Abstract
Introduction:
Adolescents are considered to be a nutritionally vulnerable segment of the population. There is a greater need to look into the nutritional status of adolescents but unfortunately, precise estimates of their dietary intake, dietary practices as well as nutritional deficiencies have been the least explored area. The general objective for conducting this study was to assess the dietary pattern and nutritional deficiencies among adolescents.
Materials and Methods:
A cross-sectional study was conducted among adolescents in schools and colleges in the urban areas of Jhansi district in Uttar Pradesh. The study sample consisted of 400 school children in the age group of 10-19 years. Food consumption of the subjects was assessed using a 3-day food intake recall method.
Results:
Mean age of the adolescents was 14.16 years. More than half of the children studied had malnutrition (53.5%). Mean intake of calorie, protein, fat, iron, and vitamins A and C were lower than the Recommended Dietary Allowances (RDAs). The habitual dietary pattern indicated poor consumption of milk, liver, and leafy vegetables. In comparison to boys (31.5%), more girls (46%) were underweight. On seeing the association, nutritional status of these adolescents within the normal limits were found to be significantly higher in those from nuclear families (P < 0.001), those with better educated parents (P < 0.000), and those from families of higher socioeconomic status (P < 0.000).
Conclusion:
Overall, among the participants, there were both macro- and micronutrients deficiencies. Therefore, there is a need to encourage people to adopt small family norms, and a need for the sensitization of both adolescents and their parents through health and nutrition education (HNE) to improve the health and nutritional status of the adolescents.
Keywords: Adolescents, body mass index, macronutrients, micronutrients, Recommended Dietary Allowances, under nutrition
Introduction
A balanced diet during childhood and adolescence is crucial not only for the well-being and growth of the child,[1] but also for the establishment of sound dietary habits that will persist in later life.[2] For example, adequate intake of energy and macronutrients has an essential role in the overall physical growth of the adolescent. On the other hand, vitamins and minerals have specific individual and synergistic roles in supporting metabolic function (B vitamins), bone mineralization (calcium), hemoglobin production (iron), and growth (zinc). Micronutrient deficiencies (MNDs) such as vitamin A deficiency (VAD), iron deficiency anemia (IDA), and iodine deficiency disorders (IDDs) have been major nutritional problems in developing countries, adversely affecting adolescents’ health and performance, and thereby becoming major impediments to economic development.[3] In India, these MNDs continue to be of public health significance.[4]
Nearly half of the world's micronutrient-deficient population is found in India.[5] Moreover, factors that sought to reduce the macro- and micronutrients intake of adolescents could be unequal intrafamilial distribution of food and adverse and harmful dietary practices including dieting, specific food taboos, and dietary restrictions. Poor nutrition among adolescents leads to short stature. Also, low lean body mass is associated with many concurrent and future adverse health outcomes.[6] Thus, achievement of optimum growth during this period should be of utmost importance for maintaining good health thereafter. Early detection of the morbidities through regular survey helps in prompt treatment and prevention of serious complications.[7] Therefore, keeping the magnitude of micronutrient malnutrition among the adolescents in view, the present study was carried out to assess the dietary pattern and nutritional deficiency disorders among the school-going adolescents.
Objectives
The specific objectives of the above study were the following:
To evaluate the dietary intake and nutritional status of the adolescents
To assess the prevalence of nutritional deficiencies among the adolescents
To determine whether the parents’ education and socioeconomic status are associated with the nutritional status of the adolescents or otherwise.
