National Center for Research Resources at the University of Cincinnati (grant Number 1UL1RR026314-01).The writing group for this article acknowledges the contributions of the following individuals to the SEARCH for Diabetes in Youth Study:
California: Jean M. Lawrence, ScD, MPH, MSSA, Kristi Reynolds, PhD, MPH, Jin-Wen Hsu, PhD, Mary Helen Black, PhD, Kim Holmquist, BA, and Harpreet S. Takhar, MPH, for the Department of Research and Evaluation and Ann K. Kershnar, MD, for the Department of Pediatrics, Kaiser Permanente Southern California; and David J. Pettitt, MD, for the Sansum Diabetes Research Institute
Colorado: Dana Dabelea, MD, PhD, Richard F. Hamman, MD, DrPH, Lisa Testaverde, MS, for the Department of Epidemiology, Colorado School of Public Health, University of Colorado Denver; Georgeanna J. Klingensmith, MD, Marian J. Rewers, MD, PhD, David Maahs, MD, and Paul Wadwa, MD, for the Barbara Davis Center for Childhood Diabetes; Stephen Daniels, MD, PhD, Kristen Nadeau, MD, Department of Pediatrics and Children’s Hospital; Clifford A. Bloch, MD, for the Pediatric Endocrine Associates; Carmelita Sorrelman, MSPH, and Alfreda Beartrack, MSPH, for the Navajo Area Indian Health Prevention Program
Hawaii: Beatriz L. Rodriguez, MD, PhD, Wilfred Fujimoto, MD, J. David Curb, MD (deceased), Fiona Kennedy, RN, Greg Uramoto, MD, Sorrell Waxman, MD, and Richard Chung, MD, for Kuakini Medical Center; Beth Waitzfelder, PhD, for the Center for Health Research, Kaiser Permanente Hawaii; and Teresa Hillier, MD for the Center for Health Research, Kaiser Permanente Northwest and Hawaii.
Ohio: Lawrence M. Dolan, MD, Michael Seid, PhD, Elaine Urbina, MD, MS, and Debra A. Standiford, MSN, CNP, for the Cincinnati Children’s Hospital Medical Center.
North Carolina: Elizabeth J. Mayer-Davis, PhD, and Joan Thomas MS, RD, for the University of North Carolina, Chapel Hill; and Mark Parker, MD, for Pediatric Endocrinology & Diabetes Specialists, Charlotte, NC.
South Carolina: Anwar Merchant, ScD, Angela D. Liese, PhD, MPH, Robert R. Moran, PhD, Gladys Gaillard-McBride, RN, CFNP, Deborah Lawler, MT (ASCP), and Malaka Jackson, MD for the University of South Carolina; Deborah Bowlby, MD, for the Medical University of South Carolina; James Amrhein, MD, for Greenville Hospital Systems; and Pam Clark, MD, for McLeod Pediatric Subspecialists.
Washington: Catherine Pihoker, MD, Maryam Afkarian, MD, Angela Badaru, MD, Lisa Gilliam, MD, PhD, Irl Hirsch, MD, Lenna L. Liu, MD, MPH, John Neff, MD, and Joyce Yi-Frazier, PhD, for the University of Washington; Beth Loots, MPH, MSW, Rebecca O’Connor, RN, Sue Kearns, RN, Mary Klingsheim, RN, Emil Buscaino, BS, Katherine Cochrane, BS, Onel Martinez, MS, and Sharla Semana, BS, for Seattle Children’s Hospital; and Carla Greenbaum, MD, for Benaroya Research Institute
Centers for Disease Control and Prevention: Giuseppina Imperatore, MD, PhD, Desmond E. Williams, MD, PhD, Henry S. Kahn, MD, Bernice Moore, MBA, Gregg W. Edward, PhD, and Sharon H. Saydah, PhD.
National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health: Barbara Linder, MD, PhD.
Central Laboratory: Santica M. Marcovina, PhD, ScD, Vinod P. Gaur, PhD, and Jessica Harting for the University of Washington Northwest Lipid Research Laboratories.
Coordinating Center: Ronny Bell, PhD, MS, Ralph D’Agostino, Jr, PhD, Bettina Beech, DrPH, Douglas Case, PhD, Jasmin Divers, PhD, Timothy Morgan, PhD, Michelle Naughton, PhD, Leora Henkin, MPH, MEd, Susan Moxley, BS, Gena Hargis, MPH, Donna Kronner, Maureen T. Goldstein, BA, Andrea Anderson, MS, Jeanette Andrews, MS, Abigail Lauer, MS, and Jennifer Talton, MS, for Wake Forest School of Medicine.
