Abstract
Objective:
To assess the degree of utilization of the radiology request form (RRF), the extent of completion each form, the frequency of filling the fields in all the forms, and its effectiveness as a communication tool between the referring clinicians and radiologists.
Materials and Methods:
All the RRFs for conventional radiographic examinations were audited over a 3-month period. A database containing all the fields in the form, type of request paper used, and legibility of the physician's handwriting was created. A few resident radiologists in the plain film reporting unit were recruited to join in collecting the data daily. We used simple statistical methods to analyze the extent of completion of each form, frequency of completion of the fields in all the request forms, frequency of use of the appropriate form, and frequency of legibility of the physician's handwriting. The results are expressed in percentages.
Results:
Five hundred eighty (580) requests were analyzed, consisting of 180 for males and 400 for females. The most-completed request form was 86.67% filled, while the least-completed was 26.67%. The most frequently filled field was the requested examination (99.66%). Of the clinicians, 28% did not use the RRF for their referrals, while 7.37% had illegible handwriting.
Conclusion:
A significant number of the referring clinicians did not make the best use of the radiology department by not using the institution's approved RRF as an effective means of communication with the radiologists, mainly due to the inadequate completion of the forms.
Keywords: Clinicians, completion, radiology request form, utilization
Introduction
A radiology request is a clinical document completed by a licensed physician. The request to a clinical radiology department represents a request for an opinion from a clinical radiologist and is usually made on a standard radiology request form (RRF).[1] The RRF is one of the means of communication between the referring clinicians and radiologists.[2] The Royal College of Radiologists in it guidelines states that this request form should be completed adequately and legibly to avoid any misinterpretation.[3] Inadequate filling of the RRF is a global problem, as observed by Rajanikanth.[4] We decided to audit only the requests sent for conventional radiographic examination because it is the most frequently requested examination: It utilizes ionizing radiation and the radiologists usually relies solely on the information provided by the referring clinician, as he/she does not usually have contact with the patients during these examinations.
Materials and Methods
This was a prospective study carried out in a public tertiary/teaching hospital in a city that is the state capital. We did not interfere with the patient's examinations and their personal information in the RRFs was not used, so we did not formally apply for approval from the hospital's Ethical Committee. Five hundred eighty (580) consecutive requests for conventional radiographic examinations from the wards and outpatient clinics were used for the study over a 3-month period, May-July 2012. A database was created and the data were obtained in conjunction with selected resident radiologists in the plain film reporting unit daily. The forms or sheets of paper on which the requests were made and the legibility of the handwriting of the referring clinician were assessed. The extent of completion of the fields (15 for female patients and 14 for male patients) in each form and the frequency of filling each field in all the forms were analyzed using simple statistical calculations. A score of zero (0) was given when a wrong request form was used, the clinician's handwriting was illegible or a field was not filled, while one (1) was given if otherwise. These were summed up; the results are expressed in percentages, which are presented in tables, bar charts, and pie charts.
Results
Five hundred eighty (580) request forms, consisting of 400 for females and 180 for males, were analyzed in the study. The most-completed request form was 86.67% filled, while the least-completed was 26.67%. Table 1 shows the frequency of the percentage completion of the request forms, with most of the RRFs being 51-70% completed (n = 402). Table 2 shows the frequency distribution of the completed fields in the forms. Figure 1 shows the frequency distribution of the utilization of the designated RRF. Figure 2 shows the frequency distribution of the legibility of the clinician's hand writing.
Table 1.
Completion of the radiology request forms
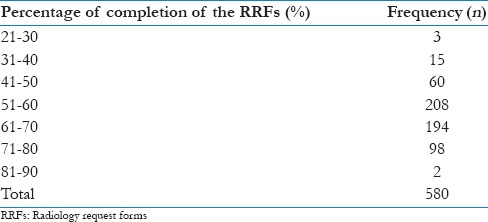
Table 2.
Frequency distribution of the completed fields
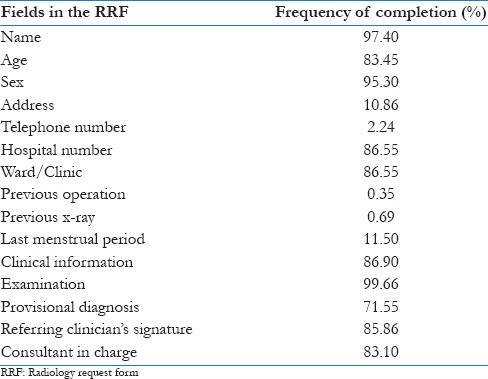
Figure 1.