Materials and Methods
This was a cross-sectional study conducted in schools and colleges in the urban areas of Jhansi district in Uttar Pradesh among adolescents (age group of 10-19 years). The study was conducted from September 1 to December 31, 2014. A predesigned and pretested 3-day food frequency intake questionnaire, along with examination schedule for recording information, was used by adopting the face-to-face interview method. The data obtained were collated and statistically analyzed by simple proportions and using the tests of significance (Chi-square test). To calculate the optimum sample size required, the current prevalence of nutritional deficiency that is common in both boys and girls was taken. The relevant literature suggested that 62% of school-going children, both boys and girls, are found to be deficient in Vitamin A.[8] For the above purpose, the formula 4PQ/L2 was used, where P = 62, Q = 38, and L = allowable error in P (12%), i.e., 7.4. Thus, the sample size was worked out to be 172. Considering the design effect to be 2, the required sample size was 172 × 2 = 344. To be on the safe side and for analytical convenience, it was increased to 400 adolescents (200 boys and 200 girls). Out of all the educational institutions in the urban areas of Jhansi, eight were selected by using the cluster sampling method.
Subject to permission from the Principal of each institution, each adolescent was then individually contacted. After explaining our objectives to them and obtaining the written informed consent from the parents of each adolescent, they were interviewed in person. Dietary intake in terms of calorie, protein, fat, vitamin A, vitamin C, iron, and calcium were assessed. Thereafter, the averages were compared with the corresponding Recommended Dietary Allowances (RDAs) recommended by the Indian Council of Medical Research (ICMR).[9] The socioeconomic class and the level of education of the parents were determined by Kuppuswamy's socioeconomic status scale. Ethical clearance was sought from the Ethics Committee of Maharani Laxmibai Medical College, Jhansi, Uttar Pradesh, India. Nutritional status of the adolescents was assessed through body mass index (BMI), according to the World Health Organization (WHO) Asian criteria.[10]