Glossary
- A1c
glycosylated hemoglobin
- CI
confidence interval
- SEARCH
SEARCH for Diabetes in Youth study
Footnotes
Dr Lotstein conceptualized and designed the study, contributed to survey development, drafted the initial manuscript, and reviewed and revised the manuscript. Dr Seid contributed to the study’s conceptualization and design, contributed to survey development, and critically reviewed the manuscript. Dr Klingensmith contributed to the study’s conceptualization and design, contributed to survey development, coordinated and supervised data collection at 1 of the 6 study sites, and critically reviewed and revised the manuscript. Dr Case contributed to the study’s conceptualization and design, carried out analyses of data, contributed to the interpretation of data, and critically reviewed and revised the manuscript. Drs Lawrence, Dabelea, and Dolan helped coordinate and supervise data collection, contributed to the study’s conceptualization and design, and critically reviewed the manuscript. Dr Pihoker helped coordinate and supervise data collection, contributed to the study’s conceptualization and design, contributed to survey development, and critically reviewed the manuscript. Drs Mayer-Davis and Imperatore contributed to the study’s conceptualization and design, contributed to survey development, and critically reviewed the manuscript. Drs Gilliam, Corathers, and Bell contributed to the study’s conceptualization and design and critically reviewed the manuscript. Ms Anderson contributed to the analysis and interpretation of data and critically reviewed the manuscript. Dr Waitzfelder helped coordinate and supervise data collection, conceptualized and designed the study, contributed to survey development, drafted the initial manuscript, and critically reviewed the manuscript. All authors approved the final manuscript as submitted.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Dr Gilliam's current affiliation is Medicine/Endocrinology, Kaiser Permanente South San Francisco, California.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
References
- 1.Busse FP, Hiermann P, Galler A, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67(3):132–138 [DOI] [PubMed] [Google Scholar]
- 2.Pacaud D, Yale JF. Exploring a black hole: transition from paediatric to adult care services for youth with diabetes. Paediatr Child Health (Oxford). 2005;10(1):31–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124(6). Available at: www.pediatrics.org/cgi/content/full/124/6/e1134. [DOI] [PubMed] [Google Scholar]
- 4.Peters A, Laffel L, American Diabetes Association Transitions Working Group . Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society).. Diabetes Care. 2011;34(11):2477–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowen M, Henske J, Potter A. Health care transition in adolescents and young adults with diabetes. Clin Diabetes. 2010;28(3):99–106 [Google Scholar]
- 6.Nakhla M, Daneman D, Frank M, Guttmann A. Translating transition: a critical review of the diabetes literature. J Pediatr Endocrinol Metab. 2008;21(6):507–516 [PubMed] [Google Scholar]
- 7.Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr. 2009;155(5):668–672.e1–3 [DOI] [PMC free article] [PubMed]
- 8.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536–1540 [DOI] [PubMed] [Google Scholar]
- 9.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26(4):1052–1057 [DOI] [PubMed] [Google Scholar]
- 10.Luyckx K, Seiffge-Krenke I. Continuity and change in glycemic control trajectories from adolescence to emerging adulthood: relationships with family climate and self-concept in type 1 diabetes. Diabetes Care. 2009;32(5):797–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.SEARCH Study Group . SEARCH for Diabetes in Youth: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25(5):458–471 [DOI] [PubMed] [Google Scholar]
- 12.The Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986 [DOI] [PubMed] [Google Scholar]
- 13.Cooley WC, Sagerman PJ, American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians. Transitions Clinical Report Authoring Group . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200 [DOI] [PubMed] [Google Scholar]
- 14.Sparud-Lundin C, Ohrn I, Danielson E, Forsander G. Glycaemic control and diabetes care utilization in young adults with Type 1 diabetes. Diabet Med. 2008;25(8):968–973 [DOI] [PubMed] [Google Scholar]
- 15.Waitzfelder B, Pihoker C, Klingensmith G, et al. SEARCH for Diabetes in Youth Study Group . Adherence to guidelines for youths with diabetes mellitus. Pediatrics. 2011;128(3):531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sparud-Lundin C, Ohrn I, Danielson E. Redefining relationships and identity in young adults with type 1 diabetes. J Adv Nurs. 2010;66(1):128–138 [DOI] [PubMed] [Google Scholar]
- 17.Chalew SA, Gomez R, Butler A, et al. Predictors of glycemic control in children with type 1 diabetes: the importance of race. J Diabetes Complications. 2000;14(2):71–77 [DOI] [PubMed] [Google Scholar]
- 18.Gallegos-Macias AR, Macias SR, Kaufman E, Skipper B, Kalishman N. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes. 2003;4(1):19–23 [DOI] [PubMed] [Google Scholar]
- 19.Lotstein DS, Kuo AA, Strickland B, Tait F. The transition to adult health care for youth with special health care needs: do racial and ethnic disparities exist? Pediatrics. 2010;126(suppl 3):S129–S136 [DOI] [PubMed] [Google Scholar]
- 20.Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115(1):112–120 [DOI] [PubMed] [Google Scholar]
- 21.Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31(8):1529–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cadario F, Prodam F, Bellone S, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf). 2009;71(3):346–350 [DOI] [PubMed] [Google Scholar]
- 23.Husted GR, Thorsteinsson B, Esbensen BA, Hommel E, Zoffmann V. Improving glycaemic control and life skills in adolescents with type 1 diabetes: a randomised, controlled intervention study using the Guided Self-Determination-Young method in triads of adolescents, parents and health care providers integrated into routine paediatric outpatient clinics. BMC Pediatr. 2011;11:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valle T, Koivisto VA, Reunanen A, Kangas T, Rissanen A. Glycemic control in patients with diabetes in Finland. Diabetes Care. 1999;22(4):575–579 [DOI] [PubMed] [Google Scholar]