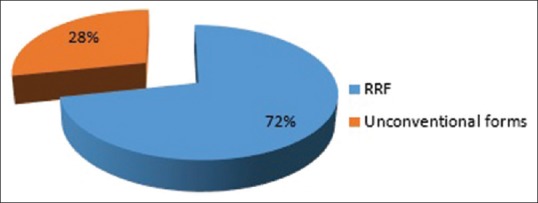
Type of request paper
Figure 2.
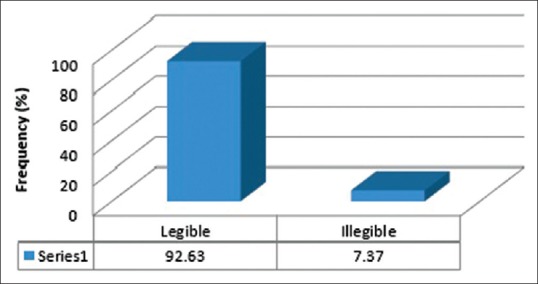
Legibility of the clinician's handwriting
Discussion
The study revealed that our radiology requesting practice is poor. None of the request forms was completely filled and the most-filled field in all the forms was the requested examination, at 99.66%. Instead of on the approved RRF of our institution, 28.3% of the requests were made on laboratory forms, prescriptions, and continuation sheets. This is a higher percentage than the finding in a similar study in southwest Nigeria, where 7.34% used similar unconventional request papers.[5] Using unconventional request forms allows the omission of important information required for the examination.
We observed that 7.37% of the requests had illegible handwriting, which is better than the findings of Longrigg and Channon (9%), and Jumah et al. (15.96%).[6,7] Illegible handwriting leads to lack of understanding of the request or wrong interpretation. The former leads to delay in carrying out the examination because the clinician needs to be contacted for clarification, while the latter can lead to a wrong examination being done, repeat examinations, and, ultimately, unnecessary radiation exposure.
The seven fields in our RRF that help in patient identification and tracking are the patient's name, age, sex, address, personal telephone number, hospital telephone number, and the ward or clinic from which the referral was made. In our study, the two least-filled fields among these were the patient's telephone number (2.24%) and address (10.86%). These two data allow direct communication with outpatients if an appointment is to be booked or rescheduled. Our finding about the patient's address is similar to that of Irurhe et al. (13%),[8] but lower than what was observed by Afolabi et al. (39.66%),[5] The patient's name was the best-filled field in this group in our study at 97.4%, but three other studies showed better filling of this field at 99.85%, 100%, and 100%.[5,8,9] When the information provided in the RRF is inadequate, the radiologist occasionally needs to visit the inpatients on the ward or retrieve his/her case notes to get the required information. The hospital number and the ward/clinic from which the patient is referred helps to get this information, but in this study they were both found filled-in in 86.55% of the forms. Entry of the sex of the patient into the RRF is at 95.3% in our study, which is comparable with the 96% observed by Afolabi et al. but less than that observed by Irurhe (99.7%). The ages of the patients were also poorly filled in our findings (83.45%), compared to two others (98% and 94.1%),[5,8] but better than one (79.2%).[9]
The patient's demographics are an important part of the request.[10] The radiologist needs to know the patient's demographics, presenting compliance, past medical and surgical history, and the clinical question (provisional diagnosis) in order to use his/her expertise to choose the most appropriate and safe imaging modality to answer the question/make the right radiological diagnosis. Clinical information was provided in 86.90% of the requests, which is suboptimal. The regulations of the Department of Health, UK, require that the referrer supply sufficient medical data, relevant to the medical exposure requested, to enable the radiation practitioner to decide whether the exposure can be justified.[11] Some medications can cause radiographic changes in patients or alter the course of a disease just as a previous surgery can alter the normal anatomy, so the provision of information on these are very important for film reporting. Only 0.35% of the RRFs provided information on the previous operation (s). The Royal College of Radiologists suggests that all radiology reports should address the questions posed by the referring doctors,[12] but the clinical question was asked in only 71.55% of the requests in our study, which is better than the findings in two other studies (at 54% and 1.4%).[13,14] Irurhe et al., however, found a higher percentage of entry at 90%.[8]
Entry of the previous x-ray exposure was very poor in our study (0.35%). A record of all the previous exposures is important so that patients are not exposed beyond the recommended dose limits, and a previous examination may be required for comparison to determine progression of a clinical condition. The last menstrual period (LMP) helps in the radiation protection of the embryo or foetus, as an overdue menstruation in a woman of reproductive age is assumed to be due to pregnancy until proven otherwise. In one study, LMP was entered in 1% of the RRFs, compared to the 11.50% gotten in our study.[15]