Results
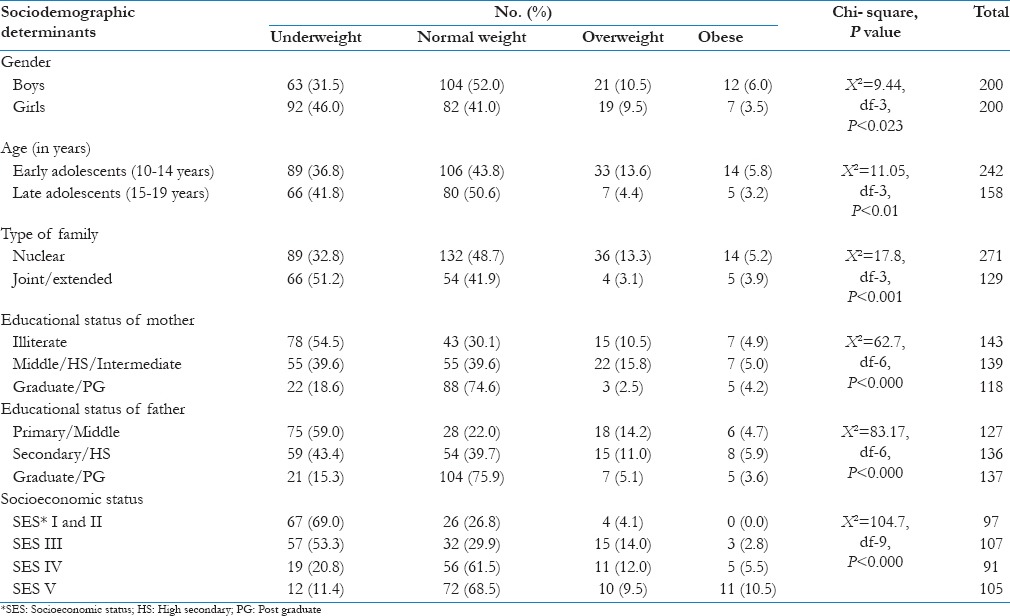
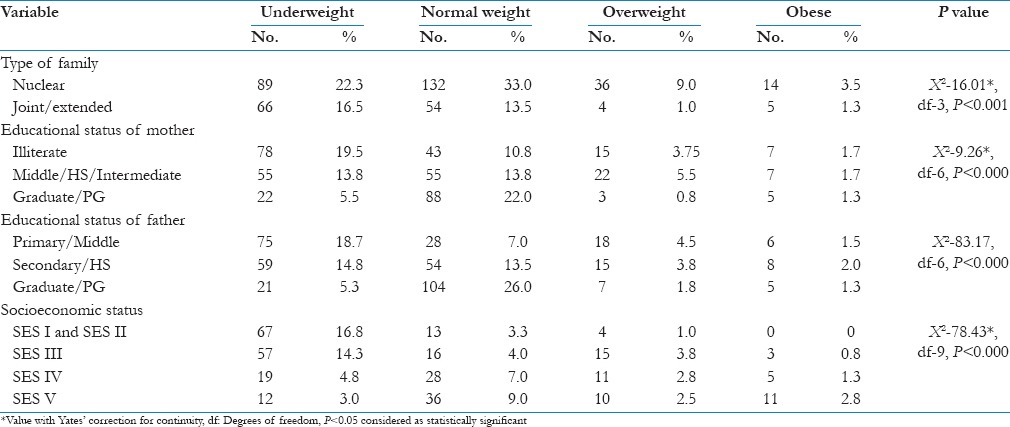
Mean age of the adolescents was 14.16 years. Of the 400 participants, majority (53.5%) were malnourished, i.e. 38.6% were underweight, 10.1% were overweight, and 4.75% were obese. It was further seen that in comparison to boys (31.5%), more girls (46%) were underweight. This may be due to particular cultural practices where the well-being of the boys are preferred to that of girls. Late adolescents (51%) were found to be more in the normal weight category than early adolescents (44%).[11] However, the early adolescents (42%) were found to be more susceptible to underweight problems compared to the late adolescents (37%). It has also been observed that a significant percentage of adolescents from nuclear families belong to the normal weight category in contrast to joint/extended families. With better education of the parents and higher socioeconomic status of the families, majority of the adolescents were able to retain their weight within the normal category, and the association was found to be highly significant [Table 1].
Table 1.
Nutritional status of adolescents and its association with sociodemographic determinants (n=400)
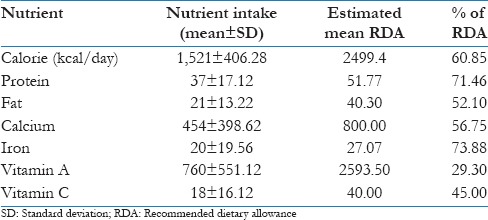
Majority of the participants consumed chapatti (94.5%) and rice (81.2%) as daily food. Most of them did not consume green leafy vegetables, milk products, fruits, and salad. Of the 400 participants, only 39.75% preferred to eat meat and fish [Table 2]. More than 50% of the participants had calorie consumption less than 80% of the RDA. Furthermore, it was also found that the consumption of macro- and micronutrients were below the par level of RDA [Figure 1]. It was further seen that the average calorie intake was 60.85% of the estimated RDA. For protein and fat, it was 71.46% and 52.10% of the estimated RDA, respectively. Vitamin A intake was only 29.30% of the estimated RDA. For calcium, iron, and vitamin C, the average intakes were 56.75%, 73.88%, and 45.00% of the estimated RDA, respectively, among the participants [Table 3].
Table 2.
Dietary consumption pattern (n=400)
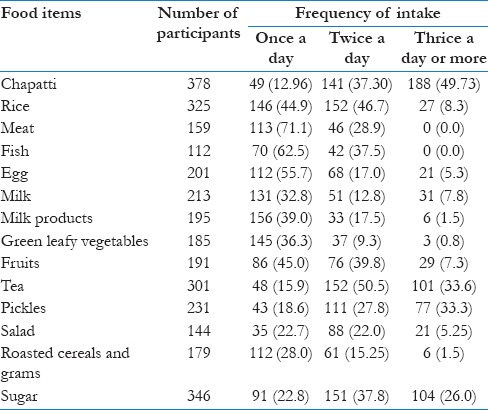
Figure 1.
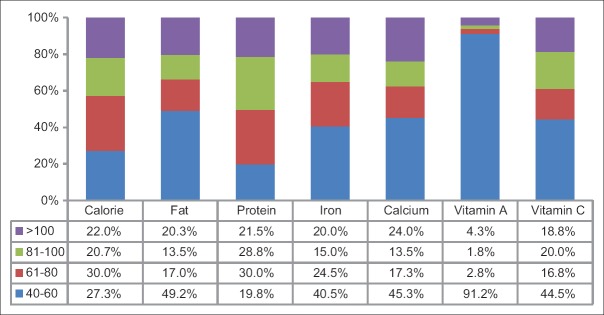
Nutrients intake in percentage to RDA (n = 400)
Table 3.
Average nutrient intake (n=400)
Discussion
Despite the fact that several national nutrition programs are in operation for the benefit of adolescents, the prevalence of nutritional deficiencies among adolescents continues to be a public health concern. In the present study, selected school-going adolescents in the age group of 10-19 years were interviewed and examined. A significant difference between the nutritional status and gender (<0.05) was found. Moreover, the early adolescents are more vulnerable to malnutrition than the late adolescents. The study conducted by Dambhar et al. had comparatively similar findings with the present study, namely, that 48.3% of the adolescents were normal and 51.7% were undernourished.[12] Kumar et al.[13] reported that 32.3% of urban school adolescents were in the normal range while 65.3% were either overweight or obese. The extent of undernutrition is lower in the present study than that reported in one Indian study (53%)[14] by Kurz et al. and in two other Kenyan studies (61%)[15] and (57%).[16]
The present study shows that dietary deficiency of both macro- and micronutrients are alarming in the study area. For vitamin A and vitamin C, the intake is less than 45% of the estimated mean RDA. These facts are so glaring that for these nutrients, urgent intervention is required. Dietary deficiencies in adolescents have also been observed by Chaturvedi et al.[17] and Eglesadi et al.,[18] where they found the deficiency of vitamin A to be glaring in their respective study areas. A study published in British Nutrition Foundation (BNF)9th section[19] has also reported that a large proportion of adolescents have low intakes of some vitamins and minerals (particularly vitamin A, riboflavin, iron, calcium, and magnesium), with more girls aged 11-18 years having low intakes compared to boys of a similar age. Another study by Akkamahadevi et al.[20] also reported lower intake of energy and blood-forming micronutrients in adolescent girls.
In the present study, it was also found that the type of family, parents’ education, and socioeconomic status of the adolescents play a pivotal role in their nutritional status. Parents with higher education show significant association with the nutritional status of the adolescents. It was also seen that higher the socioeconomic status, better the nutritional status of the adolescents [Table 4]. Documented findings in developing countries like India and Ghana report a positive association between socioeconomic status and BMI.[21] Importance of parental education in raising the nutritional status of the children is well-known.[22] Mothers’ education has profound effect on preschool children, whereas fathers’ education seems to have a greater importance in the care of adolescents.[23] Choudhury et al., in their study, found that when the nutritional status of adolescents was examined against the highest education in the family, it was evident that with the increasing level of education decline in undernutrition was noticed among the subjects. In comparison to joint families, nuclear families were more able to maintain the normal nutrition status of the adolescents.[24]
Table 4.
Relation of BMI with family characteristics of adolescents (n=400)
The strength of the study is that it is able to show the poor nutritional status among the urban adolescents. It also reveals that problem of malnutrition is multifaceted and has links with various socioeconomic and demographic factors. This study had a limitation, in that a 3-day food intake questionnaire was used instead of a 7- or 21-day one. The reason behind using a shorter version of the questionnaire was to exclude recall biases. This study also lacks biochemical assessment of the various nutrients that would have been able to give more accurate findings.
In the light of the findings, there is need and scope to design and implement adolescent nutrition education programs and establishment of operation research models.