It is important to know the consultant in charge of the case and the referring doctor so that if there is a need to clarify the information on the request or get more information about a patient, he/she can easily be contacted. The signature of the referring clinician also authenticates the request. The signature of the clinician was found in 85.86% of the RRFs in our study, which is lower than in other studies (93.8%, 91.3%, and 100%).[13] The name of the consultant in charge was provided in 83.1% of forms, which is also lower than in other studies (92.0%, 99.7%, 88.7%, 91.0%, and 97.2%).[8,9,10,13,16]
Conclusion
A significant number of the referring clinicians did not make the best use of the radiology department by not using the institution's approved RRF as an effective means of communication with the radiologists. This was mainly due to inadequate completion of the fields in the forms. We recommend that regular workshops be held to enlighten the referring physicians, especially those newly employed, on the importance of all the fields in the request forms. Subsequently uncompleted or unconventional request forms should be rejected at the radiology department to enforce standard practice.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.London: The Royal College of Radiologists; 2012. The Royal College of Radiologists. Good Practise Guide for Clinical Radiologists; pp. 2–8. [Google Scholar]
- 2.Harrogate and District NHS Foundation Trust. Yorkshire: UK: 2011. Risk Management in Radiology: A Requesting and Reporting Framework; pp. 1–15. [Google Scholar]
- 3.Davis A. 6th ed. London: The Royal College of Radiologists; 2007. Making the Best use of Radiology Services: Referral Guidelines; pp. 3–9. [Google Scholar]
- 4.Rajanikanth Rao V. Audit of radiology request forms -“Are they adequately filled?”. J Med Sci Res. 2014;2:41–4. [Google Scholar]
- 5.Afolabi OA, Fadare JO, Essien EM. Audit of completion of radiology request form in a Nigerian specialist hospital. Ann Ib Postgrad Med. 2012;10:48–52. [PMC free article] [PubMed] [Google Scholar]
- 6.Longrigg B, Channon BT. The X-ray request – An effective vehicle of communication? J Diagn Radiogr Imaging. 2006;6:35–42. [Google Scholar]
- 7.Jumah KB, Gordon-Harris L, Agahowa JI. Common faults in filling of the radiology request forms. East Afr Med J. 1995;72:744–5. [PubMed] [Google Scholar]
- 8.Irurhe NK, Sulaymon FA, Olowoyeye OA, Adeyomoye AA. Compliance rate of adequate filling of radiology request forms in a Lagos university teaching hospital. World J Med Sci. 2012;7:10–2. [Google Scholar]
- 9.Adebayo SB, Awosanya GO, Balogun BO, Osibogun A. Multicentre assessment of radiology request form completion in south-west Nigeria. Nigerian Hospital Practice Journal. 2009;3:12–3. [Google Scholar]
- 10.Depasquale R, Crockford MP. Are radiology request forms adequately filled in? An audit assessing local practice. Malta Med J. 2005;4:36–8. [Google Scholar]
- 11.Statutory Instrument No. 1059. London: HMSO; 2012. Department of Health, UK. The Ionising Radiation (Medical Exposure) Regulations 2000 (IRMER) pp. 1–26. [Google Scholar]
- 12.5th ed. London: Royal College of Radiologists (RCR); 2003. Royal College of Radiologists. Making the best use of a department of clinical radiology: Guidelines for Doctors. [Google Scholar]
- 13.Triantopoulou Ch, Tsalafoutas I, Maniatis P, Papavdis D, Raios G, Siafas I, et al. Analysis of radiological examination request forms in conjunction with justification of X-ray exposures. Eur J Radiol. 2005;53:306–11. doi: 10.1016/j.ejrad.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Akinola R, Akinkunmi M, Wright K, Orogbemi O. Radiology request forms: Are they adequately filled by clinicians? The Internet Journal of Radiology. 2009;12:1. [Google Scholar]
- 15.Akintomide AO, Ikpeme AA. Radiation safety of women of reproductive age: Evaluation of the role of referring physicians. J Family Med Prim Care. 2014;3:243–6. doi: 10.4103/2249-4863.141618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oswal D, Sapherson D, Rehman A. A study of adequacy of completion of radiology request forms. Radiography. 2009;15:209–13. [Google Scholar]