Finally, gender differences in food habits should be taken into account, as school-based interventions aiming to improve health behaviors have been shown to influence boys and girls differently.[25,26,27] Future researches should emphasize the need for more systematic evaluation of dietary habits, including studies of consumer behavior and the role of education on food intake. Moreover, future researches should evaluate which factors contribute to social inequalities in food habits, as a basis for future differentiation of interventions among the adolescents groups. Finally, we emphasize the need for future studies of trends in the consumption habits to evaluate how adolescent food habits continue to develop.
Conclusions
The overall nutritional status of the adolescents was not satisfactory. The health and nutritional status among the adolescents was found to be low, more in girls than in boys. The prevailing dietary practices of adolescents have not been up to the mark. Such practices may be due to differences in the food allocation at the family level and because of individual likes and dislikes. Overall, among the participants, there are both macro- and micronutrients deficiencies. These deficiencies lead to a decrease in the growth spurt, for both physical and mental health.
Recommendations
A periodical and regular health check-up with concerted efforts toward their nutrition, along with focused health education will improve the health and nutritional status of these school-going adolescents. There is a need for the sensitization of adolescents and their parents through health and nutrition education (HNE), information education, and communication (IEC), and appropriate behavioral change communication (BCC) activities. Socioeconomic status of any family depends primarily on the per capita monthly income, which in turn is related to the family size; therefore, there is a need to encourage people to adapt small family norms to combat with nutrition deficiency.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Report of a Joint WHO/FAO Expert Consultation. Geneva: World Health Organisation; 2003. WHO/FAO. Diet, Nutrition and the Prevention of Chronic Diseases; p. 916. [PubMed] [Google Scholar]
- 2.Westenhoefer J. Establishing dietary habits during childhood for long-term weight control. Ann Nutr Metab. 2002;46(Suppl 1):18–23. doi: 10.1159/000066396. [DOI] [PubMed] [Google Scholar]
- 3.Bowley A. Alliances against hunger. Editorial. Nutriview. 2008;4:2. [Google Scholar]
- 4.Vijayaraghavan K. Control of micronutrient deficiencies in India: Obstacles and strategies. Nutr Rev. 2002;60:S73–6. doi: 10.1301/00296640260130786. [DOI] [PubMed] [Google Scholar]
- 5.India: USAID; 2005. USAID. USAID'S OMNI Micronutrient Fact Sheets. [Google Scholar]
- 6.Geneva: World Health Organization; 1995. Physical status: The use and Interpratation of Anthropometry. Technical Report Series. Report No: 854. [PubMed] [Google Scholar]
- 7.Panda P, Benjamin AI, Singh S, Zachariah P. Health status of school children in Ludhiana city. Indian J Community Med. 2000;25:150–5. [Google Scholar]
- 8.Laxmaiah A, Nair MK, Arlappa N, Raghu P, Balakrishna N, Rao KM, et al. Prevalence of ocular signs and subclinical vitamin A deficiency and its determinants among rural pre-school age children in India. Public Health Nutr. 2012;15:568–77. doi: 10.1017/S136898001100214X. [DOI] [PubMed] [Google Scholar]
- 9.Hyderabad, India: National Institute of Nutrition; [Last accessed on 2015 Feb 26]. Dietary Guidelines for Indians: A Manual. Available from: http://www.ninindia.org/DietaryguidelinesforIndians-Finaldraft.pdf . [Google Scholar]
- 10.BMI (Body Mass Index) Classification for Asians. [Last accessed on 2013 Apr 12]. Available from: http://www.protectyourhealthtips.blogspot.in/2013/04/bmi-body-mass-index-classification-for-html .
- 11.Early and Late Adolescence. [Last accessed on 2015 Mar 15]. Available from: http://www.unicef.org/sowc2011/pdfs/Early-and-late-adolescence.pdf .
- 12.Dambhare DG, Bharambe MS, Mehendale AM, Garg BS. Nutritional Status and Morbidity among School going Adolescents in Wardha, a Peri-Urban area. [Last accessed on 2015 Mar 16]. Available from: http://www.ojhas.org/issue34/2010-2-3.htm .
- 13.Saha SK, Bag T, De AK, Basak S, Biswas SC, Ghosh Roy SC. Adolescent girls’ health profile in sub-Himalayan region of West Bengal. J Obstet Gynecol India. 2006;56:329–32. [Google Scholar]
- 14.Kurz KM. Adolescent nutritional status in developing countries. Proc Nutr Soc. 1996;55:321–31. [PubMed] [Google Scholar]
- 15.Cookson ST, Woodruff BA, Slutsker L. Atlanta: Centers for Disease Control and Prevention; 1998. Prevalence of Anemia and Low Body Mass Index among Adolescents 10–19 Years of Age in Refugee Camps in Dadaab District, Kenya. [Google Scholar]
- 16.Woodruff BA, Slutsker L, Cook ST. Atlanta: Centers for Disease Control and Prevention; 1998. Prevalence of anemia and low body-mass-index in adolescents 0–19 years age in Kakuma camp, Kenya. [Google Scholar]
- 17.Chaturvedi S, Kapil U, Bhanti T, Gnanasekaran N, Pandey RM. Nutritional status of married adolescent girls in rural Rajasthan. Indian J Pediatr. 1994;61:695–701. doi: 10.1007/BF02751982. [DOI] [PubMed] [Google Scholar]
- 18.Eglesadi S, Zargari F, Hoseinalizadeh L, Ansari N, Berengei S, Amane R, et al. Iran: 2000. Prevalence of Malnutrition and Food Insecurity in Adolescent Girls in Iran. [Google Scholar]
- 19.BNF9. [Last accessed on 2015 Mar 14]. Available from: http://www.nutrition.org.uk/nutritionscience/life/teenagers.html .
- 20.Akkamahadevi KH, Kasturiba B, Katarki PA. Energy and blood forming nutrients in the diets of urban and rural adolescent girls. The Indian J Nutr Diet. 1995;35:207–215. [Google Scholar]
- 21.Tharkar S, Viswanathan V. Impact of socioeconomic status on prevalence of overweight and obesity among children and adolescents in urban India. Open Obes J. 2009;1:9–14. [Google Scholar]
- 22.Spyckerelle Y, Herbeth R, Didelot-Barthélemy L, Bairati I, Deschamps JP. Nutrition of adolescent girls in Lorraine. Arch Fr Pediatr. 1990;47:455–9. [PubMed] [Google Scholar]
- 23.Srivastava VK, Srivastava BC, Nandan D, Bhushan V. Protein energy malnutrition amongst pre-school children in rural population of Lukhnow. Indian Pediatr. 1979;16:507–13. [PubMed] [Google Scholar]
- 24.Choudhury S, Mishra CP, Shukla K. Correlates of nutritional status of adolescent girls in the rural area of Varanasi. Internet J Nutr Wellness. 2008;7:53–61. [Google Scholar]
- 25.Bjelland M, Bergh IH, Grydeland M, Klepp KI, Andersen LF, Anderssen SA, et al. Changes in adolescents’ intake of sugar-sweetened beverages and sedentary behaviour: Results at 8 month mid-way assessment of the HEIA study–a comprehensive, multi-component school-based randomized trial. Int J Behav Nutr Phys Act. 2011;8:63. doi: 10.1186/1479-5868-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grydeland M, Bjelland M, Anderssen SA, Klepp KI, Bergh IH, Andersen LF, et al. Effects of a 20-month cluster randomised controlled school-based intervention trial on BMI of school-aged boys and girls: The HEIA study. Br J Sports Med. 2014;48:768–73. doi: 10.1136/bjsports-2013-092284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grydeland M, Bergh IH, Bjelland M, Lien N, Andersen LF, Ommundsen Y, et al. Intervention effects on physical activity: The HEIA study – a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:17. doi: 10.1186/1479-5868-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]


